Beruflich Dokumente
Kultur Dokumente
UMMC Argatroban Protocol Revised 4-2008
Hochgeladen von
damondouglas100%(1)100% fanden dieses Dokument nützlich (1 Abstimmung)
2K Ansichten2 SeitenArgatroban (argatroban) is a continuous intravenous infusion drug used to treat hepatic thrombocytopenia (hep thromboembolism). APTT should be 1. - 3 times baseline aPTT (usually between 46-90 seconds) Adjust rate of infusion based on nomogram: maximum infusion rate is 10 mcg / kg / min. Monitor CBC, Hgb / Hct, signs
Originalbeschreibung:
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
DOC, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenArgatroban (argatroban) is a continuous intravenous infusion drug used to treat hepatic thrombocytopenia (hep thromboembolism). APTT should be 1. - 3 times baseline aPTT (usually between 46-90 seconds) Adjust rate of infusion based on nomogram: maximum infusion rate is 10 mcg / kg / min. Monitor CBC, Hgb / Hct, signs
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als DOC, PDF, TXT herunterladen oder online auf Scribd lesen
100%(1)100% fanden dieses Dokument nützlich (1 Abstimmung)
2K Ansichten2 SeitenUMMC Argatroban Protocol Revised 4-2008
Hochgeladen von
damondouglasArgatroban (argatroban) is a continuous intravenous infusion drug used to treat hepatic thrombocytopenia (hep thromboembolism). APTT should be 1. - 3 times baseline aPTT (usually between 46-90 seconds) Adjust rate of infusion based on nomogram: maximum infusion rate is 10 mcg / kg / min. Monitor CBC, Hgb / Hct, signs
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als DOC, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 2
University of Maryland Medical Center
Argatroban (Argatroban®)
Continuous Intravenous Infusion Guidelines
INITIATING ARGATROBAN INFUSION
1. Obtain patient weight, round down to nearest kilogram (kg)
2. Discontinue all active orders for heparin or low molecular weight heparin, including
flushes or locks, and heparin in TPN
3. Discontinue all heparin coated catheters
4. Document heparin allergy (heparin induced thrombocytopenia) in chart
5. Draw baseline aPTT and PT/INR prior to infusion
6. Obtain baseline liver function tests
7. Begin argatroban infusion base on patient status:
a. For critically ill patients, patients with reduced cardiac output, OR patients
with hepatic insufficiency, OR pediatric patients:
Initiate argatroban infusion at 0.5 mcg/kg/min
b. For non-critically-ill patients with normal hepatic function:
Initiate argatroban infusion at 1 to 2 mcg/kg/min
8. STAT aPTT 2 hours after the start of argatroban infusion
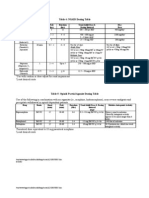
MONITORING AND ADJUSTING OF ARGATROBAN INFUSION
1. Adjust rate of argatroban infusion based on the following nomogram:
Note: Maximum infusion rate of argatroban is 10 mcg/kg/min
2. Goal aPTT is 1.5 – 3 times baseline aPTT (usually between 46-90 seconds)
3. Check aPTT two hours after any rate change
4. Adjust argatroban until aPTT is therapeutic and stable for 2 or more consecutive
measures, not exceeding aPTT greater than 100 seconds
5. Once aPTT stable, obtain aPTT daily
6. Monitor CBC, Hgb/Hct, signs/symptoms of bleeding daily
aPTT Critically Ill Patients OR
Hold Infusion Patients with Normal Hepatic
Reduced Cardiac Function OR
(sec) (min) Function
Pediatrics
<40 0 Increase by 0.25 mcg/kg/min Increase by 1 mcg/kg/min
40 – 45 0 Increase by 0.1 mcg/kg/min Increase by 0.5 mcg/kg/min
46 – 90 0 No Change No Change
91 – 100 30 Decrease by 0.25 mcg/kg/min Decrease by 0.25 mcg/kg/min
> 100 Stop infusion Notify physician
Last updated: 3/27/2008
Updated By: J. Gonzales, PharmD
Reviewed By: M. Zimrin, MD
CONVERSION TO ORAL ANTICOAGULATION FOR PATIENTS WITH HIT
1. Initiate warfarin ONLY after substantial platelet recovery, preferentially to normal
(platelet >100-150 K/mm3).
2. Initiate warfarin dose at the expected maintenance dose. Loading dose should NOT be
used. Avoid initial warfarin dose greater than 5 mg.
3. Overlap warfarin with argatroban for minimum of 5 days, and until INR is greater than 4.
(INR goal = 4-6)
NOTE: argatroban can significantly increase the INR
4. At the end of overlap, if argatroban rate is less than 2 mcg/kg/min, stop infusion:
a. Obtain INR 4 to 6 hours after discontinuation of argatroban infusion
b. If INR is 2 to 3, continue with warfarin monotherapy
c. If INR is less than 2 (sub-therapeutic), resume argatroban at previous rate and
repeat procedure the following day
5. At the end of the overlap, if argatroban rate is greater than 2 mcg/kg/min
a. Reduce infusion to 2 mcg/kg/min
b. Obtain INR 4 to 6 hours after the dose reduction
c. If INR is greater than 4, stop infusion and follow steps outlined in #4
d. If INR is less than 4, continue infusion and recheck INR the following day
6. Monitor for new thrombosis and limb ischemia while on warfarin therapy
References
1. Selleng K, Warkentin TE, Greinacher A. Heparin-induced thrombocytopenia in intensive care
patients. Crit Care Med. 2007;35:1165-1176.
2. Levine RL, Hursting MJ, McCollum D. Argatroban therapy in heparin-induced thrombocytopenia with
hepatic dysfunction. Chest. 2006;129:1167-1175.
3. Argatroban package insert. GlaxoSmithKline. 2005.
Last updated: 3/27/2008
Updated By: J. Gonzales, PharmD
Reviewed By: M. Zimrin, MD
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- A Dictionary For Psychotherapists PDFDokument1.375 SeitenA Dictionary For Psychotherapists PDFMonica100% (2)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Sleep Related Problems (GROUP 2)Dokument3 SeitenSleep Related Problems (GROUP 2)april hortilanoNoch keine Bewertungen
- Home Care RN Skills ChecklistDokument2 SeitenHome Care RN Skills ChecklistGloryJaneNoch keine Bewertungen
- A Primer For PsychotherapistsDokument136 SeitenA Primer For PsychotherapistsrichuNoch keine Bewertungen
- Cognitive MedsDokument2 SeitenCognitive MedsRNStudent1100% (1)
- Hand AssessmentDokument22 SeitenHand AssessmentVaikunthan RajaratnamNoch keine Bewertungen
- OsteosarcomaDokument25 SeitenOsteosarcomaChaitra Mahesh67% (3)
- Xinnong Cheng - Chinese Acupuncture and Moxibustion 1Dokument282 SeitenXinnong Cheng - Chinese Acupuncture and Moxibustion 1Abrar Abizar100% (1)
- Antimicrobial Renal DosingDokument5 SeitenAntimicrobial Renal DosingdamondouglasNoch keine Bewertungen
- Pain Management NCLEXDokument5 SeitenPain Management NCLEXPotchiee PfizerNoch keine Bewertungen
- BARC TrainingDokument6 SeitenBARC Trainingashfaqk100% (1)
- PIs Drug InteractionDokument1 SeitePIs Drug InteractiondamondouglasNoch keine Bewertungen
- CAP AlgorithmDokument1 SeiteCAP AlgorithmdamondouglasNoch keine Bewertungen
- NRTI NNRTI Drug Interact TBLDokument1 SeiteNRTI NNRTI Drug Interact TBLdamondouglasNoch keine Bewertungen
- IV PO Conversion P&P.V2Dokument3 SeitenIV PO Conversion P&P.V2damondouglasNoch keine Bewertungen
- CAP Order Form Admission Final VerDokument1 SeiteCAP Order Form Admission Final VerdamondouglasNoch keine Bewertungen
- University of Maryland Medical Center Fluconazole (Diflucan®)Dokument6 SeitenUniversity of Maryland Medical Center Fluconazole (Diflucan®)damondouglasNoch keine Bewertungen
- IV PO Conversion CAPDokument3 SeitenIV PO Conversion CAPdamondouglasNoch keine Bewertungen
- In B Deoxycholate Shortage Alternative TherapiesDokument2 SeitenIn B Deoxycholate Shortage Alternative TherapiesdamondouglasNoch keine Bewertungen
- 3.E.2-Caspofungin Guideline 2003Dokument3 Seiten3.E.2-Caspofungin Guideline 2003damondouglasNoch keine Bewertungen
- Restricted AntimicrobialsDokument1 SeiteRestricted AntimicrobialsdamondouglasNoch keine Bewertungen
- CAP Guidelines For UseDokument11 SeitenCAP Guidelines For Usedamondouglas100% (1)
- Sodium Content of Inject Able AntibioticsDokument1 SeiteSodium Content of Inject Able AntibioticsdamondouglasNoch keine Bewertungen
- Antibiogram 07Dokument1 SeiteAntibiogram 07damondouglas100% (1)
- Pediatric Antimicrobial DosingDokument3 SeitenPediatric Antimicrobial Dosingdamondouglas100% (2)
- NSAID Agonist Antagonist TableDokument1 SeiteNSAID Agonist Antagonist TabledamondouglasNoch keine Bewertungen
- PONV GuidelinesDokument3 SeitenPONV GuidelinesdamondouglasNoch keine Bewertungen
- Sedation Pain AlgorithmDokument1 SeiteSedation Pain Algorithmdamondouglas100% (2)
- Perioperative Antibiotics For Surgical ProphylaxisDokument1 SeitePerioperative Antibiotics For Surgical ProphylaxisdamondouglasNoch keine Bewertungen
- Pain Guidelines & Range DosingDokument3 SeitenPain Guidelines & Range Dosingdamondouglas100% (1)
- IV Insulin - FinalDokument18 SeitenIV Insulin - Finaldamondouglas100% (2)
- Opioid Equianalgesic ChartDokument1 SeiteOpioid Equianalgesic Chartdamondouglas100% (7)
- ICU Neuromuscular BlockadeDokument7 SeitenICU Neuromuscular BlockadedamondouglasNoch keine Bewertungen
- IV PO Conversion CAPDokument3 SeitenIV PO Conversion CAPdamondouglasNoch keine Bewertungen
- Hypertensive Urgency EmergencyDokument5 SeitenHypertensive Urgency Emergencydamondouglas100% (3)
- IV PO ConversionsDokument1 SeiteIV PO Conversionsdamondouglas100% (1)
- Hyperglycemia Algorithm 2Dokument1 SeiteHyperglycemia Algorithm 2damondouglasNoch keine Bewertungen
- Guideline For The Prevention of CINDokument2 SeitenGuideline For The Prevention of CINdamondouglasNoch keine Bewertungen
- HIT ProtocolDokument1 SeiteHIT ProtocoldamondouglasNoch keine Bewertungen
- The ARCPP 15th Annual Conference InvitationDokument4 SeitenThe ARCPP 15th Annual Conference InvitationLJ DusabanNoch keine Bewertungen
- Jurnal Ebm PDFDokument10 SeitenJurnal Ebm PDFagustin488Noch keine Bewertungen
- Effectiveness of A Desensitizing Agent Before In-Office Tooth Bleaching in Restored TeethDokument7 SeitenEffectiveness of A Desensitizing Agent Before In-Office Tooth Bleaching in Restored TeethFer TorresNoch keine Bewertungen
- In Vitro in Vivo Correlation Ivivc A Strategic Tool in Drug Development Jbb.S3 001Dokument12 SeitenIn Vitro in Vivo Correlation Ivivc A Strategic Tool in Drug Development Jbb.S3 001Jerome K GeorgeNoch keine Bewertungen
- Principles Involved in Bioassay by Different Methods A Minireview PDFDokument18 SeitenPrinciples Involved in Bioassay by Different Methods A Minireview PDFPankaj KushwahNoch keine Bewertungen
- Nlex 1Dokument4 SeitenNlex 1Aileen AlphaNoch keine Bewertungen
- Rotation Checklist - ClinicalDokument3 SeitenRotation Checklist - Clinicalapi-240994549100% (1)
- Crown LengtheningDokument4 SeitenCrown LengtheningArdelvie YoandaNoch keine Bewertungen
- NSAID Safety Audit Jan2019 Vs6Dokument10 SeitenNSAID Safety Audit Jan2019 Vs6Shokooh MansouriNoch keine Bewertungen
- Sevrage CannabisDokument29 SeitenSevrage CannabismihaelaNoch keine Bewertungen
- Intrathecal Injection (LP) ENGDokument1 SeiteIntrathecal Injection (LP) ENGAlina RadescuNoch keine Bewertungen
- June 2009Dokument37 SeitenJune 2009Onichan KhunNoch keine Bewertungen
- SchizophreniaDokument7 SeitenSchizophreniaMANOJ KUMARNoch keine Bewertungen
- Ca Semi FiDokument23 SeitenCa Semi FiJheanAlphonsineT.MeansNoch keine Bewertungen
- Acute and Chronic RhinitisDokument25 SeitenAcute and Chronic RhinitisagniajolandaNoch keine Bewertungen
- Inborn Errors or MetabolismDokument25 SeitenInborn Errors or MetabolismSamdiSutantoNoch keine Bewertungen
- Rubella: Congenital Clinically Significant Congenital MalformationsDokument8 SeitenRubella: Congenital Clinically Significant Congenital MalformationsAlexandraNoch keine Bewertungen
- Mindfulness Interventions For Nursing Students: Application of Modelling and Role Modelling TheoryDokument7 SeitenMindfulness Interventions For Nursing Students: Application of Modelling and Role Modelling Theoryagnesia yusupNoch keine Bewertungen
- Sialography ExaminationDokument14 SeitenSialography ExaminationEkaRahmaNoch keine Bewertungen
- Cerebral Palsy (CP) : Neurology Chapter of IAPDokument42 SeitenCerebral Palsy (CP) : Neurology Chapter of IAPWegrimel AriegaraNoch keine Bewertungen