Beruflich Dokumente
Kultur Dokumente
Glioblastoma Anti Tumor Action of Cyclosporin A and Functionally Related Drugs
Hochgeladen von
Ewa KaniaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Glioblastoma Anti Tumor Action of Cyclosporin A and Functionally Related Drugs
Hochgeladen von
Ewa KaniaCopyright:
Verfügbare Formate
Chapter 25
Glioblastoma: Anti-tumor Action of Cyclosporin A and Functionally Related Drugs
Bozena Kaminska, Magdalena Tyburczy, Konrad Gabrusiewicz, and Malgorzata Sielska
Abstract Human malignant gliomas are highly resistant to current therapeutic approaches. Major signaling pathways that have been identied as playing important roles in glioblastomas are: the PTEN/PI3K/Akt/mTOR and the Ras/Raf/MEK/ERK signaling cascades, which support cell invasion, survival and prevent apoptosis. In the face of tumor resistance to apoptosis, novel agents which can overcome resistance or/and affect cell survival by nonapoptotic mechanisms such as necrosis, senescence, autophagy and mitotic catastrophe, are highly desirable. The present chapter focuses on anti-tumor action of cyclosporin A (CsA) and rapamycin that besides their well known immunosuppressive abilities appear to be multitarget kinase inhibitors and moderately effective anti-tumor agents in glioblastomas in vitro, in vivo and in clinical trials. A compelling evidence shows that cyclosporin A induces growth arrest and programmed cell death in cultured rat and human glioblastoma cells. The molecular mechanism involves accumulation of a cell cycle inhibitor p21Cip1/Waf1, even in the absence of functional p53 tumor suppressor. In C6 glioma cells with functional TP53 and PTEN tumor suppressors CsA treatment up-regulates fasL expression, activates p53 and intrinsic mitochondrial death pathway, while in human glioblastoma cells with defects in either TP53 or PTEN, none
of those effects were observed. Molecular analysis revealed that CsA, trough yet unknown mechanisms, down-regulates PI3K/Akt and mTOR signaling pathways in glioblastoma cells, and interferes with proinvasive activity of tumor-inltrating microglia. A systemically applied CsA signicantly reduced growth of intracranial gliomas, tumor invasion and angiogenesis. Pharmacological inhibitors of the mTOR pathway: rapamycin, temsirolimus, everolimus and AP23573 were tested as potential targeted drugs in human glioblastoma cultures and in animal models. However, rapamycin and derivatives show moderate efcacy in patients with recurrent glioblastoma multiforme, they deserve further clinical studies, particularly in combination with PI-3K pathway inhibitors. Defects of innate and adaptive immunity are common in glioblastoma patients contributing to a lack of effective anti-tumor responses. Thus, immunosuppressants such as CsA, rapamycin and its derivatives may be an effective novel strategy to treat drug-resistant gliomas or complement apoptosis based-therapies. Keywords Glioblastomas Anti-tumor drugs Immunosuppressants Apoptosis Rapamycin Inhibitors
Introduction
B. Kaminska ( ) Laboratory of Transcription Regulation, Department of Cell Biology, Nencki Institute of Experimental Biology, 02-093 Warsaw, Poland e-mail: bozenakk@nencki.gov.pl
Glioblastomas are the most frequent and devastating primary malignant brain tumor in adults. Glioblastomas are highly resistant to current therapeutic approaches, in which surgery is followed
241
M.A. Hayat (ed.), Tumors of the Central Nervous System, Volume 2, DOI 10.1007/978-94-007-0618-7_25, Springer Science+Business Media B.V. 2011
242
B. Kaminska et al.
by radiotherapy with concomitant and adjuvant chemotherapy. The prognosis remains poor with a median survival in the range of 1215 months (Clarke et al., 2010). Common genetic abnormalities in glioblastoma are associated with multiple molecular mechanisms involved in drug resistance, including drug detoxication, aberrant activation or suppression of cellular signal transduction pathways, deciencies in tumor suppressors, apoptosis mediators and death ligand/receptor signaling. Signicantly high frequency of alterations in cell cycle regulators such as the TP53 tumor suppressor and the p16INK4A cyclin dependent kinase inhibitor results in reduced sensitivity to a majority of anti-cancer drugs (Ohgaki and Kleihues, 2009). Major signaling pathways that have been identied as playing important roles in glioblastomas are: the PTEN/PI3K/Akt/mTOR and the Ras/Raf/MEK/ERK signaling cascades, which support cell proliferation, survival, invasion, and prevent apoptosis (McCubrey et al., 2006). Components of these pathways are frequently mutated, aberrantly expressed or constitutively activated in glioblastomas. Monoclonal antibodies or small molecular-weight kinase inhibitors targeting specic pathways are the most common classes of agents in cancer treatment. However, highly selective or specic blocking of only one of the kinases has been associated with limited or sporadic responses. Therefore, multitargeted kinase inhibitors and combinations of single-target kinase inhibitors should be more effective to overcome therapeutic resistance. Some agents could be used together with radiation, chemotherapy, or immunotherapy to enhance treatment efcacy. Furthermore, in the face of tumor resistance to apoptosis, novel agents which can overcome resistance or/and induce cell death by non-apoptotic mechanisms such as necrosis, senescence, autophagy (type II programmed cell death) and mitotic catastrophe, are highly desirable. The present chapter focuses on anti-tumor action of drugs such as cyclosporin A and rapamycin that besides their well known immunosuppressive abilities appear to be kinase inhibitors and potential anti-tumor agents in glioblastomas. The present chapter summarizes a rationale and results of preclinical/clinical studies of these agents in therapy of glioblastomas.
Mechanisms of Cyclosporin A Induced Cell Death in Rat C6 Glioma Cells Mode of Immunosuppressant Action
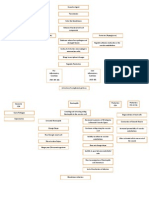
Cyclosporin A (CsA), FK506 (tacrolimus, Prograf) and rapamycin (sirolimus) are short polypeptides which have revolutionized transplantology due to ability to block the activation of lymphocytes and other immune system cells. CsA, FK506 and rapamycin bind to specic intracellular proteins called immunophilins: CsA binds to cyclophilin, FK506 and rapamycin bind to FKBP (FK506-binding protein). Drugimmunophilin complexes bind to a regulatory subunit of calcineurin and inhibit its activity. Calcineurin is a calcium- and calmodulin-dependent threonine/serine phosphatase. CsA and FK506 exert immunosuppressive effects by inhibiting of calcineurin-mediated dephosphorylation of NFAT (nuclear factor of activated T cells), thus preventing transcriptional induction of several cytokines and their receptors genes (Fig. 25.1). NFAT family proteins are transcription factors that regulate the expression of a variety of target genes and are implicated in many functions, including cell growth, survival, invasion and angiogenesis (Mancini and Toker, 2009). Several members of NFAT family were detected in C6 glioma cells pointing to a new mechanism of transcription regulation in glioma cells. A transient receptor potential 6 (TRPC6) which is required for the development of the aggressive glioblastoma phenotype and causes a sustained elevation of intracellular calcium, is coupled to activation of the calcineurin-NFAT pathway. Pharmacologic inhibition of this pathway reduced the development of the aggressive glioblastoma phenotype under hypoxia.
Molecular Mechanisms of Pro-apoptotic Action of Cyclosporin A in C6 Glioma Cells
It was reported by Mosieniak et al. (1997) that cyclosporin A at concentrations at the range of 30 60 M inhibits proliferation of rat C6 glioma cells and induces cell death. CsA-induced cell death was an
25 Glioblastoma: Anti-tumor Action of Cyclosporin A and Functionally Related Drugs
243
Fig. 25.1 Mechanism of immunosuppressant action (a) Immunosuppressants bind to immunophilines: CsA to cyclophilin (cyc) and FK506 to FKBP (FK506-binding protein); subsequently complexes bind to the calcineurin and inhibit its activity. Calcineurin is a calcium- and calmodulin-dependent phosphatase which dephosphorylates NFAT transcription factors allowing them to translocate to the nucleus, where NFAT proteins in cooperation with other transcription factors (f.e. AP-1) regulate the expression of genes coding for chemokines, cytokines and their receptors. The immunosuppressantimmunophilin complex may interfere with MAPK signaling
pathways. (b) Summary of pro-apoptotic mechanisms induced by CsA in C6 glioma cells. CsA induces activation of JNK (c-Jun amino-terminal kinase) and MKK3 (MAP kinaseactivated protein kinase)-p38 MAPK signaling pathways. It leads to activation of AP-1 and transcriptional up-regulation of FasL (ligand Fas) which binds receptor Fas expressed on glioma cells and induces cell death. Activation of p38 MAPK signaling leads to accumulation of p53 and induction of p53-dependent expression of pro-apoptotic genes involved in mitochondrial death pathway
active process requiring expression of new genes and proteins, with typical features of apoptosis: oligonucleosomal DNA fragmentation and caspase 3 activation (Mosieniak et al., 1997; Pyrzynska et al., 2000). Two major mechanisms responsible for induction of
apoptotic death by CsA were identied. Apoptotic cell death induced by CsA was associated with a persistent activation of mitogen activated protein kinases (MAPK), in particular cJun N-terminal kinase (JNK) and p38 MAPK. Prolonged activation of JNK led
244
B. Kaminska et al.
to accumulation of phosphorylated c-Jun and ATF2 (main substrates of JNK) and formation of the AP-1 transcription factor followed by transcriptional activation of the Fas Ligand expression (Pyrzynska et al., 2000). Further studies with promoter constructs depleted of DNA binding sites for particular transcription factors revealed that activation of the FasL gene promoter was only partially AP-1-dependent and collaborative action of other transcription factors was required for promoter activation. It was demonstrated that CsA down-regulates Akt signaling to facilitate activation of Forkhead family members resulting in transcriptional activation of the FasL expression (Ciechomska et al., 2003). Down-regulation of Akt signaling was necessary to permit Forkhead transcription factor translocation to the nucleus and pre-requisite to transcriptional activation of the FasL expression. Treatment of glioma cells with lower doses of CsA (110 M) was sufcient to reduce Akt phosphorylation and sensitized cells to doxorubicin, and UVC treatments (unpublished). Another event resulting from prolonged activation of MAP kinases, in particular p38 MAPK, was accumulation of the tumor suppressor p53 in glioma cells. The p53-family of transcription factors consists of three genes p53, p63, and p73 sharing significant structural and functional similarities. p53 is a potent inducer of apoptosis and tumor suppression. Many anti-cancer agents, from traditional chemo- and radiation therapies to more recently developed small molecules, exert their effects by enhancing the antiproliferative effects of p53 and transactivating p63/p73 proteins. In normal cells the p53 is expressed at low, constitutive level and localized predominantly in cytoplasm. The latent form of p53 is stabilized and activated by posttranslational modications. The activation of p53 occurs in response to DNA damage or stress such as hypoxia, nutrients or nucleotide deprivation. p53-mediated cell cycle arrest is largely brought about by induction of p21Waf1, an inhibitor of cyclindependent kinases. Activation of p53 may also result in apoptosis via transcriptional activation of a number of pro-apoptotic proteins including Bax, Fas, p85, IGF-BP3, and PIG3 and apoptotic protease activating factor-1 (apaf-1). It was reported by Pyrzynska et al. (2002) that CsA treatment results in up-regulation of p53 protein level and its accumulation in cell nuclei. Concomitantly, the levels of p21Waf1 and Bax proteins increased,
and Bcl-xL decreased in CsA-treated glioma cells. Bax protein translocated to mitochondria, as revealed by immunouorescence and double staining with a mitochondrial marker, and likely induced mitochondrial apoptotic pathway. Contribution of p53 to CsAinduced cell death was further conrmed in experiments, in which glioma cells stably transfected with a mutant p53 (p53Val135) failed to increase p21 and Bax protein levels and were less sensitive to CsA-induced apoptosis. Also primary broblasts from p53-/knockout mice were signicantly more resistant to CsA-induced apoptosis compared to their corresponding counterparts containing functional p53 (Pyrzynska et al., 2002). Accumulation and activity of p53 can be regulated by phosphorylation that occurs at several Ser and Thr residues, and a number of cellular kinases have been proposed to directly phosphorylate p53, including casein kinase I, casein kinase II, double-strandedRNA-dependent protein kinase, ATM, CDK7, DNAactivated protein kinase, Jun-NH2 kinase and p38 MAP kinase. The induction of cell death by CsA was associated with a persistent activation of MKK3-p38 MAP kinase signaling pathway. Overexpression of a dominant negative form of MKK3, an upstream activator of p38, abrogated phosphorylation of p38 MAPK and p53 accumulation (Pyrzynska et al., unpublished). Together, the compelling evidence demonstrate that the apoptotic program activated by CsA can be mediated by multiple pathways: via activation of p53 transcription factor and p53-mediated apoptosis, and through up-regulation of FasL expression by JNK-AP-1 and Forkhead (Fig. 25.1).
Cyclosporin A Induces Cell Death or Growth Arrest and Senescence of Human Glioblastoma Cells
In rat C6 glioma cells apoptotic cell death induced by CsA was associated with induction of intrinsic death pathway: p53- and mitochondria-dependent, as well as extrinsic, death ligand-dependent pathway. However, the experiments performed on glioma cells lacking a functional p53, namely the cell line stably expressing the temperature-sensitive p53 mutant, indicated that up to 20% of cells died even in the absence of functional
25 Glioblastoma: Anti-tumor Action of Cyclosporin A and Functionally Related Drugs
245
p53, suggesting also a p53-independent mode of CsA action. Therefore, we tested efcacy of CsA towards three human glioblastoma cell lines that are radioand chemotherapy resistant, in part due to mutations in the tumor suppressor PTEN or/and TP53 genes: T98G (mutated PTEN and TP53), U373-MG (mutated TP53 and PTEN) and U87-MG cells (wild type TP53/mutated PTEN). Cultured cells were exposed to increasing concentrations of CsA (Fig. 25.2) and 30 g/ml CsA affected growth of all studied glioma cells, produced dramatic changes in cell number and morphology in 24 h. The inhibitory effect of CsA on cell growth and survival was dose-dependent, and progressed with the time of exposure. CsA at the concentration range of 520 g/ml had no visible cytotoxic effects (Zupanska et al., 2005). Morphological alterations induced by 30 g/ml CsA were characterized by shrinkage of the cells, rounding up of the cell body and detachment from the bottom of the plate at 24 48 h after the treatment (Fig. 25.2). Cell death induced by CsA was blocked by cycloheximide (a protein synthesis inhibitor) and showed no signs of necrosis, such as swelling or disruption of cells. The appearance of numerous large vacuoles was observed in CsAtreated T98G cells and to less extent in U373-MG cells (Zupanska et al., 2005). Features of CsA-triggered cell death in human glioblastoma cells do not fulll all criteria of apoptosis. For example, biochemical hallmarks of apoptosis such as phosphatidylserine exposure in the external leaet of the plasma membrane bilayer, the ladder-like oligonucleosomal DNA fragmentation or appearance of the subG1 population were not detected, although condensation of chromatin, deformation of nuclei and sparse TUNEL labeling were observed. Cells in CsA-treated cultures showed bean shaped nuclei with condensed chromatin or nuclei with irregular clumps of dense chromatin. Such nuclear alterations as bean shaped nuclei with condensed chromatin usually preceded oligonucleosomal DNA fragmentation in CsA-treated rat glioma cells (Mosieniak et al., 1997). In T98G glioblastoma cells nuclear alterations were completely abolished by cycloheximide (CHX) treatment, indicating dependency of cell death on de novo protein synthesis. Measurement of changes in the mitochondrial membrane potential in response to CsA treatment with the uorescent probe JC-1 did not show alterations in mitochondrial potential, which excludes
a possibility of initiation of mitochondrial pathway along with apoptosome formation (Zupanska et al., 2005). Western blot analysis using specic antibodies recognizing intact and cleaved caspases 7, 3 and PARP (poly (ADP-ribose) polymerase-1) was employed to further characterize cell death induced by CsA. The treatment of human glioblastoma cells with 30 M CsA resulted in activation of the caspase cascade (as evidenced by the appearance of cleaved caspase 7, 3 and cleaved PARP) in T98G cells, and to lesser extent in U373-MG cells. No caspase activation was detected in U87 glioma cells (Fig. 25.2). Growth arrest may lead to replicative senescence or differentiation. Senescent cells in contrast to presenescent, proliferating or quiescent cells express a beta-galactosidase activity detectable at pH 6.0. Since atten morphology of CsA-treated U87 cells and reduction of the number of proliferating cells suggested the induction of differentiation process, a senescence-associated -galactosidase (SA-beta-Gal) staining was performed (Fig. 25.2). Untreated U87MG and T98G cells demonstrated very rare cells positive for the SA-beta-Gal staining. After 24 h of CsA treatment the percentage of cells positive for SA-beta-Gal was doubled in U87-MG cells compared to control, while only few T98G cells were positively stained. SA-beta-Gal positive U87-MG cells increased in size and attened out, thereby attaining morphology of senescent-like cells (Zupanska et al., 2005). Cell proliferation is controlled by cell cycle regulatory factors which include cyclins and cyclindependent kinases. p21WAF1/Cip1 protein is an universal inhibitor of cyclin kinases and plays an important role in inhibiting cell proliferation. The levels of p21WAF1/Cip1 protein were increased after exposure to 30 M CsA in all examined glioblastoma cell lines. The highest up-regulation of p21WAF1/Cip1 protein was observed in T98G cells and the moderate accumulation was detected in U373-MG and U87MG cells. Further studies revealed transcriptional activation of p21WAF1/Cip1 expression preceded in time by a long-term activation of ERK1/2 signaling, subsequent c-Jun phosphorylation and accumulation of AP-1 complex in CsA-treated glioblastoma cells. Pre-treatment with ERK pathway inhibitors or overexpression of dominant negative mutants MKK1, ERK2 and c-Jun reduced the p21WAF1/Cip1
246
B. Kaminska et al.
Fig. 25.2 CsA induces programmed cell death or growth arrest/senescence of malignant glioblastoma cells. (a) Morphological alterations induced by CsA treatment in human glioma cells. T98G cells cultured in DMEM with 10% fetal bovine serum, were exposed to 30 M CsA alone or with 1 g/ml cycloheximide (CHX). Upper panel shows that a majority of cells lost processes and became round in CsA-treated cultures. Lower panel shows Hoechst 33258 staining revealing deformations of cell nuclei and condensation of chromatin. CHX inhibits morphological alterations in CsA-treated T98G cells. (b) Caspase cascade activation in CsA-triggered cell death.
A representative immunoblot shows caspase activation in total protein extracts of human glioma cells treated with 30 M CsA. Specic antibodies recognizing intact and cleaved caspases 7, 3 and cleaved PARP (Cell Signaling, USA) were employed. (c) Detection of the Senescence-Associated beta-galactosidase (SA-beta-Gal) staining in CsA-treated U87-MG glioma cells. The substantial increase in cellular volume and the blue staining reecting SA-beta-Gal activity was observed in U87-MG cells treated with CsA. Original magnication for larger photos is 10; for insets 20
25 Glioblastoma: Anti-tumor Action of Cyclosporin A and Functionally Related Drugs
247
expression, conrming involvement of this pathway. Transcriptional activation of p21WAF1/Cip1 expression by CsA was independent of p53 and preceded CsA-induced growth arrest in glioblastoma cells (Zupanska et al., 2007). In conclusion, the ndings above presented demonstrate an ability of CsA to induce growth arrest or programmed, but non-apoptotic cell death in human glioblastoma cells at the concentration of 30 M or higher. Many forms of programmed cell death different from classical apoptosis have been described by the criteria of morphology, biochemistry, and response to apoptosis inhibitors, particularly in transformed cells which contain endogenous inhibitors preventing a particular pathway.
Anti-tumor Effects of CsA in Glioma Models
Good cytostatic and cytotoxic efcacy of CsA in rat and human glioblastoma cultures encouraged studies in more complex models: in organotypic brain slice cultures and in murine glioma model. Organotypic brain slice cultures injected with glioblastoma cells recapitulate many features of glioblastoma and are very useful for investigating the cellular and molecular mechanisms of glioma invasion under conditions most analogous to those of normal brains in vivo. It was reported by Markovic et al. (2005) that microglial cells contribute signicantly to invasion of glioma cells in cultured brain slices. Microglia are the intrinsic immune cells of the brain, serving principally to control the innate and the adaptive immune responses in the central nervous system, to initiate host-defense and tissue repair mechanisms. Microglial cells are attracted towards glioma (glioma tissue consists of up to 30% of microglial cells) and microglia density in gliomas positively correlates with malignancy, invasiveness and grading of the tumors (Watters et al., 2005). When glioma cells were injected into brain slices depleted of endogenous microglia (by incubation with clodronate-lled liposomes for 96 h), the invasiveness of the tumors was signicantly decreased. Inoculation of exogenous microglia together with glioma cells into cultured brain slices increased the inltrative behavior of glioma cells. Experiments with
co-culture of microglia with glioma cells revealed that soluble factors released from glioma cells strongly stimulate metalloprotease-2 (MMP-2) activity increasing breakdown of extracellular matrix and thereby promoting tumor invasiveness (Markovic et al., 2005). Further studies showed that membrane type 1 metalloproteinase (MT1-MMP) is up-regulated in gliomaassociated microglia. Microglial MT1-MMP in turn activates glioma-derived pro-MMP-2 and promotes glioma expansion. Tumor growth and invasion in ex vivo model using MT1-MMP decient brain tissue and in microglia-depleted animals were strongly reduced (Markovic et al., 2009). It was reported by Sliwa et al. (2007) that migration/invasion of uorescently labeled GL261 glioma cells in murine brain slices signicantly decreased upon treatment with CsA, even at low concentrations: 1, 10 and 30 M. Anti-invasive effects of lower, non-cytotoxic doses of CsA suggested an existence of the additional mechanism of CsA action on tumor invasion. When glioma cells were injected into slices devoid of endogenous microglia, the inhibitory effect of 1 M CsA on glioma invasiveness mostly vanished. It indicated that CsA abolishes microglia-promoting effects on glioma malignancy. The inhibitory action of CsA on microglia function has been directly demonstrated in microglia-glioma co-cultures. Glioma-derived factors in co-cultures or glioma conditioned medium induce morphological transformation of microglial cells into amoeboid phagocytes, activate MAPK signaling pathways and production of some cytokines. CsA at low doses of 0.1. and 1 M blocked transformation of microglial cells stimulated by glioma-conditioned medium and abolished pro-invasive effects of microglia (Sliwa et al., 2007). A recent study points to a crucial role of microglia-derived transforming growth factor beta 1 (TGF-1) in regulation of glioma invasion (Wesolowska et al., 2008). Blockade of TGF-1 signaling by silencing of TGF-1 type II receptor with shRNA or neutralizing anti-TGF-1 antibody abolished the promoting effect of microglia on glioma invasion. In vivo tumor models developed by intracranial or subcutaneous implantation of glioma cell lines in rodents are used to test novel therapies. The advantages of these glioma models are their highly efcient gliomagenesis, reproducible growth rates, and knowledge of tumor location. However, these
248
B. Kaminska et al.
models have been criticized for not recapitulating all pathological features of human glioblastoma multiforme (GBM), they allow to target different features of GBM, including location in the brain, invasion of brain parenchyma, angiogenesis, and secretion of immune suppressive molecules. In studies by Sliwa et al. (2007) uorescently labeled GL261 glioma cells were implanted into the striatum of DBA/2 J mice and developed gliomas of considerable size in 14 days. CsA (Sandimmun, Novartis) was administrated intraperitoneally (i.p.) every second days at doses of 2 or 10 mg/kg of body weight starting from the second day after cell inoculation. Systemically applied 2 or 10 mg/kg CsA signicantly decreased tumor volumes (by 70%) with similar efcacy. Further studies in syngenic murine models, such as GL261 mouse glioma cells implanted to C57BL6 mice, have conrmed anti-tumor action of CsA administrated intraperitoneally every second day at doses of 2 and 10 mg/kg. Immunouorescence studies with Iba1 antibody demonstrated that CsA blocks accumulation and activation of glioma-associated microglia conrming the in vitro data (unpublished). It was reported that macrophagecolony stimulating factor (M-CSF) and other cytokines secreted by high-grade glioma cells stimulate differentiation of tumor-inltrating microglia/macrophages into cells acquiring the anti-inammatory (M2) phenotype. M-CSF was signicantly correlated with histological malignancy and with the proportion of M2 microglia/macrophages in vivo. Such M2 cells instead of initiating immune responses support tumor growth and invasion. CsA with its strong effect on pro-tumorigenic activity of microglia could be effective drug in modulation of anti-inammatory M2 phenotype of microglia/macrophages in glioma therapy. CsA has been used to block the immune reaction towards human glioblastoma cells transplanted to rodent brains. It was reported by Mathiesen et al. (1989) that human glioblastoma cells implanted to cerebrum of rat hosts survive longer in immunosuppressed animals but aggressive growth of glioblastoma cells and tumor proliferation was not observed. Human glioblastoma cells implanted into the brain of Wistar rats immunosuppressed with CsA applied at 12 mg/kg/daily survived under such conditions but formed dense and poorly diffused tumors (Strojnik
et al., 2006). Up to now CsA has not been tested as anti-invasive/cytotoxic agent in clinical trials.
Anti-tumor Action of Rapamycin and Derivatives Mechanism of Action of Rapamycin
Rapamycin (Sirolimus) is a macrolide discovered 1970 as a product of the bacterium Streptomyces hygroscopicus in a soil sample from the Easter Island (Rapa Nui). Rapamycin was originally developed as an antifungal agent, but turned out to be a potent immunosuppressive drug and since 1997 has been used to prevent host-rejection in kidney transplantation. An immunosuppressive effect of rapamycin is due to the inhibition of interleukin 2 (IL-2)-mediated T-cell proliferation and activation. The mode of action of rapamycin is to bind the cytosolic immunophilin FK-binding protein 12 (FKBP12). This complex inhibits the mammalian target of rapamycin (mTOR) pathway by directly binding the mTOR Complex 1 (mTORC1). mTOR is a kinase playing a key role in the regulation of cell growth and proliferation by regulating ribosomal biogenesis and protein translation. Among others, mTOR can be activated by growth factors and hormones, which is mediated by the induction of PI-3-kinase (PI-3K). Active PI-3K generates phosphatidylinositol (3,4,5)trisphosphate [PtdIns(3,4,5)P3 ] which activates kinase Akt phosphorylating and inactivating the tuberous sclerosis complex 2 (TSC2). TSC2 acts as a GTPaseactivating protein for the small GTPase RHEB (Ras homolog enriched in brain). Inhibition of TSC2 activity leads to elevated RHEB-GTP levels and activation of mTORC1 which by its downstream effectors, such as ribosomal protein S6 kinases (S6K) and 4E-binding protein (4E-BP1), further up-regulates ribosome biogenesis and protein translation (Fig. 25.3). This results in an increase in cell size and mass, and enhanced proliferation. On the other hand, inhibition of mTOR promotes autophagy in some cell types. Autophagy is a process of degradation of organelles and macromolecules to supply cells with nutrients and can function as a cytoprotective mechanism or alternative cell death process.
25 Glioblastoma: Anti-tumor Action of Cyclosporin A and Functionally Related Drugs
249
Fig. 25.3 Rapamycin inhibits proliferation or induces cell death of malignant glioblastoma cells. (a) mTOR signaling network. mTORC1 stimulates cell growth upon activation by growth factors or insulin (for details see the text). (b) Rapamycin inhibits the kinase activity of mTOR measured by reduction of S6K phosphorylation in T98G cells. Western blot analysis of the phospho-S6K (T389) level in T98G glioma cells after treatment with 10 nM rapamycin for 24 h. S6K served as a protein loading control. (c) Rapamycin affects proliferation of T98G cells. Cell proliferation was determined 24 h after exposure to 1, 10, 30
or 60 M rapamycin using BrdU test. Bars represent the ratio of proliferating cells treated with the inhibitor related to control cells (means SEM of three independent experiments, each in triplicate). Statistical analysis was done by one-way ANOVA followed by Newman-Keuls test, p < 0.001. (d) Rapamycin induces morphological alterations in T98G cells. Phase-contrast images of T98G glioma cells performed 24 h after treatment with 10, 30 or 60 M rapamycin. Cell death was observed after using the highest drug concentration. Original magnication is 10
Rapamycin and Its Analogs in Pre-clinical and Clinical Trials in Glioblastomas
Enhanced or constitutive activation of the PI3K/Akt/mTOR pathway is an important factor in gliomagenesis (Guertin and Sabatini, 2007). In human glioblastomas Akt is activated in approximately 70% of tumors due to loss of PTEN (phosphatase and tensin homolog deleted on Chromosome 10), the tumor suppressor and negative regulator of PI-3 K/Akt signaling, and/or up-regulation of epidermal growth factor receptor (EGFR) and platelet-derived growth factor receptor (PDGFR) tyrosine kinases. PTEN mutations are present in 2040% of GBM. Since
mTOR is a crucial downstream component of the PTEN/Akt signaling, pre-clinical studies with pharmacological inhibitors of the mTOR pathway were initiated in glioblastomas. Apart from rapamycin, its analogs with improved pharmacokinetic properties were synthesized. CCI779 (temsirolimus; Wyeth), RAD001 (everolimus; Novartis) and AP23573 (Ariad) are currently being tested as potential targeted drugs in glioblastomas. Pharmacological inactivation of mTOR decreased tumor cells proliferation and tumor size in PTEN-decient mice (Rajasekhar et al., 2003). Moreover, xenografts generated from PTEN null U87 glioma cells in mice had inhibited growth and reduced proliferation rate after rapamycin treatment.
250
B. Kaminska et al.
Conversely, rapamycin did not decrease size of PTEN wild-type LN229 tumors (Wei et al., 2008). These ndings provided grounds to initiate clinical trials of mTOR inhibitors in glioblastomas. The results of six studies using sirolimus or CCI-779 (a dihydroxymethyl propionic acid ester of sirolimus) as a single agent, or sirolimus and RAD001 in combination with inhibitors of EGFR in patients with recurrent glioblastoma multiforme (GBM) are shown in Table 25.1. Treatment with CCI-779 or sirolimus alone had only a limited activity in recurrent GBM, particularly in unselected patients. In the phase II study by Chang et al. (2005) CCI-779 was administered weekly to forty-three patients with recurrent GBM (14 patients were on enzyme-inducing antiepileptic drug). Initially CCI-779 was administered at a dose of 250 mg intravenously but the dose was reduced to 170 mg because of side effects. CCI-779 was well tolerated; however, failed to demonstrate any efcacy as a single agent in patients with recurrent GBM. Despite initial disease stabilization in approximately 50% of patients, the durability of response was short. In another phase II study CCI-779 was administered in a 250-mg intravenous dose weekly to sixty-ve recurrent GBM patients with 1 chemotherapy regimen (Galanis et al., 2005). The study reported that 20 of 65 patients with recurrent GBM (36%) had radiographic improvement. Progression-free survival at 6 months was 7.8% and median overall survival was 4.4 months. Median time to progression for all patients was 2.3 months and was signicantly longer for responders
(5.4 months) versus non-responders (1.9 months). The authors assessed activation of the PI3K pathway by examining tumor specimens for total/phosphorylated Akt and p70s6 kinase, and found p70s6 kinase staining indices being signicantly more frequent in responders versus non-responders (Galanis et al., 2005). It was reported by Cloughesy et al. (2008) that rapamycin treatment leads to substantial inhibition of tumor cell proliferation in seven of 14 patients, as demonstrated by reduction of Ki-67 staining in a subset of patients with PTEN loss. Inhibition of mTOR signaling was observed in tumor tissue. However, rapamycin led to the activation of Akt in some patients, which correlated with faster tumor progression the authors concluded that rapamycin has anti-cancer activity in PTEN-decient glioblastoma and deserves further clinical study alone or in combination with PI3K pathway inhibitors. More recently, based on evidence of the synergism between inhibitors of mTOR and EGFR (Rao et al., 2005), several studies investigated such a combination. In two trials a partial radiological response (50% decrease in the product of perpendicular diameters of contrast enhancing mass without new lesions) was seen. Doherty et al. (2006) reported a trial on 22 GBMs and six anaplastic gliomas patients treated with either getinib 500 mg or erlotinib 150 mg orally/daily in combination with sirolimus administered at a dose of 6 mg orally the rst day followed by 4 mg orally once daily thereafter. Both medications were given daily in 28-day cycles. Out of this cohort, 19% of patients
Table 25.1 Results of targeted therapy trials of mTOR inhibitors used alone or in combination with inhibitors of EGFR in recurrent glioblastomas Radiological Median PFS 6-month Median OS Study Treatment Patients (n) response (%) (months) PFS (%) (months) Chang et al. (2005) CCI-779, 170250 mg 43 5 weekly Galanis et al. (2005) CCI-779, 250 mg weekly 65 0 Cloughesy et al. Sirolimus, 2, 5, or 10 mg 15 14 (2008) daily Doherty et al. Sirolimus, 4 mg daily; 22 18 (2006) getinib, 500 mg, or erlotinib, 150 mg daily Kreisl et al. (2009) RAD001, 70 mg weekly; 22 14 getinib, 250 mg daily Reardon et al. Sirolimus, 510 mg daily; 32 0 (2010) erlotinib, 150450 mg daily PFS, progression-free survival; OS, overall survival; NA, not available 2.3 2.3 NA 3 3 8 NA 25 NA 4.4 NA NA
2.6 1.8
5 3
5.8 8.5
25 Glioblastoma: Anti-tumor Action of Cyclosporin A and Functionally Related Drugs
251
experienced a partial response and 50% had stable disease; 6-month progression-free survival (6 M-PFS) was 25%. In a second study on 22 patients (all had received prior radiation and chemotherapy) receiving getinib (250 mg daily) and everolimus (70 mg weekly), 14% of patients had a partial response and 36% of patients stable disease; median overall survival was 5.8 months (Kreisl et al., 2009). Overall response rate was 19% and a 6 M-PFS of 25% in GBM patients. No molecular markers of response were described. A retrospective review of eight consecutive negative phase II trials in recurrent malignant gliomas from the M.D. Anderson Cancer Center found a 6 MPFS for GBM of 15%. For comparison, among GBM patients treated with temozolomide at 200 mg/m2 /day orally for the rst 5 days of a 28-day cycle, PFS at 6 months was 18%; median progression-free survival and median overall survival were 2.1 and 5.4 months, respectively. The 6-month survival rate was 46% (Brada et al., 2001). Although the trials demonstrate moderate clinical benets from the combination of two drugs, ongoing phase I/II studies are investigating the efcacy of using mTOR inhibitors with other targeted agents and chemoradiation, namely: sirolimus plus vandetanib, CCI-779 or RAD001 plus temozolomide, CCI-779 plus radiation or sorafenib or bevacizumab or perifosine, RAD001 plus AEE788, and RAD001 plus Gleevec and hydroxyurea (http://clinicaltrials.gov).
General Considerations
A use of CsA may raise reservations due to employment of drug blocking the immune system in tumor patients, poor drug accessibility due to blood-brain barrier or general toxicity. However, a growing evidence shows both innate and adaptive immunity impaired in glioblastomas (Yang et al., 2010). Glioblastomas are poorly immunogenic and do not express specic tumor antigens (Watters et al., 2005). Microglia inltrating glioblastomas are converted into tumor supportive cells and contribute to tumor growth (Markovic et al., 2005, 2009; Sliwa et al., 2007). Microglial cells operate as the rst line innate and adaptive immunity of the central nervous system (CNS). In the normal CNS, microglia express low levels of major histocompatibility complex (MHC)
class I and class II molecules and co-stimulatory molecules such as CD86 and CD40. Upon activation, microglia convert to an active phenotype, upregulate MHC class I and class II and co-stimulatory molecules and take part in CD4-and CD8-specic T cell responses. Furthermore, malignant glioblastoma cells secrete chemoattractants and growth factors, including monocyte chemoattractant protein 1 (MCP-1), colony stimulating factor 1 (CSF-1), granulocyte-macrophage colony stimulating factor (GM-CSF), hepatocyte growth factor (HGF) and recruit microglia. Even though glioblastoma accumulate many microglia, macrophages and a small population of lymphocytes, the defense mechanisms are down-regulated. It was reported by Hussain et al. (2006) that glioblastoma-inltrating microglia isolated from human tumor tissue samples do not produce inammatory cytokines: interleukin 1 (IL-1), interleukin 6 and tumor necrosis factor (TNF-), cytokines critical for developing effective innate immune responses. On the contrary, glioma-associated microglia/ macrophages might promote tumor growth by inducing immunosuppression in the tumor microenvironment. Glioblastoma cells and accumulating microglia release several cytokines, such as interleukin 10 (IL10) and TGF- which may inhibit T-cell activation and contribute to the local glioma immunosuppressive milieu (Watters et al., 2005). An effective antitumor T-cell response is decreased in glioblastomas, because expression of MHC class II and co-stimulatory B7 molecules is reduced and microglia appear decient in proper antigen presentation. Thus, potential immunossuppressive effects of CsA can be neglected because the immune system in glioblastoma patients is already paralyzed and anti-tumor responses are nonfunctioning. Although, tumors incidence in transplant recipients is a recognized consequence, a recent examination of reported cases of tumor in the transplant population of the Israel Penn International Transplant Tumor Registry shows that primary brain tumors, including gliomas, do not appear to be overrepresented in the Registry, indicating that they may not arise with increased frequency in transplant recipients (Schiff, 2004). As it has been shown in animal glioma model by Sliwa et al. (2007), CsA has a systemic effect, can affect cell interactions in tumor microenvironment and block pro-tumorigenic activity of tumor inltrating
252
B. Kaminska et al.
microglia/macrophages. A recent study demonstrates that mTOR signaling controls microglial activation in response to cytokines and appears to play a crucial role in regulating of microglial viability (Dello Russo et al., 2009). Thus anti-tumor action of rapamycin in vivo may be partly due to interference with cell interactions in tumor microenvironment. The blood-brain barrier (BBB) possesses a signicant impediment for the delivery of therapeutic drugs into the brain. In the normal adult brain, the BBB mainly consists of vascular endothelial cells, astrocytes and pericytes. In malignant glioblastomas, the blood vessel network is broken down. Increased permeability of tumor blood vessels is induced by angiogenic factors released by malignant glioma cells, such as vascular endothelial growth factor (VEGF) that is associated with intravascular migration of glioma cells into blood vessels and their transfer to distant areas in the brain via blood ow. The mechanism of vascular permeability is used by glioma cells to facilitate migration and invasiveness, but can be also employed to facilitate delivery of anti-tumor medicines into the brain (Tate and Aghi, 2009). Previous studies demonstrated that a systemic injection of 100 mg/kg/i.p. CsA results in a blood concentration of 10 M maintained for at least 18 h (Ciechomska et al., 2005). Thus, concentrations of CsA (2 and 10 mg/kg) tested in animal glioma model correspond to blood concentrations of 0.2 or 1 M, respectively. A permeable blood-brain barrier in brain tumors may result in similar CsA concentrations in the brain as detected in the blood. In contrast to widely accepted notion that CsA does not cross or poorly cross the blood-brain barrier, studies on immunosuppressed patients demonstrated the presence of CsA in cerebrospinal uids suggesting that the drug is able to cross the blood-brain barrier. Furthermore, CsA may impair the brain endothelial barrier function by accelerating NO production in the brain endothelial and astroglial cells. Notably, CsA at lower micromolar concentrations does not affect survival of non-transformed cells. Neurons from mixed neuronal-glial cultures developed from hippocampal dentate gyrus are affected by CsA at the concentrations higher than 810 M (Kaminska et al., 2001). Astrocytes are more resistant and CsA at concentration of 40 M or higher affects the survival of astrocytes from neonatal brain cultures. Altogether, these results suggest that CsA, particularly
at lower concentrations affecting pro-invasive activity of microglia, could be effective anti-tumor drug without inducing neurotoxicity. CsA induces cell death via multiple mechanisms and some of them are able to prevail alterations of growth regulatory and apoptotic pathways, caused by common mutations in human glioblastomas. Rapamycin and its derivatives, besides the well described inhibition of mTOR pathway in glioblastoma cells, may additionally affect proinvasive activity of glioblastoma inltrating microglia. The unique mechanism of action of CsA and pharmacological inhibitors of the mTOR pathway justies further research on their anti-tumoral properties either alone or in combined therapies.
Acknowledgements This work was supported by grant P-N/024/2006.
References
Brada M, Hoang-Xuan K, Rampling R, Dietrich PY, Dirix LY, Macdonald D, Heimans JJ, Zonnenberg BA, Bravo-Marques JM, Henriksson R, Stupp R, Yue N, Bruner J, Dugan M, Rao S, Zaknoen S (2001) Multicenter phase II trial of temozolomide in patients with glioblastoma multiforme at rst relapse. Ann Oncol 12:259266 Chang SM, Wen P, Cloughesy T, Greenberg H, Schiff D, Conrad C, Fink K, Robins HI, De Angelis L, Raizer J, Hess K, Aldape K, Lamborn KR, Kuhn J, Dancey J, Prados MD (2005) Phase II study of CCI-779 in patients with recurrent glioblastoma multiforme. Invest New Drugs 23: 357361 Ciechomska I, Legat M, Golab J, Wesolowska A, Kurzaj Z, Mackiewicz A, Kaminska B (2005) Cyclosporine A and its non-immunosuppressive derivative NIM811 induce apoptosis of malignant melanoma cells- in vitro and in vivo studies. Int J Cancer 117:5967 Ciechomska I, Pyrzynska B, Kazmierczak P, Kaminska B (2003) Inhibition of Akt kinase signalling and activation of Forkhead are indispensable for up-regulation of FasL expression in apoptosis of glioma cells. Oncogene 22: 76177627 Clarke J, Butowski N, Chang S (2010) Recent advances in therapy for glioblastoma. Arch Neurol 67:279283 Cloughesy TF, Yoshimoto K, Nghiemphu P, Brown K, Dang J, Zhu S, Hsueh T, Chen Y, Wang W, Youngkin D, Liau L, Martin N, Becker D, Bergsneider M, Lai A, Green R, Oglesby T, Koleto M, Trent J, Horvath S, Mischel PS, Mellinghoff IK, Sawyers CL (2008) Antitumor activity of rapamycin in a phase I trial for patients with recurrent PTEN-decient glioblastoma. PLoS Med 5:e8 Dello Russo C, Lisi L, Tringali G, Navarra P (2009) Involvement of mTOR kinase in cytokine-dependent microglial activation and cell proliferation. Biochem Pharmacol 78:12421251
25 Glioblastoma: Anti-tumor Action of Cyclosporin A and Functionally Related Drugs Doherty L, Gigas DC, Kesari S, Drappatz J, Kim R, Zimmerman J, Ostrowsky L, Wen PY (2006) Pilot study of the combination of EGFR and mTOR inhibitors in recurrent malignant gliomas. Neurology 67:156158 Galanis E, Buckner JC, Maurer MJ, Kreisberg JI, Ballman K, Boni J, Peralba JM, Jenkins RB, Dakhil SR, Morton RF, Jaeckle KA, Scheithauer BW, Dancey J, Hidalgo M, Walsh DJ (2005) Phase II trial of temsirolimus (CCI-779) in recurrent glioblastoma multiforme: a North Central Cancer Treatment Group study. J Clin Oncol 23:52945304 Guertin DA, Sabatini DM (2007) Dening the role of mTOR in cancer. Cancer Cell 12:922 Hussain SF, Yang D, Suki D, Grimm E, Heimberger AB (2006) Innate immune functions of microglia isolated from human glioma patients. J Transl Med 30:1524 Kaminska B, Figiel I, Pyrzynska B, Czajkowski R, Mosieniak G (2001) Treatment of hippocampal neurons with cyclosporin a results in calcium overload and apoptosis which are independent on NMDA receptor activation. Br J Pharmacol 133:9971004 Kreisl TN, Lassman AB, Mischel PS, Rosen N, Scher HI, Teruya-Feldstein J, Shaffer D, Lis E, Abrey LE (2009) A pilot study of everolimus and getinib in the treatment of recurrent glioblastoma (GBM). J Neurooncol 92:99105 Mancini M, Toker A (2009) NFAT proteins: emerging roles in cancer progression. Nat Rev Cancer 9:810820 Markovic DS, Glass R, Synowitz M, Rooijen N, Kettenmann H (2005) Microglia stimulate the invasiveness of glioma cells by increasing the activity of metalloprotease-2. J Neuropathol Exp Neurol 64:754762 Markovic DS, Vinnakota K, Chirasani S, Synowitz M, Raguet H, Stock K, Sliwa M, Lehmann S, Klin R, van Rooijen N, Holmbeck K, Heppner FL, Kiwit J, Matyash V, Lehnardt S, Kaminska B, Glass R, Kettenmann H (2009) Gliomas induce and exploit microglial MT1-MMP expression for tumor expansion. Proc Natl Acad Sci USA 106:1253012535 Mathiesen T, Collins VP, Olson L, Granholm L (1989) Prolonged survival and vascularization of xenografted human glioblastoma cells in the central nervous system of cyclosporine a treated rats. Cancer Lett 44:151156 McCubrey JA, Steelman LS, Abrams SL, Lee JT, Chang F, Bertrand FE, Navolanic PM, Terrian DM, Franklin RA, DAssoro AB, Salisbury JL, Mazzarino MC, Stivala F, Libra M (2006) Roles of the RAF/MEK/ERK and PI3K/PTEN/AKT pathways in malignant transformation and drug resistance. Adv Enzyme Regul 46:249279 Mosieniak G, Figiel I, Kaminska B (1997) Cyclosporin A, an immunosuppressive drug, induces programmed cell death in rat C6 glioma cells by a mechanism that involves the AP-1 transcription factor. J Neurochem 68:11421149 Ohgaki H, Kleihues P (2009) Genetic alterations and signaling pathways in the evolution of gliomas. Cancer Sci 100: 22352241 Pyrzynska B, Mosieniak G, Kaminska B (2000) Changes of the trans-activating potential of AP-1 transcription factor during cyclosporin a-induced apoptosis of glioma cells are mediated by phosphorylation and alterations of AP-1 composition. J Neurochem 74:4251
253
Pyrzynska B, Serrano M, Martinez-A C, Kaminska B (2002) Tumor suppressor p53 mediates apoptotic cell death triggered by cyclosporine A. J Biol Chem 277: 1410214108 Rajasekhar VK, Viale A, Socci ND, Wiedmann M, Hu X, Holland EC (2003) Oncogenic Ras and Akt signaling contribute to glioblastoma formation by differential recruitment of existing mRNAs to polysomes. Mol Cell 12: 889901 Rao RD, Mladek AC, Lamont JD, Goble JM, Erlichman C, James CD, Sarkaria JN (2005) Disruption of parallel and converging signaling pathways contributes to the synergistic antitumor effects of simultaneous mTOR and EGFR inhibition in GBM cells. Neoplasia 7:921929 Reardon DA, Desjardins A, Vredenburgh JJ, Gururangan S, Friedman AH, Herndon JE 2nd, Marcello J, Noreet JA, McLendon RE, Sampson JH, Friedman HS (2010) Phase 2 trial of erlotinib plus sirolimus in adults with recurrent glioblastoma. J Neurooncol 96:219230 Schiff D (2004) Gliomas following organ transplantation: analysis of the contents of a tumor registry. J Neurosurg 101: 932934 Sliwa M, Markovic D, Gabrusiewicz K, Synowitz M, Glass R, Zawadzka M, Wesolowska A, Kettenmann H, Kaminska B (2007) The invasion promoting effect of microglia on glioblastoma cells is inhibited by cyclosporin A. Brain 130:476489 Strojnik T, Kavalar R, Lah TT (2006) Experimental model and immunohistochemical analyses of U87 human glioblastoma cell xenografts in immunosuppressed rat brains. Anticancer Res 26:28872900 Tate MC, Aghi MK (2009) Biology of angiogenesis and invasion in glioma. Neurotherapeutics 6:447457 Watters JJ, Schartner JM, Badie B (2005) Microglia function in brain tumors. J Neurosci Res 81:447455 Wei LH, Su H, Hildebrandt IJ, Phelps ME, Czernin J, Weber WA (2008) Changes in Tumor Metabolism as Readout for Mammalian Target of Rapamycin Kinase Inhibition by Rapamycin in Glioblastoma. Clin Cancer Res 14: 34163426 Wesolowska A, Kwiatkowska A, Slomnicki L, Dembinski M, Master A, Sliwa M, Franciszkiewicz K, Chouaib S, Kaminska B (2008) Microglia-derived TGF-beta as an important regulator of glioblastoma invasion-an inhibition of TGF-beta-dependent effects by shRNA against human TGF-beta type II receptor. Oncogene 27:918930 Yang I, Han SJ, Kaur G, Crane C, Parsa AT (2010) The role of microglia in central nervous system immunity and glioma immunology. J Clin Neurosc 17:610 Zupanska A, Adach A, Dziembowska M, Kaminska B (2007) Alternative pathway of transcriptional induction of p21WAF1/Cip1 by cyclosporine A in p53decient human glioblastoma cells. Cell Signal 19: 12681278 Zupanska A, Dziembowska M, Ellert-Miklaszewska A, Gaweda-Walerych K, Kaminska B (2005) Cyclosporine A induces growth arrest or programmed cell death of human glioma cells. Neurochem Int 47:430441
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Characteristics of Compounds That Cross The Blood-Brain BarrierDokument5 SeitenCharacteristics of Compounds That Cross The Blood-Brain BarrierAlix AliNoch keine Bewertungen
- CSF, BBB pRESENTATIONDokument39 SeitenCSF, BBB pRESENTATIONyonnahNoch keine Bewertungen
- Radiofrequency/Microwave Radiation Review Examines Biological Effects & Safety StandardsDokument32 SeitenRadiofrequency/Microwave Radiation Review Examines Biological Effects & Safety StandardsjslovelyNoch keine Bewertungen
- Delivering Drug To BrainDokument26 SeitenDelivering Drug To BrainMohd Nizam MordiNoch keine Bewertungen
- How Inflammation May Cause Depression and Lead to New TreatmentsDokument12 SeitenHow Inflammation May Cause Depression and Lead to New Treatmentssimas100% (1)
- 012416R255A FNL Ascaris Fluke Tapeworm PDFDokument721 Seiten012416R255A FNL Ascaris Fluke Tapeworm PDFfumiNoch keine Bewertungen
- Drug Repurposing in Neurological Disorders: Implications For Neurotherapy in Traumatic Brain InjuryDokument30 SeitenDrug Repurposing in Neurological Disorders: Implications For Neurotherapy in Traumatic Brain InjurykabithNoch keine Bewertungen
- Pathophysiology of Septic Encephalopathy A ReviewDokument6 SeitenPathophysiology of Septic Encephalopathy A ReviewFerdila Putri A DilaNoch keine Bewertungen
- NIH Public Access: Author ManuscriptDokument12 SeitenNIH Public Access: Author Manuscriptleucos90Noch keine Bewertungen
- Dasar FarmakologiDokument102 SeitenDasar FarmakologiAvivah Rohmatul JannahNoch keine Bewertungen
- CNS Pathology SummaryDokument38 SeitenCNS Pathology Summaryimeds100% (2)
- Ammonia Blood Brain BarrierDokument2 SeitenAmmonia Blood Brain BarrierAgron DajaNoch keine Bewertungen
- Concept Map - SepsisDokument9 SeitenConcept Map - SepsismarkyabresNoch keine Bewertungen
- The Cells of the Nervous System: Neurons, Glia, and the Blood-Brain BarrierDokument5 SeitenThe Cells of the Nervous System: Neurons, Glia, and the Blood-Brain BarrierArcanus LorreynNoch keine Bewertungen
- The Blood-Brain BarrierDokument13 SeitenThe Blood-Brain BarrierCabinet VeterinarNoch keine Bewertungen
- Magnetic Iron Oxide Nanoparticles For Imaging, Targeting and Treatment of Primary and Metastatic Tumors of The BrainDokument19 SeitenMagnetic Iron Oxide Nanoparticles For Imaging, Targeting and Treatment of Primary and Metastatic Tumors of The BrainGurvinder SinghNoch keine Bewertungen
- Introduction To CNS PharmacologyDokument13 SeitenIntroduction To CNS PharmacologyDr.U.P.Rathnakar.MD.DIH.PGDHM100% (1)
- The Utility of Oligopeptidase in Brain-Targeting Delivery of An Enkephalin Analogue by Prodrug DesignDokument4 SeitenThe Utility of Oligopeptidase in Brain-Targeting Delivery of An Enkephalin Analogue by Prodrug Designamit4513Noch keine Bewertungen
- Long COVID or Post-Acute Sequelae of COVID-19 (PASC) - An Overview of Biological Factors That May Contribute To Persistent SymptomsDokument24 SeitenLong COVID or Post-Acute Sequelae of COVID-19 (PASC) - An Overview of Biological Factors That May Contribute To Persistent SymptomsRicardo Pariona LlanosNoch keine Bewertungen
- Contrast MediaDokument11 SeitenContrast MediaSam100% (8)
- Draft Information Package Leaflet Regarding Polysorbates Used Excipients Medicinal Products Human - enDokument42 SeitenDraft Information Package Leaflet Regarding Polysorbates Used Excipients Medicinal Products Human - enabhi200291Noch keine Bewertungen
- (RSC Nanoscience Nanotechnology) Albert Van Den Berg Loes Segerink Paul O'Brien Ralph Nuzzo Joao Rocha Xiaogang Liu A Khademhosseinni K SuDokument323 Seiten(RSC Nanoscience Nanotechnology) Albert Van Den Berg Loes Segerink Paul O'Brien Ralph Nuzzo Joao Rocha Xiaogang Liu A Khademhosseinni K SuAndreea SperiatuNoch keine Bewertungen
- MobileWise Mobile Phone Health Risks Compressed - WWW - Indonesu.co - IdDokument47 SeitenMobileWise Mobile Phone Health Risks Compressed - WWW - Indonesu.co - IdvicnitNoch keine Bewertungen
- HIV-associated Neurocognitive Disorders: Review Open AccessDokument10 SeitenHIV-associated Neurocognitive Disorders: Review Open AccessFajar Rudy QimindraNoch keine Bewertungen
- Cerebrospinal Fluid Flow - Anatomy and Functions - KenhubDokument8 SeitenCerebrospinal Fluid Flow - Anatomy and Functions - KenhubSajal SahaNoch keine Bewertungen
- Blood-Brain Barrier Controls Substance EntryDokument3 SeitenBlood-Brain Barrier Controls Substance EntryChidera EmmanuelNoch keine Bewertungen
- FocDokument336 SeitenFocRuban DanielNoch keine Bewertungen
- Pathophysiology of Febrile SeizuresDokument8 SeitenPathophysiology of Febrile SeizuresJaleah Gwyneth Fernandez EdullantesNoch keine Bewertungen
- High-Dose Methotrexate With R-CHOP Therapy For The Treatment of Patients With Primary Central Nervous System LymphomaDokument7 SeitenHigh-Dose Methotrexate With R-CHOP Therapy For The Treatment of Patients With Primary Central Nervous System LymphomaFariz NurNoch keine Bewertungen
- Safe Schools 2012 Wireless IniativeDokument33 SeitenSafe Schools 2012 Wireless IniativeGet the Cell Out - Atlanta ChapterNoch keine Bewertungen