Beruflich Dokumente
Kultur Dokumente
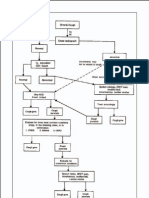
Constipation Algorithm
Hochgeladen von
IYERBK0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
1K Ansichten1 SeiteConstipation and faecal incontinence algorithm summarises the guidelines for management of constipation, especially in the elderly. The standard regime and protocol may have to be followed by any attending clinician in the times of emergency.
Originalbeschreibung:
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenConstipation and faecal incontinence algorithm summarises the guidelines for management of constipation, especially in the elderly. The standard regime and protocol may have to be followed by any attending clinician in the times of emergency.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
1K Ansichten1 SeiteConstipation Algorithm
Hochgeladen von
IYERBKConstipation and faecal incontinence algorithm summarises the guidelines for management of constipation, especially in the elderly. The standard regime and protocol may have to be followed by any attending clinician in the times of emergency.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 1
CONSTIPATION & FAECAL INCONTINENCE ALGORITHM
NB: This algorithm summarises the guidelines for management of constipation, especially in the elderly.
FAECAL LOADING?
STOOL CONSISTENCY? with infrequent or unpredictable emptying
(or no motion for 3 days, or “overflow”)
NB This is a short term regime until
regular evacuation is established –
commence oral regime concurrently
Too Hard Too Soft With hard stool With soft/
or “overflow” formed stool
•Increase diet fibre •Loperamide Regular/daily Trial of
(fit/mobile patients only) (titrate dose suppository/enema*: short-term
•Increase fluid intake carefully) •Glycerine suppos oral senna
•Increase mobility if necessary ↓ or
•Osmotic laxative-lactulose add: •Bisacodyl suppos bisacodyl
if necessary add •Codeine (or ‘microlax’)
•Faecal softener –docosate phosphate ↓
•Enema (Fleet oil
NB. Use bulk laxatives (eg &/or phosphate) *
psyllium) only if fluid intake
high – can cause constipation
Commence regular oral regime
Factors associated with Appropriate history REFERRAL if required
constipation/faecal incontinence •Past bowel habit For enema (or suppository
•Sphincter weakness •Awareness of call to not able to be managed by
•Anal sensory loss stool patient):
•Immobility •Stool consistency •Contact GP or a Nurse
•Diet/dehydration •Laxative use/ medication •Prescribe enema or
•Faecal loading •Mobility suppository
(see management above) •Diet •Complete the
•Medication (eg opiate, tricyclic) nursing medication sheet
•Slow colonic transit (eg opiates) Examination to enable follow up.
•Loss of cognitive awareness •Abdominal exam NB. The standard regime &
•Laxative abuse •Anorectal exam protocol may have to be followed
•Bulk laxatives (can constipate if •Digital rectal exam by any attending clinician in the
fluid intake insufficient) •Cognitive assessment times ahead.
Das könnte Ihnen auch gefallen
- NR 500NP WK 6 Area of Interest Power PresentationDokument2 SeitenNR 500NP WK 6 Area of Interest Power PresentationEassignmentsNoch keine Bewertungen
- Types of Stomas and Loop Ostomy CareDokument8 SeitenTypes of Stomas and Loop Ostomy CareRadhiyatul Ashiqeen Binti MoktarNoch keine Bewertungen
- Comprehensive H&P Note Template For Phase 1 Spring Assessment 2016Dokument5 SeitenComprehensive H&P Note Template For Phase 1 Spring Assessment 2016Derek JonesNoch keine Bewertungen
- Physical Exam SheetDokument6 SeitenPhysical Exam SheetDidi SaputraNoch keine Bewertungen
- Fluids Electrolytes Acid Base DisordersDokument6 SeitenFluids Electrolytes Acid Base DisordersJerikaDolorPadilloPatricioNoch keine Bewertungen
- Flash Cards Vocab For Exam 1. Jarvis CH 1-3, 8, 9, 12, 13http - P.quizlet - Com - Settitle Health Assessment Vocab For Exam 1Dokument22 SeitenFlash Cards Vocab For Exam 1. Jarvis CH 1-3, 8, 9, 12, 13http - P.quizlet - Com - Settitle Health Assessment Vocab For Exam 1tipredd100% (1)
- Transitional Care Case Study-Pulling It All TogetherDokument13 SeitenTransitional Care Case Study-Pulling It All TogethermatthewNoch keine Bewertungen
- 3806NRS Nursing Assignment HelpDokument5 Seiten3806NRS Nursing Assignment HelpMarry WillsonNoch keine Bewertungen
- 65-Year-Old Woman With Cough and FatigueDokument7 Seiten65-Year-Old Woman With Cough and Fatigue최인선100% (1)
- Elizabeth Wettlaufer - Agreed Statement of FactsDokument57 SeitenElizabeth Wettlaufer - Agreed Statement of FactsNick Westoll100% (3)
- Apollo Nashik PlansDokument11 SeitenApollo Nashik Plansjyoshnarath95% (21)
- 100+ Clinical Case Histories and Medical Study GuidesDokument8 Seiten100+ Clinical Case Histories and Medical Study GuidesAamir HamaadNoch keine Bewertungen
- Poster Template 20201217 10Dokument1 SeitePoster Template 20201217 10api-538973019Noch keine Bewertungen
- Encopresis, (Fecal Incontinence) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandEncopresis, (Fecal Incontinence) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- BIOS1168 Functional Musculoskeletal Anatomy ADokument23 SeitenBIOS1168 Functional Musculoskeletal Anatomy ALachlan NguyenNoch keine Bewertungen
- Main drug therapy for ulcerative colitis is sulfa for one yearDokument4 SeitenMain drug therapy for ulcerative colitis is sulfa for one yearcathyNoch keine Bewertungen
- 6-7 - Medical Nursing - GIS DisordersDokument108 Seiten6-7 - Medical Nursing - GIS DisordersmichaelNoch keine Bewertungen
- GI Exam 2 NotesDokument7 SeitenGI Exam 2 NotesxguardiansoullessxNoch keine Bewertungen
- Assignment 2.1soap 1Dokument5 SeitenAssignment 2.1soap 1Anonymous mX5wWmGNoch keine Bewertungen
- Liver OneDokument6 SeitenLiver Oneeswar6Noch keine Bewertungen
- Maternal Ob NotesDokument103 SeitenMaternal Ob NotesBoris OrbetaNoch keine Bewertungen
- Head, Mouth, Nose, Throat, Neck and Regional Lymph Nodes: Kristin Clephane, MSN, RN, CPNDokument44 SeitenHead, Mouth, Nose, Throat, Neck and Regional Lymph Nodes: Kristin Clephane, MSN, RN, CPNMike100% (1)
- NURS360 Pyelonephritis Care MapDokument5 SeitenNURS360 Pyelonephritis Care MapChristine RombawaNoch keine Bewertungen
- Genitourinary Problem: Nephrotic Syndrome Wilm's Tumor ManagementDokument19 SeitenGenitourinary Problem: Nephrotic Syndrome Wilm's Tumor ManagementJayson CruzNoch keine Bewertungen
- AH2 Hesi ReviewDokument46 SeitenAH2 Hesi ReviewJamie Antonini Grant100% (1)
- Function of G I System: The Primary Digestive Functions Are Break Down Food Particles "Dokument113 SeitenFunction of G I System: The Primary Digestive Functions Are Break Down Food Particles "cherryann_12100% (1)
- Morgan Soap NoteDokument2 SeitenMorgan Soap Noteapi-302927141100% (1)
- Fluid and Electrolyte DisturbancesDokument7 SeitenFluid and Electrolyte DisturbancesMarie Antionette MondragonNoch keine Bewertungen
- Insulin Therapy in Type 2 Diabetes MellitusDokument40 SeitenInsulin Therapy in Type 2 Diabetes MellitusEDWIN WIJAYANoch keine Bewertungen
- Review of Systems ANDREADokument7 SeitenReview of Systems ANDREAAndrea Dora OrtalizNoch keine Bewertungen
- Bacillus Calmette - Guérin: Oral Polio VaccineDokument1 SeiteBacillus Calmette - Guérin: Oral Polio VaccineElleNoch keine Bewertungen
- Prof. Sandra M. Covarrubias - September 24, 2021: 5.2fluid & Electrolytes ImbalancesDokument5 SeitenProf. Sandra M. Covarrubias - September 24, 2021: 5.2fluid & Electrolytes ImbalancesIvy VillalobosNoch keine Bewertungen
- Food Poisoning - Health Authority Abu Dhabi - HAADDokument6 SeitenFood Poisoning - Health Authority Abu Dhabi - HAADMedarabiaNoch keine Bewertungen
- C 13Dokument11 SeitenC 13Jo100% (1)
- SOAP Note Head AcheDokument2 SeitenSOAP Note Head AcheTravis Jack0% (1)
- Mental Capital SummaryDokument52 SeitenMental Capital SummaryaguzzzNoch keine Bewertungen
- Week 11 - Ch. 36 - UrinaryDokument27 SeitenWeek 11 - Ch. 36 - UrinaryMary SingletonNoch keine Bewertungen
- StatementDokument5 SeitenStatementtrinity_brannonNoch keine Bewertungen
- ChartingDokument1 SeiteChartingAdrianaMarreroNoch keine Bewertungen
- Presented By: Anjani.S.Kamal 1 Year MSC (N)Dokument23 SeitenPresented By: Anjani.S.Kamal 1 Year MSC (N)shubham vermaNoch keine Bewertungen
- Public Health Mini-Guides - Alcohol Misuse - 1st Edition (2015)Dokument143 SeitenPublic Health Mini-Guides - Alcohol Misuse - 1st Edition (2015)Andrei Cristea100% (1)
- Cranial Nerves Study GuideDokument6 SeitenCranial Nerves Study Guidevienny kayeNoch keine Bewertungen
- Head To Toe AssessmentDokument3 SeitenHead To Toe Assessmentjeraldine marceraNoch keine Bewertungen
- Patient Care SkillsDokument15 SeitenPatient Care SkillsIts John100% (1)
- NLN nutrition practice exam study guideDokument3 SeitenNLN nutrition practice exam study guideKaren HutchinsonNoch keine Bewertungen
- Comprehensive Nursing Assessment For Care Plan: AllergiesDokument14 SeitenComprehensive Nursing Assessment For Care Plan: AllergiesBrittany ShrewsburyNoch keine Bewertungen
- Major Hormone Glands and Their FunctionsDokument5 SeitenMajor Hormone Glands and Their FunctionsSTEFFI GABRIELLE GOLEZNoch keine Bewertungen
- Jarvis Complete Phys ExamDokument9 SeitenJarvis Complete Phys ExamYadile D BenoitNoch keine Bewertungen
- Guide to Physical Assessment DocumentationDokument3 SeitenGuide to Physical Assessment Documentationsandaman2225Noch keine Bewertungen
- Ch34 PharmDokument8 SeitenCh34 PharmShaneka WilliamsNoch keine Bewertungen
- Parenting Styles: - Dictatorial or AuthoritarianDokument45 SeitenParenting Styles: - Dictatorial or AuthoritarianCourseTree LearningNoch keine Bewertungen
- 3 Fluids and Electrolytes PPDokument112 Seiten3 Fluids and Electrolytes PPjcodoyNoch keine Bewertungen
- Aspirin: Veterinary-SystemicDokument19 SeitenAspirin: Veterinary-SystemicPeter FritzNoch keine Bewertungen
- Concept Map TemplateDokument16 SeitenConcept Map Templatenursing concept mapsNoch keine Bewertungen
- Electrolytes Lab ValuesDokument3 SeitenElectrolytes Lab Valuessublee75100% (1)
- Ch35 CardiovascularDokument11 SeitenCh35 CardiovascularJessie Jennings100% (3)
- Sample of Medical and Surirgical NursingDokument8 SeitenSample of Medical and Surirgical NursingMounir ChadliNoch keine Bewertungen
- HemiplegiaDokument17 SeitenHemiplegiaStefany CelineNoch keine Bewertungen
- Vital signs and medication reference tableDokument1 SeiteVital signs and medication reference tablejhenssineNoch keine Bewertungen
- MELD Related Files Liver MELD-PlusDokument45 SeitenMELD Related Files Liver MELD-PlusUKNoch keine Bewertungen
- NUR 215 Asepsis Lab QuestionsDokument3 SeitenNUR 215 Asepsis Lab QuestionsmlomiguenNoch keine Bewertungen
- Kidney Anatomy and Blood VesselsDokument17 SeitenKidney Anatomy and Blood VesselsMuhammad Tauseef BashirNoch keine Bewertungen
- Hypertension FactsheetDokument2 SeitenHypertension FactsheetPedro QuintasNoch keine Bewertungen
- Health AssessmentDokument15 SeitenHealth AssessmentrlinaoNoch keine Bewertungen
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideVon EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNoch keine Bewertungen
- The Transition From ForgetfulnessDokument8 SeitenThe Transition From ForgetfulnessIYERBKNoch keine Bewertungen
- Are All Angiotensin Receptor Blockers The Same?Dokument37 SeitenAre All Angiotensin Receptor Blockers The Same?IYERBKNoch keine Bewertungen
- Role of Sadhana in EnlightenmentDokument2 SeitenRole of Sadhana in EnlightenmentIYERBKNoch keine Bewertungen
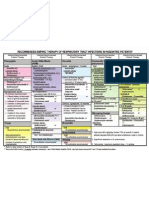
- Aids Malaria Drugs ChartDokument2 SeitenAids Malaria Drugs ChartIYERBKNoch keine Bewertungen
- List of The Greatest Indian NovelsDokument9 SeitenList of The Greatest Indian NovelsIYERBKNoch keine Bewertungen
- Chronic Cough - FLOWDokument3 SeitenChronic Cough - FLOWIYERBKNoch keine Bewertungen
- Delicious Dark Greens RecipesDokument8 SeitenDelicious Dark Greens RecipesIYERBKNoch keine Bewertungen
- Wallpaper Selection GuideDokument4 SeitenWallpaper Selection GuideIYERBKNoch keine Bewertungen
- Ida SlidesDokument47 SeitenIda SlidesIYERBKNoch keine Bewertungen
- Cough AlgorithmsDokument2 SeitenCough AlgorithmsIYERBK100% (2)
- Pneumonia GuidelinesDokument4 SeitenPneumonia GuidelinesIYERBK100% (3)
- Anti Infectives Guide For AdultsDokument5 SeitenAnti Infectives Guide For AdultsIYERBK100% (1)
- Rti Aadults AlgorithmDokument2 SeitenRti Aadults AlgorithmIYERBKNoch keine Bewertungen
- RTI Chart ChildDokument1 SeiteRTI Chart ChildIYERBKNoch keine Bewertungen
- Cap AlgorithmDokument1 SeiteCap AlgorithmIYERBKNoch keine Bewertungen
- RTI Chart AdultDokument1 SeiteRTI Chart AdultIYERBK100% (1)
- STD Treatment ChartDokument5 SeitenSTD Treatment ChartIYERBK100% (1)
- Uti AlgorithmDokument1 SeiteUti AlgorithmIYERBK100% (2)
- A.1. Community-Acquired: Use Antibiotics JudiciouslyDokument33 SeitenA.1. Community-Acquired: Use Antibiotics JudiciouslymaxgroovesNoch keine Bewertungen
- SV300 Service Training-Basic V1.0Dokument82 SeitenSV300 Service Training-Basic V1.0WALTER HUGO GOMEZNoch keine Bewertungen
- Magnesium The Miracle MineralDokument4 SeitenMagnesium The Miracle MineralScott SheltonNoch keine Bewertungen
- Corrected DissertationDokument141 SeitenCorrected Dissertationmonanoel100% (1)
- CacalF - Concept Analysis of Compassion Fatigue - NR 501Dokument10 SeitenCacalF - Concept Analysis of Compassion Fatigue - NR 501Nenette Tolentino Cacal100% (1)
- Ultrasound in Critical CareDokument4 SeitenUltrasound in Critical CareFranz MiguelNoch keine Bewertungen
- 7 Reasons Youre Tired All The Time PreventionDokument16 Seiten7 Reasons Youre Tired All The Time Preventionsharkz fujiwaraNoch keine Bewertungen
- Antepartum HaemorrhageDokument36 SeitenAntepartum HaemorrhageAfi RamadaniNoch keine Bewertungen
- Dysphagia in CPDokument19 SeitenDysphagia in CPMaria Alejandra RengifoNoch keine Bewertungen
- Vision AssessmentDokument32 SeitenVision AssessmentSamuel Ponraj100% (1)
- Critical Care Testing - Quality AssuranceDokument120 SeitenCritical Care Testing - Quality AssuranceAbhijit Mokashi100% (1)
- PROCTOSIGMOIDOSDokument5 SeitenPROCTOSIGMOIDOSJopet Llanita0% (1)
- Vide0 Assisted Thoracoscopic Surgery (VATS) : A Study ofDokument17 SeitenVide0 Assisted Thoracoscopic Surgery (VATS) : A Study ofVibha KarmarkarNoch keine Bewertungen
- Diabetic Ketoacidosis Protocol PICU Oct 2010 2Dokument9 SeitenDiabetic Ketoacidosis Protocol PICU Oct 2010 2Vidini Kusuma AjiNoch keine Bewertungen
- Diabetes Prediction Using Data Mining: 1. AdminDokument2 SeitenDiabetes Prediction Using Data Mining: 1. AdminVishal TailorNoch keine Bewertungen
- Cohort 1Dokument25 SeitenCohort 1jaish8904Noch keine Bewertungen
- Elated QuotesDokument28 SeitenElated Quotesshasha001Noch keine Bewertungen
- Acyclovir antiviral drug overviewDokument3 SeitenAcyclovir antiviral drug overviewLisaNoch keine Bewertungen
- Accupuncture Trigger Points and Musculoskeletal PainDokument744 SeitenAccupuncture Trigger Points and Musculoskeletal PainTeaganFalakNoch keine Bewertungen
- Managing corticosteroids and their side effectsDokument6 SeitenManaging corticosteroids and their side effectsKrista Madranca CastroNoch keine Bewertungen
- Oxygen-Induced Hypercapnia in COPD PDFDokument4 SeitenOxygen-Induced Hypercapnia in COPD PDFsatyagraha84Noch keine Bewertungen
- SOCIETY For ENDOCRINOLOGY ENDOCRINE EMERGENCY GUIDANCE - Emergency Management of Acute Adrenal Insufficiency (Adrenal Crisis) in Adult PatientsDokument3 SeitenSOCIETY For ENDOCRINOLOGY ENDOCRINE EMERGENCY GUIDANCE - Emergency Management of Acute Adrenal Insufficiency (Adrenal Crisis) in Adult PatientsMuhammad ReyhanNoch keine Bewertungen
- NEUROPrelims - History Taking in NeurologyDokument4 SeitenNEUROPrelims - History Taking in NeurologyRenatoCosmeGalvanJuniorNoch keine Bewertungen
- Persona Knee Surgical TechniqueDokument72 SeitenPersona Knee Surgical TechniquedrorthokingNoch keine Bewertungen
- Legal and Ethical Issues in Psychiatric NursingDokument38 SeitenLegal and Ethical Issues in Psychiatric NursingElizabeth McKee100% (2)
- Pharmacokinetics Compartment ModelingDokument94 SeitenPharmacokinetics Compartment ModelingPinkishBlue100% (1)