Beruflich Dokumente
Kultur Dokumente
Essentials of Newborn Care (1) .DOH-WHO Protocol - Pps Southern Tag (Compatibility Mode)
Hochgeladen von
Milagros MaglasangOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Essentials of Newborn Care (1) .DOH-WHO Protocol - Pps Southern Tag (Compatibility Mode)
Hochgeladen von
Milagros MaglasangCopyright:
Verfügbare Formate
Essential Newborn Care: The DOH/WHO Protocol Essential Newborn Care: The DOH/WHO Protocol Maria Asuncion Silvestre,
FAAP Consultant, Essential Newborn Care 4 March 2010
OUTLINE OUTLINE Why do we need this Protocol? What are the four core, time-bound stepsof Essential Newborn Care? How are these steps performed? What can I do to implement the Protocolin my area of practice?
<5 year old and Neonatal Mortality, 1988 to 2008 <5 year old and Neonatal Mortal ity, 1988 to 2008 <5 Yr Old mortality decreased 40% (1988-1998) Past 10 years, declined by 20% Slow decline since neonatal mortality hasn t improved 80 60 70 Under Five Mortality Rate 0 10 20 30 40 50 60 1988 1993 1998 2003 2008 Neonatal MR DHS 88, 93, 98, 03, 08
82,000 Filipino children die annually, most could have been prevented
Source: CHERG estimates of under-five deaths, 2000-03 The Philippines is one of the 42 countries that account for 90% of global under-five mortality
Majority of newborns die due to stressful events or conditions during labor, delivery and the immediate postpartum period. 3outof4newborndeathsoccurintheweekoflifeofdeathsDayofLifeNumbero NDHS 2003, special tabulations
What Immediate Newborn Care Practices will save lives?
Time Band: At perineal bulging Prepare for the Delivery Time Band: At perineal bulging Prepare for the Delivery Check temperature of the delivery room 25-28 oC Free of air drafts Notify appropriate staff Arrange needed supplies in linear fashion Check resuscitation equipment Wash hands with clean water and soap Double glove just before delivery
Four Core Steps of Essential Newborn Care Four Core Steps of Essential Newborn Care Immediate and thorough drying Early skin-to-skin contact Properly timed cord clamping Non-separation of the newborn and mother for early initiation of breastfeeding
Time Band: Within 1st 30 secs Immediate Thorough Drying Time Band: Within 1st 30 secs Immediate Thorough Drying Call out the time of birth Dry the newborn thoroughly for at least 30 seconds seconds Wipe the eyes, face, head, front and back, arms and legs Remove the wet cloth
Time Band: Within 1st 30 secs Immediate and Thorough Drying Time Band: Within 1st 30 secs Immediate and Thorough Drying Do a quick check of breathing while drying Notes: During the 1st secs: D t til t l th bbi Do not ventilate unless the baby is floppy/limp and not breathing Do not suction unless the mouth/nose are blocked with secretions or other material
Time Band 0 -3 mins: Immediate, Thorough Drying Time Band 0 -3 mins: Immediate, Thorough Drying Notes: Do not wipe off vernix Do not bathe the newborn Do not bathe the newborn Do No No No not do footprinting slapping hanging upside -down squeezing of chest
Time Band: After 30 secs of drying Early Skin-to-Skin Contact Time Band: After 30 secs of drying Early Skin-to-Skin Contact If newborn is breathing or crying: Position the newborn prone on the mother s abdomen or chest Cover the newborn s back with a dry blanket Cover the newborn s head with a bonnet
Time Band: After 30 secs of drying Early Skin-to-Skin Contact Time Band: After 30 secs of drying Early Skin-to-Skin Contact Notes: Avoid any manipulation, e.g. routine suctioning that may cause trauma or infection gy Place identification band on ankle (not wrist) Skin to skin contact is doable even for cesarean section newborns
Time Band: 1 -3 mins Properly -timed cord clamping Time Band: 1 -3 mins Properly -timed cord clamping Remove the first set of gloves After the umbilical pulsations have stopped, clamp the cord using a sterile stopped, clamp the cord using a sterile plastic clamp or tie at 2 cm from the umbilical base Clamp again at 5 cm from the base Cut the cord close to the plastic clamp
Time Band: 1 -3 mins Properly -timed cord clamping Time Band: 1 -3 mins Properly -timed cord clamping Notes: Do not milk the cord towards the baby After the 1st clamp, you may strip the cord After the 1st clamp, you may strip the cord of blood before applying the 2nd clamp Cut the cord close to the plastic clamp so that there is no need for a 2nd trim Do not apply any substance onto the cord
Time Band: Within 90 mins Non-separation of Newborn from Mother for Early Breastfeeding Time Band: Within 90 mins Non-separation of Newborn from Mother for Early Breastfeeding Leave the newborn in skin-to-skin contact Observe for feeding cues, including tonguing, licking, rooting Point these out to the mother and encourage her to nudge the newborn towards the breast
Time Band: Within 90 mins Non-separation of Newborn from Mother for Early Breastfeeding Time Band: Within 90 mins Non-separation of Newborn from Mother for Early Breastfeeding Counsel on positioning Counsel on positioning Newborn Newborn Newborn Newborn s neck is not flexed nor twisted is facing the breast s body is close to mother s body s whole body is supported
Time Band: Within 90 mins Non-separation of Newborn from Mother for Early Breastfeeding Time Band: Within 90 mins Non-separation of Newborn from Mother for Early Breastfeeding Counsel on attachment and suckling Counsel on attachment and suckling Mouth wide open Lower lip turned outwards Baby s chin touching breast Suckling is slow, deep with some pauses
Time Band: Within 90 mins Non-separation of Newborn from Mother for Early Breastfeeding Time Band: Within 90 mins Non-separation of Newborn from Mother for Early Breastfeeding Notes: Minimize handling by health workers Do not give sugar water, formula or other prelacteals Do not give bottles or pacifiers Do not throw away colostrum
Time Band: Within 90 minutes Non-separation of Newborn from Mother for Early Breastfeeding Time Band: Within 90 minutes Non-separation of Newborn from Mother for Early Breastfeeding Weighing, bathing, eye care, examinations, ij ti (h titi BBCG) h ldb injections (hepatitis B, BCG) should be done after the first full breastfeed is completed Postpone washing until at least 6 hours
Time Band: Within 90 minutes Non-separation of Newborn from Mother for Early Breastfeeding Time Band: Within 90 minutes Non-separation of Newborn from Mother for Early Breastfeeding Weighing, bathing, eye care, examinations, ij ti h ldb d ft th fi tf injections should be done after the first full llbreastfeed is completed Postpone washing until at least 6 hours
The evidence is solid:
The following Newborn Care Practices will save lives: Immediate and Thorough Drying Thorough Drying Early Skin-to-Skin Contact Properly Timed Cord Clamping Non-separation of Newborn from Mother for Early Breastfeeding
Delaying Initiation of breastfeeding increases risk of infection-related death, RR Nepal 2008, 22,838 breastfed babies 8 10 12 14 Mullany LC, et al. J Nutr, 2008; 138(3):599-603. 0 2 4 6 8 <1 1-24 24-48 48-72 >72 Hours after Birth
Delaying Initiation of breastfeeding increases risk of infection-related death, Ghana 2004, 10,947 breastfed infants
ENC Time-Bound Interventions Within 30 Seconds Objective: To stimulate breathing, provide warmth After thorough drying Objective: To provide warmth, bonding, prevent infection & hypoglycemia Up to 3 minutes Post-delivery Objective: To reduce anemia in term & preterm; IVH & transfusions Within 90 minutes Of age Objective: To facilitate initiation of breastfeeding through sustained contact warmth hypoglycemia -Put on double gloves -Dry thoroughly -Remove wet cloth -Quick check of NB s breathing -Suction only if needed -Put prone on chest/ abdomen skin to skin -Cover w/ blanket, bonnet -Place identification on ankle -Do not remove vernix IVH & transfusions in preterm -Remove 1st set of gloves -Clamp and cut cord after cord pulsations stop (1-3 mins) -Do not milk cord -Give oxytocin 10mg IM to mother contact -Uninterrupted skin to skin contact
-Observe NB for feeding cues -Counsel on positioning & attachment -Do eye care, injections etc after 1st breastfeed
Training Video
Current State of Newborn Care PracticesNewborn Care Practices in Philippine Hospitals Current State of Newborn Care PracticesNewborn Care Practices in Philippine Hospitals
Variation in Sequence of Interventions
Sobel, Silvestre, Mantaring, Oliveros, 2009
Essential Newborn Care Protocol was guideline developed to address these issues
Next Steps Dissemination DOH Administrative Order 2009-0025 on ENC signed 2009 0025 on ENC signed Unang Yakap campaign launched Dec 9, 2009 Implementation Monitoring
Scope of Application Whole hierarchy of the DOH and its attached agencies Public and private providers Development partners involved in the MNCHN strategy All health practitioners involved in maternal and newborn care
ENC Implementation ENC Implementation The current state of maternal and newborn care needs urgent action Evidence-based interventions are not practiced sufficiently. ENC Protocol provides an evidence-based, low stl tch l cka fi t ti th cost, low technology package of interventions that twill save tens of thousands of lives. Each of us, as individuals and as organizations, have to look inward to find ways to implement ENC Join us to bring Unang Yakap to your membership and every person they can influence.
How can I contribute to implementing ENC?
Organize a multidisciplinary ENC Working Group MDs: Obs, Pediatricians, Anesthesiologists Nurses, nursing assistants Midwives Administrators Infection control committee Infection control committee Conduct a situational analysis of your facility
Revise hospital policies and standard operating procedures, forms, order sheets etc
How can I contribute to implementing ENC?
Enable the environment for ENC Disable the environment that hinders ENC Join us to bring Unang Yakap to your membership and every mother, father that they can influence.
Das könnte Ihnen auch gefallen
- Legal Memorandum: Legal Research, Uv - Gullas Law SchoolDokument16 SeitenLegal Memorandum: Legal Research, Uv - Gullas Law SchoolMilagros MaglasangNoch keine Bewertungen
- Complications of PregnancyDokument33 SeitenComplications of PregnancyMilagros Maglasang100% (1)
- MyNotes NCM101 LecDokument25 SeitenMyNotes NCM101 LecMilagros MaglasangNoch keine Bewertungen
- Complications of PregnancyDokument33 SeitenComplications of PregnancyMilagros Maglasang100% (1)
- Before An OperationDokument4 SeitenBefore An OperationKewkew AzilearNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Anxiety and Depression in TeensDokument2 SeitenAnxiety and Depression in TeensHenry Alexander Gerena SalazarNoch keine Bewertungen
- Controversias en El Manejo de Las Fracturas Abiertas (2014)Dokument7 SeitenControversias en El Manejo de Las Fracturas Abiertas (2014)J. Adrian NogueraNoch keine Bewertungen
- A5 Pig Management GuidlinesDokument4 SeitenA5 Pig Management GuidlinesAnna NdunaNoch keine Bewertungen
- Venous Leg UlcersDokument28 SeitenVenous Leg UlcersamurachNoch keine Bewertungen
- Developing Biocompatibility For Medical DevicesDokument30 SeitenDeveloping Biocompatibility For Medical DevicesNagula Naresh100% (1)
- Yes, it hurts here.Roxana: I'm going to give you an injection to numb the area. Now I'm going to check the tooth with the probe again. Does it still hurtDokument5 SeitenYes, it hurts here.Roxana: I'm going to give you an injection to numb the area. Now I'm going to check the tooth with the probe again. Does it still hurtCristian IugaNoch keine Bewertungen
- Criptorquidia en PerrosDokument4 SeitenCriptorquidia en PerrosDanielaNoch keine Bewertungen
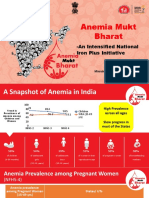
- Anemia Mukt Bharat: - An Intensified National Iron Plus InitiativeDokument23 SeitenAnemia Mukt Bharat: - An Intensified National Iron Plus InitiativeAnggun100% (1)
- Perbedaan Kepadatan Lalat Yang Hinggap Pada Fly Grill Yang Berbeda Warna Di Pasar SrimangunanDokument80 SeitenPerbedaan Kepadatan Lalat Yang Hinggap Pada Fly Grill Yang Berbeda Warna Di Pasar SrimangunanIrina MayasisianaNoch keine Bewertungen
- Arogya KavachaDokument5 SeitenArogya KavachaiamgodrajeshNoch keine Bewertungen
- MODUL 1 FKG UnairDokument61 SeitenMODUL 1 FKG UnairLaurensia NovenNoch keine Bewertungen
- Cholera: Key FactsDokument9 SeitenCholera: Key FactsDennis NjorogeNoch keine Bewertungen
- Diasys Katalog 2019 190506 ScreenDokument104 SeitenDiasys Katalog 2019 190506 Screendr-abdullah husseinNoch keine Bewertungen
- Njala University: Bo Campus-Kowama LocationDokument32 SeitenNjala University: Bo Campus-Kowama LocationALLIEU FB SACCOHNoch keine Bewertungen
- NDT 3 429Dokument13 SeitenNDT 3 429Mohammed AldaffaieNoch keine Bewertungen
- Afterword by Ilyene BarskyDokument5 SeitenAfterword by Ilyene Barskykkleiman_ppscNoch keine Bewertungen
- Ecart Medications and EquipmentDokument9 SeitenEcart Medications and EquipmentJan Philippe BelandoNoch keine Bewertungen
- Bailey's Othorhinolaryngology and Head and Neck SurgeryDokument3.775 SeitenBailey's Othorhinolaryngology and Head and Neck SurgeryDr. Christian Dimitrov92% (12)
- 2018 01 Early Pregnancy Loss LightDokument41 Seiten2018 01 Early Pregnancy Loss LightMishal FatimaNoch keine Bewertungen
- Soft Tissue Biology Around Dental ImplantsDokument76 SeitenSoft Tissue Biology Around Dental Implantsaakankshakanwar0% (2)
- Fetal Blood Sampling: 1. PurposeDokument7 SeitenFetal Blood Sampling: 1. PurposeMuathNoch keine Bewertungen
- Heat Illness Types, Causes, Symptoms and TreatmentsDokument46 SeitenHeat Illness Types, Causes, Symptoms and TreatmentsDewi Pertiwi Pertiwi0% (1)
- BD TTM Neuro Brochure Update Feb 2020 - v1Dokument2 SeitenBD TTM Neuro Brochure Update Feb 2020 - v1Hanh NguyenNoch keine Bewertungen
- Types of Studies and Research Design PDFDokument5 SeitenTypes of Studies and Research Design PDFPaulina VoicuNoch keine Bewertungen
- Abdominoperineal Resection MilesDokument17 SeitenAbdominoperineal Resection MilesHugoNoch keine Bewertungen
- ACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV InfectionDokument16 SeitenACE2 Expression in Kidney and Testis May Cause Kidney and Testis Damage After 2019-nCoV InfectionSY LodhiNoch keine Bewertungen
- English Assessment Physiotherapy & History Taking Dialogue EnglishDokument4 SeitenEnglish Assessment Physiotherapy & History Taking Dialogue EnglishRobby FahrezaNoch keine Bewertungen
- Treating Constipation and Anal Stenosis in a 7-Month-OldDokument35 SeitenTreating Constipation and Anal Stenosis in a 7-Month-OldAbigail CruzNoch keine Bewertungen
- Management of The Urologic Sepsis SyndromeDokument10 SeitenManagement of The Urologic Sepsis SyndromeNur Syamsiah MNoch keine Bewertungen
- Barrier Free ArchitectureDokument3 SeitenBarrier Free ArchitectureAmarjit SahNoch keine Bewertungen