Beruflich Dokumente
Kultur Dokumente
Managing Documentation Risk: A Guide For Nurse Managers
Hochgeladen von
Alai SjOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Managing Documentation Risk: A Guide For Nurse Managers
Hochgeladen von
Alai SjCopyright:
Verfügbare Formate
Managing
Documentation
Risk
A Guide for
Nurse
Managers
Patricia A. Duclos-Miller
MS, RN, CNA, BC
SECOND EDITION
Managing
Documentation
Risk
A Guide for
Nurse
Managers
Patricia A. Duclos-Miller
MS, RN, CNA, BC
SECOND EDI TI ON
Managing Documentation Risk: A Guide for Nurse Managers, Second Edition is published by HCPro, Inc.
Copyright 2007, 2004 HCPro, Inc.
All rights reserved. Printed in the United States of America. 5 4 3 2 1
First edition published 2004. Second edition 2007.
ISBN 978-1-60146-036-3
No part of this publication may be reproduced, in any form or by any means, without prior written consent
of HCPro, Inc., or the Copyright Clearance Center (978/750-8400). Please notify us immediately if you have
received an unauthorized copy.
HCPro, Inc., provides information resources for the healthcare industry.
HCPro, Inc., is not affiliated in any way with The Joint Commission, which owns the JCAHO and Joint
Commission trademarks.
Patricia A. Duclos-Miller, MS, RN, CNA, BC, Author Liza Banks, Proofreader
Rebecca Hendren, Senior Managing Editor Darren Kelly, Books Production Supervisor
Jamie Gisonde, Executive Editor Susan Darbyshire, Art Director
Emily Sheahan, Group Publisher Claire Cloutier, Production Manager
Janell Lukac, Layout Artist Jean St. Pierre, Director of Operations
Advice given is general. Readers should consult professional counsel for specific legal, ethical, or clinical
questions.
Arrangements can be made for quantity discounts. For more information, contact:
HCPro, Inc.
P.O. Box 1168
Marblehead, MA 01945
Telephone: 800/650-6787 or 781/639-1872
Fax: 781/639-2982
E-mail: customerservice@hcpro.com
Visit HCPro at its World Wide Web sites:
www.hcpro.com and www.hcmarketplace.com
5/2007
21196
iii
Managing Documentation Risk, Second Edition
Dedication
To my family, who have always supported my endeavors.
Acknowledgement
A sincere thank you to my editor who made this book a pleasure to revise. Her editorial skills
added tremendously to the value of the book.
oedication
CBA1lk ONl
Managing Documentation Risk, Second Edition
CON1lN1S
About the author ..........................................................................................................................................................................................viii
Introduction ........................................................................................................................................................................................................ ix
Key aspects of documentation ................................................................................................................................................... 1
What every nurse manager needs to know ................................................................................................................................... 1
Nurse manager responsibilities ................................................................................................................................................................ 2
Let the nursing process be your guide ............................................................................................................................................... 3
Nursing diagnosis and Nursing Outcome Classification ...................................................................................................... 7
Outcomes identification ............................................................................................................................................................................... 8
Planning ....................................................................................................................................................................................................................11
Implementation .................................................................................................................................................................................................12
Evaluation ................................................................................................................................................................................................................12
Organizational policies, protocols, and practices ....................................................................................................................15
Case Study: Good documentation reflects the nursing process ................................................................................16
Reducing risk and culpability through defensive documentation .............................................21
Your documentation: Truth or consequences? ........................................................................................................................21
The truth ..................................................................................................................................................................................................................21
Case Study: The truth comes out .......................................................................................................................................................23
Risk-management guidelines for documenting care ............................................................................................................23
The consequences ............................................................................................................................................................................................24
Case Study: Neglected documentation .........................................................................................................................................25
Case Study: Incomplete documentation ......................................................................................................................................26
Case Study: Improperly altered documentation ....................................................................................................................28
Case Study: Neglected documentation II .....................................................................................................................................29
Handling documentation errors ...........................................................................................................................................................30
Adverse events: When bad things happen to good nurses .............................................................................................31
Documentation of adverse events ......................................................................................................................................................33
Incident reports ..................................................................................................................................................................................................35
Tips for writing an incident report .....................................................................................................................................................36
Risk-reduction recommendations for nurse managers ......................................................................................................37
Contemporary nursing practice: Are you and your staff there? ....................................................41
Are you using contemporary nursing practice? ........................................................................................................................41
Certification ...........................................................................................................................................................................................................42
Professional standards ...................................................................................................................................................................................43
Code of ethics ......................................................................................................................................................................................................47
State Nurse Practice Act ..............................................................................................................................................................................48
Threats to licensure .........................................................................................................................................................................................50
CBA1lk
ONl
CBA1lk
1Bkll
CBA1lk
1wO
v
Managing Documentation Risk, Second Edition
Federal and state regulations ...................................................................................................................................................................51
The Joint Commission ...................................................................................................................................................................................54
Organizational policies and procedures..........................................................................................................................................54
Resources .................................................................................................................................................................................................................56
Functions of the medical record .............................................................................................................................................59
The effects of staff documentation on compliance, quality, and reimbursement........................................59
Medical record as communication .....................................................................................................................................................59
Medical record as a demonstration of compliance ...............................................................................................................61
The Joint Commission and tracer methodology .................................................................................................................64
Quality and risk-management review ..............................................................................................................................................68
Medical record as a path to reimbursement ..............................................................................................................................69
Resources .................................................................................................................................................................................................................75
Nursing negligence: Understanding your risks and culpability ....................................................77
Legal issues ..............................................................................................................................................................................................................77
Essential definitions .........................................................................................................................................................................................77
Factors that contribute to malpractice cases against nurses .........................................................................................79
Legal risks for nurse managers ................................................................................................................................................................81
Case Study: Incompetent care ..............................................................................................................................................................85
Legal risks for nurses .......................................................................................................................................................................................86
Case Study: Chart review reveals fraudulent countersignature .................................................................................87
Professional-negligence claims against nurses ...........................................................................................................................87
Case Study: Failure to follow protocol............................................................................................................................................88
Case Study: Breach in nursing standard of practice.............................................................................................................89
Case Study: Failure to properly orient, educate, and evaluate ....................................................................................90
National Practitioner Data Bank ...........................................................................................................................................................90
Liability in special practice settings.....................................................................................................................................................92
Depositions: Preparing for the worst ...............................................................................................................................95
When it happens to you ..............................................................................................................................................................................95
Essential definitions .........................................................................................................................................................................................95
Meeting with your organizations attorney/risk manager ................................................................................................96
Reviewing medical records and all associated policies ........................................................................................................97
The importance of a deposition ............................................................................................................................................................99
The players .......................................................................................................................................................................................................... 100
Prepare, prepare, prepare ........................................................................................................................................................................ 102
At the deposition ........................................................................................................................................................................................... 103
Tips for presenting an effective deposition testimony..................................................................................................... 104
Improving staff documentation ........................................................................................................................................... 111
Recognizing and correcting charting mistakes that increase your liability risks ......................................... 111
Eight common charting errors ............................................................................................................................................................ 112
Case Study: Failure to record medication given .................................................................................................................. 113
CBA1lk
IOUk
CBA1lk
SIX
CBA1lk
IIVl
CBA1lk
SlVlN
Contents
vi
Managing Documentation Risk, Second Edition
Other common charting flaws ............................................................................................................................................................ 117
The consequences of an incomplete medical record ........................................................................................................ 118
Tips to improve your staffs documentation ........................................................................................................................... 119
Developing a foolproof documentation system................................................................................................ 125
Building on the foundation of compliance standards ...................................................................................................... 125
Evaluating your current documentation system .................................................................................................................. 125
Systems of documentation .................................................................................................................................................................... 127
Using The Joint Commission standards as the foundation of your system .................................................... 137
10 steps for building a foolproof documentation system ............................................................................................. 142
Auditing your documentation system ........................................................................................................................ 147
The important role audits play in protecting you and your organization ....................................................... 147
Building your audit system around performance-improvement goals ............................................................... 147
Measuring compliance and improvement through an audit ..................................................................................... 149
Getting your staff to use the audit tool ....................................................................................................................................... 150
Advantages of audits for the nurse manager ........................................................................................................................... 151
Nurse manager tips for auditing ........................................................................................................................................................ 151
Electronic health records ............................................................................................................................................................. 153
Nurse managers roles in building a computerized system that reduces liability....................................... 153
Why we need electronic health records ...................................................................................................................................... 154
Start at the beginning ................................................................................................................................................................................. 154
Benefits of electronic documentation ........................................................................................................................................... 155
The nurse managers role ......................................................................................................................................................................... 156
Challenges associated with the change ........................................................................................................................................ 157
Computer etiquette ..................................................................................................................................................................................... 159
Strategies for success ................................................................................................................................................................................... 161
Motivating your nurses to document completely and accurately ........................................... 165
Why nurses document poorly ............................................................................................................................................................. 165
Change: Embrace it or resist it ............................................................................................................................................................. 167
The role of education and expectations ...................................................................................................................................... 169
The good, the bad, and the ugly approach ............................................................................................................................... 170
Monitoring the work environment ................................................................................................................................................. 171
Staff-motivation tips for nurse managers ................................................................................................................................... 173
Sample audit tools ................................................................................................................................................................................ 175
Nursing education instructional guide ...................................................................................................................... 179
Continuing education exam .................................................................................................................................................................. 183
Continuing education evaluation ..................................................................................................................................................... 192
CBA1lk
lIGB1
CBA1lk
NINl
CBA1lk
1lN
CBA1lk
lllVlN
AlNoIX
Contents
Managing Documentation Risk, Second Edition
Figure 1.1 Respiratory Status: Airway patency (0410) .....................................................................................10
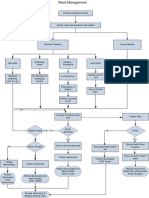
Figure 1.2 Nursing process flowchart ........................................................................................................................14
Figure 2.1 Quiz: Do I need to report this? ..............................................................................................................32
Figure 3.1 Contemporary nursing practice self-assessment .........................................................................42
Figure 3.2 ANA Standards of Nursing Practice....................................................................................................45
Figure 3.3 ANA Standards of Practice for Nurse Administrators .............................................................46
Figure 4.1 The Joint Commission hospital measure set .................................................................................66
Figure 4.2 Compliance chart review table ..............................................................................................................68
Figure 4.3 CMS Quality Measures ...............................................................................................................................72
Figure 5.1 Nurse manager risk-management checklist for adverse events ..........................................84
Figure 5.2 National Practitioner Data Bank (NPDB) Summary Report .................................................91
Figure 5.3 HIPDB reports on organizations ...........................................................................................................92
Figure 7.1 Illegible-clinical-documentation policy .......................................................................................... 116
Figure 7.2 Illegible-documentation reporting form ....................................................................................... 117
Figure 8.1 POMR example ............................................................................................................................................ 128
Figure 8.2 Example of nursing progress notes using PIE ............................................................................. 129
Figure 8.3 Example of focus charting ..................................................................................................................... 130
Figure 8.4 Example of CBE assessment standards ........................................................................................... 131
Figure 8.5 Example of outcome criteria................................................................................................................ 134
Figure 8.6 Audit tool to evaluate nursing process .......................................................................................... 136
Figure 8.7 Comparison of charting systems ....................................................................................................... 137
Figure 8.8 Nursing departmentMedical record audit (based on The Joint Commission standards) ........ 138
Figure 9.1 Steps in the quality improvement process .................................................................................. 148
Figure 11.1 Transforming a gripe into a goal in five minutes ..................................................................... 172
Appendix I Sample post-fall audit .............................................................................................................................. 175
Appendix II Sample ED documentation audit tool ........................................................................................... 176
Appendix III Sample pain assessment audit tool .................................................................................................. 177
IIGUklS
AOU1 1Bl
AU1BOk
Managing Documentation Risk, Second Edition
Patricia A. Duclos-Miller, MS, RN, CNA, BC
Patricia A. Duclos-Miller, MS, RN, CNA, BC is cur-
rently a full-time associate professor in nursing at Capital
Community College in Hartford, CT. In addition to
this position, she is a senior consultant for the Kelsco
Consulting Group in Cheshire, CT, a special lecturer for
the University of Connecticuts management in nursing
graduate program, and a per diem supervisor at Bristol
Hospital, CT.
Duclos-Miller is a registered nurse, board certified by the American Nurses
Credentialing Center (ANCC) in nursing administration. During her 33 years in
nursing, she has been a director for quality improvement, director of nursing in
acute, home health, and long-term care settings, and a staff nurse in the special-
ties of medical-surgical, mother-baby, and neonatal intensive care nursing. She is
a recognized speaker on contemporary nursing topics, including quality improve-
ment, team building, and documentation issues.
Duclos-Miller has served in key leadership positions for professional nursing
organizations and is a contributor to the newsletter Strategies for Nurse Managers,
published by HCPro, Inc. She is the author of Stressed Out About Your First Year
of Nursing, the first and second editions of Managing Documentation Risk: A Guide
for Nurse Managers, and the first and second editions of the handbook Nursing
Documentation: Reduce Your Risk of Liability, all published by HCPro, Inc.
AOU1 1Bl
AU1BOk
Managing Documentation Risk, Second Edition
IN1kOoUC1ION
Healthcare professionals acknowledge that documentation is an essential com-
ponent of good patient care. This assumption dates back to the time of Florence
Nightingale, who viewed documentation as a vital part of professional practice.
However, when push comes to shove during a busy day, documentation often
becomes the least-valued aspect of care.
Every professional must reexamine his or her commitment to safe patient care and
place documentation at the top of the priority list. When patient care is reviewed,
a complete and accurate clinical record must reflect that quality care was, in
fact, delivered. This record is reviewed by payers, external and internal quality-
improvement monitors, regulatory and accrediting agencies, and, in matters of
alleged negligence, patients themselves and their attorneys. In todays fast-paced
world with its shrinking nursing staff, a documentation system needs to be effi-
cient, timely, and complete.
Documentation can be a friend if the medical record clearly outlines the details of
care, but it becomes a foe if there are gaps. When reviewed, the medical record
must demonstrate that the patient received the best, most appropriate care pos-
sible. If the medical record does not reflect what happened, the door is open for a
claim of poor quality or questions about whether the appropriate care was admin-
istered. This possibility leads us to the old adage, If it wasnt documented, it
didnt happen. As much as we might cringe at the saying, whatever is written in
the medical recordnot what you claimwill be considered the truth.
Documentation is especially important for directors, nurse managers, and nursing
supervisors, because nursing management staff bear the burden of endorsing the
facilitys policies and protocols and ensuring that the care rendered is up-to-date,
timely, complete, and meets the standards of practice. You must protect yourself,
your staff, and your organization against claims of poor quality care. It is critical
that you recognize that documentation is an important part of everyday work for
x
Managing Documentation Risk, Second Edition
physicians, nurses, and other healthcare providers. If you do not see the value of
what is needed in the medical record, your efforts to improve documentation will
be not be successful.
As part of nursing management, your endorsement needs to be visible, in the
form of ongoing collaborative case reviews, continuing education concerning docu-
mentation, and development and design of a user-friendly documentation system.
Once the documentation system and tools are in place, you will have to design
an ongoing audit system to evaluate and measure compliance. To protect yourself
and your staff from liability, you must also be knowledgeable in the legal aspects
of nursing.
This book is a critical tool for anyone in nursing management who would like
to improve the quality of patient care, decrease their culpability in any potential
legal cases, and assist in decreasing the likelihood that their subordinates will be
cited in a medical or nursing malpractice case. The following chapters will provide
you with an understanding of why documentation is crucial, how to improve doc-
umentation, what makes a case vulnerable to legal recourse, and how to motivate
your staff to a level of excellence that is reflected in the medical record.
Remember, the medical record is a reflection of the care administered. It is read
by all those with rights to view it, and it will always stand on its own merits. You
and your staff need the nursing documentation to speak for itself.
Introduction
Managing Documentation Risk, Second Edition
CBA1lk
ONl
Key aspects of
documentation
What every nurse manager needs to know
As a member of a nursing management team, you must
assume responsibility for ensuring complete and accurate
documentation. In todays culture of accountability, your
title and scope of responsibilities will bring under scrutiny
your commitment to safe and quality patient care, so you
need to accept the responsibility whether it is part of your
job description or not. You must recognize the importance
of good clinical documentation. It is also vital that you
assist staff in practicing defensive documentation and
in avoiding the potential for legal consequences if a case is reviewed for alleged
medical malpractice.
The medical record must be accurate and complete because the information it
contains is critical for a number of people and functions. It is used to communi-
cate patients programs to other staff and the various clinical and ancillary depart-
ments involved in their care. It is used by the systems quality and risk-manage-
ment department and the utilization-management committee. In some cases, the
accuracy and completeness of the clinical record is essential to healthcare
researchers. It is also referred to when professional care rendered was considered
negligent. In addition, its content is regulated by the state in which you practice,
audited by insurers (both private and public), and reviewed for compliance with
accreditation standards.
Documenting completely and accurately is considered a professional standard of
nursing practice. For every step in the nursing process, the care delivered must
be documented. The nurse manager must assist nurses in fulfilling the necessary
requirements of good clinical care and documentation. Doing so not only validates
the universally recognized professional approach to patient care, it supplies other
care providers with consistent, clear communication and validates critical deci-
sion-making that is often necessary for quality patient care.
Learning objectives
After reading this chapter,
the participant will be able to:
Discuss how the nursing
process is used in nursing
documentation
Describe how to use Nursing
Outcomes Classification
(NOC) in nursing documen-
tation
CBA1lk ONl 2
Managing Documentation Risk, Second Edition
There are many research studies that have attempted to identify why nurses
do not value the importance of their documentation. One study by Moody and
Snyder claims an estimated 15-20% of the nursing work time is spent in documen-
tation. In addition, documentation has changed over the last few decades in both
its appearance and the advent of new technology. What is still missing with these
changes is the failure to demonstrate patient continuity of care and the evaluation
of patient outcomes (Irving 2006).
The quality of the care provided to patients can only be measured by the quality
of the nursing documentation. The major reasons for documenting nursing care
include:
Documentation of the plan of nursing care
Evaluation of the effectiveness of the nursing care provided
Facilitation of communication between the patient/family and other providers
Failure to completely document can have legal consequences. If documentation
is incomplete, contains gaps, or is not consistently completed according to the
organizations policies, it can be used to support an allegation that negligent care
was provided.
Incomplete documentation allows for juries to conclude that the nurse did not:
Collect sufficient data and plan appropriate care
Implement appropriate interventions, according to professional
and institutional standards
Make good clinical decisions
Communicate effectively
Nurse manager responsibilities
As a nurse manager, it is your responsibility to assist staff in adhering to both
clinical and documentation standards. It is also your responsibility to provide
continuing education, professional feedback, and input into policy and documen-
tation-system changes whenever possible. It is to your advantage to fulfill these
responsibilities because if your staff is involved in a medical malpractice case,
your ability to manage and meet quality and risk-management standards will be
called into question.
1 key aspects ot documentation
Managing Documentation Risk, Second Edition
As a member of the nursing-management team, you must not only demonstrate
a commitment to providing safe and efficient patient care, but also ensure that
every clinical record reflects that commitment. That is, although you must ensure
that nursing staff comply with up-to-date standards, it is equally important to
ensure that they document that compliance accurately and completely.
Your role is to support an efficient and effective documentation system and to cre-
ate an expectation that the system be followed.
Nursing management can demonstrate support for such a system by:
Developing an efficient system that meets the requirements of regulatory
standards.
Involving the end users in the development of the system.
Emphasizing the importance of documentation through written guidelines,
policies, job descriptions, and performance appraisals. The language should
include stipulations for daily supervisory oversight, audits of the system,
and feedback to the staff.
Let the nursing process be your guide
The nursing process, as outlined by the American Nurses Association (ANA)
Nursing Scope and Standards of Practice, provides us with an established, scien-
tific approach to providing nursing care. Not only does each step guide us in our
approach, it tells us how to validate what we saw, heard, felt, smelled, said, and
did while providing that care. The process accounts for all significant data and
actions taken by a registered nurse, the documentation of which is used for criti-
cal decision-making. Therefore, your documentation of patient care should follow
the framework of the nursing process.
Assessment
The first step of the nursing process is assessment. In this step, the nurse col-
lects information about the patients condition, which could include the patients
history, the physical exam, laboratory data, and so on. So as not to become over-
whelmed, the nurse must decide which information is most useful to the care of
the patient. For example, a nurse could limit the assessment data to the admission
signs and symptoms, the chief complaint, or medical diagnosis. This first step in
CBA1lk ONl 4
Managing Documentation Risk, Second Edition
the nursing processassessmentshould always be evident in the medical record
as it provides a complete clinical picture of the patient.
An assessment should include both subjective and objective data. When docu-
menting this data, beware of inappropriate documentation practices and focus on
risk management.
Subjective data
In this context, subjective data are data that can be observed, but not measured.
Statements made by the patient or family/significant other are examples of sub-
jective data. Although every conversation may not be relevant to the interaction,
there will be times when a patients words need to be recorded to establish a clear
picture of how the patient perceives his or her status.
For instance, if the patient says something that can be used to demonstrate men-
tal, behavioral, or cognitive status at the time of the assessment, documentation
of the conversation can be used to measure progress or decline over the course of
treatment. If patients are unable to speak or are cognitively impaired, nonverbal
cues are essential in determining whether there has been any change in status.
These conversations with the patient/family will need to be captured in the clini-
cal record in order to provide other clinicians with an accurate depiction of the
patients current status.
Objective data
Nurses establish patients clinical status based on objective data, which are observ-
able and measurable. Physical exam of patients, which include key assessment
techniques such as inspection, palpation, percussion, and auscultation, provide
objective data about patients health status. In simpler terms, nurses objective
assessment is based on what is seen, heard, felt and smelt. Healthcare providers
find this much easier to validate and include in their documentation than subjec-
tive data. Objective data also includes the results of diagnostic tests.
When recording this data, however, there are risks your staff should consider. If the
objective data is not reviewed in a timely manner, a reviewer of the clinical record
may point out that you failed to interpret the data and address significant changes
of condition. There also may be situations in which critical objective data were
present but there was no subsequent documentation of an appropriate intervention.
s key aspects ot documentation
Managing Documentation Risk, Second Edition
1. The entry:
Neuro signs WNL
The problem:
Which aspects of the neurological assessment are within normal limits (WNL)? Does
WNL refer to cognitive, visual, musculoskeletal, cranial nerve, Coma Scale, or
something else? Lack of documentation of a complete neurological assessment can
lead to an accusation of failure to document assessments according to contemporary
nursing standards.
The solution:
Develop a neurological assessment tool that is based on current standards and ensure
that staff complete the tool according to the policy and documentation guidelines.
In addition, if the absence of critical objective data resulted in a gap in the clinical
picture of the patient, it may contribute to a lack of appropriate intervention identi-
fication. All of these situations can lead to quality and risk-management issues.
Unacceptable assessment documentation
When documenting subjective or objective data, be careful to do so thoroughly
and appropriately. The following examples of entries into the medical record illus-
trate several common mistakes:
CBA1lk ONl
Managing Documentation Risk, Second Edition
3. The entry:
[Incomplete I&O sheet]
The problem:
Incomplete intake and outtake (I&O) sheets. Incomplete I&O sheets can lead to allega-
tions of improper assessment and insufficient data gathering. It could then be argued
that these omissions led to a lack of decision-making, which resulted in the patient
being harmed.
The solution:
Ensure that all I&O sheets are completed in their entirety. Check for accurate dates,
times, and quantities measured for both intake and output.
2. The entry:
Grand mal seizure
The problem:
This is not a complete assessment. It is the nurses responsibility to give a complete
clinical description of the incident so that any reader can visualize what happened.
The solution:
Ensure that your documentation of this episode has a beginning, middle, and end.
Start by documenting the patients status prior to the incident, if known. Describe
any report of an aura, color, posturing, or physical change during the seizure. Record
the length of time of the seizure and the condition of the patient immediately follow-
ing it, including both subjective data (what did the patient tell you about the inci-
dent?) and objective data (what were his or her vital and neurological signs?) assessed
by the nurse.
Here is an example of how the nurse should have documented:
Mrs. S. was ambulating to the BR with PCT. Pt. stated she felt funny. Pt. slowly slid
to floor with assistance. Pt. noted to turn pale white, facial grimace was fixed during
incident, contraction of large muscle of all extremities. Episode lasted 3060 seconds.
No observation of respiratory or cardiac distress. VSS after episode (taken within 1
minute), see flowsheet. Incontinent of large amount of urine (500 cc). Speech slurred,
disoriented, and complained of tiredness for first 30 minutes following episode. No
other neurological signs affected, see Neuro flowsheet. No laceration of tongue. First
observed episode.
1 key aspects ot documentation
Managing Documentation Risk, Second Edition
Gaps in documentation on any clinical assessment tool leave the provider and
the facility open to allegations that they failed to document assessments or failed
to address significant changes of condition. In the case of an incomplete I&O, it
could be alleged that the lack of analysis, intervention, and accurate documenta-
tion was the cause of circulatory collapse, dehydration, renal failure, infections,
skin breakdown, or even death.
For the nurse to arrive at a nursing diagnosis and the development of a nursing
plan of care, the assessment findings are crucial. Be sure you develop an assess-
ment tool that assists in recording a nursing examination thoroughly, accurately,
and clearly.
Here are some risk management tips for documenting assessment findings:
Describe everything exactly as found by inspection, palpation, percussion,
or auscultation
Do not allow the use of general terms such as normal, abnormal,
good, or poor
Be specific, and include both negative and positive aspects
Ensure that your policy on assessment includes the timeframe for assess-
ment completion and documentation
Encourage the staff to document their assessment as soon as possible after
completing it
Nursing diagnosis and Nursing Outcome Classification
If nurses accurately perform the assessment process, they will be able to appropri-
ately establish nursing diagnoses. This phase of the nursing process demonstrates
that the nurse reviewed the appropriate data available at the time and made a
professional determination of the clinical problem(s) at that time. Once the nurse
makes a clinical nursing diagnosis based on a thorough assessment, the rest of the
process falls into place.
The nursing diagnosis is defined by the North American Nursing Diagnosis
Association International (NANDA International) as a clinical judgment about the
individual, family, or community responses to actual or potential health problems
or life processes.
CBA1lk ONl 8
Managing Documentation Risk, Second Edition
Therefore, the nursing diagnosis expresses the nurses professional judgment of
the patients clinical status, the anticipated response to treatment, and the poten-
tial nursing-care needs. It guides the nurse and subsequent providers in their
understanding of the patients problem(s) and the plan of care developed specifi-
cally for that problem(s).
If your organization chooses to include the nursing diagnosis in its documenta-
tion system, you should promote consistency and use of correct terminology by
adopting NANDA International terminology. The NANDA International diagnostic
headings, coupled with the patients clinical etiology, provide a clear picture of the
patients needs.
Below are some examples of nursing diagnoses.
Risk for falls: Defined by NANDA International as, increased susceptibil-
ity to falling that may cause physical harm
Related to neurological changes S/P seizure: The related factors are based
on the risk factors as perceived by the etiology as stated by the nurse, and
the patients problem
S/P grand mal seizure with neurological changes, unsteady gait
Medication for seizure control has side effects for affecting gait and bal-
ance: Based on assessment data used
History of fall within one hour of seizure, over age of 65, diminished men-
tal status: Risk factors considered by the nurse
After making the nursing diagnosis, the nurse must determine the proper outcome
for the patient.
Outcomes identification
The next step in the nursing process is to determine an expected outcome, or goal,
for the patient. The outcome must be derived from the nursing diagnosis and
documented as a measurable, realistic, and patient-focused goal. It must include
a target time or date as well as an objective measurable action that the patient is
expected to achieve.
9 key aspects ot documentation
Managing Documentation Risk, Second Edition
Whenever possible, include the patient/familys perspective
on the goal of treatment and the timeframe. The expected out-
comes also should reflect the continuum of care, from admis-
sion, addressing immediate and intermediate outcomes, for
planning for discharge and follow-up care.
History of nursing outcomes
The use of patient outcomes in documentation dates back to
the mid-1960s, when for the first time nursing outcomes were
used to evaluate the effectiveness of nursing care. The use of
patient outcomes to evaluate healthcare dates back to Florence
Nightingale, who recorded and analyzed healthcare conditions
and the subsequent outcomes of those conditions during the
Crimean War (Moorehead 2004).
Although nurses have documented outcomes of their nursing
interventions for decades, there was no common language or associated way
to measure the outcomes of these interventions in the past. Today, however, a
research team at the University of Iowa has given nursing a standardized terminol-
ogy for nursing-specific and nursing-sensitive outcomes. This comprehensive classi-
fication of nursing outcomes is called the Nursing Outcomes Classification (NOC).
The current 2004 NOC lists 330 outcomes for use in nursing documentation. Each
NOC nursing outcome has a predetermined definition, a measurement scale, and
associated interventions. Each describes a possible state, behavior, or perception
of the patient (this is different from nursing diagnosis, which describes a patients
problem, either actual or potential). Once the nursing diagnosis is made the nurse
seeks to resolve it through appropriate interventions (see example in Figure 1.1).
Tips for documenting
expected outcomes:
Start with a specific action
verb that focuses on the
patients behavior
Avoid verbs that describe
the nurses behavior
(e.g., allow, let, enable)
Specify to which person
the goals refer (e.g., family,
friends)
Target dates must be realistic
Allow for flexibility of the
date if the patient needs
more time
(Goldberg 1999)
CBA1lk ONl 10
Managing Documentation Risk, Second Edition
Domain-Physiologic Health (II)
Class-Cardiopulmonary (E)
Scale(s)-Severely compromised to Not compromised (a) and Severe to None (n)
Defnition: Open, clear tracheobronchial passages for air exchange
OUTCOME TARGET RATING: Maintain at________ Increase to _______
Indicators Severely
compromised
1
Substantially
compromised
2
Moderately
compromised
3
Mildly
compromised
4
Not
compromised
5
041009 Ease of breathing 1 2 3 4 5
041004 Respiratory
rate
1 2 3 4 5
041005 Respiratory
rhythm
1 2 3 4 5
041006 Moves sputum
out of airway
1 2 3 4 5
041010 Moves blockage
our of airway
1 2 3 4 5
Severe Substantial Moderate Mild None
041002 Anxiety
041011 Fear
041003 Choking
041007 Adventitious
breath sounds
2nd edition 2000; Revised 3rd edition
Reprinted from Iowa Outcomes Project: Nursing Outcomes Classifcation (NOC), 3rd edition, page 456. Copyright (2004) with permission from Elsevier.
Respiratory Status: Airway Potency (0410) Icuar +.+
More recently, The Joint Commission has required all hospitals and long-term
care organizations seeking accreditation to use systems that provide data about the
organizations performance related to patient outcomes (Moorehead 2004).
A good example of the integration and use of outcomes identification can be found
in home healthcare. The Centers for Medicare & Medicaid Services (CMS) require
11 key aspects ot documentation
Managing Documentation Risk, Second Edition
all Medicare-certified home-health organizations to use the Outcome Assessment
Information Set (OASIS) data set, which they have been doing since 1998. The
OASIS outcomes system contains core measures that have been identified as appli-
cable to all client groups. It also contains measures specific to client groups with
a particular diagnosis or problem, the outcomes of which are measured on scales
specific to them. Using the OASIS outcome system, nurses assess whether home-
health clients have improved, stabilized, or deteriorated (Sparks 2001).
Planning
The next step in the nursing process is to develop a plan of care for the patient
based on the nurses assessment/diagnosis. Documentation of this phase demon-
strates that the clinical status of the patient was recognized and that the nurse
then developed an appropriate plan of care. It shows that the nursing process was
in place and thereby decreases the risk of incomplete or incorrect care. Having a
written road map helps everyone involved provide safe and quality care.
When developing a plan of care use the following guidelines:
Review identified nursing diagnoses and rank them in order of priority
Use evidence-based nursing interventions
The documentation tool/system should include nursing diagnosis, expected
outcomes, nursing interventions, and evaluation of care
The plan of care should be used as a communication tool between all
healthcare team members and the patient (Sparks 2001)
This step of the nursing process can be documented in a variety of ways. You
can use a specially designed form, flowsheet, patient-care plan, nursing progress
notes, clinical pathway, or specific software module. But whatever format is used,
remember that the patient plan of care is a permanent part of the clinical record
and must be treated as such. It should never be erased or destroyed. Adjustments
to the plan of care should reflect a progression of care based on the patients
needs, using the organizations standards/protocols.
CBA1lk ONl 12
Managing Documentation Risk, Second Edition
Implementation
Based on the nursing plan of care and contemporary standards of nursing care, the
nurse then documents the care provided for the patient. This phase of the nursing
process includes working collaboratively with other members of the healthcare
team, the patient, and the patients family.
Implementation may require some of the following interventions:
Assessing and monitoring
Therapeutic interventions
Comfort measures
Assistance with activities of daily living
Supporting respiratory functions
Supporting elimination functions
Providing skin care
Managing the environment to promote a therapeutic milieu
Providing food and fluids
Giving emotional support
Teaching and/or counseling
Referral to other agencies or services (Sparks and Taylor 2001)
Documentation will need to include the specific nurses intervention and the
patients response to the intervention. It should reflect the coordination of care,
health teaching and promotion, and any consultation that was done on behalf of
the patient. Like the documentation of planning, the documentation of care pro-
vided can be assigned to a specific form or location in the clinical record.
Evaluation
In this step of the nursing process, the nurse reviews the progress made in achiev-
ing established outcomes. The documentation needed to validate this step includes
the nurses comments on whether his or her assessment, diagnosis, achievement
of outcomes, plan of care, and nursing interventions were successful. In addition,
when developing a documentation system or a continuing education program for
11 key aspects ot documentation
Managing Documentation Risk, Second Edition
staff nurses, ensure that each nurse assesses the effectiveness
of the nursing process.
In determining whether the patient received high-quality care the nurse must ask
the following:
Has the patients condition improved, deteriorated, or remained the same?
Were the nursing diagnoses accurate?
Have the patients needs been met?
Did the patient meet the outcome criteria documented in the plan of care?
Do I revise or discontinue the nursing interventions?
Why did the patient fail to meet the goal? (Sparks 2001)
If the nurse uses the evaluation phase properly, the documentation will reflect
high-quality nursing care.
The graphic in Figure 1.2 shows the flow of the process and identifies the tools
associated with each phase.
CBA1lk ONl 14
Managing Documentation Risk, Second Edition
ASSlSSMlN1
Definition: Subjective and objective data from
patients health history, physical examination,
medical record, diagnostic test results.
Tools: Physical-examination form
Consultation sheets
Nursing admission assessment
Graphic flow sheets
Flow sheet
Diagnostic test results forms
Computer software module
NUkSING oIAGNOSIS
Definition: Clinical nursing judgment based on
the assessment data.
Tools: Plan of care
Patient-care guidelines
Clinical pathways
Medication administration record
Progress notes
Problem list
Computer software module
OU1COMl IolN1IIICA1ION
Definition: Specific measurable outcome.
Tools: Nursing Outcome
Classification (NOC)
Plan of care
Clinical pathway
Computer software module
Federally mandated documentation
systems
lANNING
Definition: Establish care priorities, set measur-
able goals/outcomes with target dates, describe
interventions.
Tools: Plan of care
Patient care guidelines
Clinical pathway
Discharge plan/pummary
Computer software module
IMllMlN1A1ION
Definition: Actual nursing interventions
delivered.
Tools: Graphic flow sheets
Flow sheets
Progress notes
Computer software module
Nursing Interventions
Classification (NIC)
lVAlUA1ION
Definition: Reassess data, nursing diagnoses, and
interventions for achievement of stated outcome.
Tools: Flow sheets
Clinical pathway
Computer software module
Nursing process fowchart Icuar +.z
1s key aspects ot documentation
Managing Documentation Risk, Second Edition
Organizational policies, protocols, and practices
When nurse experts are asked to review a medical record in preparation for a
legal case, they rely heavily on the medical record to determine the following:
Did the healthcare provider meet the policies and protocols of the organiza-
tion at the time of the care?
More importantly, did the healthcare provider meet the standards of nurs-
ing practice at the time of the care?
It is therefore the responsibility of the nursing management team to ensure that
the nursing staff follows the established policies of the organization and that this
compliance is demonstrated in the documentation system for that organization.
Organizational policies, protocols, and practices will always be called into review
when there is an allegation of substandard patient care. Nursing practice will be
held to national and local professional nursing standards, which are available
through the American Nurses Association (ANA) and through specialty nursing
associations such as the Association of Womens Health, Obstetric & Neonatal
Nurses (AWHONN), Association of Perioperative Registered Nurses (AORN),
American Association of Critical-Care Nurses (ACCRN), and others. If you derive
your policies and procedures from these, your organization will be better able to
justify the care that was delivered met established professional standards.
CBA1lk ONl 1
Managing Documentation Risk, Second Edition
Cnsr Svunv
Good documentation ret|ects tbe nursing process
Scenario: A patient complains of chest pain. Te nurse takes the patient seriously, as the subjec-
tive complaint may indicate a myocardial infarction. He or she acts quickly, performing a focused
assessment and documenting the essential information. Here are the critical elements of good
documentation of a patient with chest pain.
Documentation of what the patient said: Subjective data
2/15/07 16:00
Patient stated, Nurse, I am having chest pain. See Pain Flow sheet for description, loca-
tion, intensity noted. Patient in bed, increasingly anxious, used calm reassuring behavior
with patient. Redirected her to focus on remaining calm for interventions to work. Patient
responded, and pulse and respirations decreased. See VS sheet.
Te patients exact description of the symptom was noted, the nurse used quotations
around the patients words, rather than recording his or her interpretation of them.
On the pain fow sheet, the nurse indicates pain was located in the substernal region, radiat-
ing to the left shoulder. Pain level 10 out of 10. Te nurse appropriately uses the pain scale to
measure the level of intensity.
Te nurse also notes on the pain fow sheet: No preceding activity or past history of this type
of pain. Steady pain: 2-3 minutes. No SOB.
Patient care fow sheet indicated that the initial pulse and respirations at the time of the
nurses initial assessment of pain were
2/15/07 16:00 P:120 R: 40 BP: 146/90
2/15/07 16:04 P:96 R: 28 BP: 124/85
Documentation of what was assessed: Objective data
In the cardiopulmonary section of the patient care fow sheet, the nurse writes
SR (sinus rhythm), monitor fuctuated from S-tach to SR. No JVD.
O2 sats on RA: 92%
O2 sats on 4 L via cannula: 98%
continued on next page
11 key aspects ot documentation
Managing Documentation Risk, Second Edition
Cnsr Svunv
Good documentation ret|ects tbe nursing process (cont.)
Te nurse documents the vital signs, noting sinus tachycardia, an increased respiratory rate, and
above-baseline blood pressure for this patient. In addition, the nurse records auscultation of
heart sounds (e.g., regular, irregular heart rate, murmur, gallops, rubs.)
Te nurse assesses lung sounds and the respiratory rate and pattern, and measures abnor-
mal O2 saturation via pulse oximetry. Te patients actions are already noted as increasing
anxiety. Tere is no clutching of the chest by the patient. Skin assessment also is conducted
and documented.
In the cognitive section of the patient care fow sheet, the notations indicated, No changes
in mental status, no decreased level of consciousness, disorientation, or confusion.
In the narrative notes, the nurse notes, Skin cool, clammy, no peripheral edema, ashen in
color. No cyanosis noted.
Documentation of what was done: Intervention
Te nurse continues to document his or her interventions and the patients responses.
Frequent monitoring:
Te VSs were noted every few minutes until the chest pain subsided. Te nurse contin-
ues hourly VSs, pain assessments, and signs and symptoms of the patient.
All treatment activities are documented, including cardiac enzymes, ABGs and EKG, SL
NTG, morphine sulfate, etc.
Fluid intake and output: Recorded every four hours.
Oxygen therapy:
Te nurse documents the patients initial pulse-oximetry reading, respiratory-assess-
ment fndings, and ABG results, when he or she is notifed.
Te pulse-oximetry assessments are documented every hour until within normal range,
and every four hours thereafter. Based on ABG results, O2 could be decreased.
O2 decreased to 2L
Continuous cardiac monitoring:
2/15/07 16:03 Patient placed on cardiac monitor. Patient informed as to the reason for con-
tinuous monitoring.
continued on next page
CBA1lk ONl 18
Managing Documentation Risk, Second Edition
Cnsr Svunv
Good documentation ret|ects tbe nursing process (cont.)
Te nurse notes the time the patient was frst placed on the cardiac monitor (in MCL1) and
the teaching about the reason for the monitor. He or she also records which lead is being
displayed on the strip and the fow sheet. Te patients rhythm strip is labeled with the
patients name and strip intervals. Subsequent rhythm strips are obtained according to MI
protocol (such as change in condition, ectopic beats noted, or arrhythmia). Each strip has a
notation as to the heart rate and rhythm, PR-interval, and QRS-complex duration. Te pa-
tient does have a ST-segment elevation, which is noted on the strip. 2/15/07 17:02 Dr. Smith
notifed of 2mm ST elevation. New orders received and transcribed. O2 increased to 4 L, 12
lead EKG done. Stat SL NTG, Chest pain unrelieved by NTG. Morphine 2 mg. IV PRN given.
Te nurse does document notifcation of the physician for a signifcant change from the
initial strip. He or she records the physicians response and his or her actions.
Drug and IV therapy:
Te Medication Administration Record notes the names, dosages, times, and routes of the
medications the nurse gives. Te nurse also documents the patients vital signs after each
dose of nitroglycerin and morphine. Te pain fow sheet indicates the patients response to
the NTG and morphine.
On the IV section of the patient-care fow sheet, the nurse documents his or her assess-
ment of the IV sitethe date and time the IV line is inserted, catheter gauge, and person
who does the insertion. Also notes the catheter size, dressing type, and condition. During
the remainder of the shift the nurse documents his or her assessments of the IV site and line
patency.
Activity:
2/15/07 17:30 Patient informed of activity limitations due to change in her cardiac status.
Patient stated, Dont worry, Ill call you before I do anything. Te nurse notes the patient is
on bed rest and his or her instructions regarding patient-activity limitations.
Communication:
Te nurse is good at documenting his or her communication with other healthcare team
members. It is found in his or her narrative notes, names, time of notifcation, etc.
continued on next page
19 key aspects ot documentation
Managing Documentation Risk, Second Edition
Cnsr Svunv
Good documentation ret|ects tbe nursing process (cont.)
Emotional support:
2/15/07 20:10 Patient increasing in anxiety, attempted to get the patient to talk about her
feelings. Ofered medication to assist in decreasing her anxiety. Patient agreed to medication.
Te nurse ofers and documents emotional support to help the patient cope with the physi-
cal and psychological impact of her condition.
Transfer to ICU:
Tis patient does not need to be transferred, but if she had, the nurse would have docu-
mented the aspects of the patients condition that warranted the transfer. Te report to the
ICU nurse would have been documented and, if applicable, a written record of the patients
belongings would have been included. Te nurse also would have recorded the name of the
person who accompanied the patient and which monitoring devices were in place during
the transport. Someone would have to document how well she tolerated the transfer.
Documentation of what was taught
Te teaching plan needs to be tailored to the patients condition and treatment. Documentation
of patient/family teaching needs to include what was taught, the method of teaching, the materi-
als used for teaching, how well the patient/family understood the teaching, etc.
In this case, nurses discuss the following with this patient:
Heart anatomy and physiology
Disease process
Diagnostic tests and the reason for them
Treatment options such as angioplasty, stents, or thrombolytics
Signs and symptoms of an MI
Signs and symptoms to report
Actions to take when chest pain returns
Medication management (i.e., prescribed drugs and their names, dosages,
times to take them, route, any potential side efects, and how to store the medications)
Smoking cessation advice
Diet management
Activity and rest patterns
Community support groups, cardiac rehab centers (Sparks 2001)
CBA1lk ONl 20
Managing Documentation Risk, Second Edition
krrrarucrs
Goldberg, K. 1999. Surefre Documentation: How, What, and When Nurses Need to Document Philadel-
phia: Mosby, Inc.
Mosby. Mosbys Surefre Documentation: How, What, and When Nurses Need to Document, 2nd edition.
Philadelphia: Mosby, Inc.
Irving, K. et al. 2006. Discursive practices in the documentation of patient assessments. Journal of Ad-
vanced Nursing 53(2): 151-159.
Moorhead, S. et al. 2004. Iowa Outcomes Project Nursing Outcomes Classifcation (NOC), 3rd edition, St.
Louis: Mosby.
Sparks, S. and C. Taylor. 2001. Nursing Diagnosis Reference Manual, 5th edition. Springhouse, PA: Spring-
house Corp.
Das könnte Ihnen auch gefallen
- PDFDokument9 SeitenPDFNikki802Noch keine Bewertungen
- Talking Therapy: Knowledge and Power in American Psychiatric NursingVon EverandTalking Therapy: Knowledge and Power in American Psychiatric NursingNoch keine Bewertungen
- Legal Implications Document A Schneider PDFDokument52 SeitenLegal Implications Document A Schneider PDFAmrod Inglorion100% (2)
- PN FUNDAMENTALS: Passbooks Study GuideVon EverandPN FUNDAMENTALS: Passbooks Study GuideNoch keine Bewertungen
- The Complexities of Care: Nursing ReconsideredVon EverandThe Complexities of Care: Nursing ReconsideredBewertung: 5 von 5 Sternen5/5 (2)
- Real Nursing: Every Second Counts!!: A Comprehensive Guide-book on American Nursing & Healthcare Issues (From Real Nurses’ POV)Von EverandReal Nursing: Every Second Counts!!: A Comprehensive Guide-book on American Nursing & Healthcare Issues (From Real Nurses’ POV)Noch keine Bewertungen
- A few minutes to improve Risk documentation Accuracy even when you know nothing about Medicare Risk AdjustmentVon EverandA few minutes to improve Risk documentation Accuracy even when you know nothing about Medicare Risk AdjustmentNoch keine Bewertungen
- Registered Professional Nurse: Passbooks Study GuideVon EverandRegistered Professional Nurse: Passbooks Study GuideNoch keine Bewertungen
- HOME HEALTH NURSE: Passbooks Study GuideVon EverandHOME HEALTH NURSE: Passbooks Study GuideNoch keine Bewertungen
- Record Keeping for Nurses and Midwives: An essential guideVon EverandRecord Keeping for Nurses and Midwives: An essential guideNoch keine Bewertungen
- How to Succeed New Graduate Nursing Job Interview & Bachelor of Nursing Clinical Placement?Von EverandHow to Succeed New Graduate Nursing Job Interview & Bachelor of Nursing Clinical Placement?Noch keine Bewertungen
- NURSING THE CHILDBEARING FAMILY: Passbooks Study GuideVon EverandNURSING THE CHILDBEARING FAMILY: Passbooks Study GuideNoch keine Bewertungen
- Developing Advanced Assessment Skills: Patients with Long Term ConditionsVon EverandDeveloping Advanced Assessment Skills: Patients with Long Term ConditionsNoch keine Bewertungen
- Certified Long Term Care Nurse: Passbooks Study GuideVon EverandCertified Long Term Care Nurse: Passbooks Study GuideNoch keine Bewertungen
- Documentation: Basic Nursing: Foundations of Skills & Concepts DocumentationDokument8 SeitenDocumentation: Basic Nursing: Foundations of Skills & Concepts DocumentationJona GarzonNoch keine Bewertungen
- A Handbook for Student Nurses, second edition: Introducing Key Issues Relevant for PracticeVon EverandA Handbook for Student Nurses, second edition: Introducing Key Issues Relevant for PracticeNoch keine Bewertungen
- Supervising Registered Nurse: Passbooks Study GuideVon EverandSupervising Registered Nurse: Passbooks Study GuideNoch keine Bewertungen
- The Fundamentals of Quality for Long Term Care: Part 1Von EverandThe Fundamentals of Quality for Long Term Care: Part 1Noch keine Bewertungen
- Proper Nursing Documentation WillDokument4 SeitenProper Nursing Documentation Willbel_dawn019Noch keine Bewertungen
- Competencies of Staff EducatorsDokument17 SeitenCompetencies of Staff EducatorsCherry Mae L. VillanuevaNoch keine Bewertungen
- Nursing by Heart: Transformational Self-Care for NursesVon EverandNursing by Heart: Transformational Self-Care for NursesBewertung: 5 von 5 Sternen5/5 (1)
- PHYSICAL ASSESSMENT: Passbooks Study GuideVon EverandPHYSICAL ASSESSMENT: Passbooks Study GuideNoch keine Bewertungen
- Textbook of Urgent Care Management: Chapter 34, Engaging Accountable Care Organizations in Urgent Care CentersVon EverandTextbook of Urgent Care Management: Chapter 34, Engaging Accountable Care Organizations in Urgent Care CentersNoch keine Bewertungen
- Nurse Compentency ChecklistDokument17 SeitenNurse Compentency ChecklistMary ElizabethNoch keine Bewertungen
- Hospital Vocabulary: English-Arabic Medical WordsVon EverandHospital Vocabulary: English-Arabic Medical WordsNoch keine Bewertungen
- Medical Record Librarian: Passbooks Study GuideVon EverandMedical Record Librarian: Passbooks Study GuideNoch keine Bewertungen
- Medical Record Administrator: Passbooks Study GuideVon EverandMedical Record Administrator: Passbooks Study GuideNoch keine Bewertungen
- AMBULATORY WOMEN'S HEALTH CARE NURSING: Passbooks Study GuideVon EverandAMBULATORY WOMEN'S HEALTH CARE NURSING: Passbooks Study GuideNoch keine Bewertungen
- INFECTION CONTROL: Passbooks Study GuideVon EverandINFECTION CONTROL: Passbooks Study GuideNoch keine Bewertungen
- Transplant Nursing: Scope and Standards of PracticeVon EverandTransplant Nursing: Scope and Standards of PracticeNoch keine Bewertungen
- 2023 Certified Emergency Nurse (CEN) No-Fluff Study Guide:Von Everand2023 Certified Emergency Nurse (CEN) No-Fluff Study Guide:Bewertung: 2 von 5 Sternen2/5 (1)
- Guide To APRN RoleDokument4 SeitenGuide To APRN RoleLaceyNoch keine Bewertungen
- Nursing Process GuideDokument61 SeitenNursing Process GuideMrs Rehan50% (2)
- Documentation for Skilled Nursing & Long-Term Care: A Guide for Occupational TherapistsVon EverandDocumentation for Skilled Nursing & Long-Term Care: A Guide for Occupational TherapistsNoch keine Bewertungen
- A Handbook for Student Nurses, 2015–16 edition: Introducing Key Issues Relevant to PracticeVon EverandA Handbook for Student Nurses, 2015–16 edition: Introducing Key Issues Relevant to PracticeBewertung: 5 von 5 Sternen5/5 (2)
- 17 Tips To Improve Your Nursing DocumentationDokument26 Seiten17 Tips To Improve Your Nursing DocumentationAgustin Lutfiana100% (1)
- Nursing School: The Ultimate Guide with Proven Strategies and Tricks That Help You Completely Crush Nursing School and Become a Registered NurseVon EverandNursing School: The Ultimate Guide with Proven Strategies and Tricks That Help You Completely Crush Nursing School and Become a Registered NurseBewertung: 1 von 5 Sternen1/5 (1)
- Licensed Practical Nurse: Passbooks Study GuideVon EverandLicensed Practical Nurse: Passbooks Study GuideNoch keine Bewertungen
- Observation Summary 2Dokument5 SeitenObservation Summary 2api-493028287Noch keine Bewertungen
- A Core Curriculum for Nurse Life Care PlanningVon EverandA Core Curriculum for Nurse Life Care PlanningBewertung: 4.5 von 5 Sternen4.5/5 (2)
- RN Job Description PDFDokument1 SeiteRN Job Description PDFvhon100% (1)
- The Acute-Care Nurse Practitioner: A Transformational JourneyVon EverandThe Acute-Care Nurse Practitioner: A Transformational JourneyNoch keine Bewertungen
- Practical Nurse: Passbooks Study GuideVon EverandPractical Nurse: Passbooks Study GuideNoch keine Bewertungen
- Documentation 1Dokument26 SeitenDocumentation 1WaaberrinNoch keine Bewertungen
- Being a Nurse: A personal guide from graduation to revalidationVon EverandBeing a Nurse: A personal guide from graduation to revalidationNoch keine Bewertungen
- Information Security and Privacy in Healthcare: Current State of Research1Dokument40 SeitenInformation Security and Privacy in Healthcare: Current State of Research1marie parfanNoch keine Bewertungen
- Opioid Dependence GuidelinesDokument136 SeitenOpioid Dependence Guidelinesanto100% (1)
- Ward ManagementDokument1 SeiteWard Managementaman kumar jhaNoch keine Bewertungen
- 407 e Poa Audit PlanDokument4 Seiten407 e Poa Audit Planapi-270333720Noch keine Bewertungen
- Smart Health Consulting Online System Using BlockchainDokument8 SeitenSmart Health Consulting Online System Using BlockchainIJRASETPublicationsNoch keine Bewertungen
- Chapter 4Dokument9 SeitenChapter 4Banupriya BalasubramanianNoch keine Bewertungen
- SAMPLE Referral Management PolicyDokument3 SeitenSAMPLE Referral Management PolicyDarren Cariño100% (3)
- New Century Wellness Group Case Study 2Dokument4 SeitenNew Century Wellness Group Case Study 2akbarNoch keine Bewertungen
- New Patient FormDokument7 SeitenNew Patient FormajNoch keine Bewertungen
- Topic Week 2 (Tutorial 1)Dokument2 SeitenTopic Week 2 (Tutorial 1)abdo adelNoch keine Bewertungen
- Health Care Mobile ApplicationDokument4 SeitenHealth Care Mobile ApplicationSharan LimraNoch keine Bewertungen
- DPBH Technical Bulletin 08-23-16 - Transfer of Medical RecordsDokument5 SeitenDPBH Technical Bulletin 08-23-16 - Transfer of Medical RecordsBlayne OsbornNoch keine Bewertungen
- Nursing Exam Questions 2023 Part 9Dokument3 SeitenNursing Exam Questions 2023 Part 9Lejo SunnyNoch keine Bewertungen
- Hospital ProposalDokument27 SeitenHospital ProposalSiti Noor MashitahNoch keine Bewertungen
- Understanding The Hospital PlanningDokument33 SeitenUnderstanding The Hospital Planningshruti PatneNoch keine Bewertungen
- OpenERP Modul MedicalDokument33 SeitenOpenERP Modul MedicalhendrigantingNoch keine Bewertungen
- 2.mod Geron 2 DocumentationDokument43 Seiten2.mod Geron 2 Documentationnot your medz duran100% (1)
- Welcome Guide EVANSDokument16 SeitenWelcome Guide EVANSdavidjgoldbergNoch keine Bewertungen
- Trends in NursingDokument25 SeitenTrends in NursingMahalakshmiNoch keine Bewertungen
- Goals of Patient Care GuidelineDokument12 SeitenGoals of Patient Care GuidelineangelaNoch keine Bewertungen
- Hospital Billing and Coding Process PDFDokument44 SeitenHospital Billing and Coding Process PDFrahul_didoNoch keine Bewertungen
- Ethiopian Hospital Services Trasformation Guidelines (Ehstg)Dokument112 SeitenEthiopian Hospital Services Trasformation Guidelines (Ehstg)EzanaNoch keine Bewertungen
- Policies and Procedures in The Issuance of CertificatesDokument3 SeitenPolicies and Procedures in The Issuance of CertificatesREYNALDO DONIO100% (1)
- Hipaa QuizDokument4 SeitenHipaa QuizMike SidesNoch keine Bewertungen
- CHN Lecture Summary 3Dokument6 SeitenCHN Lecture Summary 3Fernand MataNoch keine Bewertungen
- Assessment of Knowledge, Attitude and Practice of Health Information Management Professionals Towards Integrated Disease Surveillance & Response (IDSR) in Abuja, Nigeria.Dokument48 SeitenAssessment of Knowledge, Attitude and Practice of Health Information Management Professionals Towards Integrated Disease Surveillance & Response (IDSR) in Abuja, Nigeria.Victor Chibueze IjeomaNoch keine Bewertungen
- 4 - AMERICAN SOCIETY of HEALTHY-SYSTEM PHARMACISTS - ASHP Guidelines On Documenting Pharmaceutical Care in Patient Medical RecordsDokument3 Seiten4 - AMERICAN SOCIETY of HEALTHY-SYSTEM PHARMACISTS - ASHP Guidelines On Documenting Pharmaceutical Care in Patient Medical RecordsMoisés PonceNoch keine Bewertungen
- Functions of The HospitalDokument6 SeitenFunctions of The Hospitalcheryl3yellow100% (7)
- AMA Code of EthicsDokument5 SeitenAMA Code of EthicsRazell Jean ArazaNoch keine Bewertungen
- Change of GenderDokument1 SeiteChange of GenderLüshī Cataluña-JamileNoch keine Bewertungen