Beruflich Dokumente
Kultur Dokumente
MEJP Memo On MOE LePage Cuts
Hochgeladen von
gerald7783Originalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
MEJP Memo On MOE LePage Cuts
Hochgeladen von
gerald7783Copyright:
Verfügbare Formate
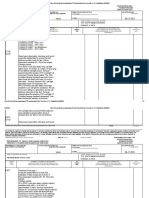
DHHS Supplemental Budget Proposals and the Maintenance of Effort (MOE) Provisions of the Affordable Care Act
Much of what is proposed with respect to elimination of eligibility under this budget violates the maintenance of effort requirements (MOE) of the Affordable Care Act (ACA) and is illegal. The ACA requires that, as a condition of receiving Federal Medicaid funding (approximately $1.5 billion in federal funding per state fiscal year in Maine), states must maintain Medicaid eligibility standards, methodologies and procedures that are no more restrictive than those in effect on March 23, 2010. The following budget proposals violate MOE requirements of the ACA:
1. Reducing eligibility for the Medicare Savings Program (MSP, or the Medicare
Buy-In Program) MOE is violated when a state puts into effect eligibility standards, methodologies, or procedures . . . that are more restrictive than the eligibility standards, methodologies, or procedures . . . than those that were in effect on March 23, 2010.1 Maines Medicare Savings Program (the MSP program for QMBs, SLMBs and QIs) is a Medicaid eligibility group. CMS approved Maines use of an eligibility standard and methodology to achieve its current eligibility levels. Making that eligibility standard and methodology more restrictive than what Maine had in place on March 23, 2010 violates MOE. This proposal was also made in the biennial budget. On May 24, 2011, CMS notified the Commissioner that it violated the MOE provisions of the ACA.
2. Eliminating eligibility for parents under 133% of the federal poverty level
MOE requirements apply to non-disabled, non-pregnant adults whose income is below 133% of FPL. Even when a State certifies to the Secretary of HHS that it has or projects a budget deficit, as our State has done, this requirement remains in force protecting adults with incomes at or below 133% of the federal poverty level.
3. Eliminating eligibility for 19 and 20 year olds under 150% of the federal
poverty level The budget deficit exemption to the MOE requirements allows states with documented budget deficits to reduce eligibility to 133% of the poverty level for non-disabled adults. However, this exemption does not apply to children. Under the ACA, 19 and 20 year olds are considered to be children. The Act strictly requires that eligibility for these children must 1 The law exempts from the MOE requirements non-disabled, non-pregnant adults whose income is over 133% of FPL.
continue without change until October 1st 2019. The State may not eliminate coverage for 19 and 20 year olds.
DHHS has acknowledged that these three proposals would violate the ACA and require waivers from the Affordable Care Act. However, a waiver could not be lawfully granted under these circumstances. The waiver authority generally available to states under Section 1115 of the Social Security Act2 permits only experimental, pilot or demonstration projects which, in the judgment of the Secretary, are likely to assist in promoting the objectives of the Act. In a recent 9th Circuit decision in the case of Newton-Nations v. Betlach,3 the Court of Appeals provided some guidance on this issue. Although analyzing a different kind of state waiver request, the Court held that a Section 1115 waiver can only be granted when the Secretary of HHS makes some judgment that the project has research or demonstration value. A simple benefits cut, which might save money, but has no research or experimental goal, would not satisfy this requirement.4 The proposals listed above do not seek to test a hypothesis; they have only been proposed to save money. Nor do these proposals assist in promoting the objectives of the Act. The MOE provisions in the ACA were designed to keep Medicaid and CHIP coverage stable and to protect people until Medicaid coverage expands under health reform. For these reasons, a waiver of the MOE requirements cannot be granted under federal law. To date, no state has received a waiver of the MOE requirements under these circumstances. Although a few states have sought waivers to circumvent this MOE requirement, no such waiver has been granted. Arizona is the only state that has actually implemented enrollment freezes or cuts in its Medicaid or CHIP program since the MOE requirement went into effect. These cuts were exempted from the MOE requirements because they only applied to populations that were covered under the states Section 1115 waiver, which expired on September 30, 2011. Notably, several other waivers that Arizona sought from CMS were denied. For example, Arizona requested permission to freeze enrollment for parents between 75% and 100% of the FPL and to expand mandatory copayments and these proposals were expressly denied by CMS. The populations discussed above that would lose MaineCare coverage are not covered by a Section 1115 waiver that is set to expire. These proposals also fail to meet the budget deficit exemption as they would impermissibly restrict eligibility in the Medicare Saving 2 42 U.S.C. Section 1315.
3 2011 WL 5084839 at 9 (9th Cir. Oct. 27, 2011).
4 Id. at 1069.
Program, cut eligibility for children ages 19 and 20, and cut eligibility for parents under 133% of the FPL.
Das könnte Ihnen auch gefallen
- Maine SY2018-19 EPS Funding by TownDokument7 SeitenMaine SY2018-19 EPS Funding by Towngerald7783Noch keine Bewertungen
- Maine Attorney General Opinion On Adjournment and LePage VetoesDokument7 SeitenMaine Attorney General Opinion On Adjournment and LePage VetoesthisdogNoch keine Bewertungen
- Maine Superior Court Decision CMP CorridorDokument30 SeitenMaine Superior Court Decision CMP Corridorgerald7783Noch keine Bewertungen
- Proposed Rockland Parking GarageDokument3 SeitenProposed Rockland Parking Garagegerald7783Noch keine Bewertungen
- Typical End of Maine Legislative SessionDokument2 SeitenTypical End of Maine Legislative Sessiongerald7783Noch keine Bewertungen
- MacDonald Letter To Thomaston BlastowDokument2 SeitenMacDonald Letter To Thomaston Blastowgerald7783Noch keine Bewertungen
- Rockland NBZ OrdinanceDokument7 SeitenRockland NBZ Ordinancegerald7783Noch keine Bewertungen
- Testimony in Support of LD87 An Act To Bottle Redemption Deposit (To 25 Cents)Dokument3 SeitenTestimony in Support of LD87 An Act To Bottle Redemption Deposit (To 25 Cents)gerald7783Noch keine Bewertungen
- Rockland NBZ OrdinanceDokument7 SeitenRockland NBZ Ordinancegerald7783Noch keine Bewertungen
- LePage Letter To Lawmakers On Madison PaperDokument2 SeitenLePage Letter To Lawmakers On Madison PaperthisdogNoch keine Bewertungen
- Global Strategy Group Maine 2nd District PollDokument1 SeiteGlobal Strategy Group Maine 2nd District Pollgerald7783Noch keine Bewertungen
- Maine Legislative Record 30 June 2015Dokument4 SeitenMaine Legislative Record 30 June 2015gerald7783Noch keine Bewertungen
- Maine Gov LePage Judicial Withdrawal Letters 10-20-17Dokument5 SeitenMaine Gov LePage Judicial Withdrawal Letters 10-20-17gerald7783Noch keine Bewertungen
- Rockland NBZ OrdinanceDokument7 SeitenRockland NBZ Ordinancegerald7783Noch keine Bewertungen
- Birth Tourist Email To Gov. LePageDokument1 SeiteBirth Tourist Email To Gov. LePagegerald7783Noch keine Bewertungen
- Rockland Meeting Schedule For Week Ending 11.6.15 PublicDokument1 SeiteRockland Meeting Schedule For Week Ending 11.6.15 Publicgerald7783Noch keine Bewertungen
- LePage Letter To President Obama Re Proposed National ParkDokument4 SeitenLePage Letter To President Obama Re Proposed National Parkgerald7783Noch keine Bewertungen
- LePage Note To LouiseDokument1 SeiteLePage Note To Louisegerald7783Noch keine Bewertungen
- Sens. Alfond/Hill Letter To Senate President Thibodeau Re Sen WilletteDokument2 SeitenSens. Alfond/Hill Letter To Senate President Thibodeau Re Sen Willettegerald7783Noch keine Bewertungen
- New Trail MapDokument1 SeiteNew Trail Mapgerald7783Noch keine Bewertungen
- Veto Letters From Gov. Paul LePageDokument11 SeitenVeto Letters From Gov. Paul LePagegerald7783Noch keine Bewertungen
- 21 Vetoes by Gov. Paul LePage 19 June 2015Dokument21 Seiten21 Vetoes by Gov. Paul LePage 19 June 2015gerald7783Noch keine Bewertungen
- LePage Veto Letters For Bills Sponsored by DemocratsDokument12 SeitenLePage Veto Letters For Bills Sponsored by Democratsgerald7783Noch keine Bewertungen
- Al DiMillo Review of Gov LePage Tax SchemeDokument7 SeitenAl DiMillo Review of Gov LePage Tax Schemegerald7783100% (1)
- Bipartisan Letter To Verso Urging Prompt Payment of SeveranceDokument4 SeitenBipartisan Letter To Verso Urging Prompt Payment of SeverancejodiquinteroNoch keine Bewertungen
- Mayhew Response To FNS Photo EBTDokument5 SeitenMayhew Response To FNS Photo EBTgerald7783Noch keine Bewertungen
- Letter From Cathy Breen To Maine SenateDokument4 SeitenLetter From Cathy Breen To Maine Senategerald7783Noch keine Bewertungen
- Rockland Waterfront Redevelopment PlanDokument71 SeitenRockland Waterfront Redevelopment Plangerald7783Noch keine Bewertungen
- Christian Civic League of Maine Says Cain Holding An "Abortion Celebration"Dokument2 SeitenChristian Civic League of Maine Says Cain Holding An "Abortion Celebration"gerald7783Noch keine Bewertungen
- Dench Confirmation Testimony (Maine Womens' Lobby)Dokument2 SeitenDench Confirmation Testimony (Maine Womens' Lobby)Andi ParkinsonNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Telemedicine: International Group Institute For Information Industry Jan 2008Dokument30 SeitenTelemedicine: International Group Institute For Information Industry Jan 2008Ted Chao100% (7)
- Long Term Care Outpatient Rotation Suggested ActivitiesDokument10 SeitenLong Term Care Outpatient Rotation Suggested Activitiesapi-240994549Noch keine Bewertungen
- Monitoring Compliance to International Patient Safety Goals in Malaysian HospitalsDokument12 SeitenMonitoring Compliance to International Patient Safety Goals in Malaysian HospitalsHosam GomaaNoch keine Bewertungen
- Raabta PresentationDokument22 SeitenRaabta PresentationMadeeehaNoch keine Bewertungen
- Resume 2010-1-31Dokument3 SeitenResume 2010-1-31smlayoNoch keine Bewertungen
- ANSI Reason Codes Denial CodesDokument7 SeitenANSI Reason Codes Denial CodesShiva ReyesNoch keine Bewertungen
- OT Practice April 23 IssueDokument64 SeitenOT Practice April 23 IssueThe American Occupational Therapy Association100% (1)
- Investor - S Guide To The Care Economy - Four Dynamic Areas of Growth - July 2021Dokument266 SeitenInvestor - S Guide To The Care Economy - Four Dynamic Areas of Growth - July 2021simyanliangNoch keine Bewertungen
- Medicare Proof of RepresentationDokument2 SeitenMedicare Proof of RepresentationHenry TownsendNoch keine Bewertungen
- Seizure IhcpDokument2 SeitenSeizure Ihcpapi-454842648Noch keine Bewertungen
- WHO - NPSA Generic Checklist PDFDokument3 SeitenWHO - NPSA Generic Checklist PDFShashwat IVF & Women's HospitalNoch keine Bewertungen
- MobilDrTech Releases White Paper On "Telemedicine Stethoscopes"Dokument2 SeitenMobilDrTech Releases White Paper On "Telemedicine Stethoscopes"PR.comNoch keine Bewertungen
- Quality management in diagnostic imagingDokument22 SeitenQuality management in diagnostic imagingJOVEMEA LIRAYNoch keine Bewertungen
- Patient-And Family-Centered Care Organizational Self-Assessment ToolDokument3 SeitenPatient-And Family-Centered Care Organizational Self-Assessment ToolAndi AbelloNoch keine Bewertungen
- MS Childrens Behavioral Health 3-6-15 FinalDokument152 SeitenMS Childrens Behavioral Health 3-6-15 Finalthe kingfishNoch keine Bewertungen
- The Medicalization of Human Conditions and Health Care A Public Health PerspectiveDokument2 SeitenThe Medicalization of Human Conditions and Health Care A Public Health PerspectiveKrisna Meidiyantoro100% (1)
- Cataract in The Adult Eye PPP PDFDokument119 SeitenCataract in The Adult Eye PPP PDFharshus12Noch keine Bewertungen
- Leo Alexander Bio With PictureDokument2 SeitenLeo Alexander Bio With PictureSusie CambriaNoch keine Bewertungen
- School Health NursingDokument4 SeitenSchool Health NursingJanelle Gimenez100% (1)
- Strengthening Health Services in Surigao del NorteDokument23 SeitenStrengthening Health Services in Surigao del NorteMaria Socorro AlcantaraNoch keine Bewertungen
- Notice: Scientific Misconduct Findings Administrative Actions: Grol, Jessica LeeDokument2 SeitenNotice: Scientific Misconduct Findings Administrative Actions: Grol, Jessica LeeJustia.comNoch keine Bewertungen
- FirstAid 2017 PDFDokument412 SeitenFirstAid 2017 PDFSylvia Diamond86% (7)
- 10 Day Workout Plan 260cf416 73ce 41ff b8f5 6b38f89aebc9Dokument6 Seiten10 Day Workout Plan 260cf416 73ce 41ff b8f5 6b38f89aebc9alexlucu21Noch keine Bewertungen
- Home Based CareDokument13 SeitenHome Based CareTom BiusoNoch keine Bewertungen
- News WritingDokument2 SeitenNews Writingpheonixmtbt100% (3)
- FINAL YOU BrochureDokument16 SeitenFINAL YOU BrochureFN2187tNoch keine Bewertungen
- Jurnal 5Dokument7 SeitenJurnal 5miraNoch keine Bewertungen
- MGT 420 Week 5 Individual Assignment Quality Organizations FinalDokument5 SeitenMGT 420 Week 5 Individual Assignment Quality Organizations FinalAbeTieh_88309155Noch keine Bewertungen
- NIAC Hospital Network List PPN and NON PPNDokument3.464 SeitenNIAC Hospital Network List PPN and NON PPNluckynaveenrajNoch keine Bewertungen
- Warren Barr South LoopDokument7 SeitenWarren Barr South LoopBeth LawrenceNoch keine Bewertungen