Beruflich Dokumente
Kultur Dokumente
MedStaff Sum 2011 EVANS
Hochgeladen von
davidjgoldbergOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
MedStaff Sum 2011 EVANS
Hochgeladen von
davidjgoldbergCopyright:
Verfügbare Formate
SUMMER 2011
FAULKNER HOSPITAL
NEWS
MEDICAL STAFF
NEWS FOR AND ABOUT FA U L K N E R H O S P I TA L P H Y S I C I A N S
Pain management at Faulkner Hospital
IN
THIS ISSUE
P3: Sagoff Centre celebrates 40th anniversary P4: Guidelines for teaching physicians, interns and residents P5: Health care unseen P8: Reducing risk during patient hand-off communication P11: New medical record documentation policy P12: Center for Robotic Surgery helps women with gynecological disorders P14: Partnering to reduce avoidable hospital readmissions
From left, Sara Robart, Mary Jane Piro, Kathleen Armando, Dr. Dana Zalkind & Amie Kandalaft.
Pain will impact you at some point in your life. Whether its a lingering back or neck strain,
clinic treats more than 5,000 patients annually for various types of syndromes. This interventional pain facility does a wide variety of procedures for spinal pain, joint pain and neuropathic pain. An average visit to the pain management clinic can last between 30 minutes to two hours. Procedures are done utilizing x-ray technology as well as cardiovascular monitoring. Conscious sedation is also available to alleviate anxiety.
C .A.R.E. STANDA RDS
C. Communicate your commitment to providing high quality service A. Appear and act as a professional R. Respect all individuals E. Extend yourself
Remember to plan for language needs (interpretation, translation and assistive devices) for all patients that may require this extra service.
an old foot injury, joint pain, neuropathy or bromyalgia, patients are nding relief at Faulkner Hospitals Pain Clinic. Faulkners Pain Clinic was established 17 years ago under the medical directorship of Dr. Dana Zalkind, who was recently named one of Boston Magazines top doctors of 2010. Dr. Zalkind and her partners from New England Pain Management Consultants have expanded the practice with the assistance of the excellent nursing staff here at Faulkner Hospital, comprised of Kathleen Armando, Mary Jane Piro, Amie Kandalaft and Sara Robart with the assistance of Maureen Schnur, MS, RN, CPAN, Nursing Director. The Nursing staff is ACLS certied with a combined work experience of 91 years. The The staffs goal is to treat every patient with respect, dignity and empathy while working to improve the patients quality of life by making their pain more manageable. The goal of improving quality of life is very important to everyone in the Pain Clinic.
continued on P2
Procedures are performed by physicians who are board certied in anesthesiology and pain management.
Summer 2011 Medical Staff News 1
DEAR MEDI CAL STAFF,
The past few months have been a time of signicant changes here at Faulkner Hospital. As Dr. Stephen Wright, Chief of Medicine and Chief Medical Ofcer, announced his retirement we have needed to take up the great challenge of considering his replacement. It is no surprise it will take more than one person to replace him so the position of Chief of Medicine will be separated from the Chief Medical Ofcer. And still these are quite big shoes to ll. I want to congratulate Dr. ONeil Britton who will be taking on the role of Chief Medical Ofcer. With his experience and skill I think this will be an exciting time for the development of that role. We are fortunate to have someone so well respected on both campuses who understands the inner workings of Faulkner and our role in the BW/F family. Please join me in congratulating and assisting him in his transition to this new role. Finally, this year marks 40 years of the Sagoff Centre, a true clinical center of excellence in breast imaging and patient care. The rst We have just initiated a search for a new Chief of Medicine. The committee is composed of myself, Pardon Kenny, ONeil Britton and Mike Querner and is being chaired by Dale Adler. We spent our rst meeting discussing the important aspects of teaching and clinical excellence the role requires and will start looking for candidates in the immediate future. Please feel free to contact any one of us with questions or comments regarding the search. I want to welcome our new Chief of Radiology, Stephen Ledbetter. He comes to us from Brigham Radiology where he was the Director of Emergency Radiology. He has shown great enthusiasm in the rst few weeks of his tenure and is known at the Brigham for his excellent patient care and administrative ability. Sincerely, Peggy Duggan, MD, FACS President, Faulkner Hospitals Medical Staff We are loosing two great leaders and physicians in Steve Wright and Norman Sadowsky and we should all feel lucky to be able to call them our colleagues and our friends. All the best to both of you in retirement. of its kind dedicated to breast imaging, the Centre has been the model so many other institutions have tried to emulate. The Sagoff Gala on May 20th was a celebration of this and Dr. Norman Sadowskys 40 years of service.
Pain management at Faulkner Hospital continued from P1
That could mean being able to play with ones grandchild, to be able to return to work, or simply to be able to perform ones daily activities comfortably. In addition to these interventional procedures, Dr. Zalkind and the other physicians in the clinic utilize many other services at Faulkner Hospital, such as Physical and Occupational Therapy, Psychiatry, Social Work, and Addiction Recovery when needed. They try to assist the patients with the additional avenues of care and act as liaisons between the two to ensure the highest quality of care is given. Using a multi-modality approach, we are able to look at a patients problem from all angles and provide the most comprehensive treatment possible in order to make their pain more manageable, says Dr. Zalkind. Faulkner Hospitals Pain Clinic is located on the 7th oor of the hospital and is open to schedule appointments Monday Friday from 8 am 4 pm. To make an appointment, call 617-983-7080.
We welcome your feedback and suggestions for future issues. Published by Marketing and Public Affairs (617) 983-7588 djgoldberg@partners.org
2 Medical Staff News Summer 2011
Chief Medical Ofcer appointed at Faulkner Hospital
ONeil A. Britton, MD, was recently appointed Chief Medical Ofcer at Faulkner Hospital, effective June 1.
Dr. Britton is a highly respected leader both within and outside the BW/F community, says BWH President Betsy Nabel, MD. I am condent that he will help position Faulkner Hospital for even greater success, ensuring that we maintain
Dr. ONeil Britton
leadership abilities. With a wealth of experience in clinical operations, he has demonstrated a deep commitment to quality improvement and mentoring the next generation of physicians. He is also serving as Vice President of Professional Services and Associate Chief of Medicine at Faulkner Hospital, as well as a vice chair of Medicine at BWH. He remains clinically active as a hospitalist at Faulkner. A graduate of the City College of New York, Dr. Britton completed his medical degree at New Jersey Medical School and did his Internal Medicine training at BWH. He was the rst associate director of the Ofce of Minority Career Development at BWH, prior to the creation of the Center of Faculty Development and Diversity. He left BWH to serve as medical director of Horizon Healthcare of New York, and returned two years later as a Deland Fellow.
the quality for which we are known as we venture forward to face the new and pressing health care challenges ahead. Dr. Britton is a leader who upholds the highest standard of personal integrity. Early on in his career, Dr. Britton was identied as an individual with incredible medical acumen and insightful
SAGOFF BREAST IMAGING AND DIAGNOSTIC CENTRE TURNS 40 AND GETS A FACE LIFT
Even from the outside, Faulkner Hospitals Sagoff Breast Imaging and Diagnostic Centre looks noticeably different. While a fresh coat of paint and weeks spent revitalizing the brick work has left the building looking brand new, its the changes inside the Centre that are the most striking. We recognized that we needed to listen to the feedback our patients were providing and make improvements based on what they wanted, states Brian McIntosh, Director of Radiology. The timing was right in that it coincided with our fortieth anniversary as a Centre. When patients rst enter the Centre on the second or fourth oors of Belkin House, they will nd natural light lling the registration and waiting areas, along with new furniture, privacy doors, updated carpeting and New patient lockers have also been installed in the refreshed handicapped accessible changing areas. The renovated gowned
Summer 2011 Medical Staff News 3
patient waiting areas have also been updated to allow for more privacy, a digital at screen television and comfort amenities, such as a coffee machine and a bottled water station. Perhaps whats most notable about the renovations that took several months to complete is the calming and peaceful atmosphere of the entire Centre. New doors prevent much of the noise from exam and reading rooms from reaching the
Hospital administrators and members of Faulkner Hospitals Sagoff Breast Imaging and Diagnostic Centre cut a ceremonial ribbon marking the completion of renovations.
waiting areas. In addition, carts and personal items that were previously stacked in halls have been permanently moved to out of
modern lighting. The sign-in desk has been moved closer to the entrance doors so that patients are greeted immediately, and three new registration areas specic to the second oor offer more privacy than before.
sight storage areas. Our breast care services have always been among the best in the country, states Jeanne Staunton, Breast Imaging Manager. Now we have a top notch facility to match the top notch services we offer.
Guidelines For Teaching Physicians, Interns, and Residents
The article provides teaching physicians, interns, and residents information about the following:
Payment for physician services in teaching settings; General documentation guidelines; and Evaluation and management documentation (E/M) guidelines. The services are identiable physician services, the nature of which Payment for Physician Services in Teaching Settings Services furnished in teaching settings are paid under the Medicare Physician Fee Schedule (MPFS) if the services are: Personally furnished by a physician who is not a resident; Furnished by a resident when a teaching physician is physically present during the critical or key portions of the service. Medical and Surgical services furnished by an intern or resident within the scope of his or her training program are covered as provider services and paid by Medicare through direct Graduate Medical Education (GME) Program and Indirect Medical Education (IME) payments, and the services of the intern or resident may not be billed or paid for using the MPFS. Dictated and transcribed; Services Furnished by an Intern or Resident Outside the Scope of an Approved Training Program (Moonlighting) Medical and surgical services furnished by an intern or resident that are not related to his or her training program and are furnished outside the facility where he or she has the training program are covered as physician services when the requirements in the rst two bullets listed below are met. Medical and surgical services furnished The teaching physician may use a computer generated macro (predetermined text not edited by the user) as the required personal documentation if he or she personally adds it in a secured or Typed; Hand-written; or Computer-generated. General Documentation Guidelines Both residents and teaching physicians may document physician services in the patients medical record. The documentation must be dated and contain a legible signature or identity and may be: require performance by a physician in person and contribute to the diagnosis or treatment of the patients condition. The intern or resident is fully licensed to practice medicine, osteopathy, dentistry, or podiatry by the state in which the services are performed. The services furnished can be separately identied from those services that are required as part of the training program. by an intern or resident that are not related to his or her training program and are furnished in an outpatient department or emergency room of the hospital where he or she is in a training program are covered as physician services when the requirements in all three bullets listed below are met. When these criteria are met, the services are considered to have been furnished by the individual in their capacity as a physician, not in their capacity as an intern or resident.
FAULKNER PHYSICIAN DONATES ORIGINAL ARTWORK
Dr. Raymond Murphy, former Chief of Faulkner Hospitals Division of Pulmonary Care, recently donated ve original pieces of his artwork to Faulkner Hospitals Patient/Family Resource Center. Dr. Murphys donated artwork is of birds, owers and other things found in nature, which he has recreated using pastels and watercolors. The paintings were done over the last ve years and donated to the hospital in 2010. I donated them as an expression of my thanks to the wonderful people Ive worked with, as well as to the patients and their families who have beneted from the excellent care they received at Faulkner Hospital, says Dr. Murphy. It is Dr. Murphys hope that viewers of his artwork are able to see the beauty in the world despite the many problems life throws at them.
4 Medical Staff News Summer 2011
password protected system. In addition, to the teaching physicians computer generated macro, either the resident or the teaching physician must provide customized information that is sufcient to support a medical necessity determination. The note in the electronic medical record must sufciently describe the specic services furnished to the specic patient on the specic date. Evaluation and Management Documentation Guidelines For a given encounter, the selection of the appropriate level of E/M services is determined according to the code of denitions in the American Medical Associations Current Procedural Terminology (CPT) book and any applicable documentation guidelines. When teaching physicians bill E/M services, they must personally document at least the following: That they performed the service or were physically present during the critical or key portions of the service furnished by the resident; and His or her participation in the management of the patient. The combined entries into the medial record by the teaching physician and resident constitute the documentation for the service and together must support the medical necessity of the service. Documentation by the resident of the presence and participation of the teaching physician is not sufcient to establish the presence and participation of the teaching physician. Evaluation and Management Documentation Provided by Students Any contribution and participation of a student to the performance of a billable service must be performed in the physical presence of
a teaching physician or resident in a service that meets teaching physician billing requirements (other than the review of systems [ROS] and/or past, family, and/or social history [PFSH], which are taken as part of an E/M service and are not separately billable). Students may document services in the medical record; however, the teaching physician may only refer to the students documentation of an E/M service that is related to the ROS and/or PFSH. The teaching physician may not refer to a students documentation of physical examination ndings or medical decision making in his or her personal note. If the student documents E/M services, the teaching physician must verify and redocument the history of present illness and perform and document the physical examination and medical decision making activities of the service. To nd additional information about documentation guidelines for E/M services, visit http://www.cms.hhs.gov/MLNEdWebguide/25_ EMDOC.asp on the CMS website. Questions or comments regarding this article can be address to Patrick V. Cerce, Director of Compliance at (617) 983-7470.
IMPLEMENTATION OF HIPAA 5010/ICD-10
As you may have heard, the Federal government has mandated changes to the 4010 HIPAA transaction standards (claims and eligibility) and the International Classication of Diseases (ICD) coding system. All covered entities, including health care providers, must convert from ICD-9 to ICD-10-CM (diagnosis) and ICD-10-PCS (procedure) codes by the compliance date of October 1, 2013.
How will this change impact Faulkner Hospital, Partners HealthCare, the health care industry and you? Working with Partners, Faulkner Hospital has a project plan in place for this mandated change. In the weeks and months ahead, you will be receiving more formal communication about this project as it relates to your department, including an initial training survey that you will receive by the end of March. If you have any questions, please contact Debra Torosian at 617-983-7458.
Summer 2011 Medical Staff News 5
Health Care Unseen
By Joe ODay, Director or Faulkner Hospitals Pharmacy A friend of mine from college, knowing I had decided to transfer to pharmacy school, would goad me, saying I heard pharmacists take pills from big bottles and put them into little bottles, and start laughing. Hed been admitted to dental school. I may have to count pills, Id respond, but youll be staring down throats the rest of your life. Dispensing medications counting pills is a fundamental activity in pharmacy. Patients need correct medications, need them promptly, and require appropriate education. But there are other parts to the job, just as important. Pharmacists help patients every day by intervening in their medication orders, discovering and correcting drug interactions and therapeutic duplications, educating other health care workers and patients, and helping to ensure the best outcomes. From an outsiders perspective, most of these actions are under the radar. A few years ago I received an urgent phone call from a medical resident covering the intensive care unit at my community teaching hospital in the Boston area. His patient had attempted suicide by drinking an extremely poisonous substance. The conventional treatment for such a poison was to administer intravenous ethyl alcohol in amounts to keep the patient intoxicated. By competing with the substances metabolism, the alcohol prevents toxic metabolites from forming, avoiding renal failure and metabolic abnormalities and allowing time for it to be removed by dialysis. I had encountered an identical situation years earlier at a different hospital. At that time, Poison Control helped us determine the concentration of the ethyl alcohol needed and how to prepare and lter these infusions. That patient survived with no permanent adverse effects, and when the physician on the case called days later to thank us, it felt great. Ten years later, the same poisoning had occurred, but there was a new antidote with fewer side effects than alcohol. Working with two other pharmacists, we acquired enough of the antidote to get the patient through this crisis, conferred with the resident to ensure correct dosing and appropriate duration of treatment, and prepared and delivered it to the patients nurse, describing its mechanism of action and side effects. Over the next few days, we delighted in the fact that our patient survived with no permanent physical injury. I once sprinted up four ights of stairs carrying gingerly the life-saving clot buster Alteplase (TPA) in order to get it into the nurses hands so she could administer it to a patient suffering a heart attack. The sooner it gets infused, the greater the amount of heart muscle saved, and the better the chances are of a successful outcome. After handing it over, I relaxed and caught my breath, then walked past the nurses station towards the elevator. The cardiologist who ordered it looked up from the patients chart and smiled, a silent thank you crossing his lips. I remember an anesthesiologist once asking me to mix a new type of preparation, an infusion to be administered into the epidural space. He wanted to use it on an inpatient with terminal cancer who, despite receiving high doses of narcotics intravenously, had intractable pain. Epidural analgesia is a technique where the tissue space around the spinal cord is injected or infused with an analgesic. Benets include enhanced pain relief (the drug is administered directly to the central nervous system), and fewer side effects (the amount needed is small so less drug gets into the systemic circulation). The preparation in this case would be a mixture of a local anesthetic and a narcotic. We gured out the amounts of each drug in the mix, ensuring compatibility, stability, and correct dose. It was administered to the patient with great pain-relieving results. Our epidural analgesia program had begun and quickly spread to include many other patients. Epidural analgesia would become an important tool in the world of pain relief. Several months later, while checking medication stock on the intensive care unit, the chief of anesthesia pulled me into a patients room and introduced me as the guy responsible for relieving your pain. I thought it a kind and overstated gesture by a nice guy, but Ive remembered it through the years. A few years ago there was a patient admitted to a surgical oor with an exceptionally confusing drug regimen. She claimed to have allergies to the excipients (inactive ingredients) in medications, was on more than ten different drugs, took them throughout the day, and had set up a nicky system of self-medication. This patient requested to take her own medications. Hospitals have a policy requiring that only those medications purchased and stocked by that hospital can be used while the patient is under its care. This makes certain the drugs have been obtained from a reputable
6 Medical Staff News Summer 2011
supplier, have been stored properly, and are still in date. However, sometimes an exception is made, and only if the patients medications are properly labeled, can be identified by the pharmacy, and will be administered by the patients nurse. This patients physician said that her certainty of reacting badly to the hospitals drugs (many identical to the ones she had brought in) was causing her great angst. We
highlights the importance of understanding the patients side of an interaction, of the role of empathy in the healing process. The group was to meet at 6:30 pm.
respected her fear about someone tampering with her system. The book had done its job. One evening I got a call that a patient had
My assistant had to leave, so I brought the patients reorganized medications to the nursing unit to review them with the nurse and physician. I needed something clarified and asked the medical resident if I could see the patient. As we entered the room and the
refractory thrombocytopenia (abnormally low platelet level), a potentially life-threatening condition, and that the physician wanted to try a seldom used medication. We worked out the dose with the patients resident and consulting hematologist, and prepared it and educated the nursing staff about its administration. This, of course, occurred at
. . . After handing it over, I relaxed and caught my breath, then walked past the nurses station towards the elevator. The cardiologist who ordered it looked up from the patients chart and smiled, a silent thank you crossing his lips.
acquiesced and picked up the patients Tupperware container with her medications inside. They were a mess, mixed together in various prescription bottles. Another pharmacist and I spent hours sorting through, organizing, and identifying as many as we could. As we finished up, I noted the time: 6 pm. I hoped to make my hospitals medical book club meeting that night. We were to discuss Anne Fadimans book The Spirit Catches You and You Fall Down. It tells a harrowing story of a Hmong family in California, how a lack of cultural understanding contributes to the tragic death of a child to seizures, and Arriving at the book club at 7:30 pm, I mentioned the irony of having read a book about the dangers of miscommunication between patients and caregivers and what I had just experienced. I was upset, but had resident introduced me as The Pharmacist, the patient became agitated, pointed at me and shrieked, thats the guy whos screwing me up! I had the impulse to say I just wasted three hours figuring out the meds just to make her happy. But there was nothing to fight against. My job was to help. When I gently reassured her that she could take her own medications and that I only needed one question answered, she settled down.
the end of the day, making a long day longer. Finishing up afterwards, I thought of the stressful hours the process took, how the pharmacy had reacted quickly and successfully, and as I threw on my coat and walked outside into the damp, cold, winter night toward my car, I clenched my fist and punched the air in victory. The drug was administered with good results: the patients platelets rose to safe levels. Days later, I asked our two pharmacy students, who rounded with the residents, about the patient. Shes a professional singer, they said. She sang O Danny Boy for St. Patricks Day, to thank everyone. I felt a wave of resentment. Surely we also deserved to receive this gift of thanks. No one knew that three of us had stayed hours after our shift to ensure her treatment went perfectly. Then I caught myself: We dont work for accolades; we work to get our patients well.
Get the latest program information, health tips and events in one of three easy ways:
1
Become a fan of Faulkner Hospital: http://www.facebook. com/faulknerhospital
2
Follow Faulkner Hospital on Twitter: http://twitter.com/ faulknerhosp
3
Sign up for online news delivered right to your inbox: http://www.faulknerhospital.org/ enews.html
Summer 2011 Medical Staff News 7
Reducing Risk During Patient Hand-Off Communication
Joanne C. Locke, RN, JD Director, QI and Risk Management Everyone understands, in principle at least, how important hand-off communication is during patient care transitions from one physician to another, or from one medical setting to another. Although the hand-off process is routine, it may become a potentially risky event for providers when the hand-off is incomplete or fumbled. As a primary care physician, the provider should inform patients when Problems with hand-off communication account for the root cause of up to 70 percent of adverse events, according to The Joint Commission. Failure to communicate important information in a timely manner may cause or substantially contribute to patient injury or death. In such cases, the hand-off failure also may lead to a malpractice claim against all providers involved in the hand-off. Vulnerability to hand-off failure rises with the increasing segmentation of care in our healthcare system. Hospitalists who may have no prior relationship with your patient now hold day-to-day responsibility for in-patient assessment and care. Consultants who provide specialized care for your patient rely upon your consultation request to determine how you wish them to assist you in the diagnosis and treatment of your shared patient. An incomplete or hastily written request may result in a diagnostic test not being ordered or failure to perform follow-up care, resulting in a delayed diagnosis and treatment for the patient. Medical schools do a poor job of teaching hand-off communication, so when new house staff arrive at the hospital, it is necessary for Be sure to communicate essential information about the patient to the accepting hospital team, in a clear and concise manner, allowing time for questions. Information about allergies, difcult airway/intubation status, and need for follow-up care require explicit instructions, and may benet from a standardized communication tool. If you receive notication that your patient was recently admitted or discharged from a hospital, be sure to have a system in place at your ofce to document your receipt and review of the discharge summary, especially regarding follow up care. Your ofce should have a system in place that logs in the documents and a place for signature or initials that prove you have seen it. a hospitalist will care for them. This will avoid additional stress upon your patient who may be admitted urgently to the hospital, and be distressed to encounter a complete stranger on the unit, seeing no sign of you. By resetting patient expectations in advance, you can head off a misinterpretation by the patient and family that you were ignoring the patient and correct a misinterpretation that you have essentially abandoned the patient. attending level physicians and senior house staff to teach the hand-off and to assess the level of competency of the trainee before placing patients in their care. Using a standardized approach with checklists is recommended to assure that all essential data points are covered.
NEW CHIEF OF RADIOLOGY
Stephen Ledbetter, MD, MPH, was recently named Chief of Faulkner Hospitals Radiology Department.
Prior to joining Faulkner, Dr. Ledbetter was the Section Head of Emergency Radiology and the Director of the NightWatch Teleradiology Program at Brigham and Womens Hospital, both of which he founded in 1999 and 2004, respectively. Dr. Ledbetter brings a progressive patientcentric vision to our department that will strengthen every aspect of care we provide, says Jeanne Staunton, Breast Imaging Manager. Under his leadership, every
8 Medical Staff News Summer 2011
decision we make as a department will enhance the quality and efciency of the services we provide, she adds. Among the goals Dr. Ledbetter hopes to accomplish at Faulkner are to increase the level of radiology sub-specialization to better meet the needs of our patients and referring physicians, strengthen the professional relationships and interactions of radiologists across the BWF enterprise, and reinvest in the Sagoff Centres remarkable history of innovation in breast imaging and interventions. When asked why he decided to come to Faulkner, Dr. Ledbetter said I came to Faulkner because of its reputation as a best-in-class community hospital, because
of its ties with BWH, and because I thought there were tremendous opportunities for my personal and professional growth as a radiologist and as a radiology administrator. Dr. Ledbetter graduated from the Bowman Gray School of Medicine, now the Wake Forest University School of Medicine in Winston-Salem, NC. He completed his residency in Radiology followed by a fellowship in Emergency Radiology, both at Brigham and Womens Hospital. Dr. Ledbetter obtained his Masters of Public Health from Harvard in 2005. In his spare time, Dr. Ledbetter enjoys spending time with his family, cooking, running, listening to music and dabbling in real estate.
When sending a patient out for a consultation, be sure that your own request is clearly written, with explicit tests and examinations you wish performed. A referral to a gastroenterologist may not automatically include a colonoscopy without the PCP documenting this expectation. If both the GI consultant and the PCP do not notice that a patient is overdue for a screening colonoscopy and fails to perform it, this creates a liability gap for both physicians if a later claim of delayed diagnosis of colon cancer is brought a year after the two practitioners saw the patient. If you recommend a test and the patient refuses, it becomes especially important to document the risks of refusing the test, and advising the patient to reconsider. You always must avoid a tone of frustration, but be sure to document your attempt to change the patients mind, and be sure that the patient signs an informed refusal, to demonstrate the patient understood the implications of his or her decision. Telephone conversations or curb-side consults are to be avoided when possible. If engaging in these practices, it is essential to document what was said and done in response to the request. Many malpractice cases hinge on the lack of a note during such conversations. At every hand-off, check and re-check medications. Five steps should occur:
Create a list of current medications Create a list of medications to be prescribed Compare the medications in each list and make a clinical determination of compatibility based on your review. Calling the pharmacy or checking the PDR can be helpful, but be sure to document that you did so. Communicate the new list to the next providers. Creating a standardized hand-off checklist will provide proof that important information was communicated to the next team caring for the patient. Whenever possible, communicate face to face without interruption and provide an opportunity for both parties to ask questions and clarify any ambiguities. Conrm that what you said has been heard and understood by using a teach back method or asking the receiving provider to summarize with you what is expected and what will be communicated. Finally, document the substance of this conversation in the medical record. Compliance with these basic rules of hand-off communication will maintain the patients safety and protect the providers from costly hand-off fumbles that may result in patient injuries and subsequent liability claims.
NEW TECHNOLOGY ALLOWS RADIOLOGISTS TO OPTIMIZE IMAGES
Faulkner Hospitals Radiology Department recently began using an eight-channel wrist coil in their MRI service to optimize both the patient experience and the images produced. The wrist coil utilizes eight channels, or frequencies, to provide more specic, high resolution images of the wrist and its components, as well as to maximize the comfort of the patient throughout the imaging process. These optimized images provide physicians with a more detailed view of the wrist, allowing them to better diagnose and treat the symptoms more accurately. The noise, or motion some images show, is also greatly reduced. Since we have implemented the coil we have seen a reduction in test time and patient satisfaction, says Catherine Brockington, RTRMR, Staff Technologist.
Summer 2011 Medical Staff News 9
Dear Faulkner Hospital,
My father suffered a horrible fall and I immediately brought him to Faulkner Hospitals Emergency Room for evaluation and treatment. From the moment we entered the hospital to the time we left every staff member we encountered treated us with genuine kindness and compassion. Beth Gangemi greeted us as we walked in and she immediately took our information and called for someone to get ice for his injuries. Lorraine Traft, RN immediately assessed my fathers condition and was very kind and warm to him while treating him. My father was immediately brought into an exam room and Anthony Paglia, PA was very thoughtful and caring while treating my father and made him feel very comfortable. There was a sweet nurse named Karen White that came in and sat next to my father on the stretcher and talked It was a difcult situation to be in with my father and the treatment that he received at Faulkner Hospital made a bad situation more endurable. We are very grateful that we can count on Faulkner Hospital to treat our valued family members with respect, kindness and compassion. I am happy to tell you that my father is recovering very quickly and feeling much better. Thank you all for being there when we really needed you. to him and made him feel cared for. Our nal encounter was with Kelly Mastroianni, RN who cleaned and treated my fathers wounds. Kelly communicated with my father before she treated him just so he was aware of what was going to be done and she was very gentle and sweet with him.
Dear Faulkner Hospital,
I am writing to thank you for the wonderful care of my mother while she was hospitalized at Faulkner Hospital. Most of the staff was helpful and measured up to expectations of a world class hospital, however, there were certain staff members on 6 south who were exceptional. Dr. Chaln was quite impressive not only as a skilled physician, but also as a leader and teacher. She advocated for her patient, managed the care team and listened to the concerns of the family and responded as quickly as possible. Her competence and awareness of cultural differences was outstanding. Not only My family and I are truly grateful for the treatment received at your hospital. There was also a nurse whose name I do not recall. She attempted to meet my mothers every need, making her feel as if she was her only patient. The nursing supervisor whom I had the opportunity to meet was also a superb employee. She was competent, caring and very professional. was she respectful and kind to all involved, she did this with ease.
Dear Faulkner Hospital,
My father was recently hospitalized at Faulkner Hospital and I am writing to commend the staff on the expert, compassionate care that they provided. From the nurse in the ED to the nursing staff and PCSs on 6 South, the care provided was outstanding. I would also be remiss if I did not mention the high level of customer service provided by transport, dietary and phlebotomy staff. Your staff exceeded my expectations in the high quality and safe patient care provided and, as such, should be recognized for their efforts. Staff was respectful and welcomed the input of family members in my fathers care. Two residents, Katherine Rose and Michelle Morse, exemplied the essence of patient- and family-centered care in their interactions with my father and his family.
10 Medical Staff News Summer 2011
NEW MANAGER OF MEDICAL INFORMATICS AT FAULKNER HOSPITAL
Dr. Ali Bahadori is the new Manager of Medical Informatics at Faulkner Hospital. He is responsible for evaluating and introducing improvements to the Meditech system to enhance the clinician experience. In his short time in his new role, Ali has already begun improving the clinical end-user experience on Meditech and his skills and expertise will be very
Dr. Ali Bahadori
New Medical Record Documentation Policy
Faulkner Hospital has a new Medical Record Documentation Policy, aimed at removing certain documentation standards from the medical staff bylaws, making them more easily changeable if and when necessary. The policy mimics a similar policy at Brigham and Womens Hospital that was recently identied as a best practice by Partners Internal Audit Services. The policy was developed by the Health Record Policy Committee and the Medical Staff QI Committee and approved by both the Medical Executive Committee and the Bylaws Committee. This policy went into effect January 1, 2011 and can be found on Faulkner411.org by clicking the following links: Policies and Procedures Administrative Health Information Services Medical Record Policies and then click on Faulkner Hospital Medical Record Documentation Policy. Please share this information will your colleagues as there are some signicant changes involving timing of operative notes, frequency of progress notes and sanctions that are imposed for non-compliance. Contact Deb Torosian, Director of Health Information Services and Chief Privacy Ofcer, at 617-983-7458 with any questions.
valuable for Faulkner Hospital going forwards, says Dr. ONeil Britton, Chief
Medical Ofcer and Vice President of Professional Services at Faulkner Hospital. Dr. Bahadori attended medical school at Penn State College of Medicine in Hershey, PA. He did both his residency and internship in Internal Medicine at Penn State/Hershey Medical Center before coming to Boston in 2008. Before joining Faulkner Hospital, Dr. Bahadori was the Physician Lead on the Acute Care Documentation project, a joint venture between Brigham and Womens Hospital and Massachusetts General Hospital. He also practices clinically both Faulkner and Brigham and Womens as a hospitalist physician. I came to Faulkner because I wanted to use my skills in technology and workow improvement to make the clinical areas of the hospital the best they can be, says Dr. Bahadori. Dr. Bahadori was born in Tehran, Iran and now lives in the Boston area.
RESOURCE CENTER OFFERS NEW DIGITAL BOOK PLAYER
Faulkner Hospitals Patient/Family Resource Center (PFRC) recently received a digital talking book player on permanent loan from the Perkins Braille and Talking Book Library. The player utilizes book cartridges and downloads from the Library of Congress digital book collection. Each month, the With this player, we are now able to expand our offerings to patients who cant see or have difculties reading print, says Cara Marcus, Director of the P/FRC. Perkins Library will send the PFRC a new cartridge for their collection.
Summer 2011 Medical Staff News 11
Center for Robotic Surgery helps women with gynecological disorders
At Brigham and Womens Center for Robotic Surgery at Faulkner Hospital, gynecologists are using cutting edge technology to treat and care for many gynecological conditions using state-of-the-art robotics to improve reproductive surgery outcomes. At Brigham and Womens Center for Robotic Surgery at Faulkner Hospital, physicians use the da Vinci Surgical System to perform a wide variety of gynecological procedures including: Hysterectomies (benign or cancer) Myomectomy (removing broids but preserving the uterus) Tubal Reversals (after prior tubal ligation) Endometriosis Ovarian cysts and masses Under the direction of Dr. James Greenberg, the Center is led by Dr. Antonio Gargiulo and Dr. Serene Srouji who are pioneers in the eld of gynecological robotic surgery, having performed New Englands rst successful robot-assisted laparoscopic tubal sterilization reversal, as well as Bostons rst robotassisted hybrid myomectomy for the removal of very large myomata. They have since
Dr. Antonio Gargiulo and Dr. Serene Srouji
This miniaturization, increased range of motion, enhanced vision, and mechanical precision ultimately allow for virtually all reproductive surgeries to be performed laparoscopically, translating into added benets for the patient, such as: Less blood loss Less post-surgical pain/less medication Quicker recovery and return to normal activities Less scarring Less likelihood of complications Many of our patients are still in their childbearing years, states Dr. Srouji. Of all the gynecological procedures performed today, the precision of robotic surgery allows us more opportunities to effectively preserve the fertility of our patients. If you have any of the symptoms described above, call us at 617-983-7500 to schedule a consultation.
continued this accomplished partnership to perform more than 350 robot-assisted surgeries. Traditional open surgery requires one large incision and retraction to accommodate human hands, but only small incisions are required for the robots hands, states Dr. Gargiulo. In fact, these hands are attached to four arms - one guides a high denition 3-D camera, two act as the surgeons main arms, and an optional arm is often used for holding back tissue. The movements of the robot are always guided by a doctor, never programmed.
Hand hygiene is the #1 way to prevent the spread of infections
Stopping infections is in our hands.
12 Medical Staff News Summer 2011
Summer 2011 Medical Staff News 13
REHABILITATION SERVICES EMPLOYEES ACCEPTED INTO LEADERSHIP PROGRAM
Kerstin Palm, an Occupational Therapist and Certied Hand Therapist and Kathy Belanger, a Licensed Physical Therapist in Faulkner Hospitals Rehabilitation Department, have been accepted into Brigham and Womens/ Faulkner Hospitals Leadership Competencies for Managers Program, a nine month leadership and development program based on best practices for management and Kerstin Palm, left, and Kathy Belanger. leadership. After seeing how therapists helped my grandmother after she broke both her hips, I knew I wanted to be a part of the rehabilitative healthcare team, Belanger recalled when asked why she chose to be a physical therapist. For Palm she was inspired to become a therapist because of the ability to work meaningfully with a diverse group of people. Both Palm and Belanger had to submit an application outlining their career path and goals, a CV/resume, a recommendation by the department director, references and undergo a formal interview to gain admission to the program, which was highly recommended to them by fellow Faulkner colleague Melissa Joseph, RN, Nurse Manager, 6 North. When asked what they hoped to accomplish by participating in the program, both emphasized a commitment to quality of care and acquiring new skills for leadership focused on providing excellent clinical care in a manner that is patient-centered and optimizes resources.
HEALTH STATUS COMMITTEE
The Health Status Committee of the Medical Staff is a resource available to all Faulkner Hospital physicians. The committee can assist with resources for medical, psychiatric and substance abuse issues, which may be affecting a physicians health status and/or practice. The committee can be accessed directly through contacting any of its members or through your service chief. 2011 Committee Members: Geoff Sherwood, MD Ric Larson, MD Stephen Wright, MD Pardon Kenney, MD Laura Miller, MD, MD Michael Querner, MD Michael Wilson, MD Peg Duggan, MD John Lewis, MD Joanne Locke, RN, JD Edward Liston-Kraft, PhD
Healthy food, healthy hospitals, healthy communities
Faulkner Hospitals Food and Nutrition Department has signed the Healthy Food in Healthcare Pledge, which was created by Health Care Without Harm and is a framework that outlines steps to be taken by the health care industry to improve the health of patients, communities and the environment. Faulkner Hospital committed to reporting annually on our progress with implementing recommended measures to provide more The department has already removed fried foods from the patient menu, increased whole grains on patient and cafeteria menus, held Farmers Markets to promote the local produce we offer, reduced polystyrene products, and added more meatless entre options. In the coming year, we are looking to offer a healthy alternative to fried foods in the cafeteria, promoting and right-pricing the healthier foods in our cafeteria, and exploring the possibility of composting, states Langill. nutritious, local and sustainable food, says Susan Langill, RD, Director of Food and Nutrition. Examples of these measures include offering more whole grains, reducing unhealthy fats, increasing availability of local fresh produce and minimizing food waste. To date, over 250 hospitals around the country have signed the Healthy Food in Healthcare Pledge, and are implementing policies and programs which demonstrate a commitment to rst, do no harm and treating food and its production and distribution as preventive medicine that protects the health of patients, staff, and communities.
14 Medical Staff News Summer 2011
Partnering to reduce avoidable hospital readmissions
Faulkner Hospital and Ethos are partnering in a project to try to reduce avoidable hospital readmissions, dened as unplanned readmissions to a hospital after a previous hospital stay. An example of an unplanned readmission would be a patient who is readmitted to a hospital for a surgical wound infection that occurred following their initial hospital stay. Its important to recognize that there are situations that can lead to unplanned hospital readmissions, states Dr. Ed Liston-Kraft, Vice President, Professional and Clinical Services at Faulkner Hospital. A hospital readmission may or may not be related to the previous visit and some unplanned readmissions are not preventable. As you may be aware, in the near future hospitals will not be paid for avoidable readmissions. This project is designed to The basis of the intervention is the Personal Health Record that gives the patient a portable, low-tech way to manage their medications, identify red ags, set personal health goals, and provide a place The underlying issue is that each time a patient transitions to a new setting, such as from acute care to rehab or from rehab to home, there are opportunities for miscommunication of treatments and medications. Using the Coleman Care Transitions Intervention model, chronically ill older patients and their care givers are taught how to ensure that their needs are met during care transitions, which may reduce the rates of subsequent readmissions. Ethos is a private, non-prot organization dedicated to promoting independence, dignity and well-being among the elderly and disabled through quality, affordable and culturally-appropriate home and communitybased care. For more information about this program, please contact Faulkner Hospitals Department of Social Work at 617-983-7932. The model currently being piloted is the Coleman Care Transitions Intervention model, which has been demonstrated to be a proven method of reducing hospital readmissions for a number of diagnoses, including heart failure, diabetes and COPD. For the pilot project, selected patients from the Faulkner Hospital will be referred to Ethos for Care Transitions. Any patient who participates in this pilot program does so voluntarily. The coaches will meet each patient in the hospital, explain the program and follow-up with a home visit and a number of telephone calls. The coaches have been trained by Dr. Eric Coleman, the developer of the program and have extensive experience working with older patients. see if a tested, evidence-based model will work in todays healthcare environment, says Liston-Kraft. to write down questions for their provider. Coaches trained in the methodology work with the patient to empower them to manage their own health, which may reduce hospital readmissions by meeting the needs of a patient prior to them feeling as though they need to go back to the hospital.
The Healthy Food in Healthcare Pledge encourages organizations to:
Implement a stepwise program to identify and adopt sustainable food procurement. Begin where fewer barriers exist and immediate steps can be taken. For example, the adoption of rBGH free milk, fair trade coffee, or introduction of organic fresh fruit in the cafeteria.
Minimize or benecially reuse food waste and support the use of food packaging and products which are ecologically protective.
Work with local farmers, communitybased organizations and food suppliers to increase the availability of locally-sourced food.
Develop a program to promote and source from producers and processors which uphold the dignity of family, farmers, workers and their communities and support sustainable and humane agriculture systems.
Encourage our vendors and/or food management companies to supply us with food that is, among other attributes, produced without synthetic pesticides and hormones or antibiotics given to animals in the absence of diagnosed disease and which supports farmer health and welfare, and ecologically protective and restorative agriculture.
Communicate to our Group Purchasing Organizations our interest in foods that are identied as local and certied.
Educate and communicate within our system and to our patients and community about our nutritious, socially just and ecological sustainable food healthy food practices and procedures.
Report annually on implementation of this Pledge.
Summer 2011 Medical Staff News 15
Faulkner Hospital offers two options to pre-register:
Please have your insurance card available when pre-registering. If you have pre-registered for your visit, please report directly to your appointment location. If you are not pre-registered or unsure if you are, please stop at the Information Desk upon arrival. They will directyou to your appointment or to registration as needed.
Online:
www.FaulknerHospital.org (24 hours a day)
Telephone:
BREAST IMAGING 617-983-7068 Monday - Thursday, 7 am - 8 pm Friday from 7 am - 3:30 pm Saturday from 8 am - 3 pm ALL OTHER SERVICES 617-983-7010 Monday - Friday from 6 am - 8 pm
Faulkner Hospital Marketing and Public Affairs 1153 Centre Street Boston, MA 02130
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- First Floor Services Map: Hillside ElevatorsDokument2 SeitenFirst Floor Services Map: Hillside ElevatorsdavidjgoldbergNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- View The Postcard Wake Up Call On WCVB-TV5Dokument3 SeitenView The Postcard Wake Up Call On WCVB-TV5davidjgoldbergNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- BWFH Welcome GuideDokument15 SeitenBWFH Welcome GuidedavidjgoldbergNoch keine Bewertungen
- Community Health Fair AdDokument1 SeiteCommunity Health Fair AddavidjgoldbergNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Senior Health and Safety SeriesDokument1 SeiteSenior Health and Safety SeriesdavidjgoldbergNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Walking ClubDokument1 SeiteWalking ClubdavidjgoldbergNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- BWFH NurseDokument8 SeitenBWFH NursedavidjgoldbergNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Final Draft 4Dokument12 SeitenFinal Draft 4davidjgoldbergNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- BWFH PulseDokument12 SeitenBWFH PulsedavidjgoldbergNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Worcester Final BrochureDokument2 SeitenWorcester Final BrochuredavidjgoldbergNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- BU Medical Donor ReportDokument44 SeitenBU Medical Donor ReportdavidjgoldbergNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Our Surgeons Reconstructed A Woman'S Sense of SelfDokument6 SeitenOur Surgeons Reconstructed A Woman'S Sense of SelfdavidjgoldbergNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- E-News 11.2011-3Dokument3 SeitenE-News 11.2011-3davidjgoldbergNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Welcome Guide EVANSDokument16 SeitenWelcome Guide EVANSdavidjgoldbergNoch keine Bewertungen
- Faulkner Nurse - EVANSDokument12 SeitenFaulkner Nurse - EVANSdavidjgoldbergNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- BWH Emergency Radiology (Nightwatch) Enhances Overnight Coverage at Faulkner HospitalDokument3 SeitenBWH Emergency Radiology (Nightwatch) Enhances Overnight Coverage at Faulkner HospitaldavidjgoldbergNoch keine Bewertungen
- L A R G e - S C A L e M e T H A M P H e T A M I N e M A N U F A C T U R eDokument21 SeitenL A R G e - S C A L e M e T H A M P H e T A M I N e M A N U F A C T U R eDaria Schka100% (1)
- Chapter 03Dokument35 SeitenChapter 03david jenil nabuaNoch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Calao Deliquente Diadi River SystemDokument15 SeitenCalao Deliquente Diadi River SystemJason MalamugNoch keine Bewertungen
- Dwnload Full Fundamentals of Nursing 1st Edition Yoost Test Bank PDFDokument35 SeitenDwnload Full Fundamentals of Nursing 1st Edition Yoost Test Bank PDFdetonateousellslbc100% (11)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- BUERGER's Inavasc IV Bandung 8 Nov 2013Dokument37 SeitenBUERGER's Inavasc IV Bandung 8 Nov 2013Deviruchi GamingNoch keine Bewertungen
- Brochure - ILLUCO Dermatoscope IDS-1100Dokument2 SeitenBrochure - ILLUCO Dermatoscope IDS-1100Ibnu MajahNoch keine Bewertungen
- Hmo Details November 2022 1Dokument6 SeitenHmo Details November 2022 1Saad BelloNoch keine Bewertungen
- Mdp36 The EndDokument42 SeitenMdp36 The Endnanog36Noch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Hamraki Rag April 2010 IssueDokument20 SeitenHamraki Rag April 2010 IssueHamraki RagNoch keine Bewertungen
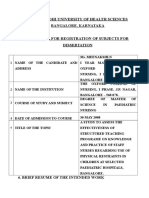
- Rajivgandhi University of Health Sciences Bangalore, KarnatakaDokument19 SeitenRajivgandhi University of Health Sciences Bangalore, KarnatakaHUSSAINA BANONoch keine Bewertungen
- Me3391-Engineering Thermodynamics-805217166-Important Question For Engineering ThermodynamicsDokument10 SeitenMe3391-Engineering Thermodynamics-805217166-Important Question For Engineering ThermodynamicsRamakrishnan NNoch keine Bewertungen
- L Addison Diehl-IT Training ModelDokument1 SeiteL Addison Diehl-IT Training ModelL_Addison_DiehlNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- A6V10424583 - 2 - and 3-Port Valves With - BR - Flanged Connections - enDokument14 SeitenA6V10424583 - 2 - and 3-Port Valves With - BR - Flanged Connections - enAjdin BuljubasicNoch keine Bewertungen
- TM - 1 1520 237 10 - CHG 10Dokument841 SeitenTM - 1 1520 237 10 - CHG 10johnharmuNoch keine Bewertungen
- Đề ANH chuyên 5Dokument7 SeitenĐề ANH chuyên 5Phạm Ngô Hiền MaiNoch keine Bewertungen
- Catalogue CV. Traka Abadi UniversalDokument15 SeitenCatalogue CV. Traka Abadi UniversalHackers StevenNoch keine Bewertungen
- RMP ContractDokument181 SeitenRMP ContractHillary AmistosoNoch keine Bewertungen
- Hospital - Data Collection & Literature StudyDokument42 SeitenHospital - Data Collection & Literature StudyNagateja MallelaNoch keine Bewertungen
- ECE R10 Certification Guide-Edition 1.3Dokument33 SeitenECE R10 Certification Guide-Edition 1.3Ôm Pŕâkẵsh PẵñdêýNoch keine Bewertungen
- Butt Weld Cap Dimension - Penn MachineDokument1 SeiteButt Weld Cap Dimension - Penn MachineEHT pipeNoch keine Bewertungen
- Issue of HomosexualityDokument4 SeitenIssue of HomosexualityT-2000Noch keine Bewertungen
- LIC Jeevan Labh Plan (836) DetailsDokument12 SeitenLIC Jeevan Labh Plan (836) DetailsMuthukrishnan SankaranNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Buss 37 ZemaljaDokument50 SeitenBuss 37 ZemaljaOlga KovacevicNoch keine Bewertungen
- f2607-#### f2607 20191203 111644Dokument2 Seitenf2607-#### f2607 20191203 111644คุณชายธวัชชัย เจริญสุขNoch keine Bewertungen
- Hydrolysis and Fermentation of Sweetpotatoes For Production of Fermentable Sugars and EthanolDokument11 SeitenHydrolysis and Fermentation of Sweetpotatoes For Production of Fermentable Sugars and Ethanolkelly betancurNoch keine Bewertungen
- 99 AutomaticDokument6 Seiten99 AutomaticDustin BrownNoch keine Bewertungen
- Bitumen BasicsDokument25 SeitenBitumen BasicsMILON KUMAR HORENoch keine Bewertungen
- Aplikasi Metode Geomagnet Dalam Eksplorasi Panas BumiDokument10 SeitenAplikasi Metode Geomagnet Dalam Eksplorasi Panas Bumijalu sri nugrahaNoch keine Bewertungen
- 10 Chapter 3 Occupancy Classification AnDokument10 Seiten10 Chapter 3 Occupancy Classification AnMatt BaronNoch keine Bewertungen
- What Has The Government and The Department of Health Done To Address To The Issues of Reproductive and Sexual Health?Dokument5 SeitenWhat Has The Government and The Department of Health Done To Address To The Issues of Reproductive and Sexual Health?Rica machells DaydaNoch keine Bewertungen
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)