Beruflich Dokumente
Kultur Dokumente
ACE Inhibitors & Angiotensin II Antagonists: October 1997
Hochgeladen von
indee533Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
ACE Inhibitors & Angiotensin II Antagonists: October 1997
Hochgeladen von
indee533Copyright:
Verfügbare Formate
ACE Inhibitors & Angiotensin II Antagonists
October 1997 ii
Highlights
ACE Inhibitors (ACEIs) are considered second line agents to thiazide diuretics and -blockers in patients with uncomplicated hypertension. They may be preferred in patients with coexisting CHF or diabetes. ACEIs have similar efficacy and side effect profiles. Low initial dosages should be chosen in patients at high risk for hypotension. Lisinopril has the advantage of low cost, od dosing, mortality data in CHF, & a favorable peak/trough ratio. Losartan (Cozaar) may be an alternative in patients with hypertension who do not tolerate ACEIs. The past decade has seen a dramatic increase in cardiovascular agents and available dosage forms. This edition of The Rx Files will evaluate and compare the angiotensin converting enzyme inhibitors (ACEIs) and the angiotensin II (AII) receptor antagonists.
because long term trials have shown reductions in mortality. Until more is known about ACEI effect on morbidity and mortality, they remain second line therapy, except in patients where thiazides or -blockers are contraindicated or not tolerated.2 ,34 ACEIs may be preferred as first line antihypertensives in patients with diabetes or CHF.2 Agents that can be given once daily may improve patient compliance. To be suitable for once daily dosing, the FDA suggests an antihypertensives trough effect should be 50 % of the peak effect.3 Compared to other ACEIs, enalapril (Vasotec) and lisinopril may offer better 24h BP control with once daily dosing due to minimal fluctuation between peak and trough effect3.
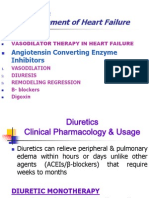
Congestive Heart Failure
ACEIs are effective in the treatment of patients with heart failure (HF) and have been shown to significantly reduce morbidity and mortality.4 ,5,6,7,8,9 ACEI therapy reduces both symptoms and hospitalizations due to HF.10,11 Long term benefits appear greater in patients with low ejection fractions. Captopril, enalapril, lisinopril and ramipril (Altace) have shown decreased mortality in studies, although the effect is thought to be a class effect.12 The optimal dosing of ACEIs in HF is unknown. Lower dosages are effective in improving symptoms and exercise performance. However, major clinical trials showing reductions in mortality have used somewhat larger target doses (See ACEI Comparison Chart: dosage range*). Slow titration up to the target dose is recommended to reduce side effects. Initial dosages (po) used in studies included enalapril 5mg bid, captopril 12.5mg tid, lisinopril 5mg od, and ramipril 2.5mg bid.4,6,9,10,13,14,15 Patients at high risk for hypotension were started at half the usual initial dose and titrated as tolerated. ACEI therapy following MI has been shown to reduce progression to symptomatic heart failure and improve survival, especially when initiated within 24 hours.13,14,15
Pharmacokinetics
All ACEIs are active when taken orally. With the exception of captopril (Capoten) and lisinopril (Prinivil/Zestril), the majority are prodrugs that are converted in the liver to their active metabolites. Captopril has a rapid onset of <1 hr but a short duration that necessitates BID-TID dosing. Lisinopril and the prodrugs have a slower onset (1-2hr) but generally a 24h duration of action so most can be given once daily; some patients may require BID dosing if the desired effect diminishes significantly towards the end of the dosing interval. ACEIs are excreted in whole or in part by the kidney and all but fosinopril (Monopril) require dose reduction in renal impairment.
Hypertension
At equipotent doses, the ACEIs are similar in efficacy and safety. When used alone, ACEIs will control BP in approximately 50% of patients1; black patients and those with low renin concentrations may not respond as well. Combination therapy with a thiazide diuretic or calcium channel blocker will control BP in an additional 30% of patients.1 In uncomplicated patients, thiazides and blockers are still considered first line antihypertensives
One conflicting study which used enalaprilat IV showed a trend towards harm, possibly due to overly aggressive administration and secondary hypotension.16,33 Caution should be taken to avoid excessive hypotension. Current literature supports the use of ACEIs for 4-6 weeks postMI in all patients who are clinically stable and do not have major contraindications to ACEIs (Table 2).16 Patients with left ventricular dysfunction (ejection fraction of <35-40%) would benefit from longer term treatment.16
responsible is likely related to ACE inhibition of bradykinin catabolism. Symptoms appear within days to weeks after starting ACEI therapy; resolution usually occurs within days of stopping the offending agent but may take up to 4 weeks.24 Severity of symptoms can sometimes be minimized with a reduction in dose. Successful changes to alternate ACEIs may be due in part to differences in dosages, rather than in the drugs themselves.24 If patients find the cough intolerable, discontinuing the drug is often the only suc-cessful option. Switching to losartan may be effective.
Diabetic Nephropathy
ACEIs are beneficial in preventing renal complications secondary to diabetes.17 They reduce proteinuria and slow the progression of nephropathy in IDDM.17,18 Some studies also show benefit in NIDDM. Beneficial effects are seen both in hypertensive and normotensive patients suggesting that some of their effects are independent of their antihypertensive effects. ACEIs also delay the development of nephropathy in diabetics with microalbuminuria.19,20,21 These appear to be a class effects.
Angiotensin II Antagonists
Recent research focusing on more selective modulation of the renin-angiotensin system (RAS) has resulted in the development of losartan (Cozaar), the first of the angiotensin II (AII) receptor antagonists. Losartan specifically inhibits angiotensin II at the tissue level. Unlike ACEIs, losartan has no effect on the kallikreinkinin system so safety and tolerability are likely to be improved if bradykinin related side effects such as cough can be avoided.25 In comparative clinical trials, losartan demonstrated similar efficacy in hypertension to ACEIs. Losartan has also shown a decrease in mortality in CHF and further studies are currently in progress.25, 26, 33 Currently losartan is only approved for treatment of hypertension, and until more is known about its overall effect on morbidity and mortality, it is considered a second line agent. Like the ACEIs, it is reserved for patients in whom thiazides or -blockers are ineffective, contraindicated, or poorly tolerated.27 An initial dose of 25mg daily can be used in elderly or volume depleted patients while 50mg daily will control BP in most individuals. Increasing the dose does not appear to significantly improve efficacy although some patients may require up to 100mg per day. Maximum BP lowering may take up to 6 weeks, therefore one should allow adequate time before increasing the dose.25,27 The most common side effects (incidence >1%) seen with losartan include headache, dizziness, and fatigue. In clinical trials only dizziness occurred more frequently than with placebo.28 In comparative trials, losartan had similar efficacy to other antihypertensives but caused less fatigue than -blockers, less edema than calcium channel blockers, and less cough than ACEIs.29 Compared with ACEIs, first dose hypotension is not as problematic with losartan probably due to more gradual generation of its active metabolite and lack of effect on bradykinin.28 Hyperkalemia can occur but is less likely due to losartans reduced effect on aldosterone.30 Losartan does cause an increase in circulating angiotensin II but it is unknown if this causes any long term side effects.28
References available on request
Pregnancy/Pediatric Considerations
ACEIs are contraindicated in pregnancy and should be avoided. ACEIs are not officially approved for the pediatric age group. There is limited clinical experience with captopril in children but its use should be under the recommendation and supervision of a specialist.
Adverse Effects
ACEIs are generally well tolerated. Side effects are summarized in Table 3. Hyperkalemia is often associated with diminished renal function and/or concurrent use of potassium(K+) sparing diuretics, K+ supplements, or salt substitutes. Serum K+ should be monitored in these patients and drugs that increase serum K+ reduced or discontinued as necessary. Acute renal failure may occur especially in patients with bilateral renal stenosis or severe nephrosclerosis. Angioedema has been reported but is a rare, although potentially fatal reaction.22 All ACEIs should be avoided if this occurs. Hypotensive reactions may occur after the first dose of an ACEI. In some cases hypotension can be severe. Time course and duration depend on the drugs kinetics and metabolism; both onset and resolution are more rapid with captopril than the longer acting ACEIs. Risk factors include CHF, volume depletion due to Na+ restriction, diuretic use, nephrotic syndrome, hemodialysis and hepatic disease. Stopping diuretics 24h prior to the first ACEI dose (given at hs) is recommended. Initial doses should be low and titrated upwards as tolerated.22 Dry, non-productive cough is now recognized as a frequent, bothersome side effect of ACEIs and is the most common reason for discontinuation. Incidence is conservatively estimated at 10%.23 The mechanism
The Rx Files: ACE Inhibitors / Angiotensin II Antagonists Supplementary Tables
Table 1 Major Drug Interactions
Lithium levels can increase 3-4X after 2-4 days of ACEI initiation reduce lithium dose and monitor lithium levels Potassium Supplements, Potassium Sparing Diuretics potassium retention, potential severe hyperkalemia Diuretics Increased risk of first-dose hypotension if hypovolemic NSAIDs sodium and water retention, decreased effect of ACEI, and increased risk of nephrotoxicity
Table 2 Contraindications
Absolute pregnancy history of angioedema or hypersensitivity to ACEIs bilateral renal artery stenosis (RAS) or RAS of a solitary kidney history of intolerance to ACEIs due to hypotension severe hyperkalemia Relative hypotension (SBP < 90mm) renal dysfunction hyperkalemia cough
Table 3 Adverse Effects
symptomatic hypotension dizziness, fatigue, headache dry, non-productive cough (>10%) angioedema - rare but serious side effect (~0.1%) hyperkalemia (with drug interactions/renal insufficiency) taste disturbance - more common with captopril (2%) rash - more common with captopril (4-7%) acute renal failure in patients with renal artery stenosis or severe nephrosclerosis bone marrow suppression: neutropenia, thrombocytopenia, aplastic anemia, pancytopenia; extremely rare, but patients with renal failure or collagen vascular disease are at increased risk. nephrotic syndrome - rare but has been seen with high dose captopril >150mg/day
Table 4 ACEI Induced Cough24
Treatment Options * Discontinue ACEI and use alternate agent(s) Reduce dosage Use alternate ACEI Sodium cromoglycate (Intal) Comments
Easiest in hypertension because many treatment options; more difficult in CHF or nephropathy. Some success with switch to losartan (Cozaar). Not always possible or effective. May decrease severity but not occurrence. Minimal success due to high crossreactivity. Some reports suggest fosinopril best alternative.31 Has shown some efficacy, and reasonably well tolerated. May induce bronchospasm.
Table 5 Comparative Cost For 30 Days Treatment With Commonly Used Antihypertensives
hydrochlorothiazide 12.5-25mg po daily atenolol 50mg po daily acebutolol 200mg po bid lisinopril 10mg po daily enalapril 10mg po daily enalapril 5mg po bid felodipine 10mg po daily diltiazem CD 180mg po daily $ 8.00 $ 20.00 $ 25.00 $ 36.00 $ 42.00 $ 64.00 $ 43.00 $ 50.00
Baclofen, NSAIDs, theophylline, nifedipine, & bupivacaine have also been tried but are not generally recommended.
* based on case reports and small trials
We wish to acknowledge those who have assisted in the development and review of this newsletter: Dr. Z. Tymchak (FM), Dr. M. Jutras (FM), Dr. J. Akhtar (Cardiol.), Dr. R. Herman (Pharmacol.), Barb Evans, BSP, MSc, and the CDUP Advisory Committee. Loren D. Regier BSP, BA Sharon L. Downey BSP
The Rx Files - October 1997
ACE Inhibitors & Angiotensin II Antagonists References:
Drugs and Therapeutics Bulletin. 1995;33(1) Jan 19:1-3. Ogilvie R, Burgess E, Cusson J. Report of the Canadian hypertension Society Consensus Conference: 3. Pharmacologic treatment of essential hypertension. Can Med Assoc J 1993;149(5):575-584. 3 Leonetti G and Cuspidi C. Choosing the Right ACE Inhibitor. Drugs 1995;49(4) 516-535. 4 Consensus Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. N Engl J Med. 1987; 316:1429-35. 5 Kjekshus J, Swedberg K, Snapinn S. Effects of enalapril on long term mortality in severe congestive heart failure. Am J Cardiol. 1992; 69:103-7. 6 Cohn JN, Archibald DG, Ziesche S et al. Effect of vasodilator therapy on mortality in chronic congestive heart failure: results of a Veterans Administration Cooperative Study. N Engl J Med. 1986;314:1547-52. 7 Cohn JN, Archibald DG, Ziesche S et al. A comparison of enalapril with hydralazine-isosorbide dinitrate in the treatment of chronic congestive heart failure. N Engl J Med. 1991; 325:303-10. 8 Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293-302. 9 Ball SG, Cowan JC, Winter C. Effect of ramipril on mortality and morbidity of survivors of acute myocardial infarction with clinical evidence of heart failure. Lancet 1993;342:821-8. 10 SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive herat failure. N Engl J Med. 1991; 325:293-302. 11 Coats AJS. Therapeutic interventions to reduce rates of hospitalization and death in patients with heart failure: new clinical evidence. Cardiology 1992;81:1-7. 12 ASHP Therapeutic Guidelines on Angiotensin-Converting-Enzyme Inhibitors in Patients with Left Ventricular Dysfunction. Am J Health-Syst Pharm. 1997;54:299-313. 13 Pfeffer MA, Braunwald E, Moye LA et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction: results of the Survival and Ventricular Enlargement Trial. N Engl J Med. 1992;327:669-77. 14 Gruppo Italiano per 934-6043 Studio della Sopravvivenza nellInfarto Miocardico. GISSI-3: effects of lisinopril and transdermal glyceryl trinitrate singly and together on 6 week mortality and ventricular function after acute myocardial infarction. Lancet 1994; 343:1115-22. 15 SOLVD Investigators. Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med. 1992;327:685-91. 16 Huckell VF,Bernstein V, Crowell R. Angiotensin-converting enzyme inhibition in myocardial infarction-Part 2: Clinical issues and controversies. Can J Cardiol. 1997;13(2):173-182. 17 Tsuneharo B, Neugebauer S, Watanabe T. Diabetic Nephropathy: Its relationship to hypertension and means of pharmacological intervention. Drugs 1997;54(2):198-234. 18 Lewis E, Lawrence G, Raymond P, et al. The effect of angiotensin-converting enzyme inhibition on diabetic nephropathy. N Eng J Med. 1993; 329(20):1456-1461. 19 Mathiesen ER, Hommel E, Smith U, et al. Efficacy of captopril in normotensive diabetic patients with microalbuminuria: 8 years of follow up[Abstract]. Diabetologia 1995; 38 Suppl. 1:A46. 20 Microalbuminuria Captopril Study Group. Captopril reduces the risk of nephropathy in IDDM patients with microalbuminuria. Diabetologia 1996;39:587-93. 21 Marre M, Leblanc H, Suarez L, et al. Converting enzyme inhibition and kidney function in normotensive diabetic patients with persistent microalbuminuria. BMJ 1987; 294:1448-52. 22 AHFS. Drug Information. ASHP, Inc. 1997:1221-23. 23 Fletcher A, Palmer A, Bulpitt C. Cough with ACEIs;how much of a problem? J of Hyperten. 1994;12(suppl 2):543-7. 24 Keisman M, Evans B, and Semchuk W. Etiology and treatment of ACEI-induced cough. Can J Hosp Pharm. 1995;48:25-36. 25 Schaefer K and Porter J. Angiotensin II receptor antagonists; the prototype losartan. Ann Pharmacother. 1996;30:625-36. 26 Kang P et al. Angiotensin II receptor antagonists; a new approach to blockade of the RAS. Am Heart J. 1994; 127:1388-401. 27 Adis International. Losartan; low incidence of cough confirmed. Drugs and Therapy Perspectives. 1996; 8(6):1-5. 28 Goldberg A and Sweet C. Efficacy and safety of losartan. Can J Cardiol. 1995;11(suppl F):27F-31F. 29 Goldberg A, Dunlay M and Sweet C. Safety and tolerability of losartan compared with hydrochlorothiazide, atenolol, felodipine ER, and ACEIs for treatment of systemic hypertension. Am J Cardiol. 1995;75:793-5. 30 Burnier M, Waeber B, Brunner H. The advantages of angiotensin II antagonism. J of Hypertens. 1994;12(suppl 2):S7-15. 31 Germino FW et al. Evaluation of the cough profile of fosinopril in hypertensive patients with ACEI associated cough- a pilot study. Curr Ther Res. 1993;54:469. 32 Swedberg K, Held P, Kjekshus J, et al. Effects of the early administration of enalapril on mortality in patients with acute myocardial infarction. Results of the Cooperative New Scandinavian Enalapril Survival Study II (CONSENSUS II). N Engl J Med. 1992;327(10):67884. 33 Pitt B, Segal R, Martinez F. Randomised trial of losartan verses captopril in patients over 65: Evaluation of Losartan in the Elderly Study (ELITE). Lancet 1997;349:747-52. 34 Saskatchewan Health-Formulary Committee Bulletin: Drug Treatment of Hypertension. 1995; January.
2 1
Das könnte Ihnen auch gefallen
- Cardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineVon EverandCardiovascular Endocrinology and Metabolism: Theory and Practice of Cardiometabolic MedicineAndrew J. KrentzNoch keine Bewertungen
- Angiotensin Converting Enzyme (ACE) InhibitorsDokument4 SeitenAngiotensin Converting Enzyme (ACE) InhibitorsPutri Mulia HasibuanNoch keine Bewertungen
- Inhibitors of AngiotensinDokument37 SeitenInhibitors of AngiotensinBoyu GrtrNoch keine Bewertungen
- ACE Inhibitors or ARBsDokument3 SeitenACE Inhibitors or ARBsJill QuilangNoch keine Bewertungen
- CVS (HF, HTN) PharmacologyDokument99 SeitenCVS (HF, HTN) PharmacologyCherenet TomaNoch keine Bewertungen
- HTN Treatment DR - VishvasDokument46 SeitenHTN Treatment DR - VishvasvishvasNoch keine Bewertungen
- Diuretic: 3. Calcium Channel BlockersDokument3 SeitenDiuretic: 3. Calcium Channel BlockersAniRafikaBullatzNoch keine Bewertungen
- Free Drug Bank GUIDE 1 PDFDokument76 SeitenFree Drug Bank GUIDE 1 PDFRaouf Ra'fat Soliman100% (11)
- Lecture 1 antihypertensionSDSDokument7 SeitenLecture 1 antihypertensionSDSSara AbbasNoch keine Bewertungen
- Angiotensin Receptor Blockers (ARBs) PDFDokument3 SeitenAngiotensin Receptor Blockers (ARBs) PDFpriya singhNoch keine Bewertungen
- Case Study Number 1Dokument5 SeitenCase Study Number 1Kevin Kyle RizarriNoch keine Bewertungen
- Anti Hypertensive Drugs - ACE InhibitorDokument16 SeitenAnti Hypertensive Drugs - ACE InhibitorApurba Sarker Apu100% (1)
- Skema HipertensiDokument4 SeitenSkema HipertensiAndri wijayaNoch keine Bewertungen
- Antihypertensive Drug - WikipediaDokument75 SeitenAntihypertensive Drug - WikipediaAngelo LagrimasNoch keine Bewertungen
- Antihypertensive DrugDokument7 SeitenAntihypertensive Drugaarti sahuNoch keine Bewertungen
- Renin-Angiotensin System Inhibition in The Treatment of HypertensionDokument14 SeitenRenin-Angiotensin System Inhibition in The Treatment of HypertensionBritneyNoch keine Bewertungen
- Name: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of SubmissionDokument10 SeitenName: Class: Department: Roll No.: Subject: Course Code: Cr. HR.: Submitted To: Date of SubmissionAnoosha FarooquiNoch keine Bewertungen
- FARMAKOGNOSI - Obat AntihipertensiDokument7 SeitenFARMAKOGNOSI - Obat AntihipertensiTrianisa FebyNoch keine Bewertungen
- ACE INHIBITORS & ARBsDokument31 SeitenACE INHIBITORS & ARBsMaria khurshidNoch keine Bewertungen
- Major Side Effects of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor BlockersDokument13 SeitenMajor Side Effects of Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor BlockersJulia PardiniNoch keine Bewertungen
- 8D - HypertensionDokument58 Seiten8D - Hypertensionmashe1Noch keine Bewertungen
- 'Heart Failure Treatment'': Name: Negin SoltaniDokument8 Seiten'Heart Failure Treatment'': Name: Negin SoltaniReyhane pashangNoch keine Bewertungen
- Which Diuretics For Which Patients With Hypertension?: Raghav Bansal - Sivasubramanian RamakrishnanDokument8 SeitenWhich Diuretics For Which Patients With Hypertension?: Raghav Bansal - Sivasubramanian RamakrishnanRajendra ChavanNoch keine Bewertungen
- 5 HypertensionDokument8 Seiten5 Hypertensioniraqeana100100Noch keine Bewertungen
- Management of Heart Failure: OutlineDokument27 SeitenManagement of Heart Failure: OutlineBoetik AlifiaNoch keine Bewertungen
- Case Challenge: Diagnosing and Managing CKD Comorbidities: Literature ReviewDokument8 SeitenCase Challenge: Diagnosing and Managing CKD Comorbidities: Literature ReviewPratik TripathiNoch keine Bewertungen
- Hypertension and KidneyDokument34 SeitenHypertension and KidneyanandababuNoch keine Bewertungen
- Ischemic Heart Diease PDFDokument33 SeitenIschemic Heart Diease PDFMahamed Wefkey OmranNoch keine Bewertungen
- Lipid Effects of Antihypertensive Medications: Nonstatin Drugs (W Borden, Section Editor)Dokument8 SeitenLipid Effects of Antihypertensive Medications: Nonstatin Drugs (W Borden, Section Editor)Septi Fadhilah SPNoch keine Bewertungen
- Chapter 17 Cardiovascular DrugsDokument35 SeitenChapter 17 Cardiovascular Drugsaisyahasrii_Noch keine Bewertungen
- Drug Bank GUIDE 1 PDFDokument76 SeitenDrug Bank GUIDE 1 PDFAdel Dib Al-jubehNoch keine Bewertungen
- Drugs Without Positive Inotropic Effect Used in HFDokument12 SeitenDrugs Without Positive Inotropic Effect Used in HFDana HamarshehNoch keine Bewertungen
- Nuove Prospettive Nel Trattamento Dello Scompenso Acuto: Congresso Regionale ANMCO Toscana, Viareggio, 7 OTTOBRE 2011Dokument35 SeitenNuove Prospettive Nel Trattamento Dello Scompenso Acuto: Congresso Regionale ANMCO Toscana, Viareggio, 7 OTTOBRE 2011Billy SNoch keine Bewertungen
- ACE Inhibitors PrintDokument5 SeitenACE Inhibitors PrintBernard TangNoch keine Bewertungen
- Jurnal 1Dokument17 SeitenJurnal 1convenienceNoch keine Bewertungen
- Pharmacology 3 - Management of Heart FailureDokument59 SeitenPharmacology 3 - Management of Heart Failurealbatros000Noch keine Bewertungen
- Antihypertensive AgentsDokument52 SeitenAntihypertensive Agentssameena ramzanNoch keine Bewertungen
- ACE InhibitorsDokument8 SeitenACE InhibitorshasaɴNoch keine Bewertungen
- NullDokument11 SeitenNullKareem SaeedNoch keine Bewertungen
- Acquired TTP - Clinical Manifestations and Diagnosis - UpToDateDokument16 SeitenAcquired TTP - Clinical Manifestations and Diagnosis - UpToDatepradeep danielNoch keine Bewertungen
- Treating Hypertension in Patients With Medical CondtionsDokument6 SeitenTreating Hypertension in Patients With Medical CondtionsSebastian ApeleoNoch keine Bewertungen
- Significant Early In-Hospital Benefit Was Seen. Clopidogrel Is Prefferd ToDokument8 SeitenSignificant Early In-Hospital Benefit Was Seen. Clopidogrel Is Prefferd TogilnifNoch keine Bewertungen
- DBP: Diastolic Blood Pressure SBP: Systolic Blood PressureDokument7 SeitenDBP: Diastolic Blood Pressure SBP: Systolic Blood PressureM. JoyceNoch keine Bewertungen
- Anti HypertensionDokument63 SeitenAnti HypertensionAngga CahyadiNoch keine Bewertungen
- Other Diuretics Final 2017Dokument4 SeitenOther Diuretics Final 2017Anonymous sSuBudwdNoch keine Bewertungen
- AntihipertensivosDokument20 SeitenAntihipertensivosFernando XavierNoch keine Bewertungen
- Ace InhibitoriDokument12 SeitenAce InhibitoriMedical StudentNoch keine Bewertungen
- Hypertension: 1-Hypertension Is Defined As (BP)Dokument37 SeitenHypertension: 1-Hypertension Is Defined As (BP)hussein alnasryNoch keine Bewertungen
- Historia Clinica Hta YachiDokument5 SeitenHistoria Clinica Hta YachiEdwin Marquez GuzmánNoch keine Bewertungen
- Cardiac DrugsDokument35 SeitenCardiac DrugsCristina Centurion100% (3)
- Heart FailureDokument6 SeitenHeart FailureNatasha MarksNoch keine Bewertungen
- Anti Hypertensive 20191211Dokument35 SeitenAnti Hypertensive 20191211helloitsmenadNoch keine Bewertungen
- Thiazide and Thiazide-Like DiureticsDokument3 SeitenThiazide and Thiazide-Like DiureticsYohanes SutrisnoNoch keine Bewertungen
- ACE Inhibitors and ARBsDokument20 SeitenACE Inhibitors and ARBsMylene MendozaNoch keine Bewertungen
- Delaying or Halting Progression of Chronic Kidney DiseaseDokument9 SeitenDelaying or Halting Progression of Chronic Kidney Diseasehannya manNoch keine Bewertungen
- Faculty of Physical TherapyDokument15 SeitenFaculty of Physical TherapyDr Abdallah BahaaNoch keine Bewertungen
- Cardio Lab MedsDokument11 SeitenCardio Lab MedsDianne Erika MeguinesNoch keine Bewertungen
- Cruz v. CA - G.R. No. 122445 - November 18, 1997 - DIGESTDokument2 SeitenCruz v. CA - G.R. No. 122445 - November 18, 1997 - DIGESTAaron Ariston80% (5)
- Colloidal Tin Injection - SPCDokument15 SeitenColloidal Tin Injection - SPCacbgdvNoch keine Bewertungen
- Skin Cancer SurgeryDokument2 SeitenSkin Cancer SurgeryContinuum Hospitals of New York100% (1)
- Pathophysiology Part 2Dokument1 SeitePathophysiology Part 2nicole alignoNoch keine Bewertungen
- Modified Fluid Wax Impression For A Severely Resorbed Edentulous Mandibular RidgeDokument4 SeitenModified Fluid Wax Impression For A Severely Resorbed Edentulous Mandibular RidgeChepe LemusNoch keine Bewertungen
- Integ 4 Answer PDFDokument12 SeitenInteg 4 Answer PDFRhasdie MandiNoch keine Bewertungen
- This Assessment Task Gives You The Opportunity To Critically Examine The Impact Professional Nursing Can Have On Individual NursesDokument8 SeitenThis Assessment Task Gives You The Opportunity To Critically Examine The Impact Professional Nursing Can Have On Individual NursesSarahJaneNoch keine Bewertungen
- Paediatric Examination Handbook 2015Dokument66 SeitenPaediatric Examination Handbook 2015Ulfa Rahmadanti SetiawanNoch keine Bewertungen
- Diana Driscoll Ehlers Danlos Syndrome Your Eyes PresentationDokument41 SeitenDiana Driscoll Ehlers Danlos Syndrome Your Eyes PresentationHanna King50% (2)
- Huntleigh BD4000 Fetal Monitor - User ManualDokument48 SeitenHuntleigh BD4000 Fetal Monitor - User ManualAtiqurrehman UmairNoch keine Bewertungen
- Hirschsprung DiseaseDokument25 SeitenHirschsprung DiseaseMuhammad Zaniar RamadhaniNoch keine Bewertungen
- New Claim Form TTK TPADokument2 SeitenNew Claim Form TTK TPAAbhijit SawantNoch keine Bewertungen
- Strattera PDFDokument5 SeitenStrattera PDFToronto StarNoch keine Bewertungen
- Labor and DeliveryDokument7 SeitenLabor and Deliveryplethoraldork100% (20)
- Electrolytes & FluidimbalancesDokument80 SeitenElectrolytes & FluidimbalancesDennis Nyambane MomanyiNoch keine Bewertungen
- The Evolution of Surgical TrainingDokument9 SeitenThe Evolution of Surgical Trainingapi-19500641Noch keine Bewertungen
- GoutDokument10 SeitenGoutAmberNoch keine Bewertungen
- A Case Study On Obstructive JaundiceDokument84 SeitenA Case Study On Obstructive JaundiceMonna Llee Monte DimarananNoch keine Bewertungen
- B. Within 24 Hours After DischargeDokument15 SeitenB. Within 24 Hours After DischargeRichard SonsingNoch keine Bewertungen
- NUR 204.intramuscular InjectionDokument65 SeitenNUR 204.intramuscular InjectionKouta SanNoch keine Bewertungen
- 5z23. ED Crowding Overview and Toolkit (Dec 2015)Dokument33 Seiten5z23. ED Crowding Overview and Toolkit (Dec 2015)Peter 'Pierre' RobsonNoch keine Bewertungen
- Establishing Priorities in The Supervision HourDokument7 SeitenEstablishing Priorities in The Supervision HourDianaSantiagoNoch keine Bewertungen
- Theory Analysis PaperDokument7 SeitenTheory Analysis PaperElite ScholarsNoch keine Bewertungen
- Operative Vaginal Delivery (Ovd)Dokument35 SeitenOperative Vaginal Delivery (Ovd)api-3705046Noch keine Bewertungen
- Instruction ManualBP380A PDFDokument11 SeitenInstruction ManualBP380A PDFVikas VermaNoch keine Bewertungen
- EE 302 Ethics ProjectDokument5 SeitenEE 302 Ethics Projecthockeymadano9Noch keine Bewertungen
- Organization of Tongue Movements Before and After Frenotomy For Posterior Tongue-Tie: An Ultrasound AnalysisDokument9 SeitenOrganization of Tongue Movements Before and After Frenotomy For Posterior Tongue-Tie: An Ultrasound AnalysisIka Ayu ParamitaNoch keine Bewertungen
- Trigger Point InjectionDokument10 SeitenTrigger Point Injectionv_vijayakanth7656Noch keine Bewertungen
- Miranda Gebell Letter of RecommendationDokument1 SeiteMiranda Gebell Letter of Recommendationapi-454489494Noch keine Bewertungen
- EMG Test Preparations: Patient InformationDokument2 SeitenEMG Test Preparations: Patient InformationShauki AliNoch keine Bewertungen