Beruflich Dokumente
Kultur Dokumente
OTT Microangiopatia
Hochgeladen von
victorcabanellasOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
OTT Microangiopatia
Hochgeladen von
victorcabanellasCopyright:
Verfügbare Formate
Cancer-Associated Hemolytic-Uremic Syndrome: Analysis of 85 Cases From a National Registry
By J. Bancroft Lesesne, Neal Rothschild, Beth Erickson, Stefan Korec, Regina Sisk, James Keller, Marvin Arbus, Paul V. Woolley, Leonard Chiazze, Philip S. Schein, and John R. Neefe
A registry of suspected cases of cancer-associated hemolytic-uremic syndrome (C-HUS) was established in May 1984. Records of 85 patients from the registry, all with history of cancer, hematocrit s 25%, platelet count < 100,000, and serum creatinine ! 1.6 mg/dL were subjected to in-depth analysis. Eighty-nine percent of patients had adenocarcinoma, including 26% with gastric cancer. Microangiopathic hemolysis was reported in 83 patients; coagulation studies were normal with rare exception. Bone marrow examination ruled out chemotherapy-induced myelosuppression in 68 of 85. Thirty-five percent of patients were without evident cancer at time of syndrome development. Mitomycin (MMC) was part of the treatment regimen in 84 patients; all but nine received a cumulative dose > 60 mg. Pulmonary edema, generally noncardiogenic, developed in 65% of patients, often after blood product transfusions. C-HUS has a high mortality: over 50% of patients died of or with syndrome, most within 8 weeks of syndrome development. Conventional treatment was ineffective, although ten of 21 treated with staphylococcal protein A (SPA) immunopheresis showed significant responses. Statistical analysis found only absence of obvious tumor and treatment with SPA to suggest favorable prognosis. C-HUS is distinguishable from related syndromes such as childhood HUS, thrombotic thrombocytopenic purpura (TTP), consumption coagulopathy, and microangiopathic hemolysis associated with advanced carcinoma. MMC is likely involved in the development of C-HUS; the risk of developing C-HUS after treatment with MMC is between 4% and 15%. However, possible bias in patients referred to the registry and reports of non-MMC C-HUS cases must be remembered. Recommendations include careful monitoring of renal and hematologic function in patients treated with MMC, aggressive nontransfusion in patients with suspected C-HUS, and consideration of treatment with SPA immunopheresis in patients with definite syndrome. J Clin Oncol 7:781-789. @ 1989 by American Society of ClinicalOncology.
RECENT YEARS the complex of microangiopathic hemolytic anemia, thrombocytopenia, and renal dysfunction has been recognized in some patients with malignancies treated with chemotherapeutic agents. As cases were reported in the literature, certain characteristics of this syndrome were frequently observed. These included presence of adenocarcinoma (especially gastrointestinal), partial to complete response of tumor to treatment, use of mitomycin (MMC) in the therapeutic regimen, noncardiogenic pulmonary edema or exacerbation of other syndrome components with blood product transfusions, and poor response to syndrome treatment with significant mortality.' The clinical characteristics specific to the syndrome are reflected in the various names ascribed to this disease entity: MMCinduced hemolytic-uremic syndrome (HUS), MMC-associated renal failure, HUS/thrombotic thrombocytopenic purpura (TTP), thrombotic microangiopathy and renal failure associated with antineoplastic chemotherapy, and carcinoma (or cancer)-associated C-HUS.'" In
IN
order better to define this syndrome with regard to causality, clinical parameters, prognosis, and treatment response, a registry of patients suspected of having C-HUS was established at Georgetown University/Lombardi Cancer Center in May 1984. Characteristics of 12 of these patients were previously published.! This report represents an analysis of 140 patients from 29 states and two foreign countries entered into the registry through November 1986.
From the Division of Medical Oncology. Department of Medicine, Vincent T. Lombardi Cancer Research Center, Georgetown University, Washington, DC;and Bristol MyersUSPG, Evansville, IN. Submitted April 19. 1988; accepted January3, 1989. Dr Lesesne's present address is Georgia Oncology Hematology Clinic,Atlanta;Dr Schein'spresent addressis University of Pennsylvania, Philadelphia; Neefe's present adDr dress is Lucille ParkerMarkey Cancer Center, University of Kentucky, Lexington. Address reprintrequests to John R. Neefe, MD, Division of Hematology/Oncology, Lucille Parker Markey Cancer Center,University of Kentucky, Lexington, KY40536. 1989 by American Society of Clinical Oncology. 0732-183X/89/0706-0012$3.00/0
Journalof ClinicalOncology, Vol 7, No 6 (June), 1989: pp 781-789
781
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
782 MATERIALS AND METHODS DataAcquisition
The C-HUS Registry was established at Georgetown University with the assistance of Bristol Laboratories, Syracuse, NY, currently Bristol Myers-USPG, Evansville, IN. Information about the syndrome and requests for referral of suspected cases of C-HUS to the registry have been disseminated in widely circulated medical journals (eg, Annals of Internal Medicine and Journal of Clinical Oncology), in literature distributed to physicians, and through presentations at the American Society of Clinical Oncology annual meetings. These media provide telephone numbers for both the Office of Medical Information at Bristol Laboratories and the C-HUS Registry at Georgetown University. Bristol (manufacturer of MMC) receives inquiries regarding MMC toxicity from physicians and copies of adverse drug reports sent to the Food and Drug Administration. Many patients registered were initially referred through one of these sources. Thus, patient accrual is passive, and cases may be brought to the attention of the registry directly by physicians aware of its existence or indirectly through Bristol Myers-USPG. When a possible case of C-HUS is referred to the registry, the registry physician requests information by telephone from the referring physician regarding patient demographics, vital status, cancer diagnosis, and manifestations of the suspected syndrome. The patient is entered into the registry if this preliminary information reveals that the patient has/had cancer and has exhibited an element of HUS (hemolysis, renal dysfunction, or thrombocytopenia). This process was designed only to eliminate obviously irrelevant cases; therefore, registration does not imply that the patient is a definite C-HUS case. After patient registration, copies of pertinent medical records are requested from the referring physician to provide more detailed information regarding initial cancer diagnosis; histology and stage; treatment given and response; chemotherapy doses and dates of administration; circumstances under which syndrome was suspected, with concomitant laboratory values and physical findings; status of cancer at time of syndrome development; presence or absence of previously described manifestations of syndrome such as microangiopathic hemolysis, renal dysfunction, thrombocytopenia, immune complexes, reactions to blood product transfusions, pulmonary edema, hypertension, neurologic abnormalities; treatment given for syndrome and response; current status of patient with regard to cancer and syndrome; and reports of biopsies or autopsies. The amount of information actually received varies widely from patient to patient. This information is abstracted onto registry data forms by the registry physician and entered into a computerized data base (R Base 5000/IBM-XT PC, Microrim, Seattle) by the registry data manager. Data are subsequently transferred to IBM 4381 for more complex statistical analysis using the Statistical Analysis System (SAS, SAS Institute Inc, Cary, NC).
LESESNE ET AL
ated by a Georgetown physician who was familiar with the syndrome. A record review diagnosis (RRD) of probable C-HUS was made if, upon record review, it could be demonstrated that the patient had cancer, at least two of the HUS triad (microangiopathic hemolytic anemia, renal dysfunction, thrombocytopenia) were present, and chemotherapyinduced marrow suppression was ruled out by bone marrow examination or sufficient time had elapsed (6 weeks) since last chemotherapy to reasonably exclude chemotherapyrelated myelosuppression. An effort was made to establish a screening definiton (SD) for C-HUS that would include as many true C-HUS cases as possible and use usually available and objective parameters. Examination of our data led to the establishment of the following arbitrary definition used to screen potential C-HUS patients: hematocrit _ 25%, platelet count : 100,000, serum creatinine __ mg/dL. When this definition was applied to 1.6 the 140 physician-reviewed cases in the registry, 85 patients met SD and RRD, 11 failed SD but met RRD, nine failed SD and RRD, zero met SD but failed RRD, eight had complete but inconclusive data, prohibiting classification, and 27 were recent registry entries, with incomplete data. Thus, our screening definition picked up 89% (85 of 96) of the cases identified by the subjective RRD. Because the objective SD missed few probable cases, we chose to subject the 85 SD-positive cases to more intensive analysis. These 85 patients are the subject of this report. RESULTS
Clinical Features The cancer diagnoses and some clinical features are detailed in Tables 1 and 2. Adenocarcinoma was present in 89% of the 85 cases, but only 26% had gastric carcinoma. The patients with diagnoses other than adenocarcinoma had epidermoid carcinoma (four), mesothelioma (two), cloacogenic carcinoma (one), islet cell carcinoma (one), germ cell carcinoma (one), and sarcoma (one). By definition, all patients had anemia (hematocrit 25%), thrombocytopenia (platelet count _< 100,000), and renal insufficiency (serum creatinine > 1.6 mg/dL). Half of the patients had hematocrit < 20%. Over 50% had platelet count < 30,000; median serum creatinine was 4.2 mg/dL at syndrome diagnosis. Thirty patients were never observed to have creatinine > 3.0; however, 21 of these 30 had an increase of at least 1.0 related in time to the development of other features of the syndrome. Bone marrow aspirations or biopsies were reported in 68 of 85 patients. In all cases either adequate erythroid precursors and megakaryocytes were present by bone marrow examination, or sufficient time had elapsed from last chemotherapy to suspected syndrome development (6 weeks) to minimize the likelihood of chemother-
Selection of Patientsfor In-Depth Analysis
Since criteria for registry entry were minimally selective (cancer and some element of HUS), the records requested and obtained from referring physicians were carefully evalu-
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
CANCER-ASSOCIATED HEMOLYTIC-UREMIC SYNDROME
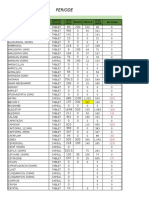
Table 1. Patient Characteristics
No. of Patients (%)*
783
Sex Male Female Age
35 (41)
50 (59) 35(41) 50(59) 75 (88)
22 (26) 15(18) 13(16) 11 (13) 4 (5)
S50
s 50
Primary adenocarcinoma Gastric Breast Colorectal Unknown primary Lung Pancreatic
6(7)
4(5)
Other
Received combination chemotherapy Including MMC Including 5-FU Cancer status at syndrome diagnosis Adjuvant treatment with no evidence of disease Complete response to chemotherapy Partial response to chemotherapy Stable disease Progression or relapse Abbreviation: 5-FU, fluorouracil. *N = 85.
85 (100) 84(99) 68(80)
ment. Thirty-three of the 85 had cancer present that had remained stable during chemotherapy, while 22 progressed during treatment. Circulating immune complexes were examined in 41 of the 85 registry cases. These complexes were measured by polyethylene glycol precipitation; normal levels were established by testing of 40 healthy controls. Significant elevation of immune complex levels was found in 36 of the 41 patients tested (89%). In several cases immune complexes were dissociated into antigen and antibody components, and the antibody was found to react with corresponding tumor-specific tissue (not the patient's actual tumor) by immunofluoresence. 1 Relationshipto ChemotherapeuticAgents All patients received combination chemotherapy for presenting neoplasms. MMC was part of the combination in 84 of 85 cases, fluorouracil (5-FU) in 68 (80%). 5-FU, Adriamycin (doxorubicin; Adria Laboratories, Columbus, OH), and MMC (FAM) was the specific treatment regimen in 68% of cases. The patient not receiving MMC was treated with vinblastine, bleomycin, and cisplatin-combination therapy. Cumulative dose of MMC was examined in all cases. One patient did not receive MMC; cumulative dose was not available for another patient. Only nine C-HUS patients received < 60 mg total MMC, whereas the remaining 74 were given 60 mg or greater (58% [48/83] between 60 mg and 100 mg) (Fig 1). There was a suggestion that surviving patients received a lower cumulative dose of MMC than patients subsequently dying. Further analysis indicated that the important variable was total cumulative dose, rather than number of courses of the drug. In 77% of cases, C-HUS developed within 4 months of the last MMC dose. The average number of days from last MMC to C-HUS development for all 85 patients was 92 (median, 75 days; range, 1 week to 15 months) of last MMC administration (Table 3). Examination of 5-FU cumulative dose did not reveal a similar dose-response pattern. Seventythree percent of cases were evenly distributed between 4,000 mg and 24,000 mg cumulative dose of 5-FU. Lack of a dose-response pattern could be taken as evidence against an etiologic role for 5-FU. However, the result could also be
17(20) 13(15) 12(14) 21(25) 22 (26)
apy-induced myelosuppression as a cause for anemia and thrombocytopenia. Cancer status at time of syndrome presentation was examined in all cases. Thirty patients (35%) were without clinical evidence of malignant disease when C-HUS developed; 17 of these had received adjuvant chemotherapy and 13 had a complete response of known disease to treatTable 2. Syndrome Characteristics No. of Patients (%) Anemia (hematocrit _ 25%) Thrombocytopenia (platelet _ 100,000) Renal dysfunction (serum creatinine _ 1.6 mg/dL) Microangiopathic hemolysis (peripheral smear) Prothrombin time (normal) Partial thromboplostin time (normal) LDH ! 300 IU/L Immune complexes present Pulmonary edema Neurologic abnormalities Received blood product transfusion Serious adverse reaction Died of or with C-HUS
85/85 (100)
85/85(100) 85/85 (100) 83/83(100) 62/64(97) 61/65 (94)
51/56(91)
36/41 (89)
55/85(65)
14/85(16)
75/85(88)
33/75(44) (52)
"44/85
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
784
LESESNE ET AL
P
""0 20
Table 3. Interval (months) From Last MMC to Development of Syndrome
No. of
Months Patients % Cumulative %
U(0
z
U
lo i-
1.0 1-1.9 2.0-2.9 3.0-3.9 4.0-4.9 5.0 Total
5 22 26 12 11 8 84
6 26 31 14 13 10 100
6 32 63 77 90 100
20 30 Cumulative Dose of Mitomycin C (mg)
Vital Status of C-HUS Cases Of our 85 C-HUS cases, 63 were dead at the time of analysis. Thirty-seven (59%) died as a direct result of the syndrome; 18 deaths (29%) were due to progressive cancer; seven deaths were attributed to both C-HUS and cancer, and one patient died of an unrelated cause. Syndrome deaths in most cases were related to renal failure. Fifty-nine percent of all deaths (37 cases) occurred within 8 weeks of syndrome development (median, 44 days; range, one day to 3 years). Of those patients who died of syndrome, median time of death from C-HUS diagnosis was 29 days (range, one to 496 days). Of the 22 living patients (as of November 1986), ten were without evident cancer and 12 had stable or progressive malignant disease. Response to Treatment of C-HUS The various treatment modalities used in CHUS are listed in Table 4. Improvement as a result of treatment was scored according to criteria determined and evaluated by the referring physician. For the most part, therapy was ineffective. The improvement reported with furosemide was generally symptomatic amelioration
Fig 1. MMC.
Relationship of C-HUS cases to cumulative dose of
explained by greater heterogeneity in the mode of administration of 5-FU. Other Syndrome Characteristics Seventy-five of 85 patients received blood product transfusions. Of these, 33 were reported to have serious adverse reactions, generally pulmonary edema or rapid worsening of hemolysis or renal function. Pulmonary edema developed in 55 (65%) of C-HUS patients. In most cases this was felt to be noncardiogenic in origin. However, cardiac pressure monitoring was rarely performed, and this distinction (cardiogenic v noncardiogenic) was often difficult to make in patients with lung metastases, possible doxorubicin cardiomyopathy, or potential fluid overload from renal insufficiency or blood transfusions. Adverse reactions were seen with transfusions of washed and unwashed red blood cells, platelet concentrates, and fresh frozen plasma. Neurological abnormalities (confusion, headache, seizures) attributable to syndrome were reported in 14 cases (16%).
Table 4. Treatment of C-HUS
No. of Patients No Response
N Corticosteroids Plasma exchange Dialysis Furosemide Aspirin Dipyridamole Heparin SPA immunopheresis 50 37 28 31 22 26 3 21
Improved (%)* 18(36) 11 (30) 10(36) 20 (65) 4(18) 5(19) 0(0) 10(48)
or Worse (%) 32 (72) 26(70) 18(64) 11(35) 18(82) 21(81) 3(100) 11 (52)
*Total patients in table exceeds 85 because many patients had more than one treatment modality and some patients had one treatment several times with different responses.
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
CANCER-ASSOCIATED HEMOLYTIC-UREMIC SYNDROME
785
Table 5. C-HUS Prognostic Factors as Assessed by
Univariate Analysis Log-Rank level of Significance Favorable prognostic factors Tumor status P < .001 SPA immunopheresis P < .005 Corticosteroids P<.05 Features of no prognostic significance (P > .05) Age tumor Cumulative MMC dose Interval from last MMC Pulmonary edema Transfusions Adverse response to transfusions Plasma exchange Aspirin Dipyridamole
of pulmonary edema and did not reflect change in hematologic or renal parameters. It should be noted that many patients received multiple simultaneous treatment interventions. Immunoperfusion over staphylococcal protein A column (SPA) was the most successful treatment.6 In this investigational procedure, patient plasma is first separated by filtration on a continuous plasma separator (Cobe, Denver), then slowly perfused over filters containing SPA covalently linked to polyacrylamide microbeads and ultimately returned to the patient. The goal of this treatment is the alteration or depletion of circulating immune complexes. Modulation of the complexes is postulated as a nonspecific interaction of SPA with the Fc portion of the immunoglobulin molecule. Treatment is given five to ten times on an every-other-day schedule according to the levels of circulating immune complexes and hematologic parameters. Responses were seen in ten of 21 patients treated with SPA. Response was defined as resolution of thrombocytopenia, improvement in anemia, and stabilization of renal function. Significant renal dysfunction was not reversible in patients treated with SPA. Survival in those treated with SPA was 6 months, whereas median survival of the entire cohort of 85 patients was 2.5 months. No patient with recurrent tumor at the time of treatment responded to SPA. PrognosticFactors The prognostic value of 13 separate variables was analyzed by evaluating equality of survival curves using a log-rank test (Table 5). Cancer status at syndrome presentation and treatment with corticosteroids and SPA immunopheresis were the only variables found to be associated with a more favorable outcome (P < .05). On subsequent multivariate analysis using a Cox proportional hazards model, only cancer status and treatment with SPA achieved levels of statistical significance.
DISCUSSION
"Primary
C-HUS appears to be a distinct entity appearing in patients with neoplastic diseases. Although there are invariably areas of overlap, C-HUS can generally be differentiated from similar pathologic conditions. HUS not related to cancer is most commonly seen in previously healthy chil-
dren and is characterized by dramatic onset (acute hemolysis with hemoglobinuria leading to oliguria) and low mortality (< 5%). When seen in adults, HUS ("conventional") is often associated with oral contraceptive use or the immediate postpartum state. TTP is a disease of young adults and is characterized in a high percentage of cases by fever and neurologic signs, features rare in C-HUS. While disseminated intravascular coagulation (DIC, consumption coagulopathy) may present with microangiopathic hemolytic anemia (MAHA), thrombocytopenia, and renal dysfunction, the characteristic derangement in coagulation parameters differentiates this state from C-HUS. 7 MAHA alone can be seen in patients with advanced disseminated cancer (especially gastric, breast, and pancreatic); however, the postulated mechanisms (damage to red blood cells flowing through microvasculature invaded by tumor) would be difficult to invoke in those C-HUS patients who are in remission or in the adjuvant setting and thus free of overt disease." 10 Known toxicities of MMC fail to explain the simultaneous occurrence of MAHA, thrombocytopenia, and renal insufficiency. Therefore, C-HUS should be distinguishable from other disorders. To facilitate analysis of a computer-based multisource registry, we sought an SD using the major easily quantifiable parameters of the syndrome. Our definition (documented cancer; hematocrit s 25%; platelet count _ 100,000; serum creatinine > 1.6 mg/dL) proved to have almost
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
786
LESESNE ET AL
90% sensitivity when applied to registry cases deemed to have C-HUS on the basis of record review. Some patients failing the SD were felt to have the syndrome. These were generally patients with milder degrees of anemia or thrombocytopenia, but with other supporting evidence of C-HUS (adenocarcinomas treated with combination chemotherapy; peripheral and bone marrow evidence of microangiopathic hemolysis; and no other evident etiology for these abnormalities). Nonetheless, our definition (SD) was useful in identifying a subset of registry patients for further analysis; if applied to a subset of patients at risk for the syndrome, it might prove useful in singling out candidates for (1) closer observation, (2) change or cessation of chemotherapeutic agents, or (3) treatment. Other clinical characteristics proved correlative with the screening definition. Initial diagnosis of adenocarcinoma, receipt of combination chemotherapy containing MMC, evidence of microangiopathic hemolysis, and pulmonary edema during the course of the syndrome were features present in over two thirds of our 85 cases. In addition, an adverse reaction to blood product transfusion (usually pulmonary edema) was seen in almost half of those patients who were transfused. When present, these findings lend support to a diagnosis of C-HUS; however, they cannot be considered a requisite part of the definition. At least 110 cases of C-HUS have been previously described in the literature, including the 12 from this institution reported by Cantrell 1 et al."' "46 Some comparisons can be made between our patients and those previously published. Eighty-nine percent of our cases had adenocarcinomas, the same percentage found in the 110 literature cases. Cantrell et all noted that half of their patients had gastric cancer, while the distribution of cancers in the registry cases corresponded more closely with that in all earlier patients examined collectively (registry: gastric 26%, breast 18%, colorectal 16%; v literature: gastric 28%, breast 17%, colorectal 25%). The patient mix reported by Cantrell et al' probably reflects the emphasis on gastric cancer prevailing at their institution at the time. Therefore, CHUS cannot be considered an entity peculiar to gastric, or even gastrointestinal, malignancies.
It has been reported that C-HUS appears in patients who have had complete or near complete responses to chemotherapy or who remain without disease following adjuvant therapy. Nineteen of the 25 patients (76%) described by Cordonnier et al were in remission at syndrome diagnosis. 39 Cantrell et al note that eight of 12 patients (67%) were without clinical evidence of disease when C-HUS appeared.' Twenty other patients previously described were reported to have minimal or no disease at the time of death from syndrome. Our cases are at some variance with these previous studies. Only 35% of registry patients were free of disease at syndrome diagnosis, while the remaining 65% had malignant disease present, either stable or progressive. This still represents a significant number of patients free of disease, and while the majority had malignant disease at time of syndrome diagnosis, the absence of obvious tumor or the induction of complete remission by chemotherapy may facilitate syndrome development. Our estimates of syndrome fatality also differ somewhat from those previously published. Excluding the 25 patients described by Cordonnier et a139 (see below), 70 of 85 (82%) earlier patients were dead when their case reports were published, virtually all deaths from complications of C-HUS. While 63 of our 85 patients have died (75%), 29% (18 of 63) of these deaths were attributable to cancer alone. The overall death rate from syndrome alone was 44% (37 of 85). We believe this difference reflects early reporting by referring physicians and a recognition of milder and reversible forms of C-HUS. However, our use of a minimal definition of C-HUS may have resulted in inclusion of patients with a different and less lethal pathophysiology. Specifically, we may not have been able to exclude a subset of patients with MAHA and unrelated minimal renal dysfunction. Only six of 25 patients in the article by Cordonnier et al had died at the time of its publication. The authors attributed this better prognosis to lower cumulative chemotherapy (particularly MMC) doses in patients treated later in their study and to aggressive treatment of syndrome in a few cases. Nevertheless, we conclude that once the syndrome has fully evolved, particularly with significant renal dysfunction, mortality is high.
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
CANCER-ASSOCIATED HEMOLYTIC-UREMIC SYNDROME
787
A causal relationship between MMC and C-HUS has been discussed since the syndrome was first described." All but one of our cases received MMC as part of combination chemotherapy. However, some caution should be exercised in examining the MMC relationship extracted from registry data. Most previously published reports of the syndrome have strongly suggested MMC as an etiologic agent. With this implied association established, physicians might tend to refer to the registry only those patients who had received MMC. Nonetheless, the evidence for MMC causality is strong. Of 110 previously reported patients, 100 received MMC. Two studies compared groups of patients treated with MMC with groups receiving other drugs. Proia et a125 describe a randomized trial in which patients with metastatic colorectal adenocarcinoma were treated with either 5-FU, vincristine, and MMC, or 5-FU, vincristine, and methylCCNU (lomustine). Four of 26 patients receiving MMC (15%) developed findings compatible with HUS, while none of the 27 patients in the lomustine group did. The British Stomach Cancer Group issued an interim report in 1983 on 411 patients participating in a randomized study of adjuvant chemotherapy in operable gastric cancer. 47 The treatment arms were placebo (normal saline); cyclophosphamide, 5-FU, vincristine, methotrexate, and MMC; or 5-FU and MMC. An HUS (not further defined) was observed in 24 patients receiving chemotherapy (8%) and in none of the placebo group. A milder degree of anemia and elevated BUN was seen in 22% of the chemotherapy-treated patients. In a noncomparative study, Valavaara and Nordman examined 142 patients with gastrointestinal cancer treated with combination chemotherapy including MMC.41 Ten of 118 evaluable patients (8%) developed renal toxicity, five of whom (4%) also manifested MAHA. These studies suggest not only an etiologic role for MMC, but also risk of between 4% and 15% for developing the full-blown syndrome during or after treatment with the drug. In contrast with these studies is the preliminary analysis (J.R. Neefe, J.S. Macdonald, personal communication, March 1988) of a randomized trial of the Southwest Oncology Group (SWOG) 7804. This adjuvant trial, begun in 1978, compared no therapy with FAM combina-
tion chemotherapy in 178 patients with gastric adenocarcinoma after surgery with curative intent and no residual disease. By 1986, no chemotherapy patient had met all the criteria of our screening definition. This negative result would still be compatible with an incidence of C-HUS of up to 5% with 95% confidence. As the SWOG trial was not designed to assess the incidence of C-HUS, a more detailed analysis will be required to justify a definitive statement. In the meantime, the difference from the other studies cited above cannot be explained, if it is other than statistical variation. Our analysis suggests an increased incidence of C-HUS at higher cumulative doses of MMC. Eighty-nine percent of our cases received > 60 mg total MMC. Of cases previously published, 89 of 100 patients who received MMC (89%) received a cumulative dose of at least 60 mg. This may suggest that careful monitoring of renal function and hematologic parameters, including peripheral smear, is necessary once the cumulative dose reaches 60 mg. Given the relative infrequency of the syndrome and the long time course over which it can develop, it would be difficult to set up a controlled trial of MMC dosing variations in order to observe effects on C-HUS incidence. Establishment of a maximum safe dose of the drug as has been done with doxorubicin would be useful; however, examination of our data did not permit this determination. That there are a few cases of C-HUS in patients not receiving MMC cannot be ignored. Approximately 10% of patients in previous studies manifested C-HUS identical in all respects to the vast majority of other cases except for the absence of MMC in the treatment regimen. Although it is likely that MMC is causally related to C-HUS, it does not appear to be essential for development of the syndrome. It may be supposed that the pathologic effects induced by MMC can also be seen with other drugs, less commonly and to a lesser degree. It should also be noted that most patients received 5-FU with MMC, and the role of drug interaction in the pathogenesis of the syndrome cannot be excluded. If physicians become aware that C-HUS may occur in the absence of MMC, then continued reporting of patients with C-HUS may reveal more non-MMC cases.
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
788
LESESNE ET AL
Until the development of the SPA immunoperfusion modality, treatment of this syndrome was generally ineffective. There are anecdotal reports both in the literature and in our registry of improvement with corticosteroids, antiplatelet agents, plasmapheresis, or observation alone. With the exception of SPA immunoperfusion, no one treatment modality or combination of modalities resulted in improvement except rarely. Aggressive nontransfusion would appear to be prudent, with blood product transfusions being reserved for patients with life-threatening bleeding or markedly symptomatic anemia. Our results with SPA are encouraging and investigation into this form of treatment is continuing. There is some indication that milder
forms of syndrome, ie, minimal renal dysfunction and less pronounced MAHA and thrombocytopenia, respond better to treatment. It would also appear that patients with little or no clinically demonstrable tumor burden respond better to SPA and in general have a more favorable prognosis. What is not clear is whether these patients might improve spontaneously with cessation of chemotherapeutic agents and close observation. Only a randomized trial of observation v treatment can answer this, and it has been difficult to initiate such a trial for a disorder that is relatively rare, not clearly defined, often lethal, and for which an effective form of therapy may exist (SPA). At present, we are continuing to gain experience with SPA in patients with CHUS and minimal malignant disease burden.
REFEREN CES
1. Cantrell JE, Phillips TM, Schein PS: Carcinoma associated hemolytic-uremic syndrome: A complication of mitomycin-C chemotherapy. J Clin Oncol 3:723-734, 1985 2. Lyman NW, Michaelson R, Viscuso RL, et al: Mitomycin-induced hemolytic-uremic syndrome: Successful treatment with corticosteroids and intense plasma exchange. Arch Intern Med 143:1617-1618, 1983 3. Hamner RW, Verani R, Weinman EJ: Mitomycinassociated renal failure: Case report and review. Arch Intern Med 143:803-807, 1983 4. Rabadi SJ, Khandekar JD, Miller HJ: Mitomycininduced hemolytic-uremic syndrome: Case presentation and review of literature. Cancer Treat Rep 66:1244-1247, 1982 5. Jackson AM, Rose BD, Graff LG, et al: Thrombotic microangiopathy and renal failure associated with antineoplastic chemotherapy. Ann Intern Med 101:41-44, 1984 6. Korec S, Schein PS, Smith FP, et al: Treatment of cancer-associated hemolytic-uremic syndrome with staphylococcal protein A immunoperfusion. J Clin Oncol 4:210-215, 1986 7. Williams JW, Beutler E, Erslev AJ, et al (eds.): Hematology (ed 3). New York, McGraw-Hill, 1983 8. Antman KH, Skarin AT, Mayer RJ, et al: Microangiopathic hemolytic anemia and cancer: A review. Medicine 58:377-384, 1979 9. Lohrmann H, Adam W, Heymer B, et al: Microangiopathic hemolytic anemia in metastatic carcinoma: Report of eight cases. Ann Intern Med 79:368-375, 1973 10. Lynch EC, Bakken CL, Casey TH, et al: Microangiopathic hemolytic anemia in carcinoma of the stomach. Gastroenterology 52:88-93, 1967 11. Krauss S, Sonoda T, Soloman A: Treatment of advanced gastrointestinal cancer with 5-fluorouracil and mitomycin-C. Cancer 43:1598-1603, 1979 12. Laffay DL, Tubbs RR, Vallenzuela R, et al: Chronic glomerular microangiopathy and metastatic carcinoma. Hum Pathol 10:433-438, 1979 13. Agnelli G, Grensele P, Neuci GG: Clotting activation after blood transfusion in patients receiving 5-fluorouracil and mitomycin-C treatment. Cancer Chemother Pharmacol 5:205-206, 1981 14. Van Spreenwel JP, Hemrika MH, DeMaat CEM, et al: Neth J Med 26:287-288, 1983 (letter) 15. Loprinzi CL: Mitomycin-C induced pulmonary and renal toxicities. Wis Med J 83:16-17, 1984 16. Huvos AG: Hemolytic anemia, thrombocytopenia and renal failure in a patient apparently cured of anal carcinoma. Cancer Invest 3:481-489, 1985 17. Jolivet J, Giroux L, Laurin S, et al: Microangiopathic hemolytic anemia, renal failure, and non-cardiogenic pulmonary edema: A chemotherapy induced syndrome. Cancer Treat Rep 67:429-434, 1983 18. Gulati SC, Sordillo P, Kempin S, et al: Microangiopathic hemolytic anemia observed after treatment of epidermoid carcinoma with mitomycin-C and 5-fluorouracil. Cancer 45:2252-2257, 1980 19. Crocker J, Jones EL: Haemolytic-uraemic syndrome complicating long-term mitomycin-C and 5-fluorouracil therapy for gastric carcinoma. J Clin Pathol 36:24-29, 1983 20. Bruntsch U, Groos G, Tigges F, et al: Microangiopathic hemolytic anemia, a frequent complication of mitomycin therapy in cancer patients. Eur J Clin Oncol 20:905-909, 1984 21. Karlin DA, Stroehlein JR: Rash, nephritis, hypertension, and haemolysis in patient on 5-fluorouracil, doxorubicin, and mitomycin-C. Lancet 2:534-535, 1980 22. Kressel BR, Ryan KP, Duong At, et al: Microangiopathic hemolytic anemia, thrombocytopenia, and renal failure in patients treated for adenocarcinoma. Cancer 48: 1738-1745, 1981 23. Laufman L, Courter S, Pritchard J: Fatal mitomycinC (MMC) syndrome heralded by pulmonary symptoms. Proc Am Soc Clin Oncol 2:197, 1983 (abstr) 24. Lempert KD: Haemolysis and renal impairment syndrome in patients on 5-fluorouracil and mitomycin-C. Lancet 2:369-370, 1980
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
CANCER-ASSOCIATED HEMOLYTIC-UREMIC SYNDROME 25. Proia AD, Harden EA, Silberman HR: Mitomycininduced hemolytic-uremic syndrome. Arch Pathol Lab Med 108:959-962, 1984 26. Pavy MD, Wiley EL, Abeloff MD: Hemolytic-uremic syndrome associated with mitomycin therapy. Cancer Treat Rep 66:457-461, 1982 27. Hanna WT, Krauss S, Regester RF, et al: Renal disease after mitomycin-C therapy. Cancer 48:2583-2588, 1981 28. Jao W, Manaligod JR: Renal disease associated with mitomycin therapy. Ultrastruct Pathol 5:83-88, 1983 29. Ravikumar TS, Sibley R, Reed K, et al: Renal toxicity of mitomycin-C. Am J Clin Oncol 7:279-285, 1984. 30. Giroux L, Bettez P, Giroux L: Mitomycin-C nephrotoxicity: A clinicopathologic study of 17 cases. Am J Kidney Dis 6:28-39, 1985 31. Price TM, Murgo AJ, Keveney JJ, et al: Renal failure and hemolytic anemia associated with mitomycin-C: A case report. Cancer 55:51-56, 1985 32. Jones BG, Fielding JW, Newman CE, et al: Intravascular haemolysis and renal impairment after blood transfusion in two patients on long-term 5-fluorouracil and mitomycin-C. Lancet 1:1275-1277, 1980 33. Khojasteh A, Reynolds RD, Garcia AR, et al: Hemolytic uremic-like syndrome following a single dose of mitomycin-C. Proc Am Soc Clin Oncol 3:4, 1984 (abstr) 34. Perry DJ: Reversible microangiopathic hemolytic anemia after mitomycin-C. Cancer Chemother Pharmacol 10: 223, 1983 35. Harden E, Lucas VS, Proia A, et al: Hemolytic uremic syndrome during therapy with mitomycin-C (MMC) plus 5-fluorouracil (5-FU). Proc Am Soc Clin Oncol 1:93, 1982 (abstr) 36. Rumpf KW, Rieger J, Lankisch PG, et al: Mitomycininduced haemolysis and renal failure. Lancet 2:1037-1038, 1980
789
37. Willie GR, Levy SM, Michaels RS, et al: Hemolyticuremic syndrome in a patient receiving mitomycin-C and 5-fluorouracil. Henry Ford Hosp Med J 31:104-109, 1983 38. van der Meer J, de Vries EGE, Vriesendorp R, et al: Hemolytic uremic syndrome in a patient on cis-platinum, vinblastine and bleomycin. J Cancer Res Clin Oncol 110: 119-122, 1985 39. Cordonnier D, Vert-Pr6 FC, Bayle F: La nephrotoxicit6 de la mitomycine C (a'propos de 25 observations). Resultats d'une euquete multicentrique organisee par la societ6 de nephrologie. Nephrologie 6:19-26, 1985 40. Sheldon R, Slaughter D: A syndrome of microangiopathic hemolytic anemia, renal impairment, and pulmonary edema in chemotherapy treated patients with adenocarcinoma. Cancer 58:1428-1436, 1986 41. Valavaara R, Nordman E: Renal complications of mitomycin-C therapy with special reference to the total dose. Cancer 55:47-50, 1985 42. Verwey J, Boven E, van der Meulen J, et al: Recovery from mitomycin-C induced hemolytic uremic syndrome: A case report. Cancer 54:2878-2881, 1984 43. Hug V, Burgess A, Blumenschein G, et al: Effects of cyclophosphamide on the mitomycin-induced syndrome of thrombotic thrombocytopenic purpura. Cancer Treat Rep 69:565-566, 1985 44. Tannock I: Methotrexate and mitomycin for patients with metastatic transitional cell carcinoma of the urinary tract. Cancer Treat Rep 67:503-504, 1983 45. Doll DC, Weiss RB, Issell BF: Mitomycin: Ten years after approval for marketing. J Clin Oncol 3:276-286, 1985 46. Levi JA, Aroney RS, Dalley DN: Haemolytic anaemia after cisplatin treatment. Br Med J 282:2003-2004, 1981 47. Fielding JWL, Fagg SL, Jones BG, et al: An interim report of a prospective, randomized, controlled study of adjuvant chemotherapy in operable gastric cancer. British Stomach Cancer Group. World J Surg 7:390-399, 1983
Downloaded from jco.ascopubs.org on November 18, 2011. For personal use only. No other uses without permission. Copyright 1989 American Society of Clinical Oncology. All rights reserved.
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Botswana Ref Ranges PaperDokument7 SeitenBotswana Ref Ranges PaperMunyaradzi MangwendezaNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- MDSAP QMS ManualDokument43 SeitenMDSAP QMS ManualmamjaguarNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Contemporary Management of Major Haemorrhage in Critical CareDokument13 SeitenContemporary Management of Major Haemorrhage in Critical CareYo MeNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Unit 5 Job and OccupationDokument3 SeitenUnit 5 Job and OccupationAstriPrayitnoNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Pulpal DiseasesDokument34 SeitenPulpal Diseasessamar yousif mohamedNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- English in Nursing - Rheynanda (2011316059)Dokument3 SeitenEnglish in Nursing - Rheynanda (2011316059)Rhey RYNNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Anaemia in Pregnancy: Dr. Lama MehaisenDokument11 SeitenAnaemia in Pregnancy: Dr. Lama MehaisenWendy EvansNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Zollinger-Ellison Syndrome (Gastrinoma)Dokument15 SeitenZollinger-Ellison Syndrome (Gastrinoma)Huy QuangNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- CSEC Biology June 2012 P2Dokument17 SeitenCSEC Biology June 2012 P2Joy BoehmerNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Research ProposalDokument3 SeitenResearch Proposalapi-446880170Noch keine Bewertungen
- AL Bio 2008 Marking SchemeDokument31 SeitenAL Bio 2008 Marking Schemes200410400% (4)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Gefico Maritime SectorDokument28 SeitenGefico Maritime SectorAugustine Dharmaraj100% (1)
- CFSS Monitoring Tool 2019Dokument7 SeitenCFSS Monitoring Tool 2019JULIE100% (10)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Coma ManagementDokument5 SeitenComa ManagementElena DocNoch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- (Norma) Guia Fda CovidDokument14 Seiten(Norma) Guia Fda CovidJhovanaNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- HypnotherapyDokument16 SeitenHypnotherapyAnonymous lsnDTjvNoch keine Bewertungen
- ARL ReportDokument24 SeitenARL ReportSaad WaqasNoch keine Bewertungen
- RP 11 - Measuring Concentration of Glucose Using A Calibration CurveDokument4 SeitenRP 11 - Measuring Concentration of Glucose Using A Calibration CurveAlfred SangNoch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- 16-Week Harvey Walden MarathonTraining PlanDokument18 Seiten16-Week Harvey Walden MarathonTraining PlanKaren MiranoNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Effects of Emotion On Short-Term Power Spectrum Analysis of Heart RateDokument5 SeitenThe Effects of Emotion On Short-Term Power Spectrum Analysis of Heart RateManuel Guerrero GómezNoch keine Bewertungen
- Backtrack 4 Information Gathering Archive Metagoofil Extract Metadata From Public Documents PDFDokument4 SeitenBacktrack 4 Information Gathering Archive Metagoofil Extract Metadata From Public Documents PDFKoushik ThyagarajanNoch keine Bewertungen
- 3.21.17 When Human Life Begins PDFDokument5 Seiten3.21.17 When Human Life Begins PDFJosue Gallegos SalasNoch keine Bewertungen
- Electrical Safety in HealthcareDokument2 SeitenElectrical Safety in HealthcareNur Aqilah IsmailNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Statement of PurposeDokument5 SeitenStatement of PurposesagvekarpoojaNoch keine Bewertungen
- Format OpnameDokument21 SeitenFormat OpnamerestutiyanaNoch keine Bewertungen
- Milk Supply Chain Management Upstream Downstream IssuesDokument25 SeitenMilk Supply Chain Management Upstream Downstream IssuesbikramNoch keine Bewertungen
- CRANE SIGNAL PERSON TRAINING SlidesDokument73 SeitenCRANE SIGNAL PERSON TRAINING SlidesAayush Agrawal100% (1)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Health and Safety at Work SlidesDokument195 SeitenHealth and Safety at Work SlidesZulfiqar Hyder100% (2)
- Annual Investment Plan: Municipality of JAGNADokument17 SeitenAnnual Investment Plan: Municipality of JAGNA39mtn7Noch keine Bewertungen
- 13fk10 Hav Igg-Igm (D) Ins (En) CeDokument2 Seiten13fk10 Hav Igg-Igm (D) Ins (En) CeCrcrjhjh RcrcjhjhNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)