Beruflich Dokumente
Kultur Dokumente
Paper For International Conference at Chennai
Hochgeladen von
bhagabata1957Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Paper For International Conference at Chennai
Hochgeladen von
bhagabata1957Copyright:
Verfügbare Formate
Prof.
Bhagabata Patro
Professor and Chairman, Board of Studies in Economics. To Dr. S.Thirunavukkarasu HOD, Economics, R.K.M.Vivekananda College Chennai-4.
Department of Economics, Berhampur University, Bhanja Bihar, Berhampur-760007 Orissa, India. 16.10.2011
Sub: Submission of paper for the proposed International Seminar. Dear Sir, Please refer to our telephonic discussion on participating in the proposed international seminar. Yesterday, I have sent a copy of the paper which could not be completed due to problem in the computer. I am now sending the paper for necessary publication in the book to be brought out on this occasion. The hardcopy of the paper ,registration form alongwith the bankdraft will be sent after my return to Berhampur on 20th . Please make arrangement for accommodation as discussed. Rest when we will meet at Chennai. Please confirm receipt of the paper within a day or two or over telephone, so that I will book ticket . With thanks. Yours Sincerely, Encl: Copy of the paper ( Bhagabata Patro)
----------------------------------------------------------------------------------------------------------Res: Plot No-15/182, Guru Dronacharya Nagar, Basanta Bihar, Ambapua, Berhampur -760010 Tel-06802227260; Res: 06802404365; Mob-09861676133; Fax: 06802343633. E-mail: patro_b1957@rediffmail.com
Challenges to Health Infrastructure Development in the Twelfth Five year Plan of India-An Inter State Analysis
Prof. Bhagabata Patro Department of Economics , Berhampur University.
Paper to be presented in the International Conference on Development Perspectives in the Post Reform Period:Challenges and Strategies." to be held at R.K.Mission Vivekananda College, Chennai on 29th October ,2011
Challenges to Health Infrastructure Development in the Twelfth Five year Plan of India -An Interstate Analysis
Introduction
For growth to be sustained in the long run, the approach should be broad-based across sectors and sections of the people. Latest emphasis on inclusive growth focuses on economic growth which is a necessary and crucial condition for poverty reduction. It adopts a long term perspective towards sustained growth. Issues of structural transformation therefore play a vital role. Any observer of the Indian economy today is struck by three puzzling observations.(World Bank, 2006) . These are; Economic optimism and changes in fundamentals. Indias economic progress has been significant over the years at around 8 percent in the recent years, but at the same time, by many individual measures of infrastructure capacity, corruption, education, and regulatory environment, India remains a difficult economic environment. Deteriorating performance of the public sector Indias sterling economic performance has been accompanied by a situation of growing concern that the basic institutions, organizations, and structures for public sector action are failing especially for those at the bottom. The contrasting situation of bad and good in plenty. Wide gap exists In India between the performance of the top and the bottom. Chronic Poverty and extreme affluence is visible side by side in the education, health and other sectors of the economy. Rural India have poverty rates comparable to borderline failed states, such as Haiti and Nigeria, and have child malnutrition rates higher than any other country in the world. Amartya Sen, the Nobel laureate emphasized that development is much more than increasing material well-being of a person. It includes expansions in capabilities and both positive and negative freedoms. Development progress is not simply to be measured as rise in aggregate of economic activity but as an assessment of the inclusiveness of economic growth, with emphasis on the right distribution of gains. An individual must be confident of full participation and enjoy the social civic life. There are heated ideological debates about the proper role of government in some economic spheres, but there is near universal agreement that the government(at all levels) has a responsibility to its citizens in certain core areas like elementary education, health, rural drinking water, rural sanitation, child nutrition, housing for the poor, employment guarantee and watershed management.(Planning Commission ,2008). The eleventh plan declared in its vision that with regard to indicators of human development such as literacy and maternal and infant mortality the improvement is slow and we lag behind several other Asian countries. (Eleventh Plan, 2007-12). The inequality in the access to these public services has not reduced over the years. Rather than stimulating broad economic and social progress,
public policy has simply reproduces the prevailing pattern of inequality. (World Development Report, 2006). Debates may continue over whether this responsibility is best discharged using direct production of services by the state or by other modes and how services in these core areas are to be financed. But there is a growing sense among politicians, civil servants, and academics that the ability of Indias existing institutions to deliver on those responsibilities is deterioratingeven as the economy booms. In the face of these problems, a striking feature of the recent Indian experience is a trend of shifting from public to private provision of many core services. The process of outsourcing few of the core services to the private sector in a haphazard manner greatly diluted the quality of these services and lack of accountability for it. The worst of all is the way it is available for a selected group of elites neglecting the requirement of masses. Status of health has significant influence on the development of an economy. It is directly linked to the productivity of human resources. In the Indian context with around 80 percent of the population living in rural areas, the quality of the rural manpower greatly determines their earning capacity and the level of economic activity in the rural economy. Poverty in India is mostly a rural phenomenon due to this. Low economic activity leads to low income and thus low nutritional intake. It acts like a vicious circle from which it is difficult to escape. Sustainable high growth of the economy is possible only when this issue is tackled at the national level. With this background this paper intends to examine i) how there exists a disparity in the interstate availability of health infrastructure and ii) as to how this influences the per capita income of these states. The assumption in the second case is that quality health will raise the productivity of all sectors of the economy.
Health Sector in India: An International Comparison
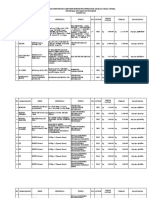
In the division of functions among the units of governments, the Indian constitution has placed health in the domain of the state list. But due to paucity of resources with the states, it is not possible to bring any significant change in health service delivery without central support. Central intervention in the health sector appears to be marginal over the years as is evident from the place of the social sector (which is placed in the last ) in the Economic Survey document of the central government. The NRHM is the latest flagship programme of the central government in the health sector to improve the basic health indicators. It has a focus on child and maternal health care. The earlier efforts of the centre is mostly related to family welfare and specific disease control programmes. A comparison of basic health indicators among selected countries reveals the highly deplorable health situation of the country. Table-I below gives the picture with regard to few key variables. Table -1: Selected Health Indicators of Selected Countries in the World Indicators Infant Mortality Rate (under five )2001 Maternal Mortality rate (per 1,00,000 live India 93 440 USA 11 12 China 12 60 Global 81 NA
birth)1995 Birth attended by skilled 42 99 health staff( % of total ) 2000 Per capita health 23 4499 Expenditure (in dollars) (1997-2000 Source : World Development Report ,2004.
70 45
Na 482
The situation with regard to health workforce and infrastructure is given in table 2 below Table-2: A Comparative Picture of Selected Countries . (2000-10) Items/ Country India Numb er (in 000s) Density per 10,000 people 6 13 Health Workforce and Infrastructure In USA Numb er (in 000s) 794 2927 464 250 China Number (in 000s) 1905 1855 51 342 1113 31 11.8 41 1.1 Global Number (in 000s) 9172 19380 1933 2587 1370 29 1.8
Physician 660 Nursing and 1430 Midwife Personnel Dentistry Personnel 78 7 Pharmaceutical 578 5.2 Personnel Community Health 51 0.5 Workers Hospital Beds per 9 10000 population Radio Therapy Units 0.4 per 1000000 population Source: World Health Statistics, 2011.
Density per 10,000 people 26.7 98.2 16.3 8.8
Density per 10,000 people 14.2 13.8 0.4 2.5 8.3
Density per 10,000 people 14 29.7 3.0 4.1 4.0
Strategy of the Eleventh Plan:
The eleventh plan has not made any major departure from the earlier plans with regard to health sector priority. As usual it declared, We need to transform public healthcare into an accountable, accessible and affordable system of quality service. The plan thought of a comprehensive approach covering individual healthcare, public health, sanitation, clean drinking water, access to food and knowledge of hygiene and feeding process. The time bound goals identified are; Reducing MMR to 1 per 1000 live birth
Reducing IMR to 28 per 1000 live birth Reducing TFR to 2.1 Providing clean drinking water to all villages by 2009. Reducing malnutrition among children of age group 0-3 to half its present level Raising the sex ratio for age group 0-6 to 935 for 1000 male child by the end of the plan.
In addition to all these the 11th plan also targeted to reduce Kala-azar by 100 percent, Malaria by 70 percent, Filarial/Microfilaria by 80 percent, Dengue by 50 percent and other diseases substantially. With regard to infrastructure, the 11th plan through NRHM stated to have one ASHA for every 1000 population, 2 ANMs for each SCs, Three staff nurses for each PHCs, seven specialists, and nine staff nurses for each CHCs., mobile health units for each districts, strengthening of SDH and DHs and untied and annual maintenance grants to all SCs, PHCs and CHCs to meet local health action.
Mid-Term Appraisal of the 11th Plan:
Public Spending on Health
Total public expenditure on health which was targeted to be around 2-3 percent of GDP has not reached till 2010-11. Only on health it has gone up from 1.02 in 07-08 to 1.09 in 09-10 which is a very small increase. This clearly indicates the gap between target and the actual situation of public funding of the health sector. Status of Maternal Mortality
The target of MMR for 11-12 was fixed at 100 per 1, 00,000 live birth from the initial level of 254. The Mid-term appraisal candidly admitted that it is not at all possible to achieve this unless there is area specific interventions. Infant Mortality Situation
The IMR target for the 11th plan was to achieve 28 per thousand live births. By 2008, for which data is available it has gone down by 4 points in a period of about 2 years which means the decline is 2 points annually. However, the target is to reduce by 6 points per annum which appear to be impossible for the government to achieve with the present institutional and manpower pattern. Total Fertility Rate
Population growth depends on total fertility rate of women which can be controlled by artificial methods. The target for this is 2.1 by the end of the plan. By 2008, it has reached to 2.6 as against 2.9 in the year 2006. As the situation reveals, this variable can be achieved by the end of the plan. But it is worthy to mention that limiting the size of the
family is probably more due to awareness and education of the people rather than government measures to have this. Health Infrastructure
The programme to have an ASHA activist for every 1000 population has not reached so far. As against the requirement of 12 lakh Asha Karmis (population of 121 crore) by the end of 2010 only 8.33 lakh Asha Karmis are at place. The appointment of specialists, doctors, staff nurses, ANMs and paramedical staff has increased but not as promised in the plan documents. The appointment of all these personnel on contract basis defeats the requirement of committed service requirement in hilly and interior regions. It is difficult to evaluate the performance in these areas due to specific targets mentioned in the original plan document. With regard to Mobile Medical unit in each of the around 6oo districts it is reported that only 381 districts have got it . The Economic Survey 10-11 admitted that there is still shortage of 20,486 sub-centers, 4477 PHCs and 2337 CHCs as per the requirement of 2001 census. So if we take 2011 census figures, the gap will definitely be enormous. The growth of health services in the private sector over the past few years indicate that the health services are beyond the reach of the common man. About 70 percent of hospitals and 37 percent beds are in the private sector as per the report of NCMH, 2005.
Health Indicators over Time:
One basic question comes to the mind of a researcher in health economics while evaluating the role of public sector is whether there is any quantum change in the health infrastructure in the country over the last sixty years. This is likely to influence the health indicators of the country. Table below makes a comparison between situation in 1951, 1981 and in 2011. Table 3: Evolution of Health Infrastructure in India. Item Number of Medical colleges No. of Hospitals and dispensaries PHCs, CHCs & Sub Centers Beds 1951 28 9209 725 117178 1981 111 23555 57363 569495 % change 2011 in 81 over 51 396 273 156 7812 486 % change in 2011 over 81 246
Doctors 65130 277360 426 Nurses 16550 154280 932 Source: Economic Survey, 1994-95 & 2010-11 and Government of India.
43322 (by 84 2000) 163181(b 184 y 2000) 870161 53 (by 2000) 757377 273 1652161 1071 National Health Policy, 2002,
There exists a clean slow down in the health infrastructure and men power in the 8111 period as compared to the earlier 51-81 period. The rate of growth of medical colleges in the country has slowed by about half. Similar is the situation for hospitals and dispensaries. Extreme slow growth is recorded in the availability of bed and doctors. The only satisfaction is with regard to availability of nurses which has identical growth over he two periods. Table -4: Trend of Health Indicators in India Indicator 1951 1981 % change 2011 or the % change latest situation 63.5 116
Life Expectancy at 32.1 54.4 169 birth Birth Rate (1000) 39.9 33.9 85 22.5 66 Death Rate (do) 27.4 12.5 46 7.3 58 IMR (1000) 146 110 75 50 45 Source: Economic Survey, 1994-95 & 2010-11 and National Health Policy, 2002, Government of India.
The health indicators for the country over the two periods has shown mixed result. The rise in life expectancy at birth has improved in lesser percentage in the second period over he first period. The decline in birth rate and in IMR is however very significant I the 81-11 period. The IMR fall appears to be very sharp. The fall in birth rate has almost remained constant. Some of the improvement in the indicators are the result of general improvement in awareness and spread of education of the country .
InterState Variation in Health Services:
Availability of health services across the states in India vary widely. This need to be recognized at the national level and suitable programmes are required to be formulated to ensure access to quality health service to all people without any discrimination. Speedy growth of private health service providers and lagging response of the government system resulted in right to live being monopolized by the rich people. Treatment of diseases like Cancer, CVD, AIDS involve huge expenses without any assurance about the patients survival. The incidence of some of diseases is highly localized and need immediate attention. Table -5 below gives the regional variation in the status of health indicators among the states in India. Table-5:Inter-State Variation in Health Indicators in India Sl.No State Life Expectancy birth 2002-06 at IMR 2009 Birth Rate 2009 18.3 23.6 28.5 25.7 22.3 22.7 17.2 25.6 19.5 14.7 27.7 17.6 21.0 17.0 27.2 16.3 28.7 19.7 17.2 22.5 Death Rate 2009 7.6 8.4 7.0 8.1 6.9 6.6 7.2 7.0 7.2 6.8 8.5 6.7 8.8 7.0 6.6 7.6 8.2 6.5 6.2 7.3
1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18. 19 20
Male Female Andhra Pradesh 62.9 65.5 49 Assam 58.6 59.3 61 Bihar 62.2 60.4 52 Chhattisgarh --54 Gujarat 62.9 65.2 48.0 Haryana 65.9 66.3 51.0 HP 66.5 87.3 45.0 Jharkhand --44.0 Karnataka 63.6 67.1 41.0 Kerala 71.4 76.3 12.0 MP 58.1 57.9 67.0 Maharashtra 66 68.4 31.0 Orissa 59.5 59.6 65.0 Punjab 68.4 70.4 38.0 Rajasthan 61.5 62.3 59.0 Tamilnadu 65.0 67.4 28.0 UP 60.3 59.5 63.0 Uttarakhand --41.0 WB 64.1 65.8 33.0 All India 62.6 64.2 50.0 Source: Economic Survey, Government of India, 2009-10
The table clearly indicates wide variation in the health statistics across states in India. While Kerala is the best performer state in most of the indicators, the least performer states are M.P, Orissa and West Bengal. This is probably due to poor health infrastructure in these states.
The chart clearly reveals least fluctuation in case of DR (Death Rate) and wide fluctuation in case of FLE (Female Life Expectancy)
Health Indicators and Development Status of States:
The health condition of the people of a state greatly influences the working and earning capability of the population and hence the gross domestic product. In this section , there is an attempt to link up health variable across states and the GSDP and PCI of the states for a particular year. The information relates to major 15 states of the country. The health variables identified for the purpose are the Life expectancy at birth and the Infant Mortality rate (0-5 Years ). Both these variables taken together reflects the availability of public health service in an economy and the general health condition of the population The impact of these variables on the GSDP and PCI of the states is examined through fitting a linear multiple regression model.There are two models assumed for the purpose. One is the dependency of GSDP (X 1) on Infant Mortality Rate(X2) and Life Expectancy (X3). In the second model, the Per Capita Income (X4) is substituted for GSDP keeping the other two independent variables as such. The regression results are presented in the table given below.
Table 10: Relationship between Health Indicators and GSDP and PCI of 15 Major States in India
Name States
the Life Expectancy at Birth (avg of male and female ) Andhra Pradesh 66 Assam 60 Bihar 65 Gujarat 67 Haryana 67 Karnataka 67 Kerala 74 Madhya Pradesh 61 Maharastra 68 Odisha 61 Punjab 69 Rajastan 66 Tamil Nadu 68 Uttar Pradesh 62 W. Bengal 68
of
Infant Mortality Rate 52 64 56 50 54 45 12 70 33 69 41 63 31 67 35
GSDP in Current Per Capita Prices (in 000 Income (in crores ) 2008-9 rupees) 377 79 143 337 183 271 190 172 693 143 166 202 339 412 354 40902 23993 13663 49251 68914 41513 49316 21648 54867 30121 52879 27001 45058 18710 36322
Source ; Economic Survey, Government of Odisha, 2010-11, Planning and co-ordination Department , Bhubaneswar.
Model-1: X1 = b0 + b1 X2 +b2 X3 + U
R2 = .134 Items Estimated Value se t-value p-value b0
1524.450
b1
-14.467
b2
-6.062
2104.346 .724 .483
27.657 -.523 .610
6.126 -.990 .342
In Model-1, with 14 degrees of freedom, the theoretical value of t is higher than the calculated value of t and thus we have to accept the null hypothesis that there is no relationship between the independent and the dependent variable. This is applicable for both the independent variables. However , the low value of R2 indicates the inadequacy of the independent variables. Model-2: X4 = b0 + b1 X2 +b2 X3 + U
R2 = .316 Items Estimated Value se t-value p-value b0
175677.21
b1
3174.666
b2
93.763
170841.972 -1.028
2245.326 1.414
497.335
.189 .854
.324
.183
In Model-2 also, the situation is similar. The value of R2 is however slightly more here. This means the growth of GSDP and PCI has not been influenced by the health indicator variables across the states in India. Health Situation in Selected States The working of health sector in selected states is carried out in this section. Information for Orissa, and Gujarat is taken for this purpose. The health services improvement greatly depends on the role of the centre as most of the schemes belong to CSP and CP category. The states role is to implement the schemes in the best possible manner. The analysis of the state specific situation gives rise to a finding that plan expenditure in health sector was very less in the earlier years and is rising in the recent years but it is still about one third of the total expenditure. Table-6 gives this situation. Table-6: Pattern of Health Expenditure in Selected States (Rs. In Crores) Year 2004-05 Orissa Plan Exp 271 Total Exp 633 % 43 Gujarat Plan Exp
348
Total Exp
899
%
38.8
2005-06 2006-07 2007-08 2008-09 2009-10 2010-11
34 114 211 234 304 512
467 588 712 895 1128 1533
7 19 30 26 27 34
289 376 320 404 476 700
989 1145 1250 1376 1662 2330
29.2 32.8 25.6 29.4 28.7 30.1
Source:1. Budget at a Glance 2011-12, Finance Department , Government of Orissa. 2. State Finances in India ,RBI, Mumbai.(for different years) In case of Orissa the plan expenditure is around 30 percent of the total expenditure. It was a single digit figure for 05-06.This much of plan expenditure is against substantial vacancy in the non-plan posts of the state health care services. If all the posts in the health sector are filled up, then this much plan expenditure may not be possible given the total expenditure on health. For Gujarat also , the situation is not much different . The highest plan expenditure is recorded for 2004-05 about 38 percent. Thereafter it hoovers around 30 percent only. The vacancy position of manpower in the health sector is given in Table -7 in the two states. Table-7: Health Manpower Position in the Selected States Orissa Gujarat 1 Man in Vacanc Total Man in Vacancy Position y Position Grade-A 4082 943 5025 1039 448 Grade-B 4620 634 5254 404 74 Grade-C 21936 976 22912 1203 1352 Grade-D 13679 2119 15797 2775 863 Total 44316 4672 48988 5421 2737 Casual 223 106 329 G.Total 4539 4478 49317 Sources: Budget documents of the respective states. relates to only medical education wing of the health sector Grade Total 1487 478 2555 3638 8158
The table reflects that in Orissa a Group-A health worker (who is normally a doctor or a specialist) serves about 10,000 population, whereas, the national doctor population ratio is only 1:1600. The vacancy position in Gujarat appears to be more worse than Orissa. Taking, the all India figure, it can be concluded that due to this acute shortage of health manpower, the general population are depending more on pharmacists, nurses, medical sub-staffs and quacks which leads to high mortality rate in all cases.
Agenda for the 12th Plan:
The healthcare activities of the 12th plan must emphasise on two important points. One is the improvement in the quality of health service provided by the public sector which must be at par with the private sector. The second is as there are lot of health service providers in the private sector (a report puts it at 70 percent of the total), there must be a health service provider regulator to oversee the functioning of theses agencies. Health cannot be allowed to be traded like any other private goods. Denying the health service to a person because he is born in a rural dalit family tantamount to gross violation of human rights. The public sector health service must emphasise on the following points in the 12th plan Realistic Targets: The targets set by the 10th and 11th plan appear to be highly unrealistic which is difficult to realize. Setting a high target requires significant alteration in budgetary allocation to health sector. Further, it is noticed that the government is only targeting the health outcomes but not the health infrastructure. Targeting a SC in every village, a PHC in every panchayat, a CHC in every block a 300 bedded hospital in each sub-division and a 500 bedded hospital in each district will give the health outcomes automatically. Most of the institutions up to the block level may be required to function round the clock. The manpower requirements of all these institutions are carried out seriously and institutions be established to generate these man powers within a specific time frame of five years. Imposition of Health Cess: Provisioning the health institutions as mentioned in the earlier point requires huge public expenditure. The number of institutions producing doctors, nurses and other health workers need to be increased substantially. The present health budget or the normal rise of around 10 percent may not achieve this desired goal. For this purpose, it is suggested that the government must go for a health cess of around 5 percent on income tax which will generate about Rs.20, 000 crores per annum. This is required to be exclusively spent on strengthening of health education institutions in the country as a CS Scheme. States with deficient medical education institutions may be supported fully for building and equipment for new medical colleges. In case of Orissa, it is required to go for 2/3 new medical colleges in the 12th plan in the government sector. It can not be left to the private sector, as the doctors coming out of such institutions may not be interested to serve in tribal and rural area. Redesigning NRHM: The scope of NRHM has to be broadened to include general health conditions of the people. Like IMR and MMR the life expectancy of the population shall be taken as an important objective and a targeted variable. Problems of the senior citizens is required to be looked after more seriously as the joint family system has crippled due to the influence of western civilization. Orphans, destitutes and disabled persons may be allowed to live with dignity with
full support of the government rather than begging here and there. Elimination of begging should be one of the goals of the 12th plan health policy. Cost of Health Care: In rural areas there exists a fear for allopathic treatment due to high cost involved in it. Normally, in the first few days of illness, people go to unscientific treatment practices like witchcraft which still exists in rural areas. The high cost of allopathic treatment can be brought down if proper regulatory mechanism of the government is in place. There exists a huge gap between cost of pathological tests and the price charged to the patients. A uniform and standard price of all types of tests be determined by the government and made mandatory for the diagnostic laboratories to display it for public knowledge. Similarly, the prices of the drugs manufactured by the pharmaceutical companies need to be regulated. The BPL families may be allowed to get their costs reimbursed by the government for pathological tests and medicines. Backward Districts Health Development Scheme: It is noticed that there exists wide variation in the health services not only among states, but also among districts and blocks of a state. To reduce this disparity, there must be a separate central sector scheme to improve health infrastructure in those areas. For round the clock stay of all personnel in the PHC or SC , it is necessary that the place must have good quality schools, piped water supply, easy transport facility and communication network. There must a conscious effort to create all these within a specified period of time. Provision of Ambulance Facilities: Health problems normally require immediate attention. Every minute in such a situation matters for the patients survival. The government has to ensure availability of ambulance facilities within a distance of 5-10 kms. For this an ambulance network can be created like fire control network. It must be available round the clock. Water Supply and Sanitation: Awareness of general hygiene and clean drinking water supply are the two complementary areas which cannot be ignored when one is interested in good health. The government is progressing very slowly in these two areas. The achievement, the government is claiming appears to be far from truth. Government organizations are submitting inaccurate data on these services. Independent agencies may be requested to carry out small surveys to know the exact situation. Greater role of PRIs and ULBs: To get better results, the GPs be given power to monitor the performance of SCs and the blocks will look after PHCs and CHCs. All other hospitals will be kept under the charge of health department officials. Health Insurance Coverage : Health insurance coverage of the general population is probably a low priority area for the government of India. The GOI is more particular about its own employees and covers them under a CGH coverage scheme. The 11th plan tried to put the onus of this on the private providers which
will not work as it is not a high profit yielding area. Given the experience of the 11th plan , the 12th plan should focus this area more intensively and by 2017 each and every household in the country must have to be covered under a health insurance scheme. The premium of such a scheme must be as low as possible for the informal sector and to be totally borne by the government for BPL category population. Facility for Poor in Private Hospitals : The private sector health providers are using much of the common property resources and they have a social responsibility to discharge. Even though it is mandatory to give their facility to the poor people at subsidized rates , they are not doing that due to inadequate vigilance by the government. The 12th plan is required to redesign this arrangement for grater benefit of the common people. The Andhra Pradesh model can be followed in reimbursing the cost of poor people for treatment in these hospitals. Nutritional improvement of Mothers and Children: Underweight children and mothers are a very common scene in rural areas. This is the prime cause of infant and maternal mortality. Provision of nutritional food is not possible for these families due to their abject poverty. The government is satisfied by only providing rice at a subsidized rate. Other food items like dal, milk etc are equally important for health living. These items are required to be made available at a subsidized rate in the rural areas. Immunisation of children: Regular vaccination of the children in the age group of 0-5 is very important for preventing many diseases. The availability of such vaccination shall be made in each villages under a central scheme. Provision of a refrigerator and other instruments are to be made to such centres.
References: 1. World Bank (2006):India Inclusive Growth and Service delivery: Building on Indias Success Development Policy Review 2. World Bank (2006); World Development Report-2006 Equity and Development; Oxford
University Press.
3. Planning commission (2006) Towards Faster and More Inclusive Growth: An Approach to the 11th five Year Plan. New Delhi 4. Parliamentarians Forum on Economic Policy Issues (PAR-FORE)(2009) : Social Sector Budgeting: Higher Allocations Mask Poor Utilisation from website 5. Price Waterhouse coopers (2007): Healthcare in India Emerging Market Report 6. Government of India., Economic Survey Different years. , Ministry of Finance , New Delhi. 7. Jos Manuel Roche (2009): Capability and Group Inequalities: Revealing the latent structure Working paper, revised by October 2009 8. Ministry of Finance Department of Economic Affairs (1990-2008), Indian Public Finance Statistics, Economic Division, Government of India.
9. Planning and Coordination Department (1981 - 2012), Five Year Plans, Government of Odisha. 10. Sen, Amartya (2001) Development as Freedom, Oxford: Oxford University Press.
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- JCIPDokument5 SeitenJCIPdinesh.nayak.bbsrNoch keine Bewertungen
- Shift in Business Strategy of 10 Minute School - B2B To B2CDokument40 SeitenShift in Business Strategy of 10 Minute School - B2B To B2CSadiaNoch keine Bewertungen
- CL200 PLCDokument158 SeitenCL200 PLCJavierRuizThorrensNoch keine Bewertungen
- EmployWise JAVA ASSIGNMENTDokument2 SeitenEmployWise JAVA ASSIGNMENTPreet PatelNoch keine Bewertungen
- USDA List of Active Licensees and RegistrantsDokument972 SeitenUSDA List of Active Licensees and Registrantswamu885Noch keine Bewertungen
- Advanced Physiotherapeutic SyllabusDokument1 SeiteAdvanced Physiotherapeutic SyllabusAnup SharmaNoch keine Bewertungen
- Rab Sikda Optima 2016Dokument20 SeitenRab Sikda Optima 2016Julius Chatry UniwalyNoch keine Bewertungen
- Nature of Science-Worksheet - The Amoeba Sisters HWDokument2 SeitenNature of Science-Worksheet - The Amoeba Sisters HWTiara Daniel25% (4)
- Catalogue of Archaeological Finds FromDokument67 SeitenCatalogue of Archaeological Finds FromAdrinaNoch keine Bewertungen
- BA 4722 Marketing Strategy SyllabusDokument6 SeitenBA 4722 Marketing Strategy SyllabusSri GunawanNoch keine Bewertungen
- 13507Dokument5 Seiten13507Abinash Kumar0% (1)
- 2 - Sample Kids Can Read and Write 2 and 3 Letter Words - Step 2 Final Downloadable Version For Website PDFDokument18 Seiten2 - Sample Kids Can Read and Write 2 and 3 Letter Words - Step 2 Final Downloadable Version For Website PDFsantoshiNoch keine Bewertungen
- Uts Cmo Module 5Dokument31 SeitenUts Cmo Module 5Ceelinah EsparazNoch keine Bewertungen
- BluePrint & High Pressure Pascalization (HPP)Dokument3 SeitenBluePrint & High Pressure Pascalization (HPP)Prof C.S.PurushothamanNoch keine Bewertungen
- Slides - SARSDokument191 SeitenSlides - SARSCedric PoolNoch keine Bewertungen
- Generator ControllerDokument21 SeitenGenerator ControllerBrianHazeNoch keine Bewertungen
- CUET 2022 General Test 6th October Shift 1Dokument23 SeitenCUET 2022 General Test 6th October Shift 1Dhruv BhardwajNoch keine Bewertungen
- O'Dell v. Medallia, Inc. Et Al, 1 - 21-cv-07475, No. 1 (S.D.N.Y. Sep. 7, 2021)Dokument15 SeitenO'Dell v. Medallia, Inc. Et Al, 1 - 21-cv-07475, No. 1 (S.D.N.Y. Sep. 7, 2021)yehuditgoldbergNoch keine Bewertungen
- Saif Powertec Limited Project "Standard Operating Process" As-Is DocumentDokument7 SeitenSaif Powertec Limited Project "Standard Operating Process" As-Is DocumentAbhishekChowdhuryNoch keine Bewertungen
- Reproduction in PlantsDokument12 SeitenReproduction in PlantsAnand Philip PrasadNoch keine Bewertungen
- Ransomware: Prevention and Response ChecklistDokument5 SeitenRansomware: Prevention and Response Checklistcapodelcapo100% (1)
- Grasa LO 915Dokument2 SeitenGrasa LO 915Angelo Carrillo VelozoNoch keine Bewertungen
- Epistemology and OntologyDokument6 SeitenEpistemology and OntologyPriyankaNoch keine Bewertungen
- Rubber Band Arrangements - Concert BandDokument25 SeitenRubber Band Arrangements - Concert BandJonatas Souza100% (1)
- Ose Sample QuotationDokument37 SeitenOse Sample Quotationrj medelNoch keine Bewertungen
- Jones Et - Al.1994Dokument6 SeitenJones Et - Al.1994Sukanya MajumderNoch keine Bewertungen
- Jota - EtchDokument3 SeitenJota - EtchRidwan BaharumNoch keine Bewertungen
- Case Study On Goodearth Financial Services LTDDokument15 SeitenCase Study On Goodearth Financial Services LTDEkta Luciferisious Sharma0% (1)
- SAP HR - Legacy System Migration Workbench (LSMW)Dokument5 SeitenSAP HR - Legacy System Migration Workbench (LSMW)Bharathk KldNoch keine Bewertungen
- Ankle Injury EvaluationDokument7 SeitenAnkle Injury EvaluationManiDeep ReddyNoch keine Bewertungen