Beruflich Dokumente
Kultur Dokumente
Pneumonia Concept
Hochgeladen von
Revie IglesiasOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pneumonia Concept
Hochgeladen von
Revie IglesiasCopyright:
Verfügbare Formate
encourage pt to take deeper breaths.
Do pt teaching to explain
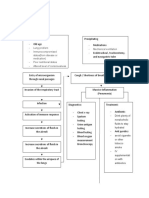
CONCEPT MAP
Collaborate with physician to administer antibiotics to resolve infection
administer supplemental O2 as needed to maintain adequate oxygenation help the client cough and deep breath at least q2hrs to clear airways and expand the lungs at the bases administer prescribed nebulizer breathing treatments to open airways
Saucier, Hali SNPLU 2/25/08
importance of lung expansion with pneumonia. sit pt up in bed (high fowlers) to decrease pressure on chest and allow for adequate lung expansion. Obtain an incentive spirometer for the pt to encourage deep breathing. Pt teaching on the importance of weight loss
Medical Diagnosis
Pathophysiology
Patients Story
Diagnostic Workup
Clinical Manifestation
Nursing Diagnosis
Etiology & Risk Factors
Expected Outcome
Pt. will achieve adequate ventilation
Ineffective breathing pattern r/t obesity and fatigue, AEB SOB, RR, depth of breathing, and pt reports difficulty taking deep breaths (4).
Pt will experience improved oxygenation
Impaired gas exchange r/t ed functional lung tissue
(4) AEB dyspnea, tachycardia, ed RR, and O2 of less than 92% on RA.
Secondary Diagnosis
Nursing Interventions
Patients Medications: (2).
For pneumonia: - Levofloxacin (Levaquin): anti-infective - Cefalosporin): anti-infective, 3rd generation. - Albuterol: adrenergic bronchodilator - Ipratropium (Atrovent): anticholinergic bronchodilator Other Medications: - Viramune: antiviral (plus one other antiviral that I forgot the name) - Insulin coverage for diabetes - Nystatin (candida) - Heparin sc (DVT prevention) - Warfarin (DVT prevention anticoagulant) - Furosemide (Lasix): edema - Acetaminophen (for pain) Discharge Planning: - communicate with LCT facility to update on pt discharge status - ensure pt has adequate ventilation/oxygenation before d/c. Arrange for portable O2 if needed. - Pt teaching on pneumonia prevention
My patient was a female in her 60s who lives in an assisted living rehab facility. She came to the hospital with chest pain, SOB, fever, and productive cough. She also had cellulitis in her lower extremities that was getting worse. She was admitted for 5 days to receive IV antibiotics. I cared for her on the 5th day, so she had few s/s of pneumonia. Pneumonia is an inflammation in the alveoli and the interstitium of the lung, usually caused by an infection (3). There are several different types, including community acquired, hospital acquired, aspiration, fungal, and opportunistic (1). This particular patient had what is called health-care associated pneumonia, because she had been living in an assisted living facility. However, I think it could also be considered opportunistic because of her compromised immune status. In pneumonia, the infective agent enters the lung (pseudomonas in this case), multiplies, and triggers inflammation. The alveoli fill with exudative fluid which impairs gas exchange. Exudate can consolidate and become difficult to cough up (3). Bacterial pneumonia is usually associated with a productive cough, whereas viral is not (1).
Pneumonia
Incidence: Health-care Associated Pneumonia occurs in about 5-15 cases out of every 1000 hospital admissions. HAP is the 2nd most common nosocomial infection after UTIs (1.)
Chest X-ray shows white shadows (parenchymal infiltrates (3). Culture and sensitivity. Gram-stain of sputum to differentiate bacterial from viral causes and gram + vs. -. WBC elevation (greater than 15,000/l (3).)
sudden onset of fever/chills SOB, increased RR Productive cough (bacterial) Pleuritic chest pain Confusion or stupor (due to hypoxia) Crackles, fremitus, bronchial breath sounds
- breast cancer
HIV (both of the above are 2 diagnoses that could have contributed to the development of pneumonia due to compromised immunity from HIV and from chemotherapy.) Diabetes Lymphedema and Cellulitis in lower extremities Hx of MRSA, Hep C, CHF, MI, A-fib
Risk factors: chronic illness immobility immunosuppression post-surgery/anesthesia
References:
1. Lewis S.L., Heitkemper M.M., Dirkesen S.R., OBrien P.G., & Bucher L. (2007). Medical surgical nursing: Assessment and management of clinical problems (7th ed.). St. Louis: Mosby Elsevier. 2. Deglin J.H., & Vallerand A.H. (2007). Daviss drug guide for nurses (10th ed.). Philadelphia: F.A. Davis Company 3. Copstead L.C., & Banasik J.L. (2005). Pathophysiology (3rd ed.). St. Louis: Elsevier Saunders. 4. Ackley B.J. & Ladwig G.B. (2006). Nursing diagnosis
Das könnte Ihnen auch gefallen
- Pa Tho Physiology Sle, CompDokument5 SeitenPa Tho Physiology Sle, CompHassan Bj MarabongNoch keine Bewertungen
- Reproductive System Development: Ob NotesDokument2 SeitenReproductive System Development: Ob NotesLykee PadillaNoch keine Bewertungen
- Congestive Heart Failure and Pulmonary Edema Concept MapDokument1 SeiteCongestive Heart Failure and Pulmonary Edema Concept MapAndrew Godwin100% (5)
- CHF Cardiomegaly Volume OverloadDokument1 SeiteCHF Cardiomegaly Volume Overloadnursing concept mapsNoch keine Bewertungen
- Concept Map HypertensionDokument1 SeiteConcept Map Hypertensiongeorge pearson0% (1)
- Reason For Needing Health Care: Key Problem / ND: Noncompliance Key Problem / NDDokument6 SeitenReason For Needing Health Care: Key Problem / ND: Noncompliance Key Problem / NDnursing concept mapsNoch keine Bewertungen
- Shock Comparison ChartDokument2 SeitenShock Comparison Chartlinnaete88% (8)
- PathoPhysiology of Renal Failure OverviewDokument7 SeitenPathoPhysiology of Renal Failure Overviewnursing concept maps100% (1)
- Congestive Heart Failure. Case Study ExplanationDokument6 SeitenCongestive Heart Failure. Case Study ExplanationOkenabirhie100% (1)
- Concept Map COPDDokument2 SeitenConcept Map COPDJilian McGugan88% (40)
- Pharmacology Drug ClassificationDokument4 SeitenPharmacology Drug ClassificationjetdoctrzNoch keine Bewertungen
- Change Your Breakfast Change Your Life PDFDokument189 SeitenChange Your Breakfast Change Your Life PDFDrUmeshSharmaNoch keine Bewertungen
- Concept Map PEDokument3 SeitenConcept Map PERobert MariasiNoch keine Bewertungen
- Heart Failure COncept MapDokument2 SeitenHeart Failure COncept MapJrBong SemaneroNoch keine Bewertungen
- Renal and Urinary Concept MapsDokument8 SeitenRenal and Urinary Concept Mapsnursing concept maps100% (1)
- Pneumonia Concept Map - KPoindexterDokument1 SeitePneumonia Concept Map - KPoindexterKatie_Poindext_5154100% (2)
- System Disorder - Cystic FibrosisDokument1 SeiteSystem Disorder - Cystic Fibrosisjorge herreraNoch keine Bewertungen
- Pneumonia Concept MapDokument11 SeitenPneumonia Concept Mapiz11100% (3)
- ARDS Concept MapDokument1 SeiteARDS Concept Mapadro100% (2)
- ABGs Respiratory/MetabolicDokument3 SeitenABGs Respiratory/MetabolicJoe B100% (1)
- Asthma Pathophysiology and TreatmentDokument3 SeitenAsthma Pathophysiology and TreatmentKaren HutchinsonNoch keine Bewertungen
- Respiratory Distress SyndromeDokument3 SeitenRespiratory Distress SyndromeAshNoch keine Bewertungen
- Pathophysiology of PneumothoraxDokument1 SeitePathophysiology of PneumothoraxDizah Faye OsboroNoch keine Bewertungen
- Patho AsthmaDokument1 SeitePatho AsthmaAyel JimenezNoch keine Bewertungen
- Hide 1 Description 2 Classification 2.1 Chronic Bronchitis 2.2 Emphysema 3 Pathophysiology 4 EpidemiologyDokument29 SeitenHide 1 Description 2 Classification 2.1 Chronic Bronchitis 2.2 Emphysema 3 Pathophysiology 4 EpidemiologyAngie Mandeoya100% (1)
- Concept MapDokument5 SeitenConcept Mapmild_tea100% (1)
- Pathophysiology of Heart FailureDokument4 SeitenPathophysiology of Heart FailureTiger Knee100% (2)
- Pediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsDokument2 SeitenPediatrics Pediatrics Pediatrics Pediatrics Pediatrics: Pediatrics Pediatrics Pediatrics Pediatrics PediatricsBobet Reña100% (2)
- PneumoniaDokument1 SeitePneumonianursing concept mapsNoch keine Bewertungen
- Fluidsandelectrolytes 090224074347 Phpapp02Dokument102 SeitenFluidsandelectrolytes 090224074347 Phpapp02IsaacJ22Noch keine Bewertungen
- COPD Risk Factors, Signs, Treatments & Nursing CareDokument2 SeitenCOPD Risk Factors, Signs, Treatments & Nursing CareJilian McGugan100% (9)
- Med Surg Week 6Dokument11 SeitenMed Surg Week 6Eunice Cortés100% (1)
- Survival Strategies For Parenting The Child & Teen With BipolarDokument236 SeitenSurvival Strategies For Parenting The Child & Teen With Bipolarseptiadhi wirawanNoch keine Bewertungen
- Sicle Cell Concept MapDokument1 SeiteSicle Cell Concept MapRosa100% (1)
- Tonsillectomy Slides 050427Dokument62 SeitenTonsillectomy Slides 050427Aidiel FikriNoch keine Bewertungen
- HELLP Concept Map RevisedDokument1 SeiteHELLP Concept Map RevisedwandaNoch keine Bewertungen
- ATLS ProtocoloDokument21 SeitenATLS Protocoloedgarjavier65100% (2)
- Hypertension Concept MapDokument1 SeiteHypertension Concept Mapgfhbgfhgf71% (7)
- Cardiovascular Disease Concept MapDokument5 SeitenCardiovascular Disease Concept MapRye Anch100% (1)
- Hypothyroidism Concept MapDokument5 SeitenHypothyroidism Concept Mapnursing concept maps0% (1)
- Concept MapDokument1 SeiteConcept MapChristine Marie Barce Martinez100% (2)
- Dental Caries IndexDokument35 SeitenDental Caries Indexdr parveen bathla100% (1)
- Pathophysiology of PneumoniaDokument2 SeitenPathophysiology of PneumoniaIrene Demegillo SalongaNoch keine Bewertungen
- COPD Concept MapDokument1 SeiteCOPD Concept MapSherree HayesNoch keine Bewertungen
- Nursing KardexDokument2 SeitenNursing Kardexjerimiah_manzon100% (3)
- Community Health Nursing Bag TechniqueDokument10 SeitenCommunity Health Nursing Bag TechniqueKBDNoch keine Bewertungen
- Pathophysiology SARSDokument4 SeitenPathophysiology SARSStephanie Joy Escala71% (7)
- CC Concept MapDokument9 SeitenCC Concept Mapapi-606252228Noch keine Bewertungen
- 1 Ineffective Breathing PatternDokument8 Seiten1 Ineffective Breathing PatternNoel MontemayorNoch keine Bewertungen
- Rehabilitation in The Dynamic Stabilization of Lumbar SpineDokument41 SeitenRehabilitation in The Dynamic Stabilization of Lumbar SpineYip Song ChongNoch keine Bewertungen
- CC-Concept Map 2Dokument5 SeitenCC-Concept Map 2MDCITY50% (2)
- OB Concept MapDokument2 SeitenOB Concept MapJennifer Lewis100% (1)
- Pa Tho Physiology of Congestive Heart FailureDokument3 SeitenPa Tho Physiology of Congestive Heart FailureErin MarieNoch keine Bewertungen
- Pa Tho Physiology of URTIDokument3 SeitenPa Tho Physiology of URTIJericho Moris U. LagmayNoch keine Bewertungen
- ACTIVE LEARNING TEMPLATE: System DisorderDokument1 SeiteACTIVE LEARNING TEMPLATE: System DisorderDeo FactuarNoch keine Bewertungen
- Pathophysiology PneumoniaDokument2 SeitenPathophysiology PneumoniaChiro Rouy Malaluan100% (2)
- Mnemonics PDFDokument15 SeitenMnemonics PDFbeingfiredNoch keine Bewertungen
- UTI Patient Concept Map Nursing Diagnosis Interventions OutcomesDokument1 SeiteUTI Patient Concept Map Nursing Diagnosis Interventions OutcomesDon Rieza100% (1)
- Nursing Management Concept MapDokument1 SeiteNursing Management Concept MapXy-Za Roy Marie100% (1)
- Concept Map Finished 2Dokument6 SeitenConcept Map Finished 2api-352785497100% (1)
- Causes, Symptoms and Complications of Acute and Subacute Infective EndocarditisDokument6 SeitenCauses, Symptoms and Complications of Acute and Subacute Infective EndocarditisRobert So Jr100% (1)
- Concept Map Pleural EffusionDokument1 SeiteConcept Map Pleural Effusionapi-341263362Noch keine Bewertungen
- Pediatric DisorderDokument35 SeitenPediatric DisorderDenaise MarieNoch keine Bewertungen
- Anemia: Ch. 31 Hematologic ProblemsDokument36 SeitenAnemia: Ch. 31 Hematologic Problemshops23100% (3)
- TMendoza CriticalCareConceptMap2Dokument5 SeitenTMendoza CriticalCareConceptMap2Theresa Fernandez Mendoza0% (1)
- Nursing Care Plan WeeblyDokument8 SeitenNursing Care Plan Weeblyapi-277498943Noch keine Bewertungen
- PneumoniaDokument7 SeitenPneumoniaJhgrace Mary Pacaña GalloNoch keine Bewertungen
- Pneumocytis Carinii PneumoniaDokument26 SeitenPneumocytis Carinii Pneumoniafrancis00090Noch keine Bewertungen
- Respiratory Problems in PregnancyDokument16 SeitenRespiratory Problems in PregnancyYvette Carmelle Barroma GellangNoch keine Bewertungen
- Resume 2014nhDokument1 SeiteResume 2014nhRevie IglesiasNoch keine Bewertungen
- Vision Mission: B P S UDokument3 SeitenVision Mission: B P S URevie IglesiasNoch keine Bewertungen
- High School Life: - Finish Studying in High School - Avoid Failing Grades - Pass The Dost-Sei ScholarshipDokument1 SeiteHigh School Life: - Finish Studying in High School - Avoid Failing Grades - Pass The Dost-Sei ScholarshipRevie IglesiasNoch keine Bewertungen
- Rose Ann I. Escropolo: ObjectiveDokument1 SeiteRose Ann I. Escropolo: ObjectiveRevie IglesiasNoch keine Bewertungen
- My Self ProfileDokument13 SeitenMy Self ProfileRevie IglesiasNoch keine Bewertungen
- Answer Key 3rd G Unified Test g9Dokument1 SeiteAnswer Key 3rd G Unified Test g9Revie IglesiasNoch keine Bewertungen
- Transfer LetterDokument1 SeiteTransfer LetterRevie IglesiasNoch keine Bewertungen
- A Newspaper Story by ODokument3 SeitenA Newspaper Story by ORevie IglesiasNoch keine Bewertungen
- 2Dokument2 Seiten2Revie IglesiasNoch keine Bewertungen
- Head Nsg. Med Ob TopicsxfDokument1 SeiteHead Nsg. Med Ob TopicsxfRevie IglesiasNoch keine Bewertungen
- Strong FamilyDokument2 SeitenStrong FamilyRevie IglesiasNoch keine Bewertungen
- African Musical InstrumentDokument1 SeiteAfrican Musical InstrumentRevie IglesiasNoch keine Bewertungen
- This Video Presents How To Use A Meter To Fix TelevisionDokument1 SeiteThis Video Presents How To Use A Meter To Fix TelevisionRevie IglesiasNoch keine Bewertungen
- Chocolate Brownies RecipeDokument4 SeitenChocolate Brownies RecipeRevie IglesiasNoch keine Bewertungen
- 2Dokument2 Seiten2Revie IglesiasNoch keine Bewertungen
- YANA's YANA's YANA's YANA's: Contact #: Contact #: Contact #: Contact #Dokument1 SeiteYANA's YANA's YANA's YANA's: Contact #: Contact #: Contact #: Contact #Revie IglesiasNoch keine Bewertungen
- ASSESSMEN3Dokument31 SeitenASSESSMEN3Revie IglesiasNoch keine Bewertungen
- This Video Presents How To Use A Meter To Fix TelevisionDokument1 SeiteThis Video Presents How To Use A Meter To Fix TelevisionRevie IglesiasNoch keine Bewertungen
- Compre-Foundation of Educ. VilmaDokument54 SeitenCompre-Foundation of Educ. VilmaRevie IglesiasNoch keine Bewertungen
- Activity 3. Pick and MatchDokument2 SeitenActivity 3. Pick and MatchRevie IglesiasNoch keine Bewertungen
- College of Education: Bataan Peninsula State UniversityDokument3 SeitenCollege of Education: Bataan Peninsula State UniversityRevie IglesiasNoch keine Bewertungen
- 7-3-47 - Care of Endotracheal Nasotracheal Tracheostomy TubesDokument4 Seiten7-3-47 - Care of Endotracheal Nasotracheal Tracheostomy TubesRevie IglesiasNoch keine Bewertungen
- 9Dokument5 Seiten9Revie IglesiasNoch keine Bewertungen
- Aging in PlaceDokument9 SeitenAging in PlaceRevie IglesiasNoch keine Bewertungen
- A Newspaper Story by ODokument3 SeitenA Newspaper Story by ORevie IglesiasNoch keine Bewertungen
- My Self ProfileDokument13 SeitenMy Self ProfileRevie IglesiasNoch keine Bewertungen
- Ideaspace Mechanics and GuidelinesDokument2 SeitenIdeaspace Mechanics and GuidelinesRevie IglesiasNoch keine Bewertungen
- Activity 3. Pick and MatchDokument2 SeitenActivity 3. Pick and MatchRevie IglesiasNoch keine Bewertungen
- Loyalty Card Application Form (HQP-PFF-108, V02)Dokument2 SeitenLoyalty Card Application Form (HQP-PFF-108, V02)Revie Iglesias100% (1)
- Rose Ann EscropoloJune20Dokument1 SeiteRose Ann EscropoloJune20Revie IglesiasNoch keine Bewertungen
- My ResumeDokument4 SeitenMy ResumeJal-Fem AngelesNoch keine Bewertungen
- Meningitis Beyond Neonatal AgeDokument57 SeitenMeningitis Beyond Neonatal AgeTilahun Kegne100% (2)
- Academic Style - Practice-1Dokument5 SeitenAcademic Style - Practice-1Anonymous 3s2uAgNoch keine Bewertungen
- Medical History QuestionnaireDokument3 SeitenMedical History QuestionnaireSachitra Nirman MalwatteNoch keine Bewertungen
- Chronic Care ManagementDokument8 SeitenChronic Care Managementsyion971Noch keine Bewertungen
- 11 Conditions Mistaken For Child AbuseDokument7 Seiten11 Conditions Mistaken For Child AbuseAlison PalethorpeNoch keine Bewertungen
- Total Gastrectomy - Options For The Restoration of Gastrointestinal Continuity PDFDokument6 SeitenTotal Gastrectomy - Options For The Restoration of Gastrointestinal Continuity PDFJorge SalinasNoch keine Bewertungen
- Gallstones: American College of Gastroenterology Common Gastrointestinal ProblemsDokument2 SeitenGallstones: American College of Gastroenterology Common Gastrointestinal ProblemsanonNoch keine Bewertungen
- Weebly ResumeDokument4 SeitenWeebly Resumeapi-295640482Noch keine Bewertungen
- Dehydration PPDokument17 SeitenDehydration PPApol PenNoch keine Bewertungen
- Tracheo-Oesophageal FistulaDokument19 SeitenTracheo-Oesophageal Fistularajan kumar100% (3)
- Medtronic Shares Ventilation Design Specifications To Accelerate Efforts To Increase Global Ventilator ProductionDokument1 SeiteMedtronic Shares Ventilation Design Specifications To Accelerate Efforts To Increase Global Ventilator Productionmorton1472Noch keine Bewertungen
- Baby Gap: The Surprising Truth About America's Infant-Mortality RateDokument2 SeitenBaby Gap: The Surprising Truth About America's Infant-Mortality RateJoseph AltmannNoch keine Bewertungen
- 8 Emergency Formative Clinical Evaluation ChecklistDokument1 Seite8 Emergency Formative Clinical Evaluation Checklistمهند الرحيليNoch keine Bewertungen
- Dengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaDokument3 SeitenDengue Disease Spectrum Among Infants in The 2001 Dengue Epidemic in Chennai, Tamil Nadu, IndiaReju VijayandranNoch keine Bewertungen
- Introduction To AnesthesiologyDokument68 SeitenIntroduction To AnesthesiologyOzza AlhudaNoch keine Bewertungen
- ICNCDRS Blindness Registry FormDokument4 SeitenICNCDRS Blindness Registry FormAprilAngeliRobleNoch keine Bewertungen
- Shock Resident LectureDokument38 SeitenShock Resident Lecturepapermate9293Noch keine Bewertungen
- Diet and NutritionDokument92 SeitenDiet and NutritionSheeba AnilNoch keine Bewertungen
- Instrument ProcessingDokument47 SeitenInstrument ProcessingMarwa Temirek100% (1)
- Poster PresentationDokument1 SeitePoster PresentationAayat KhanNoch keine Bewertungen