Beruflich Dokumente
Kultur Dokumente
Review: Benjamin O Anderson, Riccardo Masetti, Melvin J Silverstein
Hochgeladen von
sanineseinOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Review: Benjamin O Anderson, Riccardo Masetti, Melvin J Silverstein
Hochgeladen von
sanineseinCopyright:
Verfügbare Formate
Review
Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques
Benjamin O Anderson, Riccardo Masetti, Melvin J Silverstein
Lancet Oncol 2005; 6: 14557 Department of Surgery, Section of Surgical Oncology, University of Washington, Seattle, WA, USA (Prof B O Anderson MD); Department of Surgery, Breast Surgery Unit, Catholic University of Rome, Italy (R Masetti MD); and USC/Norris Comprehensive Cancer, Los Angeles, CA, USA (Prof M J Silverstein) Correspondence to: Prof Benjamin O Anderson, Department of Surgery, Box 356410, University of Washington, Seattle, WA 98195, USA banderso@u.washington.edu See Lancet Infect Dis 2005; 5: 94106 for a Review on infection in breast implants
Oncoplastic surgery refers to several surgical techniques by which segments of malignant breast tissue are removed to achieve wide surgical margins while the remaining glandular tissue is transposed to achieve the best possible cosmetic outcome. We summarise the general approach to oncoplastic lumpectomy for surgeons who recognise the limitations of standard lumpectomy for large breast cancers, and review different cancer distributions in the breast and their associated imaging characteristics. Full-thickness broglandular excision of the mass and surrounding breast tissue allows resection with wide surgical margins. Subsequent breast-ap advancement (mastopexy) results in closure of the resulting surgical defect with good or excellent cosmetic closure. These approaches can improve both the aesthetic outcome of breast cancer resections and the likelihood of surgeons obtaining wide surgical margins in preparation for breast-conserving radiotherapy. Advanced volume-displacement techniques, which are based on the key principles of breast reductive surgery, can greatly increase the options for breast conservation in complex cancer cases. Breast-conservation therapy with lumpectomy is a valuable component of breast cancer treatment, with an equivalent survival outcome to that of mastectomy.1,2 In addition to physical preservation, women who undergo breast conservation have a better view of their body image, are more comfortable with nudity and breast caressing, and might have less adverse physical sequelae from asymmetry, chest wall adhesions, and numbness associated with mastectomy.3,4 However, for breast conservation to be effective, surgeons need to remove cancers completely with an adequate surgical margin width and maintain the breasts shape and appearance.5 The undertaking of both goals together in the same operation can be challenging, depending on the tumour location and relative size in the breast (gure 1). If a lesion is large or located in a region that is too difcult to excise without the risk of cosmetic deformity, special approaches to resection should be considered. The value of full-thickness excision with breast-ap mastopexy closure is intuitively apparent. The term oncoplastic surgery is used differently depending on the specialty in which it is being referred.610 In plastic surgery, the term typically refers to large partial mastectomy combined with a volumereplacement technique of partial breast-myocutaneousap reconstruction using the latissimus dorsi or transrectus abdominus muscles. Oncoplastic surgery has now been used to describe several volumedisplacement operations that are technically simple, in which the defect created by large partial breast excisions is covered by a breast-ap mastopexy closure. In this procedure, breast tissue is advanced along the chest wall to ll the defect created by primary resection (gure 2). Without breast-ap advancement, the loss of breast tissue can create a substantial defect in the shape and appearance of the breast, yielding poor cosmetic results. In breast-ap advancement, a full-thickness segment of breast broglandular tissue is advanced on
http://oncology.thelancet.com Vol 6 March 2005
the chest wall or beneath the skin envelope to best preserve breast shape and appearance. Major reconstructive procedures using myocutaneous aps are technically demanding, time consuming, and need special training to learn and apply properly. The complexity of these total or partial
Figure 1: Three-dimensional orientation of typical breast tumour Tumour is shown relative to skin, chest wall, and nipple-areolar complex.
145
University of Washington
Review
Localised cancers extend from one focus in the breast and seem to expand circumferentially during growth. Segmentally extended cancers are distributed along the length of duct-lobular segments, which themselves form a cone or wedgeshaped distribution in the breast. Irregularly extended cancers have thick branches of stromally invasive carcinoma extending out from the index tumour, crossing through breast tissue irrespective of the segmental anatomy.
breast reconstructive operations demands a two-team operative approach, in which a plastic-surgery team works independently from oncological surgeons to reconstruct the breast after the cancer has been removed. By contrast, many small to intermediately sized cancers can be dealt with by use of simple oncoplastic procedures based on breast-ap advancement. These basic operations are easily taught and are used by surgeons with experience in routine breast surgery, because the techniques are technically straightforward and intuitively obvious after the basic principles are understood. Avoidance of poor cosmetic appearance after wide excision by simple oncoplastic methods will increase the number of women who can be treated with breast-conserving surgery by allowing larger breast excisions with improved cosmetic results that potentially achieve widened surgical margins around the cancer.11 We focus on the use of breastap oncoplastic techniques that do not need myocutaneous-ap reconstruction to achieve the best cosmetic outcomes.
Classication by distribution within the breast
Cancers have differing anatomical distributions in the breast. By comparison of preoperative MRI studies with postoperative histopathological ndings in a series of patients with breast cancer, Amano and colleagues15 classied the distribution of breast cancer into three patterns of histological spread: localised (55%), segmentally extended (35%), and irregularly extended (10%). Although this classication might not yet be universally recognised, it denes an important framework for oncological surgeons to use when thinking about breast cancer distribution. During imaging, localised cancers show a distinct focal mass of invasive disease. When tumour satellites are identied around a primary mass, they are located within a few cm of the index lesion. Many localised tumours can be successfully treated by standard lumpectomy without breast-ap advancement. However, success of the procedure depends on the size of the cancer, its position, and the volume of resection needed to achieve clear margins in relation to the volume of the breast. With large localised tumours, the value of oncoplastic breast advancement increases. The extent of disease is generally well predicted by standard imaging (mammography and ultrasound), and the margins of cancer are more obvious to operating surgeons. Localised tumours usually do not include an extensive intraductal component. Because segmentally extended cancers follow the ductal anatomy of the breast, they commonly extend toward the nipple in a radial fashion, down the arborising ductal tree to the contiguous major lactiferous sinus at the nipple, or can extend peripherally in the breast to occupy a large portion of a breast quadrant.
Anatomical distribution of cancer in the breast
Since the lumpectomy procedure was developed for breast conservation, few surgeons considered the anatomical orientation of tumours in the breast for planning surgical resections. Although this modest interest in anatomy might not cause problems for small cancers, resection of large tumours can be challenging, in view of the need to both remove diseased tissue with adequate margins and retain enough histologically non-malignant tissue for a good cosmetic outcome. Increasingly, the need for special surgical approaches to lumpectomy has been recognised.6,10,1214
University of Washington
Figure 2: Closure of breast-ap mastopexy advancement in oncoplastic partial mastectomy resection (A) Resection at full thickness from pectoralis fascia to skin, with an overlying skin island to allow proportional reduction in skin and broglandular tissue. (B) Fibroglandular tissue lifted off the pectoralis muscle to allow its advancement over the chest wall. (C) Closure of defect.
146
http://oncology.thelancet.com Vol 6 March 2005
Review
In classic studies using serial, subgross, whole-organ sectioning of mastectomy specimens, Holland and colleagues16 showed that ductal carcinoma in situ (DCIS) generally occupied one breast segment and was usually distributed in a radial fashion. Amano and coworkers15 recorded that segmentally extended cancers tend to include lesions that are histologically pure or predominant tumours of DCIS. Although some cancers seem to have a multifocal distribution in the breast (ie, include separate islands of disease interspersed with histologically non-affected tissue), Holland and Faverly17 showed that these multifocal lesions were usually contiguous disease arising within one anatomical segment in the breast. Treatment of segmentally extended cancers by standard lumpectomy will probably result in positive margins on excision, or conversely will need a large lumpectomy that is cosmetically unacceptable. Thus, these tumours are best excised by oncoplastic resections with breast-ap advancement. However, if segmental cancers extend to the nipple, which can happen in some extensive DCIS cases, the patient will need resection of the nipple by mastectomy or central lumpectomy.18 Such cancers could present with bloodstained nipple discharge or Pagets disease of the nipple. Irregularly extended cancers tend to be histologically aggressive variants with local growth patterns that are less amenable to breast-conservation treatment if their size becomes prohibitively widespread. In addition to the great need for mastectomy for denitive local control, these lesions could be systemically aggressive with worsened overall prognosis.
Use of preoperative imaging to determine cancer distribution
In many circumstances, the removal of enough tissue to obtain adequate surgical margins might need extensive resections. Bad surgical planning and little forethought can result in a postoperatively deformed breast. Surgery that can both remove enough broglandular tissue and leave the breast shape intact is valuable. To plan an optimum surgical resection, surgeons should not only understand the distribution of cancer within the breast, but also know the degree to which imaging can accurately predict the true histological extent and orientation of disease.
Mammography and ultrasound are not as reliable in determining the distribution of non-invasive cancer. DCIS can be seen on both mammography imaging when microcalcications are present and on radiographs. However, the extent of calcications seen mammographically can be a serious underestimation of the degree of histological spread when these calcications in the lesion form centrally but are absent peripherally.19 Because DCIS usually fails to induce mass-like changes, ultrasound has little or no use in measuring the extent of disease in preparation for lumpectomy. Thus, although standard imaging can predict the distribution of locally extended cancers, it might not predict the full extent of segmentally extended cancers in many cases, especially if an important non-invasive component is present. Incomplete excisions are more probable if the mammographical abnormality does not correspond to the entire extent of the lesion.20 This detection is especially likely to fail with low-grade DCIS, because microcalcication deposition is often absent.1 In such events, the surgical margins are often noted to be positive at resection, even if radiographical images of specimens indicate that all disease has been removed. Second operations need to be done either with an oncoplastic, segmentally orientated re-excision or with mastectomy. Therefore, the surgeon should consider the possibility of positive margins when undertaking an initial excision. Ideally, the incision should be placed in a location that will not prevent a good cosmetic re-excision result. Re-excision of cavity margins is usually done through the same incision without any need for extension of the cut. A subsequent mastectomy needs an extended or new incision.
Breast MRI
MRI is making headway for measuring the extent of disease within the breast. Unlike mammography, breast MRI is not affected by the density of surrounding broglandular tissue in determining the presence of invasive cancer. Breast MRI can also show the presence of cancer that is mammographically occult. When mammographically occult lesions are seen on MRI, subsequent breast ultrasound directed to the same area often shows the malignant disease. Therefore, these lesions can be localised preoperatively under ultrasound guidance to plan an accurate oncoplastic resection. In other cases, the distinct area of malignant tissue also cannot be detected on ultrasound. In such events, MRI-guided biopsy techniques can be used to place clips in the breast that can be localised by mammography during lumpectomy. Boetes and colleagues21 compared the accuracy of MRI with that of mammography and ultrasonography to assess the extent of 61 breast tumours in 60 women
147
Standard breast imaging
The combination of mammography and ultrasound often, but not always, predicts the orientation and extent of cancer within the breast. Invasive cancers form tumour masses that can be seen well with both imaging methods used together. Ultrasound complements mammography, especially if invasive masses are concealed by dense broglandular tissue on radiographs.
http://oncology.thelancet.com Vol 6 March 2005
Review
undergoing mastectomy for carcinoma. The index tumour could not be seen in 10% of cases with mammography, in 15% with ultrasound, but in only 2% with MRI. On mammography and ultrasound images, tumour size was underestimated substantially, by 14% and 18%, respectively, whereas MRI imaging showed no great difference in size compared with that seen in a pathological assessment in this series. Mammography detected 31% of the additional invasive lesions, whereas ultrasound showed 38% and MRI showed 100%. MRI could be especially useful in assessing the extent of disease of invasive lobular carcinoma.22 Compared with mammography and ultrasound, contrast-enhanced MRI has the lowest false-negative rate in detecting invasive lobular carcinoma and has the highest accuracy in measuring the size of these tumours. However, a negative MRI does not stop the need for biopsy in the setting of suspicious mammographical ndings. Occasional cancers, and in particular DCIS, might fail to enhance on MRI but nevertheless be seen on mammography because of radiographically detectable microcalcications.23 Although preliminary data regarding MRI is encouraging, an important limitation of MRI is its high rate of false-positive results. About a third of MRI studies will show some area of enhancement that needs further assessment but ultimately proves to be dense but histologically benign breast tissue.24,25 Practically speaking, the use of MRI in the absence of MRI-guided sampling or clip placement is not recommended, because in many cases the questions raised by studies cannot be resolved before lumpectomy. Additionally, MRI does not always accurately predict the extent of non-invasive cancer, especially when low-grade DCIS is present. Currently, the use of MRI off-trial should be restricted to centres with substantial experience in MRI interpretation and when MRI-guided biopsy is available. MRI could prove to have increased use in planning oncoplastic procedures in the future, but currently the technique would not be considered the standard of care. Furthermore, the high cost of MRI is prohibitive in many health-care settings. More clinical studies regarding patient selection for MRI will undoubtedly shape the future application of this procedure.
The crucial issue is actually margin clearance, which is established by the ratio of tumour-to-breast size rather than absolute tumour dimensions. Serial, subgross, whole-organ sectioning suggests that when margin widths exceed 10 mm, the likelihood of residual disease is small.16 In multivariate analysis, if the tumour margin width is greater than 10 mm, tumour size does not seem to be an independent predictor of local recurrence after breast-conserving therapy.29 Unless histologically adequate margins in surgery are achieved, the absolute tumour size is of secondary importance. However, achievement of the dual goals of oncological clearance and good cosmesis is clearly difcult with increasing tumour size.30 Cosmetic failure with lumpectomy directly relates to breast volume loss, creating an upper limit beyond which volumedisplacement operations will be unsuccessful in achieving an adequate cosmetic result.31,32
Multispecialty collaboration in oncoplastic surgery
The development of techniques for oncoplastic resections of the breast has needed a collaborative approach from different specialties to technical design and operative planning. Surgical oncologists, consulting with plastic-surgery colleagues, have been formalising approaches to oncoplastic lumpectomy. Surgeons without formal plastic-surgery training must determine which procedures they can undertake without plastic surgery consultation and which warrant intraoperative consultation or collaboration. Oncoplastic approaches also need to be closely associated with breast imagery, so that the location of disease can be found and marked as accurately as possible in preparation for operative intervention, by use of needle localisation wires placed before surgery or, in selected cases, intraoperative ultrasound. Oncological surgeons benet from a solid understanding of the strengths and limitations of imaging studies. Similarly, breast imagers benet from understanding the surgical goals in resection to best communicate the location and distribution of malignant tissues within the breast.
Diagnostic biopsy and therapeutic lumpectomy
Diagnostic biopsy and therapeutic lumpectomy are fundamentally different in design and execution. During excisional biopsy for diagnosis, the aim is to remove as little tissue as possible ( 20 g) through the least conspicuous incision. When breast tumour removal is the denitive treatment, the aim is to take out the target lesion completely with widely negative margins (23 cm of macroscopically healthy tissue around the tumour). The undertaking of oncoplastic lumpectomy merely for diagnosis is excessive, because too much tissue would be removed. During diagnostic biopsy, location of the incision should be considered
http://oncology.thelancet.com Vol 6 March 2005
Oncoplastic principles for partial mastectomy
Oncoplastic resections allow the removal of large breast tumours with improved cosmetic outcome and widened surgical margins, which are associated with objective indicators measuring patients quality of life.26,27 Although partial mastectomy for large cancers could hypothetically lead to raised rates of local recurrence, Asgeirsson and colleagues28 recorded little evidence to justify the use of tumour size only as an exclusion criterion for breast-conservation treatment.
148
Review
carefully, since a subsequent therapeutic procedure might be incorporated into the nal oncoplastic design. Preoperative diagnosis of cancers by use of percutaneous image-guided core needle biopsy or vacuum-assisted sampling is best because where the needle is inserted gives no constraints of the surgical approach to therapeutic lumpectomy. Whenever possible, a diagnosis should be made preoperatively by use of a needle with the goal of a single-stage denitive surgical procedure in mind that yields both widely clear margins and good cosmesis.
If the defect is large, such that there is a great deal of redundant skin over the defect, cosmetic and unsatisfactory infolding results, in which the skin adheres to the chest wall and the nipple deviates towards the lumpectomy site.
Full-thickness lumpectomy
Although typical localised cancers of small size might be excised well by standard lumpectomy, segmentally extended cancers need more creative approaches to surgical excision to remove large breast tumours from nipple to periphery. Oncoplastic techniques need careful preoperative surgical planning, whereby the diseased broglandular tissue and surrounding healthy tissue margin is removed together with skin, creating a full-thickness resection down to the chest wall (gure 2).34 The breast gland is lifted off the pectoralis muscle with preservation of the fascia over the muscle. A notable advantage of this posterior dissection and tissue mobilisation is that it allows bimanual palpation of the target lesion to nd where the breast tissue should best be divided. Additionally, broglandular tissue mobilisation helps close the breast after tumour removal (gure 2B). The undermining of broglandular tissue at the pectoralis fascia is sufciently developed for breast-tissue advancement over the muscle, without being too extensive to threaten the blood supply to residual breast tissue. Cosmetically undesirable displacement of the nippleareolar complex can be avoided by widely undermining the nipple-areolar complex at the level of the pectoralis fascia, which allows the tissues to shift to an anatomically natural position.8
C D
Standard lumpectomy resections
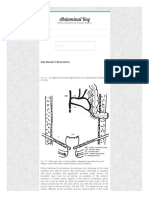
During standard lumpectomy, surgeons generally make a small, cosmetically placed incision directly over the area to be removed. For lesions in the upper breast, incisions are curvilinear following Langers lines (concentric lines parallel to the edge of the areola) or Kraissls lines (natural skin-wrinkle creases that are horizontally oriented).33 For lesions in the lower half of the breast, radial incisions might be chosen, especially if the area to be removed is large. The cancer and surrounding tissues are then removed through the incision. Lateral dissection in the subcutaneous layer is undertaken, but this supercial dissection is not completely benecial because it can cause saucerisation of the skin at nal healing (gure 3). Surgeons should refrain from scooping out the tumour from the breast, but rather methodologically dissect the tissue down to the pectoralis fascia. Failure to adhere to basic principles will compromise ultimate margin clearance. The remaining defect, typically spherical or oblong in shape, is left to ll up with seroma uid and then reabsorb at radiation (gure 3).
A B
Standard lumpectomy
Figure 3: Comparison of standard lumpectomy with parallelogram mastopexy lumpectomy (A) Before incision. (B) After excision of the lesion. (C) After wound closure with seroma. (D) After seroma reabsorption.
http://oncology.thelancet.com Vol 6 March 2005
University of Washington
Parallelogram mastopexy lumpectomy
149
Review
Care should be taken to keep major vascular perforators between pectoralis and the breast intact where possible. The main blood supply of the breast comes from the lateral thoracic and internal mammary and intercostal vessels.35 Collateral circulation in the breast allows ligation of the small intercostal perforators without the vascular compromise that takes place when the larger vessels from lateral thoracic and internal mammary arteries remain intact. Overall, the collateral blood supply of the breast allows much exibility for operative approaches to oncoplastic resections. Breast reduction procedures have been successfully done without glandular necrosis based on posterior pedicle aps from the upper, inner, lower, and outer quadrants of the breast. Once the broglandular tissues are appropriately mobilised, the breast defect is closed at full thickness. Margins of the residual cavity are shifted together by the advancement of breast tissue over muscle, and the defect is sutured at the deepest and most supercial edges (gure 2C). Thr resulting seroma cavity can be drained or left to reabsorb. The remaining breast gland heals with a much better long-term cosmetic outcome than that seen with standard lumpectomy. A limitation of full-thickness excision with the skin of the upper inner breast quadrant is that it can cause upward displacement of the nipple-areolar complex, which results when too much skin is removed above the nipple. Grisotti36 denes a no mans land as the area in the upper inner quadrant and superior breast that is at the lateral edge of the pectoralis major muscle. A large skin resection in this area followed by dermoglandular-ap advancement including the nipple-areolar complex will shift the nipple in an upward or medial fashion that would look highly unnatural in location. Grisotti36 suggests that the areola should not be moved higher than 16 cm to the sternal notch or closer than 7 cm to midline. In the upper inner quadrant of the breast, excisions are typically best closed with a simple reapproximation of breast tissue and skin without removal of any skin island.
approach to wire localisation can make the difference between complete excisions with negative margins and the need for surgical re-excision. Multiple hooked wires can help dene the radiographic extent of the tumour, especially with large non-palpable calcic lesions.37 By use of bracketing wires, surgeons should attempt to excise the entire lesion within one piece of tissue. Complete excision should not be attempted by use of one guide wire with large lesions, especially when they contain DCIS, because it could result in incomplete removal. The bracketing-wire technique does not guarantee complete removal of the lesion, but makes this outcome more likely.11 Specimen radiography and orientation should be undertaken in wire-directed cases, because they can provide surgeons with accurate and immediate feedback as to the adequacy of excision. If mass lesions are seen by ultrasound, intraoperative ultrasound can be used to direct the parenchymal excision and assess the thoroughness of wide local excision.38 In some settings, intraoperative ultrasound can be used in place of wire localisation, if target lesions show a similar extent of disease on both mammography and ultrasound imaging.39
Parallelogram skin incision design
In oncoplastic resections that include overlying skin, a superior and inferior incision margin is created and closed mainly at the end of the operation. Ideally, the lengths of these two margins should be equal so that neither edge is bunched up at nal healing. Because the excision design is a rounded parallelogram, equal length of the two margins is assured (gure 3). The two skin incisions are tapered at the corners so that the two incision lines can approach each other asymptotically at the incision corner, keeping the V angle of the corner to a minimum. This so-called sh-tailing of the incision keeps to a minimum the degree to which the corners will protrude in a dog-ear fashion.40 Although standard lumpectomy use is reasonable for small cancers, the parallelogram approach will probably result in wider margins than the standard technique. The parallelogram lumpectomy also preserves the breast shape without leaving an underlying divot of tissue. Surgeons should not remove a large island of breast skin that shifts the nipple to create undesirable asymmetry. To avoid substantial shifting of the nipple-areolar complex, surgeons need to ensure that the ellipse of skin is not too broad compared with the length of incision.
Perimeter wire localisation, specimen radiography, and intraoperative ultrasound
Irrespective of the technique chosen for partial breast excision, accurate localisation of the lesion is important in surgical planning. When a lesion is nonpalpableeg, DCIS or invasive cancer after a good clinical response to preoperative chemotherapythe
Type of lumpectomy Batwing mastopexy Radial-segmental (quadrantectomy) Donut mastopexy Reduction mastopexy Tumour location Central breast Lateral breast Upper or lateral breast Lower breast Tumour distribution Localised Segmentally extended Segmentally extended Localised
Oncoplastic partial mastectomy procedures
Many cancers can be excised with good cosmetic results by application of the fundamental principles of oncoplastic surgery described so far. In some settings, special approaches can be advantageous and achieve good or excellent cosmesis at the same time as obtaining wide surgical margins (table).
http://oncology.thelancet.com Vol 6 March 2005
Table: Oncoplastic lumpectomy procedures of intermediate complexity
150
Review
Figure 4: Batwing mastopexy lumpectomy (A) Preoperative view. (B) Full-thickness excision. (C) Advancement of remaining broglandular tissue to close defect. (D) Final result at closure.
Batwing mastopexy
The batwing mastopexy is a surgical approach that is most ideal for cancers located deep within or adjacent to the nipple-areolar complex but not directly connected with the area (gure 4).11 Two closely similar half-circle incisions are made with angled wings to each side of the areola. Full-thickness excision is undertaken and the broglandular tissue is advanced to close the subsequent defect. This procedure will cause some lifting of the nipple, which can lead to asymmetry. However, in pendulous breasts, this effect might be deemed desirable by the patient. A contralateral lift can be undertaken afterwards to achieve symmetry. Viability of the areola is generally not at risk with batwing mastopexy. However, the extent of dissection behind the nipple restricts the degree of central dissection in the procedure. The blood supply of the external nipple arises from underlying broglandular tissue using major lactiferous sinuses rather than the collateral circulation from surrounding areolar skin. Thus, nipple necrosis could take place if dissection extends high up behind the nipple. Surgeons should carefully mark the edge of the specimen closest to the underside of the nipple if tumours are close to the areola. In some cases, the nipple-areolar complex will be found to be histologically associated with cancer. Because the batwing mastopexy relates to an incision that centres around the complex, the approach can be revised to a central lumpectomy in which the complex itself is resected, which preserves the breast mound shape well.18
http://oncology.thelancet.com Vol 6 March 2005
Radial-segmental lumpectomy (quadrantectomy)
The notion of segmental broglandular wide resection at full thickness that included skin was originally developed as the quadrantectomy developed by Veronesi and colleagues,41 which was a sentinel event in the evolution of breast-conserving treatment. Combination of a formal parenchymal quadrantectomy with ap advancement results in a radial-segmental lumpectomy (also called cosmetic quadrantectomy). In this procedure, a segmentally extended tumour on the lateral side of the breast is resected through a long skin incision that approaches the nipple-areolar complex tangentially in a radial rather than circumareolar orientation.42 With radial-excision lumpectomy, overlying skin is removed with the full-thickness broglandular excision to avoid excessive redundant skin and postoperative skin-pectoral adherence deformities, which preserves breast shape and appearance. An advantage of this approach is its ease in execution. A limitation is the length of radial incision and the necessity to cross both Langers and Kriesls lines of skin, with increasingly visible scarring (gure 5). Postoperative radiation therapy can sometimes shorten scars, but might cause nipple deviation towards the skin incision if undertaken with nipple-segmental lumpectomy.
Donut mastopexy lumpectomy
As an alternative to radial-segmental lumpectomy, the donut mastopexy lumpectomy is a unique breast resection in which a tissue segment is removed through a periareolar incision.5,43,44 This operation is especially
151
University of Washington
Review
Figure 5: Postoperative results of radial-excision lumpectomy or cosmetic quadrantectomy (A) Anterior-posterior view. (B) Lateral view.
effective for segmentally distributed cancers in the upper or lateral portion of the breast (gure 6). The donut mastopexy procedure is more technically challenging and time consuming than the radial approach, and uses a modied skin-sparing mastectomy in which only a segment of the breast is removed. Because the technique is a complex operation associated with such wide skin-sparing dissections, it should not be undertaken until basic oncoplastic techniques are fully understood and mastered. Initially, a donut of skin is excised around the nippleareolar complex with a Benelli-type round-block incision that is used as one technique in breast reduction surgery (gure 6A).45 The areola should be carefully separated from the underlying tissues to avoid devascularisation of the areolar skin. Removal of this tissue ring is needed to allow both adequate access to the breast tissue and closure of the skin envelope around the remaining broglandular tissue that will reduce tissue volume overall. A generous, segmentally oriented wedge of tissue is removed, including the entire breast tumour with adequate or generous surgical margins. The remaining broglandular tissue is returned to the skin envelope and sutured at deep and supercial margins to close the resulting defect (gure 6B). A purse-string closure around the nipple completes the procedure, leaving only a periareolar closure at the end of the operation (gures 6C and 6D). Because donut mastopexy lumpectomy needs more complex dissection than other techniques, it is generally reserved for more extensive, segmentally distributed cancers. As a result, most patients will undergo mastectomy if surgical margins of the donut mastopexy procedure are regarded as inadequate.
152
However, because the incision of this operation is exclusively periareolar, a skin-sparing total mastectomy with immediate ap reconstruction remains an excellent option for breast conservation.
Reduction mastopexy lumpectomy
Cancers in the lower region of the breast can be very difcult for cosmetic excision. Standard lumpectomy in this area can cause a down-turning of the nipple because of loss of tissue inferior to the nipple-areolar complex without associated breast-ap advancement. For lesions in the lower hemisphere of the breast (ie, 4 oclock to 8 oclock position, going clockwise), the same reduction incision that is undertaken in breast reduction mastopexy can also be used with good cosmetic results.8 Large amounts of breast tissue can be removed with excellent aesthetic outcomes and wide and clear margins (gure 7). Like donut mastopexy lumpectomy, reduction mastopexy lumpectomy is an advanced oncoplastic technique based on the basic skills of full-thickness excision and breast-ap advancement. Surgeons without specic oncoplastic training should be cautious in using this approach that maintains broglandular blood ow as a superior pedicle-based ap. An important limitation is that if positive surgical margins are seen, surgeons might regard the procedure as technically challenging to include both the initial incisions and nipple-areolar complex in a subsequent total mastectomy. Occurrence of substantial positive margins after the procedure in some patients suggests that these individuals had relatively large tumours and should have undergone mastectomy at the outset. However, this conclusion is
http://oncology.thelancet.com Vol 6 March 2005
Review
sometimes apparent only in retrospect when the nal pathology report becomes available. Correct patient selection is essential.
Additional margin excision
For every oncoplastic lumpectomy approach, the area of known disease should be removed with the intention of containing the entire region of disease. If the specimen is removed in many pieces rather than one, pathologists might nd denitive statements about the adequacy of surgical margins quite difcult to make. On the other hand, when painted on the lumpectomy margins, ink can run down between fat lobules of loosely adherent broglandular tissue into deeper portions of the initial surgical specimen, giving the erroneous impression of close or positive surgical margins. This inking artifact is alleviated if separately excised surgical margins ( 5 mm) are additionally taken at the edge of the cavity to represent the true breast margins. However, this technique should be used sparingly, since condence in the accuracy of this additional resection is subjective and such surgical margin excision can be incomplete.
Multicoloured specimen inking
Operating surgeons can best dene correct specimen orientation at the time of surgical excision. The commonly used technique of suture marking (in which long stitches represent the lateral side and short
stitches indicate the superior side) leaves much to be desired, because specimens can be greatly altered during radiography before they are given to pathologists. Multicoloured inking kits are now available with six colours (black, blue, yellow, green, orange, and red) and are very useful for labelling of margins (superior, inferior, medial, lateral, supercial, and deep). Some tumours excised with oncoplastic techniques have complex shapes and are not cubic pieces of tissue. Orientation of the tissue with respect to the breast anatomy is best understood by operating surgeons. If these surgeons personally ink the specimen, they will have much improved condence for correct orientation if margin issues arise. After inking the specimen, surgeons need to apply acetic acid or a similar xative available, to avoid the running of ink during transport. Careful margin inking has shown to be associated with improved outcome as measured by residual tumours in the breast.46 With full-thickness excisions, the supercial and deep margins are already taken in the mastectomy plane, and therefore would not be improved by additional surgery. Surgeons can accurately paint these mastectomy-plane margins, which could help avoid additional and unnecessary re-excision before radiation treatment. However, to adopt an intraoperative inking protocol, a collaborative agreement needs to be established between surgeons and pathologists to avoid misunderstanding or miscommunication.
Figure 6: Donut mastopexy lumpectomy (A) Periareolar incision and removal of skin donut. (B) Full-thickness excision of broglandular tissue and cancer. (C) Purse-string skin closure. (D) Final result at closure.
http://oncology.thelancet.com Vol 6 March 2005
153
Review
Figure 7: Breast reduction lumpectomy (A) Preoperative image of lower pole cancer at 6 oclock position showing tenting of breast skin overlying an invasive cancer. (B) Skin marking indicating location of cancer and design of operative incision. (C) Intraoperative development of incision before broglandular excision. (D) Final result at closure.
Re-excision lumpectomy
If reoperation is needed for positive surgical margins, surgeons must consider both the surgical approach and timing of the operation. In some instances, use of the same incision is feasible. In others, a new incision and lumpectomy need to be done, which has a technical advantage by allowing some time for healing of the previous excision. If re-excision is delayed for 34 weeks, the previous seroma cavity is nearly reabsorbed, which leaves a brous biopsy cavity that can be easily located by intraoperative palpation. When positive margins are restricted in extent, as can best be determined with differential multicoloured inking, the entire biopsy cavity does not need re-excision. Instead, one or two margins of the previous biopsy cavity can be taken.
154
When all the margins are positive, mastectomy will probably be needed to attain satisfactory surgical clearance. With non-invasive cancer, some surgeons will delay re-excision for 34 months, at which point the seroma cavity has fully reabsorbed. These surgeons think that this approach can yield the best cosmetic outcome after resection.11 It is noteworthy that in a study of specimens removed in a delayed fashion, fewer cases were seen to contain residual carcinoma than for those removed immediately, presumably because of brosis.47 These ndings suggest that local acute repair mechanisms might be responsible for the destruction of up to 50% of the residual tumour load and could complement the cytocidal effects of radiotherapy. This effect was apparent within 2 months (1369 days).
http://oncology.thelancet.com Vol 6 March 2005
Review
Selection of oncoplastic operative approach
Masetti and colleagues5 described four steps to the design of an oncoplastic operation (panel). During excision of segmentally extended or irregularly extended lesions, surgeons face two opposing goals: establishment of widely clear margins and achievement of acceptable cosmetic results. From an oncological point of view, the largest specimen possible should be removed to achieve the widest possible margins. From a cosmetic point of view, a much smaller amount of tissue should be removed. The rst attempt to remove cancerous lesions is critical; it offers the best chance to remove the entire lesion in one piece, assess its extent and margin status, and achieve the best possible cosmetic result.
Panel: Four-step design of oncoplastic operations 1 Planning of skin incisions and parenchymal excisions following templates used for reduction mammoplasty and mastopexy 2 Reshaping of the gland after parenchymal excision 3 Repositioning of nipple-areolar complex to the centre of new breast mound 4 Correction of contralateral breast to improve symmetry
Localised breast cancers
For small localised cancers, a standard lumpectomy technique can be used. This procedure is best applied for treatment of tumours in the upper breast. In the lower breast, standard lumpectomies are notoriously unsuccessful from a cosmetic standpoint, because removal of large areas of breast tissue under the nipple-areolar complex without some type of oncoplastic closure causes the nipple to turn downwards, which both fails to resemble the typical breast anatomy and eliminates symmetry between both breasts. Surgeons who are familiar with the parallelogram full-thickness approach to oncoplastic lumpectomy might regard the standard approach as unappealing in many circumstances. With large localised cancers, the parallelogram technique is a great improvement because they can be removed effectively with widened surgical margins.
any subsequent operation, including skin-sparing mastectomy with immediate reconstruction, remains a viable option if surgical margins are seen to be positive. A disadvantage is that the operation is more timeconsuming than other approaches, and needs cautious technique to avoid devascularisation of the breast gland at its posterior aspect by inadvertent division of perforating vessels from the pectoralis muscle.
Irregularly extended breast cancers
Irregularly extended cancers might be the least amenable to breast conservation unless they are small. Although breast conservation is ideal and desirable, it might be achievable with these tumours only if they develop in very large breasts. The fact that irregularly extended cancers could be less amenable to breast conservation is not because of lesions crossing anatomical boundaries between breast segments. Instead, irregularly extended cancers tend to have aggressive growth characteristics associated with local extension in the breast that prohibits resection with negative margins using any operation smaller than mastectomy. Ultimately, mastectomy is an important and sometimes necessary approach to properly treat the cancer. Good cosmetic surgery should not be used as an excuse for inadequate surgical excision and proper cancer therapy.
Segmentally extended breast cancers
If breast imaging indicates that a tumour is oriented in a segmental fashion, surgeons should consider using an oncoplastic approach that allows generous fullthickness excision of the related segment or quadrant. The radial-segmental excision achieves this goal if the breast tumour is in the lateral or upper outer quadrant. The advantage of this approach is its technical ease. However, the dermal cosmetic outcome might not be the best, because excisions can cross Langers lines and cause nipple deviation if the procedure foreshortens with radiation treatment. Medial repositioning of the nipple-areolar complex at primary resection can prevent such deviation. The donut mastopexy is especially well suited for removal of segmentally extended cancers in the lateral or upper outer quadrant, since it allows dissection from the nipple-areolar complex out to the periphery. The donut mastopexy also produces good or excellent results with segmentally extended cancers in the upper breast at the 12 oclock position. An advantage of the technique is that because it uses a periareolar incision,
http://oncology.thelancet.com Vol 6 March 2005
Contralateral breast reduction
Contralateral breast reduction can be undertaken at the same or later time as the initial lumpectomy,48 which can be especially advantageous if a woman has macromastia.49 The major advantage of simultaneous breast reduction is that it can avoid further surgery when the cancer is successfully removed with clear margins and can achieve excellent or outstanding cosmetic results. Some surgeons have incorporated contralateral breast reduction into their practices with very acceptable results.5 Other investigators recommend that surgery on the opposite breast be withheld until nal pathology, especially if the margin status is known. If positive margins are encountered during nal analysis, re-excision or mastectomy will need to be done, at which point the contralateral reduction could prove inadequate. Furthermore, the ipsilateral breast will need to undergo radiotherapy
155
Review
11
Search strategy and selection criteria
12
Data for this review were identied by searches of PubMed and references from relevant articles by use of the search terms "oncoplastic surgery" and "breast cancer" or "partial mastectomy" and "cosmetic outcome". Abstracts and reports from meetings were included only when they related directly to previously published work. Only papers published between 1988 and 2004 were included.
13 14 15
16
after successful lumpectomy, which itself could increase breast asymmetry when contralateral reduction is undertaken in the same procedure as the lumpectomy. These issues should be discussed extensively with patients in the planning of an oncoplastic procedure so that they understand the risks and benets of immediate versus delayed contralateral breast reduction.
17
18
19
20
Conclusions
Oncoplastic partial mastectomy with full-thickness excision and removal of overlying skin can be done by surgeons without formal training in plastic surgery but with additional help. The approach needs forethought and planning but is technically achievable with relative ease. Surgical results both from cosmetic and oncological views are desirable. Once surgeons begin to adopt these procedures, they will nd modications and approaches that can be adapted to unique situations. Ultimately, the care of women with breast cancer can be improved with increased satisfaction for both patients and surgeons.
Conict of interest We declare no conicts of interest. References 1 Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 2002; 347: 123341. 2 Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 2002; 347: 122732. 3 Schover LR. Sexuality and body image in younger women with breast cancer. J Natl Cancer Inst Monogr 1994: 17782. 4 Schrenk P. Surgical and plastic reconstructive therapy of breast carcinoma. Wien Med Wochenschr 2000; 150: 6371. 5 Masetti R, Pirulli PG, Magno S, et al. Oncoplastic techniques in the conservative surgical treatment of breast cancer. Breast Cancer 2000; 7: 27680. 6 Benson JR, Querci della Rovere G. Towards a scientic basis for oncoplastic breast surgery. Eur J Surg Oncol 2003; 29: 629. 7 Brown IM, Wilson CR, Doughty JC, et al. The future of breast surgery: a new sub-speciality of oncoplastic breast surgeons? Breast 2004; 13: 82. 8 Clough KB, Lewis JS, Couturaud B, et al. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg 2003; 237: 2634. 9 Mustonen P, Harma M. Viewpoints on oncoplastic surgery in invasive breast cancer. Scand J Surg 2002; 91: 255, 25862. 10 Skillman JM, Humzah MD. The future of breast surgery: a new subspecialty of oncoplastic breast surgeons? Breast 2003; 12: 16162. 27 21
22 23 24 25
26
28
29
30
31
32
33
34
Silverstein MJ. An argument against routine use of radiotherapy for ductal carcinoma in situ. Oncology (Huntingt) 2003; 17: 151133. Rew DA. Towards a scientic basis for oncoplastic breast surgery. Eur J Surg Oncol 2003; 29: 10506. Baum M. Is it time for a paradigm shift in the training of breast surgeons as a sub-speciality? Breast 2003; 12: 15960. Rainsbury RM. Training and skills for breast surgeons in the new millennium. Aust N Z J Surg 2003; 73: 51116. Amano G, Ohuchi N, Ishibashi T, et al. Correlation of threedimensional magnetic resonance imaging with precise histopathological map concerning carcinoma extension in the breast. Breast Cancer Res Treat 2000; 60: 4355. Holland R, Schuurmans Stekhoven JH, et al. Extent, distribution, and mammographic/histological correlations of breast ductal carcinoma in situ. Lancet 1990; 335: 51922. Holland R, Faverly DRG. Whole-organ studies. In: Silverstein MJ, ed. Ductal carcinoma in situ of the breast. Baltimore: Williams & Wilkins, 1997: 23340. Pezzi CM, Kukora JS, Audet IM, et al. Breast conservation surgery using nipple-areolar resection for central breast cancers. Arch Surg 2004; 139: 3237. Holland R, Hendriks JH. Microcalcications associated with ductal carcinoma in situ: mammographic-pathologic correlation. Semin Diagn Pathol 1994; 11: 18192. Page DL, Dupont WD, Rogers LW, et al. Continued local recurrence of carcinoma 1525 years after a diagnosis of low grade ductal carcinoma in situ of the breast treated only by biopsy. Cancer 1995; 76: 1197200. Boetes C, Mus RD, Holland R, et al. Breast tumors: comparative accuracy of MR imaging relative to mammography and US for demonstrating extent. Radiology 1995; 197: 74347. Boetes C, Veltman J, van Die L, et al. The role of MRI in invasive lobular carcinoma. Breast Cancer Res Treat 2004; 86: 3137. Bluemke DA, Gatsonis CA, Chen MH, et al. Magnetic resonance imaging of the breast prior to biopsy. JAMA 2004; 292: 273542. Van Ongeval C. MR imaging of the breastpresent indications. JBR-BTR 2000; 83: 8084. Trecate G, Tess JD, Vergnaghi D, et al. Breast microcalcications studied with 3D contrast-enhanced high-eld magnetic resonance imaging: more accuracy in the diagnosis of breast cancer. Tumori 2002; 88: 22433. Krishnan L, Stanton AL, Collins CA, et al. Form or function? Part 2. Objective cosmetic and functional correlates of quality of life in women treated with breast-conserving surgical procedures and radiotherapy. Cancer 2001; 91: 228287. Stanton AL, Krishnan L, Collins CA. Form or function? Part 1. Subjective cosmetic and functional correlates of quality of life in women treated with breast-conserving surgical procedures and radiotherapy. Cancer 2001; 91: 227381. Asgeirsson KS, McCulley SJ, Pinder SE, Macmillan RD. Size of invasive breast cancer and risk of local recurrence after breastconservation therapy. Eur J Cancer 2003; 39: 246269. Kerlikowske K, Molinaro A, Cha I, et al. Characteristics associated with recurrence among women with ductal carcinoma in situ treated by lumpectomy. J Natl Cancer Inst 2003; 95: 1692702. Schmidt-Ullrich R, Wazer DE, Tercilla O, et al. Tumor margin assessment as a guide to optimal conservation surgery and irradiation in early stage breast carcinoma. Int J Radiat Oncol Biol Phys 1989; 17: 73338. Bulstrode NW, Shrotria S. Prediction of cosmetic outcome following conservative breast surgery using breast volume measurements. Breast 2001; 10: 12426. Cochrane RA, Valasiadou P, Wilson AR, et al. Cosmesis and satisfaction after breast-conserving surgery correlates with the percentage of breast volume excised. Br J Surg 2003; 90: 150509. Brunnert KE. The Osnabrueck experience with reconstruction of the partial mastectomy defect. In: Spear SL, ed. Surgery of the breast: principles and art. Philadelphia: Lippincott-Raven, 1998: 197220. Chang DW, Beahm EK. Reconstructive strategies in breast conserving therapy. In: Singletary SE, Robb GL, Hortobagyi GN, eds. Advanced therapy of breast disease. 2nd edn. Hamilton, Ontario: BC Decker, 2004: 39096.
156
http://oncology.thelancet.com Vol 6 March 2005
Review
35
36
37
38
39
40 41
42
43
Hoffman S. Inferior pedicle technique in breast reduction. In: Spear SL, ed. Surgery of the breast: principles and art. Philadelphia: Lippincott-Raven, 1998: 76172. Grisotti A. Conservation treatment of breast cancer: reconstructive problems. In: Spear SL, ed. Surgery of the breast: principles and art. Philadelphia: Lippincott-Raven, 1998: 13753. Liberman L, Kaplan J, Van Zee KJ, et al. Bracketing wires for preoperative breast needle localization. AJR Am J Roentgenol 2001; 177: 56572. Kaufman CS, Jacobson L, Bachman B, Kaufman LB. Intraoperative ultrasonography guidance is accurate and efcient according to results in 100 breast cancer patients. Am J Surg 2003; 186: 37882. Rahusen FD, Bremers AJ, Fabry HF, et al. Ultrasound-guided lumpectomy of nonpalpable breast cancer versus wire-guided resection: a randomized clinical trial. Ann Surg Oncol 2002; 9: 99498. Shrotria S. Techniques for improving the cosmetic outcome of breast conservation surgery. Eur J Surg Oncol 2001; 27: 10912. Veronesi U, Luini A, Galimberti V, Zurrida S. Conservation approaches for the management of stage I/II carcinoma of the breast: Milan Cancer Institute trials. World J Surg 1994; 18: 7075. Senofsky GM, Gierson ED, Craig PH, et al. Local excision, lumpectomy, and quadrantectomy: surgical considerations. In: Spear SL, ed. Surgery of the breast: principles and art. Philadelphia: Lippincott-Raven, 1998: 12935. Amanti C, Moscaroli A, Lo Russo M, et al. Periareolar
44
45
46
47
48
49
subcutaneous quadrantectomy: a new approach in breast cancer surgery. G Chir 2002; 23: 44549. Amanti C, Regolo L, Moscaroli A, et al. Total periareolar approach in breast-conserving surgery. Tumori 2003; 89 (suppl 4): 16972. Benelli LC. Periareolar Benelli mastopexy and reduction: the Round Block. In: Spear SL, ed. Surgery of the breast: principles and art. Philadelphia: Lippincott-Raven, 1998: 68596. Neuschatz AC, DiPetrillo T, Steinhoff M, et al. The value of breast lumpectomy margin assessment as a predictor of residual tumor burden in ductal carcinoma in situ of the breast. Cancer 2002; 94: 191724. Nasir N, Rainsbury RM. The timing of surgery affects the detection of residual disease after wide local excision of breast carcinoma. Eur J Surg Oncol 2003; 29: 71820. Petit JY, Garusi C, Greuse M, et al. One hundred and eleven cases of breast conservation treatment with simultaneous reconstruction at the European Institute of Oncology (Milan). Tumori 2002; 88: 4147. Newman LA, Kuerer HM, McNeese MD, et al. Reduction mammoplasty improves breast conservation therapy in patients with macromastia. Am J Surg 2001; 181: 21520.
http://oncology.thelancet.com Vol 6 March 2005
157
Das könnte Ihnen auch gefallen
- Oncoplastic Breast SurgeryDokument27 SeitenOncoplastic Breast SurgeryReem Amr El-DafrawiNoch keine Bewertungen
- Incision in Breast Oncoplastic SurgeryDokument26 SeitenIncision in Breast Oncoplastic Surgeryccmcshh surgeryNoch keine Bewertungen
- Oncoplastic and Reconstructive BreastDokument14 SeitenOncoplastic and Reconstructive BreastYefry Onil Santana Marte100% (1)
- Oncoplastic Breast SurgeryDokument20 SeitenOncoplastic Breast SurgeryGeorge Yacoup100% (1)
- Breast Augmentation Mentor and Eurosilicone ImplantsDokument5 SeitenBreast Augmentation Mentor and Eurosilicone ImplantsSecret SurgeryNoch keine Bewertungen
- The Guide to Breast Reconstruction: Step-By-Step from Mastectomy Through ReconstructionVon EverandThe Guide to Breast Reconstruction: Step-By-Step from Mastectomy Through ReconstructionBewertung: 4 von 5 Sternen4/5 (1)
- Breast Cancer Radiation TherapyDokument439 SeitenBreast Cancer Radiation TherapyJuan RivasNoch keine Bewertungen
- Pouchitis and Ileal Pouch Disorders: A Multidisciplinary Approach for Diagnosis and ManagementVon EverandPouchitis and Ileal Pouch Disorders: A Multidisciplinary Approach for Diagnosis and ManagementNoch keine Bewertungen
- National Oncoplastic Breast FellowshipDokument3 SeitenNational Oncoplastic Breast Fellowshipplastauk100% (1)
- Breast AugmentationDokument7 SeitenBreast AugmentationnikitagustiNoch keine Bewertungen
- Abdominal Organ Transplantation: State of the ArtVon EverandAbdominal Organ Transplantation: State of the ArtNizam MamodeNoch keine Bewertungen
- Innovative Radiotherapy Techniques for Prostate CancerVon EverandInnovative Radiotherapy Techniques for Prostate CancerNoch keine Bewertungen
- A.Valeri Et Al - Surgery of The Adrenal Gland - 2013Dokument200 SeitenA.Valeri Et Al - Surgery of The Adrenal Gland - 2013Sergiu FedoretNoch keine Bewertungen
- London Cancer Breast Radiotherapy Guidelines 2017 Version 4Dokument17 SeitenLondon Cancer Breast Radiotherapy Guidelines 2017 Version 4Novi WiarniNoch keine Bewertungen
- Use of Retroauricular Temporal Flap For Large Post Oncosurgical Glabellar and Forehead DefectsDokument4 SeitenUse of Retroauricular Temporal Flap For Large Post Oncosurgical Glabellar and Forehead DefectsPalwasha Malik100% (1)
- 2023 OB/GYN Coding Manual: Components of Correct CodingVon Everand2023 OB/GYN Coding Manual: Components of Correct CodingNoch keine Bewertungen
- Breast Reconstruction Seminar FinalDokument62 SeitenBreast Reconstruction Seminar FinalSumi TranNoch keine Bewertungen
- 4 Oral Cavity ProceduresDokument10 Seiten4 Oral Cavity ProceduresAnne MarieNoch keine Bewertungen
- Surgical Principles in Inguinal Hernia Repair: A Comprehensive Guide to Anatomy and Operative TechniquesVon EverandSurgical Principles in Inguinal Hernia Repair: A Comprehensive Guide to Anatomy and Operative TechniquesMelissa Phillips LaPinskaNoch keine Bewertungen
- Current Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderVon EverandCurrent Challenges with their Evolving Solutions in Surgical Practice in West Africa: A ReaderNoch keine Bewertungen
- Augmentasi Mammae & MastopexyDokument52 SeitenAugmentasi Mammae & MastopexySitha ChristineNoch keine Bewertungen
- Gastrointestinal Oncology - J. Abbruzzese, Et Al., (Oxford, 2004) WW PDFDokument938 SeitenGastrointestinal Oncology - J. Abbruzzese, Et Al., (Oxford, 2004) WW PDFRaluca MărgulescuNoch keine Bewertungen
- 2014 Breast Surgery A Companion To SpecialistDokument99 Seiten2014 Breast Surgery A Companion To Specialiststeve shrimp100% (1)
- Abdominalkey Com Hartmanns ResectionDokument5 SeitenAbdominalkey Com Hartmanns ResectionAnonymous RFVIG7IaNoch keine Bewertungen
- The Bethesda System for Reporting Thyroid Cytopathology: Definitions, Criteria and Explanatory NotesVon EverandThe Bethesda System for Reporting Thyroid Cytopathology: Definitions, Criteria and Explanatory NotesNoch keine Bewertungen
- Breast Cancer Atlas of Clinical Oncology PDFDokument300 SeitenBreast Cancer Atlas of Clinical Oncology PDFPanuta AndrianNoch keine Bewertungen
- Urinary System: Cytology, Histology, Cystoscopy, and RadiologyVon EverandUrinary System: Cytology, Histology, Cystoscopy, and RadiologyNoch keine Bewertungen
- Diagnostic Laparoscopy in Penetrating Abdominal TraumaDokument4 SeitenDiagnostic Laparoscopy in Penetrating Abdominal TraumaNicolás Joel Peñalosa CupajitaNoch keine Bewertungen
- Breast Cancer The LANCET Abril 2021Dokument20 SeitenBreast Cancer The LANCET Abril 2021Hernán Salazar RománNoch keine Bewertungen
- 2022 Modern Breast Cancer ImagingDokument466 Seiten2022 Modern Breast Cancer ImagingBeagabcn100% (2)
- Surgical Endoscopy Journal 1Dokument86 SeitenSurgical Endoscopy Journal 1Saibo BoldsaikhanNoch keine Bewertungen
- Surgical Anatomy and Operative Technique of The Axillary Lymph Node Dissection.Dokument5 SeitenSurgical Anatomy and Operative Technique of The Axillary Lymph Node Dissection.juanrangone100% (2)
- Ambulatory Anorectal SurgeryDokument234 SeitenAmbulatory Anorectal SurgeryHermina DicuNoch keine Bewertungen
- Chemotherapy and targeted therapy in pancreatic cancerVon EverandChemotherapy and targeted therapy in pancreatic cancerNoch keine Bewertungen
- Essentials CompleteDokument66 SeitenEssentials CompleteNovriman LiviaNoch keine Bewertungen
- Breast Cancer DetectionDokument5 SeitenBreast Cancer DetectionalexlingmanchesterNoch keine Bewertungen
- The Role of Radiotherapy in Cancer TreatmentDokument9 SeitenThe Role of Radiotherapy in Cancer TreatmentarakbaeNoch keine Bewertungen
- Breast Cancer - Use of Screening Strategies For The Detection of Breast CancerDokument71 SeitenBreast Cancer - Use of Screening Strategies For The Detection of Breast Canceriyad.alsabiNoch keine Bewertungen
- (Comprehensive Gynecology and Obstetrics) Hidetaka Katabuchi (Eds.) - Frontiers in Ovarian Cancer Science-Springer Singapore (2017)Dokument313 Seiten(Comprehensive Gynecology and Obstetrics) Hidetaka Katabuchi (Eds.) - Frontiers in Ovarian Cancer Science-Springer Singapore (2017)Suci NopitriNoch keine Bewertungen
- Sentinel Lymph Node ConceptDokument27 SeitenSentinel Lymph Node ConceptKarthikeyan RadhakrishnanNoch keine Bewertungen
- A System of Operative Surgery, Volume IV (of 4)Von EverandA System of Operative Surgery, Volume IV (of 4)Bewertung: 4 von 5 Sternen4/5 (1)
- Atlas of Trauma: Operative Techniques, Complications and ManagementVon EverandAtlas of Trauma: Operative Techniques, Complications and ManagementPaula FerradaNoch keine Bewertungen
- Breast SarcomaDokument4 SeitenBreast SarcomaMinh Thư DươngNoch keine Bewertungen
- Breast Cancer in Women - A Narrative Literature ReviewDokument7 SeitenBreast Cancer in Women - A Narrative Literature ReviewAnnie McSolsticeNoch keine Bewertungen
- WeBSurg Winners 42 1Dokument129 SeitenWeBSurg Winners 42 1Ana Adam100% (1)
- Breast Reconstruction - Current TechniquesDokument288 SeitenBreast Reconstruction - Current Techniquesamirekhalili1100% (1)
- Mohsmicrographic Surgerytechnique: Paul X. Benedetto,, Christine Poblete-LopezDokument11 SeitenMohsmicrographic Surgerytechnique: Paul X. Benedetto,, Christine Poblete-LopezDaniel Holthausen NunesNoch keine Bewertungen
- Pediatric Urology: Surgical Complications and ManagementVon EverandPediatric Urology: Surgical Complications and ManagementNoch keine Bewertungen
- Breast Cancer Risk Assessment and Genetic TestingDokument58 SeitenBreast Cancer Risk Assessment and Genetic TestingSahirNoch keine Bewertungen
- Safe CholecystectomyDokument60 SeitenSafe CholecystectomyCarlos Reyes100% (1)
- Proceeding 2018 PDFDokument312 SeitenProceeding 2018 PDFashish gaurNoch keine Bewertungen
- GI Surgery Annual Volume 23 2017Dokument247 SeitenGI Surgery Annual Volume 23 2017Antonov RAJAONARYNoch keine Bewertungen
- Surgery For Recurrent Soft Tissue SarcomaDokument584 SeitenSurgery For Recurrent Soft Tissue SarcomaAr-pardo RogerNoch keine Bewertungen
- Breast Sonography: Gopal KhanalDokument96 SeitenBreast Sonography: Gopal KhanalDr KhanNoch keine Bewertungen
- Oral Meds ChecklistDokument2 SeitenOral Meds ChecklistMonika Sarmiento100% (1)
- Persepsi Mahasiswi Tentang Kanker Payudara Dan Perilakunya Terhadap Pencegahan Kanker Payudara Di Fakultas Keperawatan Universitas AndalasDokument8 SeitenPersepsi Mahasiswi Tentang Kanker Payudara Dan Perilakunya Terhadap Pencegahan Kanker Payudara Di Fakultas Keperawatan Universitas AndalasAfifah AzhariNoch keine Bewertungen
- Tobacco Lesson PlanDokument4 SeitenTobacco Lesson Planapi-240857737Noch keine Bewertungen
- FAQ On Blood DonationDokument2 SeitenFAQ On Blood DonationAnilNoch keine Bewertungen
- Cure Gum Disease Naturally: Heal and Prevent Periodontal Disease and Gingivitis With Whole Foods - Ramiel NagelDokument5 SeitenCure Gum Disease Naturally: Heal and Prevent Periodontal Disease and Gingivitis With Whole Foods - Ramiel Nageljopupima50% (4)
- PediatricsDokument33 SeitenPediatricsnageshwarioshNoch keine Bewertungen
- FHTMonitoringDokument21 SeitenFHTMonitoringlaarnie100% (1)
- 10a. HipoksiaDokument21 Seiten10a. HipoksiaputrianitaNoch keine Bewertungen
- Drug Study of Antidiabetic DrugsDokument6 SeitenDrug Study of Antidiabetic DrugsLorina Lynne ApelacioNoch keine Bewertungen
- Elderly PrimigravidaDokument5 SeitenElderly PrimigravidaDeepti Kukreti100% (5)
- Case of A Patient Having Congestive Heart FailureDokument13 SeitenCase of A Patient Having Congestive Heart Failuresykie joy albina100% (1)
- Infection PreventionDokument38 SeitenInfection PreventionAmanda ScarletNoch keine Bewertungen
- ARTG Summary For Health NavigatorDokument2 SeitenARTG Summary For Health NavigatorinergetixNoch keine Bewertungen
- Catheter Care and MaintenanceDokument4 SeitenCatheter Care and MaintenanceSha BtstaNoch keine Bewertungen
- Cannabis Versus Rx-AntidepressantsDokument2 SeitenCannabis Versus Rx-AntidepressantsDimitri HalleyNoch keine Bewertungen
- Bacte01 STREPTOCOCCUS ENTEROCOCCUSDokument8 SeitenBacte01 STREPTOCOCCUS ENTEROCOCCUSAngelic AngelesNoch keine Bewertungen
- Immunity (Lecture Notes)Dokument5 SeitenImmunity (Lecture Notes)Anisha NishanthNoch keine Bewertungen
- Infopia Clover A1cDokument31 SeitenInfopia Clover A1cAde NasutionNoch keine Bewertungen
- Allergies: A Protective Mechanism Out of ControlDokument29 SeitenAllergies: A Protective Mechanism Out of Controlडा. सत्यदेव त्यागी आर्यNoch keine Bewertungen
- Aceclofenac 100 MG Film-Coated Tablets - Summary of Product Characteristics (SMPC) - Print Friendly - (eMC) PDFDokument9 SeitenAceclofenac 100 MG Film-Coated Tablets - Summary of Product Characteristics (SMPC) - Print Friendly - (eMC) PDFHabibNoch keine Bewertungen
- Episode ListDokument25 SeitenEpisode ListhectorNoch keine Bewertungen
- Ngo Module 1aDokument7 SeitenNgo Module 1aAmiel simon NgoNoch keine Bewertungen
- Combinazioni SSC Unico PDFDokument73 SeitenCombinazioni SSC Unico PDFGiovanni PasqualiniNoch keine Bewertungen
- Questionário Ii - Fundamentos Etimológicos Do InglêsDokument4 SeitenQuestionário Ii - Fundamentos Etimológicos Do InglêsDébora Bandeira David100% (1)
- Reproductive Arranged (MedicalBooksVN - Com)Dokument63 SeitenReproductive Arranged (MedicalBooksVN - Com)Rabooh AyashiNoch keine Bewertungen
- Rule 15Dokument2 SeitenRule 15begenyolNoch keine Bewertungen
- Bühler Heim 2018 General Introduction To The Psychotherapy of Pierre JanetDokument18 SeitenBühler Heim 2018 General Introduction To The Psychotherapy of Pierre JanetsammyNoch keine Bewertungen
- Pedia-Formulas and DripsDokument6 SeitenPedia-Formulas and DripsNerak LuNoch keine Bewertungen
- Hyperbilirubinemia: West Visayas State University College of Medicine Neonatal Intensive Care UnitDokument49 SeitenHyperbilirubinemia: West Visayas State University College of Medicine Neonatal Intensive Care UnitDonna LabaniegoNoch keine Bewertungen
- FLCCC Alliance I RECOVER Management Protocol For Long Haul COVID 19 SyndromeDokument3 SeitenFLCCC Alliance I RECOVER Management Protocol For Long Haul COVID 19 SyndromeAizaz ul HaqNoch keine Bewertungen