Beruflich Dokumente
Kultur Dokumente
Group A Streptococcal Carrier Versus Acute Infection - The Continuing Dilemma
Hochgeladen von
Jehimy AlvarezOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Group A Streptococcal Carrier Versus Acute Infection - The Continuing Dilemma
Hochgeladen von
Jehimy AlvarezCopyright:
Verfügbare Formate
E D I T O R I A L C O M M E N TA R Y
Group A Streptococcal Carrier versus Acute Infection: The Continuing Dilemma
Harry R. Hill
Departments of Pathology, Pediatrics, and Medicine, University of Utah School of Medicine, and the ARUP Institute for Clinical and Experimental Pathology, Salt Lake City, Utah
(See the article by Johnson et al, on pages 48190.)
An age old question reappears in the article by Johnson et al in this issue of Clinical Infectious Diseases [1]. Dening what is an acute infection due to group A streptococci versus the carrier state of this very common pathogen is of considerable signicance because nonsuppurative sequelae, such as acute rheumatic fever and acute glomerulonephritis, are said to only follow acute disease. Moreover, transmission of group A streptococci and the development of invasive disease are felt to be associated more often, if not exclusively, with a new acquisition and acute infection rather than the carrier state. The problem, of course, is that as much as 20%25% of the school-age population may be positive for group A streptococci during the late winter and spring months, even extending into June here in Utah. Intercurrent, viral infection may result in the patient being seen and tested by antigen detection or group A streptococcal culture for this very common pathogen. A positive result for streptococci will likely
Received 10 September 2009; accepted 16 November 2009; electronically published 12 January 2010. Reprints or correspondence: Dr Harry R. Hill, University of Utah School of Medicine 5B, Dept of Pathology, Salt Lake City, UT 84132 (hillhr@aruplab.com.). Clinical Infectious Diseases 2010; 50:4912 2010 by the Infectious Diseases Society of America. All rights reserved. 1058-4838/2010/5004-0006$15.00 DOI: 10.1086/650168
result in antimicrobial therapy being administered for 510 days, depending on the antimicrobial agent selected, because such therapy has been shown to markedly decrease the incidence (90%) of acute rheumatic fever, decrease acute glomerulonephritis by perhaps 50%, and aid in preventing invasive disease and further spread. Numerous authors, including these same investigators at the University of Minnesota, have pointed out that serologic studies targeting nonspecic streptococcal extracellular products, such as streptolysin O and DNase B, may be useful in differentiating the carrier state of group A streptococci from acute infection. Longitudinal analysis of group A streptococcal culture results combined with sequential serologic studies have conrmed what Zimmerman et al [2] reported years ago in patients and families they followed in 3 Colorado communities. This group reported that certain families acquired a new streptococcal M or T type that often persisted in individual patients and the family for extended periods of time, up to 23 years in some cases. These carriers often developed signicantly elevated nonspecic streptococcal antibody responses but almost never seem to develop nonsuppurative sequelae. The present studies by Johnson et al [1] certainly conrm those ndings. As one who has observed the streptococcal world for the past 40 years,
including working with the group at the Fort Collins Centers for Disease Control and Prevention Streptococcal Disease Laboratory and with the streptococcal group at the University of Minnesota, I am struck by how often important observations in medicine have to continue to be remade to affect the current status of medical care. Our memory may be too short or perhaps we just need to refocus our attention to what we may already know and make use of it in medical decision making. As one who directs a large clinical immunology laboratory at the University of Utahowned Associated Regional and University Laboratories as well as being a clinician, I can only agree with the ndings and comments of Johnson and colleagues on the inadequacy of using a single serologic result to try to predict the presences of acute infection versus chronic carriage of an organism. In my experience, a single serologic response, especially to something as common and nonspecic as streptolysin O and DNase B, should never be used to distinguish between acute infection and the carrier state or even the response to vaccination. One has to look at acute and convalescence responses to determine whether there is a new exposure to a particular pathogen. The overall concentration of that antibody in the acute sample likely depends on past exposure to that or similar pathogens, vaccination,
EDITORIAL COMMENTARY CID 2010:50 (15 February) 491
cross-reacting microbes, or even the individual immunologic responsiveness or characteristics of decay of the antibody response in the patient. Comparison to normal values obtained from healthy, agematched controls, in my opinion, has little role in dening the presences of acute infection or vaccine responses to an individual pathogen or one of its components. One must have serologic sampling over time to rationally use such data. This brings up another question about the clinical usefulness of the excellent data contained in the article by Johnson et al [1], especially to the practicing clinician. These data suggest that serologic studies performed on at least 2 occasions, 24 weeks apart, can perhaps separate the patient with acute group A streptococcal pharyngitis from the chronic carrier of this pathogen. Currently, the busy pediatrician or family practitioner or perhaps even the local mini-clinics physicians assistant or nurse practitioner has only time to collect a swab for antigen detection for group A streptococci, which hopefully is followed by culture for this organism if the result is negative (because such rapid tests are only 80%90% sensitive). To prevent
acute rheumatic fever, recommendations are for 10 days of antimicrobial therapy (shorter courses with a 6-pack of antibiotics, such as azithromycin, has not always prevented acute rheumatic fever in our experience here in Utah; L.G. Veasy and H.R.H., unpublished observations) initiated shortly after the detection of the organism. Very early therapy is also needed to show any benet in preventing acute glomerulonephritis, and only very early treatment has been demonstrated to shorten the clinical course of streptococcal pharyngitis. Waiting 24 weeks for a serologic response is simply unacceptable as routine criteria for detecting acute infection versus the carrier state in the practicing clinicians setting. Could early antibody responses or even T cell responses (such as cytokines) to specic or nonspecic streptococcal antigens be detectable at the time of acute infection? Perhaps this possibility needs to be explored in the future. The above comments should not be misconstrued as indicating that the study by Johnson and colleagues is not of real value in understanding group A streptococcal infections and their nonsuppurative
sequelae. Just by pointing out that a single elevated group A streptococcal serologic antibody determination cannot always indicate that an observed clinical disorder is ascribable to a past or present group A streptococcal infection, the authors have done a great service. If one were to demand that such sequential serologic and culture-based data be present to conrm the streptococcal etiology of certain syndromes, it is likely that a causative agent or event would still be sought for PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococci) and obsessive/compulsive disorders. Perhaps Dr Kaplans group, as indicated, will address this question in a future study.
Acknowledgment
Potential conicts of interest. H.R.H.: no conicts.
References
1. Johnson DR, Kurlan R, Leckman J, Kaplan EL. The human immune response to streptococcal extracellular antigens: clinical, diagnostic and potential pathogenetic implications. Clin Infect Dis 2010; 50:481-90 (in this issue). 2. Zimmerman RA, Wilson E, Familial susceptibility to acquisition of group A b-hemolytic streptococci. Am J Dis Child 1968; 116:292300.
492 CID 2010:50 (15 February) EDITORIAL COMMENTARY
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Window of Tolerance GuideDokument19 SeitenWindow of Tolerance GuideLê Trung DũngNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Foundations of Addictions Counseling, 4th EditionDokument509 SeitenFoundations of Addictions Counseling, 4th EditionWesleyNoch keine Bewertungen
- CureDokument338 SeitenCureThiago Cavalli Azambuja100% (1)
- Assignment 2 HLTH 103 Bhima Devi Poudel Adhikari 220179000Dokument10 SeitenAssignment 2 HLTH 103 Bhima Devi Poudel Adhikari 220179000api-525310113Noch keine Bewertungen
- Ig2-Latest Format AugustDokument24 SeitenIg2-Latest Format AugustFaizan AliNoch keine Bewertungen
- Birth AsphyxiaDokument32 SeitenBirth AsphyxiaSANCHAYEETANoch keine Bewertungen
- T1 (Introduction To Inclusive Education) PDFDokument50 SeitenT1 (Introduction To Inclusive Education) PDFBlossomsky9675% (4)
- Consciousness: Darren J. Gonzales Faculty, College of Arts and SciencesDokument46 SeitenConsciousness: Darren J. Gonzales Faculty, College of Arts and SciencesDarren Javier GonzalesNoch keine Bewertungen
- Pathology MBBSDokument12 SeitenPathology MBBSDinah Penserga100% (1)
- Vaishali Bujad Project..2Dokument54 SeitenVaishali Bujad Project..2Mitesh Prajapati 7765Noch keine Bewertungen
- K-37 Septic Tank Treatment SDSDokument7 SeitenK-37 Septic Tank Treatment SDSRicardo AlvaradoNoch keine Bewertungen
- Asthma Management in 40 CharactersDokument10 SeitenAsthma Management in 40 CharactersAmalNoch keine Bewertungen
- Ethical Issues Faced by Nurses During Nursingpractice in District Layyah PakistanDokument7 SeitenEthical Issues Faced by Nurses During Nursingpractice in District Layyah PakistanMawadah Setya RahmawatiNoch keine Bewertungen
- Viva XT Brochure - 201203539IEp3Dokument6 SeitenViva XT Brochure - 201203539IEp3Lubna LuaiNoch keine Bewertungen
- Block M2 EYE Distribution by MMCDokument3 SeitenBlock M2 EYE Distribution by MMCF ParikhNoch keine Bewertungen
- Daftar AntibiotikDokument448 SeitenDaftar AntibiotikevaNoch keine Bewertungen
- TFNVirginia HendersonDokument13 SeitenTFNVirginia HendersonJheslyn BalagulanNoch keine Bewertungen
- Pharmacology: A Career inDokument2 SeitenPharmacology: A Career insnikt7863443Noch keine Bewertungen
- Glaucoma Management and Target IOPDokument24 SeitenGlaucoma Management and Target IOPElfi RisalmaNoch keine Bewertungen
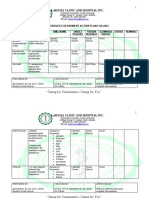
- Maternity and Newborn MedicationDokument34 SeitenMaternity and Newborn MedicationNicholas ClaytonNoch keine Bewertungen
- SOCIAL SERVICES aCTION PLAN FOR 2022Dokument6 SeitenSOCIAL SERVICES aCTION PLAN FOR 2022Rocel Cañete Ordoyo-GabrielNoch keine Bewertungen
- Lupus and Pregnancy ComplicationsDokument4 SeitenLupus and Pregnancy ComplicationsDivika ShilvanaNoch keine Bewertungen
- Curriculum: Minimal Access UrologyDokument14 SeitenCurriculum: Minimal Access UrologyANOOP HANDANoch keine Bewertungen
- Bias and Confounding: Nayana FernandoDokument31 SeitenBias and Confounding: Nayana FernandoanojNoch keine Bewertungen
- SCSD Application Summary Form PDFDokument2 SeitenSCSD Application Summary Form PDFJoserie HernaneNoch keine Bewertungen
- Mic Ielts Speaking Exercises-VDokument22 SeitenMic Ielts Speaking Exercises-VAbhilaksh MohanNoch keine Bewertungen
- Legacy of Tuskegee Syphilis StudyDokument2 SeitenLegacy of Tuskegee Syphilis StudyLcgessamanNoch keine Bewertungen
- How Doctors ThinkDokument3 SeitenHow Doctors ThinkRubad UstNoch keine Bewertungen
- 0 Notes 190815 204331 f4b PDFDokument4 Seiten0 Notes 190815 204331 f4b PDFLovejeet KaurNoch keine Bewertungen
- Bryana Russell Cover LetterDokument1 SeiteBryana Russell Cover Letterapi-303090959Noch keine Bewertungen