Beruflich Dokumente
Kultur Dokumente
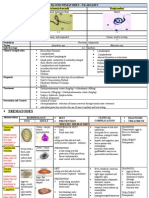
Pharmacology of Adrenergic Agonists
Hochgeladen von
fiena92Originalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pharmacology of Adrenergic Agonists
Hochgeladen von
fiena92Copyright:
Verfügbare Formate
Physiologic considerations of Sympathetic system
Classify Nervous system Central Nervous system - Brain; Spinal cord Peripheral Nervous system ( efferent) Somatic ( Voluntary control) Autonomic ( Involuntary control) Sympathetic Parasympathetic
Name the neurotransmitters (NT) in somatic ANS and the respective receptors Nerve fibre Organ supplied NT Receptor Somatic Skeletal muscle Acetylcholie (Ach) Nicotinic (Nm) Parasympathetic & Ganglia & Ach Nicotinic ( Nn) Sympathetic Preganglionic Adrenal medulla Postganglionic Visceral organs Ach Muscarinic parasympathetic (M) Postganglionic Visceral organs Nor adrenaline (NA) , sympathetic Adrenal medulla (into Visceral organs Adrenaline (Ad) , blood circulation)
List the steps involved in neuronal transmission Impulse conduction Transmitter release Transmitter action of Postjunctional membrane Post junctional activity Termination of transmitter action
How the action of NT is terminated? Ach- action terminated by metabolism by the enzyme acetyl cholinesterase (AChE) present in the synaptic cleft. There is an enzyme pseudocholinesterase ( PChE) in the plasma, liver, the physiological function of which is not known. Since the Ach released by the nerve ending is immediately metabolized hence no Ach in blood circulation for PChE to metabolize it. NA: action is terminated by axonal uptake and subsequently vesicular uptake or metabolism by Monoamino oxidase (MAO) enzyme in the axonal cytoplasm. NA in the synaptic cleft can diffuse into blood and metabolized by liver enzyme catecholamine-omethyltransferase (COMT)& MAO. Ad & NA released by adrenal medulla are metabolized by COMT & MAO in liver.
Axonal Uptake
17
State the physiological importance of Autonomic responses Cholinergic responses meant for Rest & Digest ( Digestion & Absorption of nutrients) Adrenergic responses meant for Fight or Flight - Pupillary dilatation (1) to see properly ; cardiac output (1) to maintain blood supply to myocardium, brain and skeletal muscle; bronchodilatation for more Oxygen supply; skeletal muscle function supported by increased blood supply (2vasodilatation) and energy production (2 glycogenolysis)
State the chemical transmitters involved in adrenergic functions Noradrenaline (Norepinephrine) is the neurotransmitter secreted by the sympathetic nerve endings to the synaptic cleft to act at 1 & 2 & 1receptors. Adrenaline is the hormone released by the adrenal medulla (a modified ganglion without postsynaptic fibres). Adrenaline from blood will act at 2 receptors which are not located with sympathetic nerve terminals and also can diffuse into the synaptic cleft and act at 1& 1receptors Dopamine, a precursor of both Adrenaline & Nor adrenaline is a neurotransmitter at adrenergic nerve terminals supplying splanchnic and renal vascular smooth muscle
Actions of Noradrenaline / Adrenaline at different receptors 1 Vasoconstriction Mydriasis 2 pre synaptic NE release pre synaptic Ach release Sympathetic outflow from brain medulla 1 Heart rate Myocardial contractility AV conduction 2 Vasodilatation Bronchodilatation
Bladder sphincter muscle, liver closure glycogenolysis GIT spincter Renal rennin Relaxation of uterine closure release smooth muscle Livergluconeogenesis Ejaculation male genital D1 receptors- vasodilatation of mesenteric and renal blood vessels
Flight & Fight - Adrenergic Responses
Pharmacology of Adrenergic Receptor Agonists
Classify adrenergic receptor agonists (drugs) / sympatho mimetic (SM) drugs SM drugs are basically classified based on structure Catecholamines & Noncatecholamines What is the therapeutic significance of this structural difference? Catecholamines are inactive by oral rout as metabolized by GIT MAO & COMT so only injected; Even when injected by IV route has few minutes of action because of metabolism by liver MAO & COMT; where as Non cate cholamines can be given by oral route and when injected have long duration of action. Can still cross BBB unlike catecholamines. Noncatecholamines are once again classified on receptor specific action.
Catecholamines Adrenaline Dopamine Dobutamine
Noncatecholamines 1-Selective agonists 2-Selective agonists 2-Selective agonists
List the therapeutic uses of Adrenaline with basis 1. Anapahylactic shock: Purpose is to maintain BP Basis: In anaphylactic shock, antigen-antibody reaction leads to severe vasodilatation, there is drastic fall in BP so the perfusion to vital organs is cut off. Adrenaline when injected IV (1:10000 solution) or IM (1,1000 solution) increases cardiac output (1) thereby maintains BP and perfusion to vital organs. Anaphylactic mediators can also bring about bronchoconstriction relieved by Adrenaline (2mediated bronchodilatation). Anaphylactic reactions can result in edema of mucosa because of capillary dilatation that can be relieved by Adrenaline (1mediated vasoconstriction) 2. Cardiac arrest: Purpose is to maintain cardiac rhythmicity Electrocution and salt water drowning can stop heart suddenly due to stop in pacemaker activity. 0.1/ml Adrenaline injected into the cardiac ventricular lumen maintains rhythm city of myocardium by 1 activation. In anaphylactic shock, since blood is not in movement in blood vessels, IV injection does not help for the drug to reach myocardium. So need to inject directly into heart 3. Adrenaline when applied on mucosa (1:100,000) brings about 1 vasoconstriction decreases bleeding. Can be used in nasal bleeding
4. Used along with a local anesthetic (1:100,000) during minor surgeries: Adrenaline (1)vasoconstriction decreases the washing away of local anesthetic (LA) from the site of injection into blood circulation hence prolongs the duration of action of LA at the site of surgery. In the first two conditions, Adrenaline is a life saving drug. Whereas in the last two cases, Adrenaline is not life saving ; use otptional so one must weigh the benefits of using it over the risks ( hypertensive crisis; cardiac arrhythmias; cerebral hemorrhage)
What are the therapeutic uses of Dopamine Dopamine is used in Cardiogenic shock, septic shock to maintain BP In these conditions, because of renal vasoconstriction, renal blood flow is compromised. Dopamine at doses 5 -10 microgram/ Kg/ min infusion- 1 mediated increase in CO and maintaining BP and renal vasodilatation (D1receptor). At higher doses, Dopamine (1) renal blood vessels and precipitate acute renal failure. So dose needs to be titrated carefully. Adrenaline should not be used to maintain BP as it is further going to constrict renal blood vessels (1) and precipitate acute renal failure.
What are uses of Dobutamine Cardiogenic shock, septic shock Acute cardiac failure- to maintain BP Dobutamine acts at 1 & 1 receptors. Maintains BP. (Advantage) Dobutamine produces less of tachycardia compared to Dopamine. (Disadvantage) Dobutamine produces renal vasoconstriction , so whenever renal blood flow is drastically decreased, Dopamine is preferred over Dobutamine
Name 1 receptor selective agonists & Uses Methoxamine, Phenylephrine, Ephedrine: During spinal anesthesia, due to blockade to sympathetic outflow ( lumbar) to blood vessel, vasodilatation takes place resulting in fall of BP. These drugs (IV) route) bring about 1 mediated vasoconstriction that helps to rise BP. Pseudoephedrine, Phenyl propanolamine: used by oral route to decrease mucosal
edema of nasal mucosa in rhinitis. In rhinitis, there is inflammation of nasal mucosa and vasodilatation in nasal mucosa resulting in edema. Vasoconstriction by these drugs decrease the fluid movement from vascular compartment to extra vascular space and there by decreases edema. Xylometazoline, Naphazoline (Nasal de congestants) : used as nasal drops to decrease mucosal edema of nasal mucosa in rhinitis. Prolonged use can result in atrophic rhinitis and also rebound rhinitis on stopping List 2-Selective agonists and their therapeutic use Salbutamol, Terbutaline; Salmeterol These drugs bring about 2-receptor bronchodilatation hence used in treatment of bronchial asthma ( will be discussed during a separate class in respiratory module)
List 2-Selective agonists and uses Clonidine; Methyl dopa Used in treatment of hypertension to bring down BP Physiological regulation of BP involves baroceptor reflex pathway. Rise in BP stretches the baro receptors of carotid sinus and aortic arch which send impulses to vasomotor center (VMC) of medulla. VMC inhibits (Noradrenaline acts at 2 receptor) sympathetic flow to Heart (CO) and blood vessels (vasodilatation) both leading to BP. This is the physiological regulation of BP. This VMC inhibition of sympathetic outflow involves NA activation of 2receptors in medulla The above 2 drugs act at the same 2 receptors at VMC in place of nor adrenaline resulting in decreased sympathetic outflow and fall in BP.
Baro receptor reflex regulation of BP
Methyldopa Clonidine agonists
Medulla
12
2 selective agonists Slabutamol, Terbutaline Agonist at 2 receptors in bronchial smooth muscle bronchodilatation. Used in treatment of bronchial asthma
13
Das könnte Ihnen auch gefallen
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingVon EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováNoch keine Bewertungen
- Clinical Physiology and Pharmacology: The EssentialsVon EverandClinical Physiology and Pharmacology: The EssentialsBewertung: 4 von 5 Sternen4/5 (1)
- Adrenergic AntagonistsDokument6 SeitenAdrenergic Antagonistsfiena92100% (2)
- Cholinergic DrugsDokument32 SeitenCholinergic DrugsApt FianNoch keine Bewertungen
- Cholinergic Antagonists "Anticholinergic Drugs" (ParasympatholyticsDokument32 SeitenCholinergic Antagonists "Anticholinergic Drugs" (ParasympatholyticsmiznahNoch keine Bewertungen
- Cholinergic and AnticholinergicDokument77 SeitenCholinergic and Anticholinergicsweta sumanNoch keine Bewertungen
- Introduction To Cns PharmacologyDokument66 SeitenIntroduction To Cns PharmacologyYazan Emad Salem100% (1)
- Adrenergic Receptors ChartDokument1 SeiteAdrenergic Receptors ChartLeon ChenNoch keine Bewertungen
- Cell Wall InhibitorsDokument52 SeitenCell Wall InhibitorsApurba Sarker Apu100% (1)
- Pharmacology of The GITDokument31 SeitenPharmacology of The GITmarviecute22Noch keine Bewertungen
- Introduction To Autonomic PharmacologyDokument55 SeitenIntroduction To Autonomic PharmacologyMuammar Alfarouq100% (1)
- PharmacologyDokument3 SeitenPharmacologyMohd Afiq AizuddinNoch keine Bewertungen
- Antiviral Drugs Acting Against RNA Viruses: HIV: PHRM 412Dokument57 SeitenAntiviral Drugs Acting Against RNA Viruses: HIV: PHRM 412Apurba Sarker ApuNoch keine Bewertungen
- Cell Wall Inhibitor PPT SlideDokument47 SeitenCell Wall Inhibitor PPT Slidekhawaja sahabNoch keine Bewertungen
- Aminogycoside AntibioticsDokument31 SeitenAminogycoside AntibioticsNurul Febrina100% (2)
- Clinical Pharmacology, Toxicology and Poisoning: 1. Drug Metabolism and InteractionsDokument26 SeitenClinical Pharmacology, Toxicology and Poisoning: 1. Drug Metabolism and InteractionsNadia Ancharuz100% (1)
- Sem 5/unit-3 Autocoids & Related DrugsDokument28 SeitenSem 5/unit-3 Autocoids & Related DrugsDARSHAN BhirudNoch keine Bewertungen
- Antiplatelet and Thrombolytic DrugsDokument48 SeitenAntiplatelet and Thrombolytic DrugsNofa PuspitaNoch keine Bewertungen
- Pharmacology of Autonomic Nervous SystemDokument106 SeitenPharmacology of Autonomic Nervous Systemoscar3spurgeonNoch keine Bewertungen
- Lecture 4, 5 - Drugs Used in Bronchial Asthma & COPDDokument57 SeitenLecture 4, 5 - Drugs Used in Bronchial Asthma & COPDBalakrishnan Thangaraj100% (1)
- Pharma ChartsDokument33 SeitenPharma ChartsNooreen Hussain100% (1)
- Cardiovascular PharmacologyDokument61 SeitenCardiovascular PharmacologyTeeOne920% (1)
- 6 Beta Adrenergic BlockersDokument19 Seiten6 Beta Adrenergic Blockersmatchees-gone rogue100% (1)
- 2&3-Pharmacology of Drugs Used in Bronchial Asthma & COPDDokument58 Seiten2&3-Pharmacology of Drugs Used in Bronchial Asthma & COPDKishan SethNoch keine Bewertungen
- Drug Interactions: What Is An Interaction?Dokument4 SeitenDrug Interactions: What Is An Interaction?Leyla MajundaNoch keine Bewertungen
- Parasympathetic Pharmacology Drugs Muscarine and Nicotinic RecpetorsDokument56 SeitenParasympathetic Pharmacology Drugs Muscarine and Nicotinic RecpetorsMatthewNoch keine Bewertungen
- Drugs Acting On The Gastrointestinal TractDokument27 SeitenDrugs Acting On The Gastrointestinal TractJames PerianayagamNoch keine Bewertungen
- Summary of Adrenergic DrugsDokument3 SeitenSummary of Adrenergic DrugsrabduljabarrNoch keine Bewertungen
- Pharmacology Notes: By: Khurram AbbasDokument48 SeitenPharmacology Notes: By: Khurram AbbasAsma AnjumNoch keine Bewertungen
- AntiemeticsDokument10 SeitenAntiemeticsnk999999100% (1)
- Adrenergic AntagonistsDokument23 SeitenAdrenergic AntagonistsMirza Shaharyar BaigNoch keine Bewertungen
- Key Point Summaries Pharmacy Examination Preparation NotesDokument38 SeitenKey Point Summaries Pharmacy Examination Preparation NotesArrian JanfadaNoch keine Bewertungen
- 7 - Cholinomimetic DrugsDokument50 Seiten7 - Cholinomimetic DrugslalitrajindoliaNoch keine Bewertungen
- Mechanism of Action For Each Class of AntiDokument146 SeitenMechanism of Action For Each Class of AntiReynaldo RiveraNoch keine Bewertungen
- Pharmacology2 (Drug Receptors & Pharmacodynamics)Dokument58 SeitenPharmacology2 (Drug Receptors & Pharmacodynamics)Durge Raj Ghalan100% (2)
- Antibiotics 9Dokument11 SeitenAntibiotics 9Beth Morales100% (1)
- Autocoids and Their AntagonistsDokument19 SeitenAutocoids and Their AntagonistsHossein Sehati100% (1)
- Cholinergic Anticholinergic DrugsDokument60 SeitenCholinergic Anticholinergic DrugsMD. RASEL MAHMUD MIMNoch keine Bewertungen
- ANS-Pharmacology Adrenergic DrugsDokument65 SeitenANS-Pharmacology Adrenergic DrugsMarc Imhotep Cray, M.D.75% (4)
- ANS PharmacologyDokument58 SeitenANS Pharmacologyalemu100% (1)
- AutacoidsDokument32 SeitenAutacoidsRenellie TrimidalNoch keine Bewertungen
- Pharmacology McqsDokument7 SeitenPharmacology McqsAshraf AboNoch keine Bewertungen
- Pharmacology of Drugs Used in Bronchial Asthma & COPDDokument84 SeitenPharmacology of Drugs Used in Bronchial Asthma & COPDdfngjlnNoch keine Bewertungen
- Anti Parkinson Drugs FinallDokument36 SeitenAnti Parkinson Drugs FinallandrapradeshsseNoch keine Bewertungen
- AntiemeticsDokument25 SeitenAntiemeticsPridho GaziansyahNoch keine Bewertungen
- GIT DrugsDokument180 SeitenGIT DrugsMaria Linevel Balderamos Dalida100% (1)
- PharmacologyDokument74 SeitenPharmacologyKiara Denise Tamayo100% (1)
- 4 - Pharmacology-II QP BankDokument8 Seiten4 - Pharmacology-II QP BankMadhu Kiran DhondalayNoch keine Bewertungen
- Cholinergic DrugsDokument44 SeitenCholinergic Drugskhuzaima9100% (1)
- Pharmacology Summary Notes Unit 9Dokument9 SeitenPharmacology Summary Notes Unit 9Denny HempataweeNoch keine Bewertungen
- Drugs Affecting The Autonomic Nervous System (ANS)Dokument40 SeitenDrugs Affecting The Autonomic Nervous System (ANS)HiwaNoch keine Bewertungen
- Autacoids: Group No. 1Dokument92 SeitenAutacoids: Group No. 1Rohan Pal100% (1)
- Adrenergics & Adrenergic BlockersDokument5 SeitenAdrenergics & Adrenergic Blockersapi-3739910100% (4)
- Anti-Viral Drugs AltDokument42 SeitenAnti-Viral Drugs AltSidraNoch keine Bewertungen
- Clinical Pharmacology: Proceedings of the 7th International Congress of Pharmacology, Paris 1978Von EverandClinical Pharmacology: Proceedings of the 7th International Congress of Pharmacology, Paris 1978P. Duchêne-MarullazNoch keine Bewertungen
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): An OverviewVon EverandNSAIDs (Nonsteroidal Anti-Inflammatory Drugs): An OverviewNoch keine Bewertungen
- Pharmacology of Cholinergic and Adrenergic Transmission: Proceedings of the Second International Pharmacological Meeting, August 20—23, 1963Von EverandPharmacology of Cholinergic and Adrenergic Transmission: Proceedings of the Second International Pharmacological Meeting, August 20—23, 1963G. B. KoelleNoch keine Bewertungen
- Pharmacology of Autonomic Nervous System Cholinergic AgonistsDokument6 SeitenPharmacology of Autonomic Nervous System Cholinergic Agonistsfiena920% (1)
- Muscarinic (M) Receptor Blockers (Antagonists) Anti Muscarinic Drugs Anti Cholinergic DrugsDokument4 SeitenMuscarinic (M) Receptor Blockers (Antagonists) Anti Muscarinic Drugs Anti Cholinergic Drugsfiena92Noch keine Bewertungen
- Adverse Drug ReactionDokument5 SeitenAdverse Drug Reactionfiena92Noch keine Bewertungen
- Helminth Revision 2Dokument1 SeiteHelminth Revision 2fiena92Noch keine Bewertungen
- Helminth 5Dokument5 SeitenHelminth 5fiena92100% (2)
- Helminth 4Dokument1 SeiteHelminth 4FarlogyNoch keine Bewertungen
- Protozoa RevisionDokument6 SeitenProtozoa Revisionfiena92100% (1)
- Helminth 3Dokument2 SeitenHelminth 3Farlogy100% (6)
- CellDokument36 SeitenCellNORHANANI BINTI BAJURI STUDENT100% (1)
- Anatomy and Physiology of Intrinsic Cardiac Autonomic Nervous SystemDokument5 SeitenAnatomy and Physiology of Intrinsic Cardiac Autonomic Nervous SystemSori B. Requena C.Noch keine Bewertungen
- Pearson Science New South Wales 9 Chapter 6 TestDokument13 SeitenPearson Science New South Wales 9 Chapter 6 TestAbigail ScottNoch keine Bewertungen
- Peripheral Nervous SystemDokument1 SeitePeripheral Nervous SystemChris_Barber09Noch keine Bewertungen
- GC ANS Part II 2016 Phy2011Dokument25 SeitenGC ANS Part II 2016 Phy2011Lisa KangNoch keine Bewertungen
- Anesthesia QuizDokument4 SeitenAnesthesia QuizMarites L. DomingoNoch keine Bewertungen
- SCIENCEDokument6 SeitenSCIENCEFerlyn SolimaNoch keine Bewertungen
- Autonomic Nervous System: DR S S Ranasinghe CNTH - RagamaDokument63 SeitenAutonomic Nervous System: DR S S Ranasinghe CNTH - RagamawellawalalasithNoch keine Bewertungen
- Nervous System - QuizDokument65 SeitenNervous System - QuizrmmmsNoch keine Bewertungen
- Beyond Telepathy Andrija PuharichDokument292 SeitenBeyond Telepathy Andrija PuharichWild CardNoch keine Bewertungen
- Book Review - Electrodermal Responses What Happens in The BrainDokument12 SeitenBook Review - Electrodermal Responses What Happens in The BrainamishcarNoch keine Bewertungen
- Physiology 12th Lecture - Control of Heart ActivityDokument1 SeitePhysiology 12th Lecture - Control of Heart ActivityarikfischerNoch keine Bewertungen
- Biological Psychology NotesDokument16 SeitenBiological Psychology Notesaleeshawasfy43Noch keine Bewertungen
- Manan 1000 Q - ADokument294 SeitenManan 1000 Q - ADrSamia El Wakil0% (1)
- Physiology MCQ - CNSDokument5 SeitenPhysiology MCQ - CNSKamaluddin KhanNoch keine Bewertungen
- Lie Detwction (Polygraphy)Dokument33 SeitenLie Detwction (Polygraphy)jimwellsiego74% (27)
- 60 Samples Questions and Answers For MRCOphth IDokument26 Seiten60 Samples Questions and Answers For MRCOphth Imacheso0% (1)
- Arterial HyperemyDokument10 SeitenArterial HyperemyRohit NaiduNoch keine Bewertungen
- NorepinephrineDokument9 SeitenNorepinephrineDimitris KaragkiozidisNoch keine Bewertungen
- Pharmacology Questions With AnswersDokument84 SeitenPharmacology Questions With AnswersAquiles Vaesto100% (9)
- Chapter 10 The Nervous SystemDokument9 SeitenChapter 10 The Nervous SystemDXN LUDHIANANoch keine Bewertungen
- Dr. ChintanDokument24 SeitenDr. ChintanamrendraNoch keine Bewertungen
- Nervous Systemchapt 28Dokument58 SeitenNervous Systemchapt 28Emerito PerezNoch keine Bewertungen
- Gastrointestinal and Abdominal Problems 3.LfDokument68 SeitenGastrointestinal and Abdominal Problems 3.LfapocruNoch keine Bewertungen
- Altered Cognitive-Perceptual Patterns: Clients With Neuroligic DisordersDokument96 SeitenAltered Cognitive-Perceptual Patterns: Clients With Neuroligic DisordersJobelle AcenaNoch keine Bewertungen
- Post-Exercise Recovery: Effects of Whole-Body Cryostimulation ExposureDokument8 SeitenPost-Exercise Recovery: Effects of Whole-Body Cryostimulation ExposureCherbiti Mohammed AmineNoch keine Bewertungen
- Sci10 Q3 Module3Dokument24 SeitenSci10 Q3 Module3Jennifer Lomboy50% (2)
- Lecture On The Physiology of Hypothalamus and Thalamus by Dr. RoomiDokument27 SeitenLecture On The Physiology of Hypothalamus and Thalamus by Dr. RoomiMudassar Roomi100% (1)
- 13 Home TreatmentDokument300 Seiten13 Home TreatmentHatfulloftricks700Noch keine Bewertungen