Beruflich Dokumente
Kultur Dokumente
Ctangiographyincomplexupperextremity Reconstruction: Keywords: CT Angiography, Upper Extremity Reconstruction
Hochgeladen von
Irinel BuscaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Ctangiographyincomplexupperextremity Reconstruction: Keywords: CT Angiography, Upper Extremity Reconstruction
Hochgeladen von
Irinel BuscaCopyright:
Verfügbare Formate
ARTICLE IN PRESS
CT ANGIOGRAPHY IN COMPLEX UPPER EXTREMITY RECONSTRUCTION
M. A. BOGDAN, M. B. KLEIN, G. D. RUBIN, T. R. MCADAMS and J. CHANG From the Division of Plastic and Reconstructive Surgery, Department of Radiology, and Hand and Upper Extremity Surgery, Stanford University Medical Center, Stanford, CA 94305 and Section of Plastic Surgery, Veterans Affairs Palo Alto Health Care System, Palo Alto, CA 94304, USA
Computed tomography angiography is a new technique that provides high-resolution, threedimensional vascular imaging as well as excellent bone and soft tissue spatial relationships. The purpose of this study was to examine the use of computed tomography angiography in planning upper extremity reconstruction. Seventeen computed tomography angiograms were obtained in 14 patients over a 20-month period. All studies were obtained on an outpatient basis with contrast administered through a peripheral vein. All the studies demonstrated the pertinent anatomy and the intraoperative ndings were as demonstrated in all cases. Information from two studies signicantly altered pre-operative planning. The average charge for computed tomography angiography was $1,140, compared to $3,900 for traditional angiography. Journal of Hand Surgery (British and European Volume, 2004) 29B: 5: 465469
Keywords: CT angiography, upper extremity reconstruction
INTRODUCTION Vascular imaging is often necessary for pre-operative planning of complex upper extremity reconstructions. Digital subtraction angiography (DSA), magnetic resonance angiography (MRA), and duplex ultrasound have all been used to evaluate the vasculature (Disa et al., 1997; Hutchinson, 1993). Although digital subtraction angiography is considered the gold standard, it has limitations including that it mainly evaluates the arterial system and gives little information regarding the venous anatomy or soft tissue anatomic relationships, and it is relatively expensive. Digital subtraction angiography also has signicant potential complications, including those related to arterial access (bleeding, haematoma, thrombosis, pseudoaneurysm, arteriovenous stula) and the contrast medium (AbuRahma et al., 1993; Dublin et al., 1997; Katz and Kohl, 1994; Sakamoto et al., 1994). Magnetic resonance angiography is another imaging modality that has been used for pre-operative evaluation prior to reconstructive surgery. One potential benet of MRA is that it is less invasive than traditional angiography (Disa et al., 1997; Koelemay et al., 2001; Manaster et al., 1990; Mast, 2001). However, MRA is highly susceptible to movement artefact (due to long acquisition time) and it provides poor visualization of intravascular calcications and bony landmarks. Furthermore the test cannot be performed if the patient has metallic implants in situ. Lastly, patients with claustrophobia do not tolerate the procedure well (Mast, 2001). Computed tomography (CT) angiography is a relatively new procedure that provides high-resolution
465
vascular images and detailed images of the adjacent bone and soft tissue. It is relatively non-invasive, with injection of the contrast medium through a peripheral vein. The accuracy of arterial visualization provided by CT angiography is comparable to that of DSA, and venous phase images are easily obtained (Rubin et al., 1995). Additionally, three-dimensional reformatting allows for excellent appreciation of anatomic relationships between bones, soft tissues, and the vascular system. Application of CT angiography is becoming more widespread, both for major vessel evaluation (thoracic and abdominal aorta) and smaller vascular beds such as the cerebral, pulmonary, renal, and mesenteric arterial systems (Gracias et al., 2001; Rubin et al., 1995; Wilms et al., 1996). Recently, our group has reported the potential utility of CT angiography in planning microsurgical reconstruction (Klein et al., 2003). Indications for upper extremity vascular imaging are varied. In cases of trauma, indications include abnormal distal pulses, signs of haemorrhage, limb ischaemia, turbulent blood ow, injury of an adjacent structure (nerve injury or severe skeletal fracture), or a penetrating injury close to a major vessel (Rose and Moore, 1988). In particular, there is a high incidence of arterial injury in blast injuries and gun shot wounds. In addition, patients with non-traumatic vascular insufciency with either diminished peripheral pulses or clinical signs of ischaemia may require imaging of the upper extremity vasculature. Vascular malformations or tumours near to vessels may also require imaging to assess their resectability and determine the extent of involvement of the vasculature (Disa et al., 1997).
ARTICLE IN PRESS
466
THE JOURNAL OF HAND SURGERY VOL. 29B No. 5 OCTOBER
2004
We report our initial experience with the routine use of CT angiography for vascular assessment in cases of complex upper extremity reconstruction.
PATIENTS AND METHODS Seventeen CT angiograms were obtained in 14 patients from March 2001 to November 2002. All had been referred for a soft tissue and/or bony reconstruction and had an abnormal vascular examination, symptoms of vascular insufciency (cold intolerance, positional weakness and parasthesiae with associated loss of pulse), or a history of a crush injury. Fourteen of the 17 CT angiograms were obtained to evaluate the upper extremity of interest, and three were obtained to evaluate the vascularized bular donor site before an upper extremity reconstruction. All images were performed on an outpatient basis using either a four detector-row Somatom Volume Zoom CT scanner (Siemens Medical Systems, Erlangen, Germany), or an eight or 16-row General Electric LightSpeed CT scanner (General Electric Medical Systems, Milwaukee, WI). An initial scout image was obtained to determine the scan volume. After placement of a 20-gauge intravenous catheter in a vein in the antecubital fossa of the contralateral arm, a dynamic timing-bolus acquisition was performed. Time to peak enhancement at this level was determined by region-ofinterest analysis and used as the scan delay for the CT angiogram. Non-ionic contrast with 300 mg I/ml (Omnipaque) was administered intravenously with a power injector (EnVision CT, Medrad, Indianola, PA) at a rate of 5 ml/s. The total volume of contrast administered was determined by the product of the scan time (s) and the injection rate. The following scan parameters were used: 1.25 mm nominal section thickness, beam pitch 1.5, and 4 1 mm2 mode on the Volume Zoom and 8 1.25 mm2 or 16 1.25 mm2 modes on the LightSpeed scanners.
Computed tomography data were transferred to an Advantage Windows 4.1 workstation (General Electric Medical Systems, Milwaukee, WI) for the creation of alternative visualizations using volume rendering, curved planar reformations, and maximum intensity projections. All studies were interpreted by a single staff radiologist with expertise in CT angiography (G.D.R.) and evaluated for arterial variants and anomalies, the presence of vascular disease, and bone and soft tissue anatomy. Several criteria were utilized to assess the suitability of CT angiography for routine use in upper extremity imaging. These included clarity of the images, correlation with the intraoperative ndings, complications related to the study and the cost of the study compared with digital subtraction angiography.
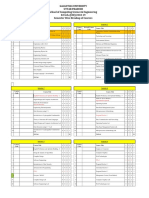
RESULTS Seventeen CT angiograms were performed in 14 patients with a mean age of 37 (range 565) years (Table 1). Eight were men and six were women. Twelve patients were undergoing reconstruction of traumatic injuries, six of which were acute. Five patients were being evaluated for symptomatic vascular insufciency. The upper extremity was studied in all patients, as well as the lower extremities of three patients in whom bula free aps were planned. One patient had a shellsh allergy, and premedication with Benadryl and SoluMedrol was administered. There were no complications related to the CT angiograms, and all studies were technically adequate. Six patients had abnormal peripheral vascular examinations and their computed tomography angiograms all revealed defects which were consistent with the clinical ndings. Two patients with normal pulses had signicant abnormalities on CT angiography (vascular calcications and incomplete palmar arch). Intraoperative ndings were as predicted by CT angiography in all cases. Information from two studies
Table 1 Patient 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Age 58 65 46 31 20 18 59 18 61 57 16 37 5 23 Sex M F F F M F M F M M M M M F Study UE Upper Thorax UE/LE UE UE UE UE UE UE/LE UE UE UE/LE UE UE Indication Hand ischaemia Subclavian pseudoaneurysm Fibrous dysplasia (s/p proximal radius resection) Palmar wrist ganglion with vascular compromise Avulsion injury, open elbow Degloving injury Crush injury, exposed exors Crush-avulsion, exposed bone Crush injury, segmental bone loss Crush injury Near amputation (arm) Both bone forearm fracture, segmental bone loss Supracondylar fracture, vascular compromise Crush-avulsion, exposed tendon
ARTICLE IN PRESS
CT ANGIOGRAPHY
467
(Cases 7 and 9) signicantly altered the preoperative planning, with both showing sub-optimal recipient vessels for a vascularized tissue transfer. We did not feel patient number seven had a suitable target vessel and the leg vessels of patient number nine had signicant calcications. Therefore, plans for free ap reconstruction were aborted. We also performed a cost analysis of CT angiography at our institution. The average CT angiogram charge was $1,140, while for traditional arteriography it was $3,900 (professional fees included). The average costs for extremity duplex ultrasound was $450 and for upper extremity magnetic resonance angiography it was $2,500. Case reports Case 3 This 46-year-old woman with a history of brous dysplasia had undergone a resection of her proximal radius 20 years previously. She presented with painful progressive wrist instability with proximal migration of the distal radius. The operative plan was to reconstruct the radius with a vascularized bula ap. Computed tomography angiography was performed on the forearm and both lower extremities and the study demonstrated a normal forearm arterial tree and three-vessel runoff to the foot bilaterally (Fig 1). These images demonstrate the spatial anatomic information attainable with volume rendering. Proximal radial reconstruction was performed with a free bula ap and a radial head prosthesis without complication. Case 4 This 31-year-old woman had 5 years previously suffered a laceration to the ulnar aspect of her wrist, with injury to ulnar artery and nerve, and several exor
tendons. Repair of all these structures, except the artery, had been performed at an outside medical center. She presented to our clinic with a palmar wrist ganglion over her radial artery and complaints of cold intolerance. Physical examination revealed an intact radial artery directly abutting the 2 2 cm2 ganglion, and no palpable ulnar artery. A CT angiogram was obtained to evaluate her vasculature (Fig 2). One of the benets of CT angiography is the ability to add and subtract bone and soft tissues from the vasculature and to highlight objects of interest. This study demonstrates this ability, clearly showing the intimate association of the radial artery with the ganglion. Of note, the
Fig 2
Hand CT angiogram of a patient with previous ulnar artery laceration and a symptomatic palmar wrist ganglion.
Fig 1 Upper and lower extremity CT angiogram revealing normal vasculature in a patient with a proximal radius defect following to resection for brous dysplasia.
ARTICLE IN PRESS
468
THE JOURNAL OF HAND SURGERY VOL. 29B No. 5 OCTOBER
2004
resolution of current generation CT scanners is not high enough to study the digital vasculature. The patient eventually declined reconstruction of the ulnar artery, and ganglion excision was performed without event. Case 8 This 18-year-old woman was a passenger involved in a rollover motor vehicle accident in which her dominant hand suffered a dorsal crush avulsion injury to the level of bone. The vascular examination revealed weak radial and ulnar pulses. The pre-operative plan was to use either a reversed radial forearm ap or a lateral arm free-ap to resurface the dorsum of the hand. A CT angiogram was obtained to assess the radial artery since it was within the zone of injury. This demonstrated normal upper extremity vascular anatomy (Fig 3), and the patient underwent a reversed radial forearm ap reconstruction without complications. Case 9 This 61-year-old man was involved in a motorcycle accident and sustained an open comminuted Monteggia fracture with a radial head dislocation and soft tissue loss. Initial debridement and external xation were performed at an outside facility. Postoperatively, the patient developed osteomyelitis requiring debridement and signicant bone resection. Both upper and lower extremity pulses were normal and there was symmetric ow on Allens test. Due to his history of massive crush injury, CT angiography of the upper extremity was performed as well as bilateral lower extremity CT angiograms to evaluate the vasculature for potential free bular donor sites (Fig 4). There was minimal interference from the external xator (EBI, Parsippany, New Jersey), except on the axial views. Lower extremity
CT angiograms demonstrated severe calcications bilaterally. Based on the extent of the vascular disease, a one-bone forearm procedure was performed instead of a free bula reconstruction.
DISCUSSION Computed tomography angiography is a relatively new technique which is capable of providing high-resolution
Fig 3
Normal upper extremity CT angiogram of a patient with exposed bone and tendon following a dorsal hand crushavulsion injury.
Fig 4 A Monteggia fracture with severe comminution and bone loss following a high-energy injury. Upper and lower extremity CT angiograms reveal extensive arterial calcication in the ulnar artery and lower extremity vessels. (Note the minimal interference from the external xator).
ARTICLE IN PRESS
CT ANGIOGRAPHY
469
vascular imaging. In this study, we examined the utility of CT angiography for imaging of the upper extremity following trauma, as well as for patients with symptoms of vascular insufciency. Although angiography is the standard technique for vascular imaging, the potential complications, high cost and prolonged recovery period make conventional angiography less desirable for routine use. CT angiography has many advantages over traditional angiography. It demonstrates more anatomical detail and has the ability to add and subtract bone, soft tissue, hardware, arteries and veins to provide unparalleled spatial detail. In addition, CT angiography is performed by contrast injection through a peripheral vein, eliminating the risks associated with arterial puncture. Three to ve per cent complication rates have been reported for arterial puncture and include bleeding, haematoma, thrombosis, arteriovenous stula and pseudoaneurysm (AbuRahma et al., 1993; Dublin et al., 1997; Katz and Kohl, 1994; Sakamoto et al., 1994). Furthermore, the radiation exposure with conventional angiography is nearly four times the amount with comparable CT angiography (Rubin et al., 2001). When compared with traditional angiography, the acquisition time and examination cost of CT angiography are signicantly lower. Given the short acquisition and processing times and the need for only a peripheral intravenous catheter, we have been able to obtain these studies on as required, even in emergencies, basis. The cost of traditional angiography includes the study itself, the interventional radiology suite time, reading of the study, and the hospital stay (following a conventional angiogram patients must have 6 hours of bed rest) (Dublin et al., 1997). At our institution, the average CT angiogram charge was $1,140 and for traditional arteriography it was $3,900, including professional fees. The amount of contrast required for each procedure was approximately equivalent and, thus CT angiography does not decrease the risk for renal failure.
References
AbuRahma AF, Robinson PA, Boland JP et al. (1993). Complications of arteriography in a recent series of 707 cases: factors affecting outcome. Annals of Vascular Surgery, 7: 122129. Disa JJ, Chung KC, Gellad FE, Bickel KD, Wilgis EFS (1997). Efcacy of magnetic resonance angiography in the evaluation of vascular malformations of the hand. Plastic and Reconstructive Surgery, 99: 136144. Dublin BA, Karp NS, Kasabian AK, Kolker AR, Shah MH (1997). Selective use of preoperative lower extremity arteriography in free ap reconstruction. Annals of Plastic Surgery, 38: 404407. Gracias VH, Reilly PM, Philpott J et al. (2001). Computed tomography in the evaluation of penetrating neck trauma. Archives of Surgery, 136: 12311235. Hutchinson DT (1993). Color duplex imaging. Applications to upper-extremity and microvascular surgery. Hand Clinics, 9: 4757. Katz SG, Kohl RD (1994). Angiographic catheter induced arterial occlusion. Journal of the American College of Surgery, 178: 439442. Klein MB, Karanas YL, Chow LC, Rubin GD, Chang J (2003). Early experience with computed tomographic angiography in microsurgical reconstruction. Plastic and Reconstructive Surgery, 112: 498503. Koelemay MJW, Lijmer JG, Stoker J, Legemate DA, Bossuyt PM (2001). Magnetic resonance angiography for the evaluation of lower extremity arterial disease: a meta-analysis. Journal of the American Medical Association, 285: 13381345. Manaster BJ, Coleman DA, Bell DA (1990). Magnetic resonance imaging of vascular anatomy before vascularized bular grafting. Journal of Bone and Joint Surgery, 72-A: 409414. Mast BA (2001). Comparison of magnetic resonance angiography and digital subtraction angiography for visualization of lower extremity arteries. Annals of Plastic Surgery, 46: 261264. Rose SC, Moore EE (1988). Trauma angiography of the extremity: the impact of injury mechanism on triage decisions. Cardiovascular and Interventional Radiology, 11: 136139. Rubin GD, Dake MD, Semba CP (1995). Current status of three-dimensional spiral CT scanning for imaging the vasculature. Radiologic Clinics of North America, 33: 5170. Rubin GD, Schmidt AJ, Logan LJ, Solos MC (2001). Multi-detector row CT angiography of lower extremity arterial inow and runoff: initial experience. Radiology, 221: 146158. Sakamoto I, Hayashi K, Matsunaga N et al. (1994). Aortic dissection caused by angiographic procedures. Radiology, 191: 467471. Wilms G, Guffens M, Gryspeerdt S et al. (1996). Spiral CT of intracranial aneurysms: correlation with digital subtraction and magnetic resonance angiography. Neuroradiology, 38: S20S25.
Received: 1 October 2003 Accepted after revision: 7 April 2004 Dr J. Chang, Division of Plastic Surgery, Stanford University Medical Center, NC-104, Stanford CA 94305, USA. Tel.: +1-650-723-5824; fax: +1-650-725-6605; E-mail: changhand@aol.com
r 2004 The British Society for Surgery of the Hand. Published by Elsevier Ltd. All rights reserved. doi:10.1016/j.jhsb.2004.04.006 available online at http://www.sciencedirect.com
Das könnte Ihnen auch gefallen
- The Pattern and Prevalence of Vertebral Artery Injury in Patients With Cervical Spine FracturesDokument4 SeitenThe Pattern and Prevalence of Vertebral Artery Injury in Patients With Cervical Spine FracturesFrontiersNoch keine Bewertungen
- 249 FullDokument7 Seiten249 Fullwan hanisaNoch keine Bewertungen
- CT Angiography in Vertebral Artery DissectionDokument6 SeitenCT Angiography in Vertebral Artery DissectionDaniel AraujoNoch keine Bewertungen
- 2013 Adjustment of The Surgical Plan in Repair of Congenital Heart Disease - The Power of Cross-Sectional Imaging and Three-Dimensional VisualizationDokument6 Seiten2013 Adjustment of The Surgical Plan in Repair of Congenital Heart Disease - The Power of Cross-Sectional Imaging and Three-Dimensional Visualizationccvped3dNoch keine Bewertungen
- CT Angiography Versus Digital Subtraction Angiography For Intracranial Vascular Pathology in A Clinical SettingDokument9 SeitenCT Angiography Versus Digital Subtraction Angiography For Intracranial Vascular Pathology in A Clinical SettingPari Pengda BaliNoch keine Bewertungen
- Inggris PDFDokument6 SeitenInggris PDFChimul Lavigne 'L'Noch keine Bewertungen
- RAD Head and Neck Vascular Lesions by CT Korean J RadiolDokument10 SeitenRAD Head and Neck Vascular Lesions by CT Korean J RadiolyellowbieNoch keine Bewertungen
- 319 FullDokument8 Seiten319 FullDavy JonesNoch keine Bewertungen
- Carotid Endarterectomy: Experience in 8743 Cases.Dokument13 SeitenCarotid Endarterectomy: Experience in 8743 Cases.Alexandre Campos Moraes AmatoNoch keine Bewertungen
- 1 s2.0 S1010518216000652 Main PDFDokument9 Seiten1 s2.0 S1010518216000652 Main PDFRoberto AmayaNoch keine Bewertungen
- Norbash 99 AjnrDokument7 SeitenNorbash 99 Ajnrthor112Noch keine Bewertungen
- 1996 A Novel Computer-Assisted Volumetric Stereotactic Approach For Resecting Tumors of The Posterior Parahippocampal GyrusDokument6 Seiten1996 A Novel Computer-Assisted Volumetric Stereotactic Approach For Resecting Tumors of The Posterior Parahippocampal Gyrusİbrahim ErkutluNoch keine Bewertungen
- CT Angiography in The Evaluation of Acute StrokeDokument10 SeitenCT Angiography in The Evaluation of Acute StrokeDio SukardiNoch keine Bewertungen
- 17 Myectomy in HCMDokument5 Seiten17 Myectomy in HCME-hastaneNoch keine Bewertungen
- CT AngioDokument5 SeitenCT Angiocooldude_secbad1712Noch keine Bewertungen
- Management of True Aneurysms of Hemodialysis Access FistulasDokument7 SeitenManagement of True Aneurysms of Hemodialysis Access FistulasbobbyNoch keine Bewertungen
- Radiology Case ReportsDokument5 SeitenRadiology Case ReportsLaila Maria UlfahNoch keine Bewertungen
- CT Angiography of The Lower Extremities The Peripheral Vascular System Presents Unique Imaging ChallengesDokument7 SeitenCT Angiography of The Lower Extremities The Peripheral Vascular System Presents Unique Imaging ChallengesDavid Puyó100% (1)
- Paper 1Dokument18 SeitenPaper 1Ying-Chi ChuNoch keine Bewertungen
- 405 2013 Article 2598Dokument5 Seiten405 2013 Article 2598M Shiddiq GhiffariNoch keine Bewertungen
- A-Line Complication PDFDokument8 SeitenA-Line Complication PDFaeagesNoch keine Bewertungen
- Koyama Et Al 2002 Primary Hepatic Angiosarcoma Findings at CT and MR ImagingDokument7 SeitenKoyama Et Al 2002 Primary Hepatic Angiosarcoma Findings at CT and MR ImagingThanh NguyenNoch keine Bewertungen
- Mitral Valve Annular Downsizing Forces: Implications For Annuloplasty Device DevelopmentDokument8 SeitenMitral Valve Annular Downsizing Forces: Implications For Annuloplasty Device Developmentdiana25Noch keine Bewertungen
- Percutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaDokument6 SeitenPercutaneous Transluminal Angioplasty and Stenting As First-Choice Treatment in Patients With Chronic Mesenteric IschemiaCotaga IgorNoch keine Bewertungen
- 1369 Full PDFDokument9 Seiten1369 Full PDFIqbal AbdillahNoch keine Bewertungen
- 1 s2.0 S0894731723002006 MainDokument7 Seiten1 s2.0 S0894731723002006 Mainflying highNoch keine Bewertungen
- Cardiac ValveDokument21 SeitenCardiac ValveSean ChenNoch keine Bewertungen
- Lemus Rangel 2010Dokument2 SeitenLemus Rangel 2010audiNoch keine Bewertungen
- Asensio, JA, (2020) - Tratamiento Quirúrgico de Las Lesiones de La Arteria Braquial y Predictores de Resultado.Dokument12 SeitenAsensio, JA, (2020) - Tratamiento Quirúrgico de Las Lesiones de La Arteria Braquial y Predictores de Resultado.Edgar Geovanny Cardenas FigueroaNoch keine Bewertungen
- Evaluation of A Scoring System For Extracranial Carotid Atherosclerosis Extent With B-Mode Ultrasound, 1986Dokument7 SeitenEvaluation of A Scoring System For Extracranial Carotid Atherosclerosis Extent With B-Mode Ultrasound, 1986CAMILO ARMANDO BENAVIDES BURBANONoch keine Bewertungen
- Nuclear Cardiology: Role in The World of Multimodality Cardiac ImagingDokument5 SeitenNuclear Cardiology: Role in The World of Multimodality Cardiac ImagingElena FlorentinaNoch keine Bewertungen
- The Fate of The Distal Aorta After Repair of Acute Type A Aortic DissectionDokument10 SeitenThe Fate of The Distal Aorta After Repair of Acute Type A Aortic Dissectionapi-160333876Noch keine Bewertungen
- Preoperative Angiography and Embolization of Large Pelvic TumorsDokument4 SeitenPreoperative Angiography and Embolization of Large Pelvic TumorsPaul AsturbiarisNoch keine Bewertungen
- Advanced Assessment of Cardiac Morphology and Prediction of Gene Carriage by CMR in Hypertrophic Cardiomyopathy The Hcmnet Ucl CollaborationDokument3 SeitenAdvanced Assessment of Cardiac Morphology and Prediction of Gene Carriage by CMR in Hypertrophic Cardiomyopathy The Hcmnet Ucl CollaborationAfreen BegumNoch keine Bewertungen
- (10920684 - Neurosurgical Focus) Falcotentorial Meningiomas - Clinical, Neuroimaging, and Surgical Features in Six PatientsDokument7 Seiten(10920684 - Neurosurgical Focus) Falcotentorial Meningiomas - Clinical, Neuroimaging, and Surgical Features in Six PatientsPutri PrameswariNoch keine Bewertungen
- Hybrid Repair of Aortic Arch AneurysmDokument8 SeitenHybrid Repair of Aortic Arch AneurysmFrancesca MazzolaniNoch keine Bewertungen
- Lymphedema Rates in Pedicled ALTP For Coverage in Irradiated Groin Defects 2019Dokument4 SeitenLymphedema Rates in Pedicled ALTP For Coverage in Irradiated Groin Defects 2019yeapdshengNoch keine Bewertungen
- Angiosarcoma of The Spleen: Imaging Characteristics in 12 PatientsDokument10 SeitenAngiosarcoma of The Spleen: Imaging Characteristics in 12 PatientsHuyen NguyenNoch keine Bewertungen
- CarcassoaDokument7 SeitenCarcassoaIulia LupascuNoch keine Bewertungen
- (10920684 - Neurosurgical Focus) Surgical Treatment of Primary Sacral Tumors - Complications Associated With SacrectomyDokument8 Seiten(10920684 - Neurosurgical Focus) Surgical Treatment of Primary Sacral Tumors - Complications Associated With Sacrectomyfloroiu.ioana.valeriaNoch keine Bewertungen
- Aspect ScoreDokument9 SeitenAspect ScorePretty RoselyNoch keine Bewertungen
- CardiologyDokument11 SeitenCardiologyandreaNoch keine Bewertungen
- s0735 1097 (85) 80117 0Dokument8 Seitens0735 1097 (85) 80117 0John DoeNoch keine Bewertungen
- CTperfusion TeoreticDokument7 SeitenCTperfusion TeoreticarthaaaaaNoch keine Bewertungen
- Kim 2001Dokument5 SeitenKim 2001DH SiriruiNoch keine Bewertungen
- 145 Full PDFDokument7 Seiten145 Full PDFWildaHanimNoch keine Bewertungen
- 10 1 1 525 6842Dokument6 Seiten10 1 1 525 6842sandyNoch keine Bewertungen
- Rolf2013 Article PreproceduralCoronaryCTAngiogrDokument9 SeitenRolf2013 Article PreproceduralCoronaryCTAngiogrرقية ياسينNoch keine Bewertungen
- Arteriovenous Malformations of The Body and Extremities: Analysis of Therapeutic Outcomes andDokument12 SeitenArteriovenous Malformations of The Body and Extremities: Analysis of Therapeutic Outcomes andClaudio SalazarNoch keine Bewertungen
- Vertebrobasilar Dolichoectasia Diagnosed by Magnetic Resonance Angiography and Risk of Stroke and Death: A Cohort StudyDokument6 SeitenVertebrobasilar Dolichoectasia Diagnosed by Magnetic Resonance Angiography and Risk of Stroke and Death: A Cohort StudyRajesh SharmaNoch keine Bewertungen
- Functional Outcome Following A Locked FRDokument6 SeitenFunctional Outcome Following A Locked FRAndrejShNoch keine Bewertungen
- 3D Transthoracic Echocardiography Provides Accurate Cross-Sectional Area of The RV Outflow Tract - 1Dokument3 Seiten3D Transthoracic Echocardiography Provides Accurate Cross-Sectional Area of The RV Outflow Tract - 1Thumper KatesNoch keine Bewertungen
- Retrolaparoscopic Adrenalectomy Assisted by Three-Dimensional Reconstructed Digital Model in A Patient With Situs Inversus TotalisDokument5 SeitenRetrolaparoscopic Adrenalectomy Assisted by Three-Dimensional Reconstructed Digital Model in A Patient With Situs Inversus Totalisyerich septaNoch keine Bewertungen
- Multidetector Row Computed Tomography ArteriographDokument2 SeitenMultidetector Row Computed Tomography ArteriographApple StarNoch keine Bewertungen
- Right Coronary Artery-Right Atrial Fistula in Right Atrial Myxoma A Rare CombinationDokument3 SeitenRight Coronary Artery-Right Atrial Fistula in Right Atrial Myxoma A Rare CombinationAxel Hiram Hernandez PinedaNoch keine Bewertungen
- Carotid ArteryDokument5 SeitenCarotid ArteryAsif AyazNoch keine Bewertungen
- PregnancyDokument4 SeitenPregnancymutiahmuftihNoch keine Bewertungen
- P1337430319048 - Artikel Jurnal 1Dokument6 SeitenP1337430319048 - Artikel Jurnal 1maulanagam69Noch keine Bewertungen
- 1 s2.0 S0735109786800183 Main PDFDokument252 Seiten1 s2.0 S0735109786800183 Main PDFdangthieuhoiNoch keine Bewertungen
- MRI Issue 5Dokument91 SeitenMRI Issue 5Irinel Busca100% (1)
- GEHC Site Planning Final Drawing Senographe Essential PDFDokument8 SeitenGEHC Site Planning Final Drawing Senographe Essential PDFIrinel Busca100% (1)
- Waiting For Answers After An Abnormal Mammogram?: Know Sooner With Senobright CesmDokument2 SeitenWaiting For Answers After An Abnormal Mammogram?: Know Sooner With Senobright CesmIrinel BuscaNoch keine Bewertungen
- GEHC Site Planning Final Drawing Discovery CT 750 HD 1700 Table 8x System PDFDokument8 SeitenGEHC Site Planning Final Drawing Discovery CT 750 HD 1700 Table 8x System PDFIrinel BuscaNoch keine Bewertungen
- GEHC Site Planning Final Drawing Performa System PDFDokument6 SeitenGEHC Site Planning Final Drawing Performa System PDFIrinel BuscaNoch keine Bewertungen
- GEHC Site Planning Final Drawing Senographe Essential PDFDokument8 SeitenGEHC Site Planning Final Drawing Senographe Essential PDFIrinel BuscaNoch keine Bewertungen
- GEHC Site Planning Technical Guide Mammo QUICK GUIDE XLS 1Dokument5 SeitenGEHC Site Planning Technical Guide Mammo QUICK GUIDE XLS 1Irinel BuscaNoch keine Bewertungen
- 5160036-11-8EN Rev 1Dokument92 Seiten5160036-11-8EN Rev 1Irinel BuscaNoch keine Bewertungen
- GEHC Site Planning Final Drawing Diamond System PDFDokument6 SeitenGEHC Site Planning Final Drawing Diamond System PDFIrinel BuscaNoch keine Bewertungen
- GEHC Site Planning Final Drawing Discovery CT 750 HD 1700 Table 8x System PDFDokument8 SeitenGEHC Site Planning Final Drawing Discovery CT 750 HD 1700 Table 8x System PDFIrinel BuscaNoch keine Bewertungen
- MMSLists Successful Email Marketing MethodsDokument15 SeitenMMSLists Successful Email Marketing MethodsIrinel Busca0% (1)
- Document of The World BankDokument92 SeitenDocument of The World BankIrinel BuscaNoch keine Bewertungen
- Aquilion16 Mpdct0220eadDokument16 SeitenAquilion16 Mpdct0220eadIrinel BuscaNoch keine Bewertungen
- Maya Deren PaperDokument9 SeitenMaya Deren PaperquietinstrumentalsNoch keine Bewertungen
- 18 Composition Rules For Photos That ShineDokument20 Seiten18 Composition Rules For Photos That Shinemahfuzkhan100% (1)
- Chapter 5 Constructing An Agile Implementation PlanDokument4 SeitenChapter 5 Constructing An Agile Implementation PlanAHMADNoch keine Bewertungen
- Case Study - Suprema CarsDokument5 SeitenCase Study - Suprema CarsALFONSO PATRICIO GUERRA CARVAJALNoch keine Bewertungen
- The Mooring Pattern Study For Q-Flex Type LNG Carriers Scheduled For Berthing at Ege Gaz Aliaga LNG TerminalDokument6 SeitenThe Mooring Pattern Study For Q-Flex Type LNG Carriers Scheduled For Berthing at Ege Gaz Aliaga LNG TerminalMahad Abdi100% (1)
- Virtual WorkDokument12 SeitenVirtual Workdkgupta28Noch keine Bewertungen
- Sundar Pichai PDFDokument6 SeitenSundar Pichai PDFHimanshi Patle100% (1)
- Genuine Fakes: How Phony Things Teach Us About Real StuffDokument2 SeitenGenuine Fakes: How Phony Things Teach Us About Real StuffGail LeondarWrightNoch keine Bewertungen
- W.C. Hicks Appliances: Client Name SKU Item Name Delivery Price Total DueDokument2 SeitenW.C. Hicks Appliances: Client Name SKU Item Name Delivery Price Total DueParth PatelNoch keine Bewertungen
- Fuzzy Gain Scheduled Pi Controller For ADokument5 SeitenFuzzy Gain Scheduled Pi Controller For AOumayNoch keine Bewertungen
- Lab 3 Arduino Led Candle Light: CS 11/group - 4 - Borromeo, Galanida, Pabilan, Paypa, TejeroDokument3 SeitenLab 3 Arduino Led Candle Light: CS 11/group - 4 - Borromeo, Galanida, Pabilan, Paypa, TejeroGladys Ruth PaypaNoch keine Bewertungen
- CURRICULUM PharmasubDokument10 SeitenCURRICULUM PharmasubZE Mart DanmarkNoch keine Bewertungen
- Engleza Referat-Pantilimonescu IonutDokument13 SeitenEngleza Referat-Pantilimonescu IonutAilenei RazvanNoch keine Bewertungen
- Pathogenic Escherichia Coli Associated With DiarrheaDokument7 SeitenPathogenic Escherichia Coli Associated With DiarrheaSiti Fatimah RadNoch keine Bewertungen
- FMEA Minus The PainDokument7 SeitenFMEA Minus The PainMUNISNoch keine Bewertungen
- Safety Data Sheet SDS For CB-G PG Precision Grout and CB-G MG Multipurpose Grout Documentation ASSET DOC APPROVAL 0536Dokument4 SeitenSafety Data Sheet SDS For CB-G PG Precision Grout and CB-G MG Multipurpose Grout Documentation ASSET DOC APPROVAL 0536BanyuNoch keine Bewertungen
- SIVACON 8PS - Planning With SIVACON 8PS Planning Manual, 11/2016, A5E01541101-04Dokument1 SeiteSIVACON 8PS - Planning With SIVACON 8PS Planning Manual, 11/2016, A5E01541101-04marcospmmNoch keine Bewertungen
- Safety Bulletin 09 - Emergency Escape Breathing Device - Product RecallDokument2 SeitenSafety Bulletin 09 - Emergency Escape Breathing Device - Product RecallMuhammadNoch keine Bewertungen
- ST Arduino Labs CombinedDokument80 SeitenST Arduino Labs CombineddevProNoch keine Bewertungen
- Vitamins - CyanocobalaminDokument12 SeitenVitamins - CyanocobalaminK PrashasthaNoch keine Bewertungen
- Central University of Karnataka: Entrance Examinations Results 2016Dokument4 SeitenCentral University of Karnataka: Entrance Examinations Results 2016Saurabh ShubhamNoch keine Bewertungen
- DirectionDokument1 SeiteDirectionJessica BacaniNoch keine Bewertungen
- Mcdaniel Tanilla Civilian Resume Complete v1Dokument3 SeitenMcdaniel Tanilla Civilian Resume Complete v1api-246751844Noch keine Bewertungen
- PETAL Sentence StartersDokument1 SeitePETAL Sentence StartersSnip x Hunt manNoch keine Bewertungen
- Galgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesDokument2 SeitenGalgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesRohit Singh BhatiNoch keine Bewertungen
- Full Project LibraryDokument77 SeitenFull Project LibraryChala Geta0% (1)
- Ch-10 Human Eye Notes FinalDokument27 SeitenCh-10 Human Eye Notes Finalkilemas494Noch keine Bewertungen
- Saiva Dharma ShastrasDokument379 SeitenSaiva Dharma ShastrasfunnybizNoch keine Bewertungen
- GGG Sri MDokument2 SeitenGGG Sri MGiovanni LuigiNoch keine Bewertungen
- ICMApprovedCentres - Ghana PDFDokument8 SeitenICMApprovedCentres - Ghana PDFPrince Kelly100% (2)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (31)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4 von 5 Sternen4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsVon EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsBewertung: 4.5 von 5 Sternen4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisVon EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisBewertung: 5 von 5 Sternen5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassVon EverandTroubled: A Memoir of Foster Care, Family, and Social ClassBewertung: 4.5 von 5 Sternen4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingVon EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingBewertung: 4 von 5 Sternen4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (253)