Beruflich Dokumente
Kultur Dokumente
Acute Biologic Crisis
Hochgeladen von
Eniryz M. SalomonOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Acute Biologic Crisis
Hochgeladen von
Eniryz M. SalomonCopyright:
Verfügbare Formate
Acute Biologic Crisis: 07-21-11 Cardiovascular ICU= the nurse is assigned to a single patient for proper management CCU=
coronar care unit stabilize first the patient before wheeling to the ward 150-200 SBF malignant HPN ex. Sublingual isordil If patient was not managed in the ER, ex continuous/ maintained increase in BP, HR (a biologic crisis) Legalities and and liability of nurses, partient will be sent to ICU RD is now ERD (emergency room department) Coronary Artery Disease refers to a variety of pathologic conditions that cause narrowing or obstruction of the arteries resulting to decreased blood supply in the myocardium Coronary circulation Arteries (systemic manifestation) Right coronary artery a. 1. Posterior descending artery= supplies the right atrium, the anterior wall of the right ventricle, and the posterior wall of the left ventrivle a.2. 2 marginal artery= supplies the right ventricle and the right atrium including SA node and AV node B. Left coronary artery (respiratory manifestation) b. 1. anterior desending and diagonal artery= supplies anterior wall of left ventricle and ventricular septum,intralumina, muscularis, submucosa) atheroma= progression: Clinically silent: 30 y.o. p. 1414 In ruptured aneurysm, it becomes an acute biologic crisis. Prodromes: predeterminant factor; detector of ertain disease process Angina pectoris= pain in the pectoris muscle Neovascularisation= collateral circulation Anaerobic= lysozome ruptures due to lytic acid= goes out (concentric pattern) irritating the nerves causing pain Concentric pattern (closed fist); if spread, open fist Sealing of compensation= patiet may not ne manifesting angina anymore b.2. circumfles artery= supplies left atrium and left lateral and posterior walls Etiology: >results from the development of atherosclerotic lesions within the coronary arteries that narrow and obstruct the blood vessels > atherosclerosis= is a disorder in lipid metabolism characterized by a deposit of fat containing substances along the intima of blood vessels and proliferation of smooth muscle cells Risk factors: p.1411 non-modifiable: heredity
age male sex modifiable: Smoking HPN Increased serum cholesterol
>the disease of the new generation; the fast generation > stroke in the young >LDL= 4.5-9 L women 5.5-6 L men >Y chromosomes= has less capacity to take away atheromatous plaque >CY- cystic fibrosis >anything that has unequal ratio will undergo hypercoagulability >11. 5 min of constriction to the blood vasculature= nicotine > periphery of RBC is collagenous so it attaches to other RBCs (agglutinate) Contributory factors: stress response obesity (acquired, chromosomal, congeniotal) physical inactivity diabetes (11 yrs) Medical management: dietary modification cessation of smoking controlling diabetes and hypertension administration of anticholesterol drugs Surgical management: PTCA ( percutaneous coronary transluminal angioplasty) p. 1419 Nursing management: instruct to minimize intake of fats and cholesterol to increase exercise and keep body weight at ideal levels ( to control diabetes and hypertension) Congestive heart failure p.1430 Kubler rauss the heart fails when: there is intrinsic disease or structural defects it cant handle a normal blood volume it cant tolerate a sudden increase in blood volume during exercise cause of the heart failure: abnormal loading conditions abnormal muscle function conditions that precipitate or exacerbate heart failure physical/ emotional stress dysrrythmia infection
anemia thyroid disorder pregnancy pagets disease nutritional deficiency pulmonary disease Hyperlipidemia Mechanical property of the heart CO(4-8L/m) cardial index 2.5-4L/min/m2) Cyanosis by periphery= fingers Central cyanosis= tongue Stroke volume Determinants: preload= frank starting low end of diastole/ filling in of blood afterload= during systole and eject blood (contraction) contractile state (inotropic) See Kozier and Erb Clinical Manifestation: If hyporeflexia , patient is having hypokalemia (fluid congestion) If CHF, IV is given. Infectious co morbidity hallmark. LV Failure dyspnea cheynestokes respiration orthopnea cough paroxysmal nocturnal dyspnea pulmonary edema CV signs Cerebral hypoxia Renal changes Fatigue and muscular weakness peripheral edema dependent edema (early sign) anxiety, frightened, depressed anoxic venous congestion of organs involved anorexia, bloating secondary to congestion of GIT congested liver lobules (anoxic) to confirm: liver profile
Cardiac transplant on or mechanical heart may be employed
Nursing Interventions: Monitor the respiratory status. >02 >semi/ high-fowler position >monitor ABG >assess breath sounds 2. 3. Increase cardiac output. Vasodilator p.1438 Diuretic: to increase CO p. 1439 Digitalis: to increase cardiac contractility DIGITALIS Preterm 15-25mcg Full-term 20-30 mcg 1-24 mon 30-fo mcg 2-5 y.o. 25-35 mcg 5-10 y.o. 15-30 mcg 10 years and above 8-12mcg Digitalis enters cells, stop Na, K, ATP -0 phase contraction: Na enters -phase 1: K goes out -phase 2 Ca enters (has the ability to stimulate Ca cytosome), K goes out Digitalis sends impulse to send precalcuim (to stop Na, K, ATPase activity) Increases cardiac contractility, stimulate free Ca to enter cell to the Ca cytosome (stimulate cytosol to release Ca in the cell) and stop NaK ATPase action. Ca send impulse to actin and myosin to contract VASODILATORS
RV Failure
acts on preloaod and afterload ACE (captopril. inalapril,etc.) A1 converts A2 in lungs to stimulate kidney to release ADN so that Na will be absorbed back (read kidney etc) so that fluid volume will return the circulatory system (increased BP) Stimulate at Z globulin in the blood (angiotensinogen enzyme stimulate A1 to stimulate A2 to stimulate ADN) ACE inhibitor stop A1 conversion to A2 (lungs, liver, kidneys)
Medical Management: Determine underlying conditions. Drug treatment, digitalis preparation, diuretics, vasodilators Na-restricted diet to decrease fluid retention
3 Mechanisms of Action 1. Decrease SNS (adrenergic response) = decreased tachycardia, regulate arrhythmic contraction. = decreased preload/ afterload increased vasodilation in the smooth muscle
=nitrate: searches blood vasculature, degraded into an oxideso it can enter blood vessel musculator and relaxes blood vasculature to dilate. decreased aldosterone: increased bradykinin (vasodilator) decreased retention of h20 and Na from release of AND July 22, 2011 ECG p. 1451 Holter monitoring Electrocardiograph (Encarta) Exercise ECG (stress test) Atrium: passive gradient Q-wave= ventricular filling closing R-wave= contracyion, opens aortic valve maximum peak of opening/ contraction S-wave= goes to systematic circulation; epties the blood vessel Loading= filling of blood again P-R interval= AV conduction time;time it takes an impulse to travel from the atria down through the AV node; measured from beginning of P wave to beginning of QRS complex = heart abnormality; the lesser the blood, the lesser SAAV electric gradient QRS complex (0.06-0.10 sec) = indicates ventricular depolarization = measured from onset of Q-wave to end os S-wave. ST segment = indicates time interval between complete depolarization and repolarization of ventricles T wave: represents ventricular repolarization; follows ST segment SA node (Keith-flack node) -pacemaker -in a cavity/ sinus in the right epicardium - 60-100 bpm 2. Internodal tracts - carry impulses from SA to AV node As impulse pass along this tract, the right atrium contracts 3. AV node (node of tawara) - it delays the impulses from the SA node and atria for a fraction of a second a. heart rate -60-100bpm
-variations: size of individual, exercise, age gender, temperature, hormones BP, anxiety, stress, pain b. atrial pressure - pressure of blood against arterial wall Types: Systolic pressure: maximum pressure of blood exerted against the artery walls when heart contracts (100-140 mmHg) QRS complex. Afterload. Diastolic pressure: preload, ST segment (60-90 mmHg) Bidirectional Contraction: bundle of his sends impulse to the purkinje fibers to contract at the same time. Criteria for normal sinus rhythm rhythm: regular rate: 60-100 bpm atrial conduction: one p wave before each QRS, normal shape, consistent in shape AV conduction: PR interval; 0.12-0.20 seconds, same across; the strip may vary with rate Ventricular conduction: QRS 0.06- 0.10 seconds, uniform in shape Read how to rate in the book. Dysrrythmias Chart 29-1 Identification of Dysrrythmias according to origin Bradycardia p. 1454 Cardioversion p. 1458 Defibrillation p. 1470 Patient with pacemaker p. 1473 Classes of Meds Class 1 ABC Na channel blockers 1a= to slow 0 phase of repolarization 1b= to slow phase 3 of repolarization 1c= markedly slow 0 phase of depolarization Class 2 beta-adenoreceptor= suppresses phase 4 depolarization; -olol,propanolol,etc Class 3 K- channel blockers= prolongs phase 3 repolarization; bretilium, sotalol, amniodarun Class 4 Ca-channel blockers= shortens action potential; verapamil, diltiazem Complications Cardiogenic Shock power failure end-stage marked reduction of cardiac output no more CO proportional to level of ventricular dysfunction
Conduction System
decreased BP, rapid weak pulse, cerebral hypoxia (confusion,agitation) cold clammy skin, sudden increase in UO treatment: major dysrrythmias are corrected >catecholamines (epinephrine, endorphins) increased BP, increased CO >vasodilator (nitroglycerin,nitroprusside) increase cardiac output
Nursing Implication: careful pt assessment measure fluid intake and urinary output dysrrythmia monitoring hemodynamic status observation of pts Thromboembolic episodes intracardiac and intravascular thrombosis manifestation: sestemic embolism may occur in left ventricle; identify and report for signs and symptoms. Pericardial Effusion -escape of fluid into pericardial ac resulting in rapid effuin resulting on cardiac tamponade - causes: infectious process >TB has the ability to cavitate >Military= exists pulmonary sac >Secondary type= if with cavitation/ scar formation is at the upper side then goes to the lower part (caceous necrosis) >ibtracranial aspiration= feeling of precordial compression, SOB, drop and fluctuation in BP, lowest BP during inspiration >Pulsus paradoxus > falling arterial BP, narrowing pulse pressure Management: pericardial centisis/ aspiration; 45-60 head elevated; assist in positioning the patient Myocardial Rupture Cardiac Arrest CPR= to secure an airway; to provide ventilation and external cardiac compression Management: oxygenation infectious process weakening of cardiac muscle death is due to cardiac tamponade myocardial rupture management: pericardiocentesis (emergency measure); repair of cardiac muscle via open thoracic surgery
lidocaine: to suppress ventricular dysrrythmia give procainamide Hcl (if lidocaine is ineffective) give atropine to accelerate cardiac rate by creating (+) inotropic/ chronotropic effect (same regular synchronous contraction) parasympathetic action: reversal of vagus action decreased vagus tone due to decreased cardiac rate if cardiac rate is decreased, (+) intoropic effect will occur so atropine and procainamide can act create a (+) chronotropic effect (accelerates AV contraction) 5. Epinephrine - increased perfusion pressure during cardiac
compression - improve myocardial contractility state - stimulate spontaneous contraction - increase vigor of the contraction 6. Na bicarbonate - to correct metabolic and respiratory acidosis (abnormality in blood circulation produces acidity) - CO2 produces acidosis - Na enters cell so acidotic cell to excrete toxic products ( CA, K excess) so consequently Ca goes out -As Na enters, carbonate also enters to balance fluid - chloride becomes a buffer -Fastest route of acidosis ( expiration) - if electrolyte enters, buffer also enters If fluid, use chloride
July 29, 2011 Management of Cardiac Patients in Surgical Approach History: NOTE: According to sir Nic, 1895 was the 1st successful cardiac surgery. September 4,1895 >>>First surgery on the heart itself done by Axel Cappelen. >>>He ligated a bleeding coronary artery in a 24 year old man who had been stabbed in the left axillae and was in deep shock upon arrival. >>>Patient died from mediastinitis. September 17,1896 >>>First successful surgery to the heart performed by Dr. Ludwig Rehn. >>>Repaired a stab wound to the right ventricle. 1923-1925- valvular syrgery 1937-1938: Closure of PDA was done. December 3, 1967
>>>53-year-old Lewis Washkansky received the first human heart transplant at Groote Schuur Hospital in Cape Town, South Africa. >>>he died 18 days after due to the immunosuppressive medications given to him leading to the development of double pneumonia. Mid-1970s >>>Jean Borel discovered cyclosporine >>> Cyclosporine is an immunosuppressive drug derived from soil fungus. 1980s >>>also known as AGE of SCIENTISTS >>>new medications were developed, e.g. the new amoxicillin >>>Cystic Fibrosis was given more attention by the scientists of their era. 1989- 250,000 procedures in cardiopulmonary by-pass Pero-op Management: patient and family experience major life crisis. Provide support. Pre-op Management: Identify and inform significant other regarding the patients condition. Assess the patients knowledge regarding the surgery. Impart knowledge as needed. Perform physical and psychological assessment. Secure informed consent for the operation, blood transfusion, etc. Cardiopulmonary by-pass >>> extracorporeal circulation; provides mechanical means of circulation and respiration while by-passing the heart and lungs >>>mechanically circulates and oxygenates blood for the body while bypassing the heart and lungs. >>>It uses a heartlung machine to maintain perfusion to other body organs and tissues while the surgeon works in a bloodless surgical field. >>> The blood is cooled at about 28-30C (because warm blood causes an increase in metabolism which would lead to an increase in metabolic epinephrine hormone thus causing heart to contract faster). >>>this is a common technique used during heart surgery. patient is attached to artificial oxygenator machine main tube is attached to vena cava and right atrium D5LR is used to suspend the blood: lactate has bicarbonate which attaches to the carbon dioxide in the body; prevents clumping of blood (venous reservoir) Lactate: anything that has acid/ capable of producing acid. Anticoagulants are given to prevent clumping with the foreign body structure Filter: separates blood from other substances Enters oxygenator. Vagal response= either hypervagal or hypovagal response Heat exchanger: to warm up blood. -hyperthermia: response of inflammatory cells occur. TELEMETRY= patient is placed here 24-72 hours post-op. Indications of cardiac surgery:
Circulatory Disorder Valvular Disorder Conductive Disorder: defibrillator no longer works. Medications no longer work.
Surgical Laboratory -circulatory cardiac surgery -valvualr cardiac surgery -conductive cardiac surgery *70% damage to the heart TAKE IT OUT! (Remove the coronary artery) Percutaneous Transluminal Coronary Angioplasty Indications: severe atherosclerosis; stenotic vessels Contraindication: presence of stenotic structure at the end-point (pre-post stenotic) stenotic: due to bacteria; the area will be scarred and forms stenosis Angiography during the procedure. Complications of PTCA: Dissection of artery: causes cascade of thinning to the rest of the linings. Ruptured aneurysm. Abrupt closure. Spasm of coronary artery.
>>>Prognosis: patient may live for 6-10 years or 3-7 years; or pt may develop[ other disease process >>>not a surgical procedure >>> Less invasive procedure; balloon is inflated to a sclerotic vessel. >>>if myocardium is occluded by 70%, PTCA is performed (distal portion will have ischemia) >>>patient will be having increased respirations since there is a decrease in oxygenation to the ventricle A patient who has undergone cardiac surgery usually receives an anticoagulant therapy, e. g. heparin. >>> 10th day of anticoagulant therapy,pt is at risk for spontaneous bleeding >>>bruises and gum bleeding may appear >>>monitor pts RBC,PT,PTT Protamine sulfate is also given to counteract the effects of heparin. 3 alternatives 1. Redilation 2. Redilation with intravascular stent. 3.Redilation of the lumen. Redilation with intravascular stent over the balloon.
Shunt= placed inside the vessel to provide blood to the ischemic area; has catheter with holes.
Inserting a laser= still for study/research; heat emitted from laser produces a weld and opening the obstructed structure; melting process Place patient in anticoagulant therapy
Opaque=fluid filled >>>patient is admitted to critical unit >>>Placed in an incision to the aortic aneurysm (clumped in the proximal area) >>>a prosthesis is inserted (Dacron type stainless) >>>annular ring (above the valve) >>>artificial valve replacement >>>structural cardiac surgery Valvuloplasty >>>commissures (in between leaflets) >>>due to scars/ stenosis (group b haemolytic group streptococcus from RHD) >>>since foreign body (bacteria) are there, immune cascade occurs. *Comissurotomy -close: do not require cardiopulmonary by-pass; closed adherence of leaflets bring commissure are stenosed. : valve is not directly visualized -open: performed with direct visulaization of valve, withCPB, median sterntomy Stricture: apposition of vessels Hand of surgeon/ dilation/ scalpel or balloon is used to open the valve Balloon Valvuloplasty >>>mitral and aortic valve stenosis >>>tricuspid and pulmoni valve stenosis >>>double single catheter >>>intaatrial septal dilatation will be done (from femoral/brachial vein to right atrium to left atrium to left ventricle to aorta) >>>usually have guide wires >>>if already placed, guidewire is removed >>>Balloon is deflated with dilute liquid angiographic solution >>>2 balloons may be used Annuloplasty >>>Annulus (junction of valve leaflets with the junction of the heart valve wall) attachment of leaflet to the heart muscle >>>insertion of an annular plasty ring >>>general anesthesia,CPB >>>narrows diameter of valve orifice >>>for patients with regurgitation (if elderly,degenerative,if 30-40 y.o., is due to RHD or bacteria) >>>memorize percentage of organismic characteristic >place annuloplasty rings, leaflets of the valve are sewn to the ring to create the desired annular size >>>also called tucking >>>any mechanical manipulation in the GIT adhesions Leaflet Repair >>>damaged by stretching of the shape >>>may be shortened/ develop holes
If given in prolonged time, bleeding may occur at 7th to 10th day Monitor stool in blood, bruises and gum bleeding Computation of coagulant depends on body weight Protamine sulphate combats anticoagulant (heparin) Identify that the patient should not have substances that stimulate more bleeding if taking anticoagulant Protamine + Vitamin K (biosynthesis) > intestine processes vitamin K and becomes a coagulative process (because as protamine decreases its action, Vitamin K takes days before its peak and will increase as protamine decreases)
Coronary Artery By-pass Grafting Indications: Chronic angina (uncontrolled with therapy) Unstable angina (even at rest, there is chest pain) (+) tolerance exercise test: at stage 1,pt already has tracing of ST segment Left main coronary artery lesion of more than 60%: peripheral cyanosis. (branches to marginal coronary artery and branches to the left ventricle and the aorta; also check for nevascularizations) Complications from unsuccessful PTCA. Other info about CABG >>>performed under general anesthesia >>>median sternotomy opening: type of surgical procedure in which a vertical inline incision is made along the sternum, after which the sternum itself is divided, or "cracked" >>>arteries and veins that were used for grafting during an anstomosis: -great saphenous vein: may lead to atherosclerosis 3-5 years after the anastomosis was done. -internal mammary artery: since it is near the pectoralis muscle, it might result to conmtracture since the nerve may be pulled; may lead to atherosclerosis 6-10 years after the anastomosis was done:at the 10th year, plaquing usually occurs. - gastroepiploic artery: its from the lesser curvature of the stomach but because of its physiologic process of giving off blood,leser blood is given to the heart; may lead to hypertrophy and other complications.
Ascending Aortic Aneurysm >>> requires cardiopulmonary by-pass >>>dissecting aneurysm due to presence of blood, so structure is thinned (either above/ below the muscularis)
Leaflet placation: falling over itself Chordoplasty >>>repair of the chordae tendinae >>>tacking technique, suturing, implication, placate, etc. Valve replacement >>>prosthetic valve(1960s) >>>started in PGH Causes: calcification >>>general anesthesia,CPB >>>post-mitral valve, chordae tendinae and papillary muscle must be left in place to maintain ventricle shape Xenograph = biosynthetic; from another organism caged ball valve tilting disk valve porcine valve = steroid is given ABO compatibility is taken = no battery needed = due to muscle contraction
>>>monitor neurologic status >>>Monitor cardiac status CVP,PCWP, pulmonary artery >>>monitor respiratory status (chest movement, lung sounds) >>>peripheral vascular status assessment >>>renal function, UO >>>F&E status >hypokalemia(digitalis toxicity; dysrythmia, U wave, inverted T wave) >hyperkamlemia (confirm via extracting blood), note for mental confusion, restlessness, muscle weakness, paresthesias,dysrythmia, tall peaked T waves increasing in amplitude, prolonged QT interval) >hyponatremia (weakness, fatigue,confusion due to urea and creatinine accumulation, convulsion*motor nuclei,muscular motor fiber*,coma*brainstem*, respiratory arrest >hypocalcemia(tetany, paresthesia, carpal pedal spasm, muscle cramps,asystolic,digitalis toxicity,pain) August 4, 2011 Continuation of Acute Biologic crisis N= 78.62% O2= 20.87% CO2= 0.04% Traces of helium, argon Watervapor= 0.05% Atm pressure= 760 mmHg (sea level) Partial pressure of N= 79% of 760 (0.79x760)= 600 mmHg O2= 21% of 760 (0.21x760)= 160 mmHg P= pressure Types of alveolar cells pneumocyte type 1 pneumocyte type 2= surfactant pneumocyte type 3= macrophages *surfactant= stimulated during last trimester *O2 pro,otes alveolar dilation SIDS in adult due to decreased surfactant (???,as in.ha adult?!ok,so wa ak sumulod,meada hai an sids ha lagas?OMG!) SIDS in infant is idiopathic. SIDS causes: absence of surfactant (preterm) Term infant (delayed surfactant development) V/Q= ventilation- perfusion quotient 1:1 ratio Ventilation= O2 enters the lung Q= O2 enters blood vasculature; circulation in the alveolar capillary/ arterioles Terminal bronchus-> alveoli Alveolar-capillary= single epithelial cell for easy passage Factors: pressure
2 Types of Heart Transplantation 1. Orthotopic >>> portion of the atria, vena cava and aorta are left in place >>>pulmonary artery and aorta are anastomosed >>>nerves are not sutured so this heart will not have an autonomic response >>>it takes 10-20 min before the catecholamines would take effect on the heart during stimulation, e.g. delayed fight-or-flight response 2. Heterotopic >>>donor heart is placed slightly anterior to the recipients heart >>>donor heart is placed to the right of the right, original heart is still in place >>>the original heart may provide protection to the individual >>>70-90bpm=transplanted heart, it contracts due to electric gradients and blood filling. Nursing Consideration: when a donor heart is already available, a computer generates a list of possible recipient heart must be transplanted within 4 hours or else it dies ABO compatibility, sizes, weight and distance between the donor and recipient is given consideration when matching heart donations Hearts function depends on the time it was implanted. Mechanical Assistive Device >>>external control heart (read in the book) >>>cardiac assistive devices (total artificial heart) Post-op Cardiac Team
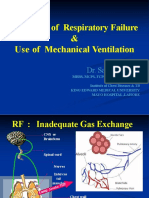
V/Q imbalance can lead to acute biologic crisis Decreased ventilation/ absent with perfusion= alveoli collapse and atelectasis, pneumonia, foreign body (2:2) Ventilation with absent perfusion= (2:2) pneumonic Absence of V/Q= ARDS Neuromuscular= myasthenia gravis; Guillian barr syndrome, ascending paralysis the other one is descending paralysis
Assist/ control ( patient triggers the machine; if patient fails to breath, machine controls breathing)- 2mmHg Intermittent mandatory ventilation (machine allow patient to breath spontaneously while providingO2 and # of ventilator breaths to ensure adequate ventilation without fatigue respiratory machine is not attached if no ABG result record minute volume of PCO2; after 20 min of continuous mechanical ventilation in other countries, nurse practitionerajust ventilation without doctors order if bucking the ventilator O2 100% Indications: -Pa O2 < 15 mmHg with FiO2 >0.60 -PaO2 > 50 mmHg with pH < 7.25 -vital capacity <2 x the tidal volume -(-) inspiratory volume is < 25 cm H2O (external thoracic pressure) -RR > 35/min Classification of ventilator (-) pressure ventilator (exert a pressure on external chest) ~ decreased intrathoracic pressure, chronic respiratory failure secondary to neuromuscular condition (polio, muscular dystrophy/ organic in nature; myotropic lateral sclerosis (encapsulation of a nerve of a sclerosis, fibrous cell), myasthenia gravis (+) pressure ventilator Iron lang? = (-) pressure, used during polio epidemics Body wap= rigid cage/ shell to create a (-) pressure (+) pressure ventilator inflates lung by exerting (+) pressure on the airway ET intubation and tracheostomy is required *read and memorize tracheo care 3 types of (+) pressure ventilators >Pressure cycle ventilator - deliver gases at a preset pressure, then allow passive expiration. - volume of air can vary to patient airway resistance/ compliance changes Adults= short-term use >Time cycled ventilator - control ventilation after a preset time, regulated by the length on inspiration - most ventilation has rate control to determine RR - used in NB and infants >Volume cycled ventilator -most commonly used - volume of air to be delivered with each inspiration is preset Nursing care for mechanically ventilated patient monitor VS, hypoxia evidences ( cyanosis is the last manifestation of hypoxia), restlessness (primary manifestation), anxiety, tachycardia, increased RR, cyanosis
Lung volumes and lung capacities (memorize, check book) tidal volume= inhaled and exhaled inspiratory reserve volume= inhaled maximum expiratory RV= exhaled residual volume= remaining Lung capacities VC IC FRC TLC= 4 volume sum Pulmonary function test FVC FEVt, FEV1 FEVt/ FVC%, FEV/ FVC% FEF200-1200 FEF25%-75% FEF75%-88% MVV Diff. types of O2 delivery system Cannula device= 1-2L/min Nasal catheter Simple mask= 6-8 L/min Partial rebreather mask= 8-11 L/min Non-rebreather mask= 12L/min Ventura mask= 4-6 L/min. highest % Inhaled mixture of 100% O2 Important Device: Mechanical ventilator is used specially in ARDS/ respiratory arrest, may it be structural, alveolar gaseous Table 25.4 Nursing consideration: adjustment of ventilator, disinfect Team nursing: post-op team {at CCU the physicaian/ pulmonologist computes L/min} Biomedical engineer (usually calibrates the machine; checks the functionality of the machine) LPN= practical nurses/ Nursing assistant TV required= 10-15ml/kg= 12-16/min RR Lowest partial O2= 80-100mmHg Controlled (machine completely controls patient ventilation)
Problems of ventilator
monitor for RR and pattern assess breath sounds monitor neurologic status ( end products toxicity, if frontal lobe (behavioural), brainstem (unconsciousness), medulla (seizure attack), pons and medulla( respiratory center), lower pons (deep inspiration and apneustic area) above pons (pneumatic center , synchromy of respiration 1:3 ratio) tidal volume, minute ventilation, FVC nutritional status (TPN) sunctioning needs (since no cough/ gag reflex) psychological status spontaneous ventilatory effort equipment assessment (type of ventilator, controlling mode, tidal volume of rate settings, FiO2 settinginspiratory pressure reached and limit sigh setting (unit of measurement) 1.5 x tidal volume, i-3 x per hour assess presence of H2O in the tubing (pour it out) know disconnections/ kninking of tubings assess humidification/ see humidifier filled with water to prevent drying and provide smooth passage assess functioning alarms note (+) and expiratory pressure (eak) impaired verbal communication, ineffective coping, powerlessness increased in peak airway pressure causes: coughing= lavage and suction airway pt bucking ventilator= manually bag ventilate tubing kinking pnuemothorax= manually ventilate, notify physician to remove air decreased in pressure volume increase in compliance: leak in ventilator/ tubing, cough, not tight humidifier/ tube
CNS depression drug overdose, anxiety/ panic attack anesthesia head injury stroke brain tumor, encephalitis, meningitis hypoxia, hypercapnia narcolepsy= REM trauma= motor vehicle accident alcohol= inhibitor of inhibitants
pleural effusion (hemothorax, pneumothorax) chemical pneumonitis= inhalation of irritant fumes. Aspiration of acidic gases bronchial asthma Factors of ARDS *aspiration from gastric secretions - drowning, hydrocarbons, drug ingestion, overdose *hematologic disorder -DIC, massive transfusion *prolonged inhalation of high O2 concentration; hyperbaric? *smoke, corrosive substances (more on acidic) *localized infection -metabolic disorder; shock,trauma, major surgery, fat. Air embolism, 5-10 ml of air embolism *systemic sepsis Read patho of ARDS Diagnosis: acute respiratory failure bilateral pulmonary infiltrates hypoxemia 50-60 mmHg FiO2 0.5-0.6 PAWP= >18mm Hg Management: define and treat cause provide adequate ventilation provide circulatory support provide adequate fluid / nutritional support early diagnosis and treatment systemic hypotension is not uncommon; toxins increases permeability in the blood vasculature, thins out, opens and blood goes out intravenous crystalloid inotropic swan- ganz, CVP
Book Respi Ox
Patient
Problems CV compromise: decreased venous retur barotraumas: apply (+) pressure pulmonary function: bypass of normal defense mechanism; aseptic technique cause: frequent breaks in generator circuit, decreased mobility, impaired cough reflex increased respiratory failure: hypoxemia, hypercapnia causes: CR failure chronic bronchitis, emphysema, failure resulting from inadequate ventilation, upper airway obstruction, ARDS
corticosteroids (controversial) immunosuppressormay decrease pulmonary function and development of superinfection ARDS 35-45 kacal/ kg a day Nutritional supplements: note kcal, increased metabolism, increased CO, decreased metabolic state
Nursing intervention: Close monitoring (quick change of health status) If not attached to a mechanical ventilator, position pt to high fowler (maximum excursion of thorax) Mobility Explain procedure, deliver care in a calm, patient manner Rest If attached to a mecha vent, go back to assessment of mech vent machine
Das könnte Ihnen auch gefallen
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideVon EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNoch keine Bewertungen
- CBQmedsurgDokument17 SeitenCBQmedsurgshenric16Noch keine Bewertungen
- C C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMDokument4 SeitenC C C M MMMM MM M MMM 3mm MMMMM MM M MMMMMjohkieNoch keine Bewertungen
- Universally Accepted AbbreviationsDokument4 SeitenUniversally Accepted AbbreviationsPamela Dela Cerna BrionesNoch keine Bewertungen
- First Semester 2020-2021 Study Guide: University of The CordillerasDokument13 SeitenFirst Semester 2020-2021 Study Guide: University of The CordillerasJonalyn EtongNoch keine Bewertungen
- MSN 0419 4thpart AppendicitisPeritonitisDokument3 SeitenMSN 0419 4thpart AppendicitisPeritonitisAnna Sofia ReyesNoch keine Bewertungen
- Fluid and Electrolytes, Burns, G.UDokument56 SeitenFluid and Electrolytes, Burns, G.Uapi-3735995100% (4)
- MedSurg 2Dokument69 SeitenMedSurg 2Claire Maurice JuaneroNoch keine Bewertungen
- Learner'S Worksheet: Clinical RotationDokument3 SeitenLearner'S Worksheet: Clinical RotationLecery Sophia WongNoch keine Bewertungen
- Medicine Ward NCPDokument11 SeitenMedicine Ward NCPKimsha ConcepcionNoch keine Bewertungen
- Zollinger EllisonDokument2 SeitenZollinger EllisonFrama Intan MiguelNoch keine Bewertungen
- Nur 1210 Pedia Concept Module 4B Alterations With Infectious, Inflammatory and Immunologic ResponseDokument19 SeitenNur 1210 Pedia Concept Module 4B Alterations With Infectious, Inflammatory and Immunologic ResponseweissNoch keine Bewertungen
- NCM106 AcuteBiologicCrisisDokument156 SeitenNCM106 AcuteBiologicCrisisrimeoznek100% (2)
- Assessment of Immune FunctionDokument3 SeitenAssessment of Immune Functionhalloween candyNoch keine Bewertungen
- Fluid and Electrolyte NotesDokument6 SeitenFluid and Electrolyte NotesAshley H Locklear100% (1)
- Management of Patients With Intestinal and Rectal DisordersDokument54 SeitenManagement of Patients With Intestinal and Rectal DisordersJills JohnyNoch keine Bewertungen
- Exam Progam May 2024 PnleDokument3 SeitenExam Progam May 2024 Pnlejimenezchristian1003Noch keine Bewertungen
- MM M M MDokument20 SeitenMM M M MAshok KumarNoch keine Bewertungen
- Pediatric Nursing Edison O Dangkeo RNDokument59 SeitenPediatric Nursing Edison O Dangkeo RNshenric16100% (1)
- PNLE IV For Care of Clients With Physiologic and Psychosocial Alterations (Part 2)Dokument23 SeitenPNLE IV For Care of Clients With Physiologic and Psychosocial Alterations (Part 2)ASDF ASDFNoch keine Bewertungen
- Acute Kidney Injury (AKI) :: FeaturesDokument3 SeitenAcute Kidney Injury (AKI) :: FeaturesDavid PerezNoch keine Bewertungen
- Oncology Nursing Part 1 2Dokument51 SeitenOncology Nursing Part 1 2fleur harrisonNoch keine Bewertungen
- Group 5 - Hemodialysis - Chronic Kidney FailureDokument31 SeitenGroup 5 - Hemodialysis - Chronic Kidney FailureKimberly Abella CabreraNoch keine Bewertungen
- AtireviewDokument163 SeitenAtireviewGlory Mimi0% (1)
- 118 Skills Lab-Week 1-Responses To Altered Ventilatory FunctionsDokument8 Seiten118 Skills Lab-Week 1-Responses To Altered Ventilatory FunctionsKeisha BartolataNoch keine Bewertungen
- NCM 112 Fluids & Electrolytes Quiz AssignmentDokument4 SeitenNCM 112 Fluids & Electrolytes Quiz AssignmentJoyce Kathreen Ebio LopezNoch keine Bewertungen
- Renal Fabs NotesDokument9 SeitenRenal Fabs NotesLucky GomezNoch keine Bewertungen
- Grand Coaching: Medical Surgical NursingDokument22 SeitenGrand Coaching: Medical Surgical NursingEsarpy (Nana)Noch keine Bewertungen
- Musculoskeletal BulletsDokument9 SeitenMusculoskeletal Bulletswinner gift flowersNoch keine Bewertungen
- F&E ExamDokument3 SeitenF&E ExamDino PringNoch keine Bewertungen
- Assessment and Management of Patients With Biliary DisordersDokument16 SeitenAssessment and Management of Patients With Biliary DisordersJills JohnyNoch keine Bewertungen
- NCM 118Dokument8 SeitenNCM 118Zanie CruzNoch keine Bewertungen
- Biologic Crisis: Prepared By: Ronnie M. Amazona, RN, ManDokument162 SeitenBiologic Crisis: Prepared By: Ronnie M. Amazona, RN, ManLex CatNoch keine Bewertungen
- Cardio QuizDokument100 SeitenCardio QuizEvidence ChaibvaNoch keine Bewertungen
- Volume ImpairmentDokument32 SeitenVolume ImpairmentAcohCChaoNoch keine Bewertungen
- Primary Health Care: Prepared By: Ezra Angeli C. Joaquin, RNDokument18 SeitenPrimary Health Care: Prepared By: Ezra Angeli C. Joaquin, RNRaRe TV0% (1)
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDokument5 SeitenTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellNoch keine Bewertungen
- Therapeutic: Communication Technique Examples RationaleDokument2 SeitenTherapeutic: Communication Technique Examples RationaleArian May MarcosNoch keine Bewertungen
- Endocrine GlandDokument10 SeitenEndocrine GlandRS100% (1)
- Board Questions 2009Dokument16 SeitenBoard Questions 2009Erick EspinoNoch keine Bewertungen
- Hepatobiliary DisordersDokument2 SeitenHepatobiliary DisordersFreeNursingNotes0% (1)
- Pathognomonic Signs of Communicable Diseases: JJ8009 Health & NutritionDokument2 SeitenPathognomonic Signs of Communicable Diseases: JJ8009 Health & NutritionMauliza Resky NisaNoch keine Bewertungen
- Chapter 17 End-Of-Life CareDokument29 SeitenChapter 17 End-Of-Life CarePearl DiBerardinoNoch keine Bewertungen
- Nursing Management Pancreatic CancerDokument2 SeitenNursing Management Pancreatic CancerKit NameKo100% (2)
- NCM 107 SwotDokument7 SeitenNCM 107 SwotpauchanmnlNoch keine Bewertungen
- Management of Patients With Gastric and Duodenal DisordersDokument47 SeitenManagement of Patients With Gastric and Duodenal DisordersJor GarciaNoch keine Bewertungen
- Chapter27-Assessment and Management of Patients With HypertensionDokument31 SeitenChapter27-Assessment and Management of Patients With HypertensionAhmed 123Noch keine Bewertungen
- Chain of Survival: Adult and Pediatric Out of Hospital Cardiac ArrestDokument10 SeitenChain of Survival: Adult and Pediatric Out of Hospital Cardiac ArrestJapeth John M. FloresNoch keine Bewertungen
- CD HandoutsDokument27 SeitenCD HandoutsricogonzzzNoch keine Bewertungen
- PalmerDokument5 SeitenPalmerHershey LerionNoch keine Bewertungen
- Professional Adjustment: Mila Delia M. Llanes, PHD, RN Ust College of NursingDokument45 SeitenProfessional Adjustment: Mila Delia M. Llanes, PHD, RN Ust College of NursingNikkie SalazarNoch keine Bewertungen
- Acute Biologic CrisisDokument6 SeitenAcute Biologic CrisismikErlhNoch keine Bewertungen
- NCM 31112L Midterm Exams: RationalizationDokument202 SeitenNCM 31112L Midterm Exams: RationalizationWen SilverNoch keine Bewertungen
- Fluid and ElectrolytesDokument29 SeitenFluid and ElectrolytesLinh Tra100% (1)
- Chronic Renal FailureDokument29 SeitenChronic Renal Failuregeorgia.langNoch keine Bewertungen
- 119a - Concepts of Leadership and ManagementDokument15 Seiten119a - Concepts of Leadership and ManagementJoanna TaylanNoch keine Bewertungen
- ANEMIADokument48 SeitenANEMIAjomcy0% (2)
- Haad QuestionDokument20 SeitenHaad QuestionNimraj PatelNoch keine Bewertungen
- Final Copy of Invitation To BidDokument4 SeitenFinal Copy of Invitation To BidEniryz M. SalomonNoch keine Bewertungen
- Admin - Admin Cash - Cashier Deal With Payments Inpatient-Inpstaff Inpatient Department Outpatient-Outstaff Outpatient DepartmentDokument1 SeiteAdmin - Admin Cash - Cashier Deal With Payments Inpatient-Inpstaff Inpatient Department Outpatient-Outstaff Outpatient DepartmentEniryz M. SalomonNoch keine Bewertungen
- Invitation To BidDokument3 SeitenInvitation To BidEniryz M. SalomonNoch keine Bewertungen
- Tarui DiseaseDokument3 SeitenTarui DiseaseEniryz M. SalomonNoch keine Bewertungen
- Pemberton SignDokument2 SeitenPemberton SignEniryz M. SalomonNoch keine Bewertungen
- John Nash BiographyDokument2 SeitenJohn Nash BiographyEniryz M. SalomonNoch keine Bewertungen
- 2 Man CarryDokument3 Seiten2 Man CarryEniryz M. SalomonNoch keine Bewertungen
- Phil - HX Places (Cap, Redona, People CNTR, Madonna of Japan)Dokument2 SeitenPhil - HX Places (Cap, Redona, People CNTR, Madonna of Japan)Eniryz M. SalomonNoch keine Bewertungen
- Blood Gas AnalysisDokument5 SeitenBlood Gas AnalysisLucy BrittainNoch keine Bewertungen
- Acute Respiratory Distress SyndromeDokument7 SeitenAcute Respiratory Distress SyndromeDashhh RamirezNoch keine Bewertungen
- Care of The Critically Ill PatientDokument9 SeitenCare of The Critically Ill Patientdayana perdomoNoch keine Bewertungen
- Aeonmed VG70 User ManualDokument168 SeitenAeonmed VG70 User ManualApsb. BphNoch keine Bewertungen
- CombitubeDokument38 SeitenCombitubebrentupdegraffNoch keine Bewertungen
- Basics of Respiratory Mechanics and Artificial VentilationDokument248 SeitenBasics of Respiratory Mechanics and Artificial VentilationRogério Ferro Do NascimentoNoch keine Bewertungen
- Romer & Polkey 2008Dokument11 SeitenRomer & Polkey 2008Ισαάκ ΑλέξανδροςNoch keine Bewertungen
- VentilatorDokument90 SeitenVentilatorthenaloveNoch keine Bewertungen
- Basic Principles of Mechanical Ventilation Andventilator GraphicsDokument70 SeitenBasic Principles of Mechanical Ventilation Andventilator GraphicsSupriya PattnayakNoch keine Bewertungen
- EVM500041 Rev L, Manual, User, Evolution 3eDokument206 SeitenEVM500041 Rev L, Manual, User, Evolution 3ejangum wonogiriNoch keine Bewertungen
- Perfect Combination of Technology and Arts: Anesthesia MachineDokument4 SeitenPerfect Combination of Technology and Arts: Anesthesia MachineCarlos RebouçasNoch keine Bewertungen
- ArdsDokument69 SeitenArdsdrabdallakawareNoch keine Bewertungen
- Ads Ii: Anesthesia Delivery SystemDokument4 SeitenAds Ii: Anesthesia Delivery SystemWaleedNoch keine Bewertungen
- Airway Assessment MeDokument46 SeitenAirway Assessment MePeter AbikoyeNoch keine Bewertungen
- Ards and RF FileDokument12 SeitenArds and RF FileEdwin Delos Reyes Abu100% (1)
- Settings and Management Tip Sheet For Providers: Isp Elevated?Dokument1 SeiteSettings and Management Tip Sheet For Providers: Isp Elevated?mohamedkorieshNoch keine Bewertungen
- Respi MVDokument25 SeitenRespi MVtimie_reyesNoch keine Bewertungen
- Effect of PEEP On Dead Space in An Experimental Model of ARDSDokument10 SeitenEffect of PEEP On Dead Space in An Experimental Model of ARDSFernando SousaNoch keine Bewertungen
- Comen Bilanx AX-700 Anesthesia Machine - EN - V1.0Dokument6 SeitenComen Bilanx AX-700 Anesthesia Machine - EN - V1.0EliezerNoch keine Bewertungen
- TracheostomyDokument14 SeitenTracheostomyBryan Dorosan100% (1)
- The Effect of Exercise On The Cardiorespiratory SystemDokument15 SeitenThe Effect of Exercise On The Cardiorespiratory SystemBASAVARAJ100% (1)
- Overview of Respiratory Failure & Use of Mechanical VentilationDokument89 SeitenOverview of Respiratory Failure & Use of Mechanical VentilationsheharyarNoch keine Bewertungen
- Full Download Test Bank For Pilbeams Mechanical Ventilation 6th Edition J M Cairo PDF Full ChapterDokument13 SeitenFull Download Test Bank For Pilbeams Mechanical Ventilation 6th Edition J M Cairo PDF Full Chapterinclusa.darn8wlzuv100% (17)
- Advanced Mechanical VentilationDokument96 SeitenAdvanced Mechanical VentilationMukhtar KhanNoch keine Bewertungen
- Spontaneous Awakening and Breathing TrialsDokument12 SeitenSpontaneous Awakening and Breathing TrialsntnquynhproNoch keine Bewertungen
- Stephan F-120 Globetrotter Paediatric Ventilator - User Manual PDFDokument36 SeitenStephan F-120 Globetrotter Paediatric Ventilator - User Manual PDFngocbienk56Noch keine Bewertungen
- Drager Savina - User ManualDokument216 SeitenDrager Savina - User ManualDiana InfanteNoch keine Bewertungen
- Competencies Needed by Graduate Respiratory Therapists in 2015 and BeyondDokument16 SeitenCompetencies Needed by Graduate Respiratory Therapists in 2015 and BeyondFelipe AlbornozNoch keine Bewertungen
- 30 Facts You NEED To Know Your Covid Cribsheet - OffGuardianDokument5 Seiten30 Facts You NEED To Know Your Covid Cribsheet - OffGuardianjohnsmithdosNoch keine Bewertungen
- Lung Protective Mechanical Ventilation Strategies in Pediatric Acute Respiratory Distress SyndromeDokument9 SeitenLung Protective Mechanical Ventilation Strategies in Pediatric Acute Respiratory Distress SyndromeDenna Refnaldi SatryaNoch keine Bewertungen