Beruflich Dokumente
Kultur Dokumente
Genrl
Hochgeladen von
Saba KhanOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Genrl
Hochgeladen von
Saba KhanCopyright:
Verfügbare Formate
World Applied Sciences Journal 5 (3): 267-271, 2008 ISSN 1818-4952 IDOSI Publications, 2008
Antibacterial Activity of Important Medicinal Plants on Human Pathogenic Bacteria-a Comparative Analysis
1
H.V. Girish and 2S. Satish
Department of Studies in Botany, Plant Biotechnology Laboratory, University of Mysore, Manasagangotri, Mysore- 570 006, Karnataka, India 2 Department of Studies in Microbiology, Herbal Drug Technology Laboratory, University of Mysore, Manasagangotri, Mysore- 570 006, Karnataka, India
Abstract: The use of plants in treatment of burns, dermatophytes and infectious diseases is common in traditional medicine. Based on ethno pharmacological and taxonomic information, antibacterial activities of aqueous and methanol extracts of some medicinal plants were determined by in vitro by agar diffusion-method against some human pathogenic bacteria. The leaves of five different plants, belonging to the different family and which have some ethnomedicinal applications were studied for antibacterial activity. Powdered leaf materials of all selected plants were extracted with aqueous and methanol. The solvent extracts were evaporated to dryness using rotary flash evaporator. Dry residue was dissolved in methanol (1:10 w/v) and tested for antibacterial activity. The antibacterial screening of aqueous and methanol extract carried out in vitro on the following bacteria viz., Bacillus cereus, Bacillus megaterium, Bacillus subtilis, Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Salmonella typhi, Staphylococcus aureus, Streptococcus faecalis and Yersinia enterocolitica. It has been showed that the methanol extracts had wider range of activity on these organisms than the aqueous extracts, which indicates that the methanol extracts of all selected plants may contain the active components. This study supports, the traditional medicines (herbal extracts) to cure many diseases like diarrhea, intestinal tract, throat, ear infections, fever and skin diseases. Key words: Antibacterial % Medicinal plants % Human pathogens INTRODUCTION Plant based antimicrobials represent a vast untapped source for medicines and further exploration of plant antimicrobials needs to occur. Antimicrobials of plant origin have enormous therapeutic potential [1]. Human infections particularly those involving microorganisms i.e. bacteria, fungi, viruses, they cause serious infections in tropical and subtropical countries of the world. In recent years, multiple drug resistance in human pathogenic microorganisms has been developed due to indiscriminate use of commercial antimicrobial drugs commonly used in the treatment of such diseases [2, 3]. In general, bacteria have the genetic ability to transmit and acquire resistance to drugs, which are utilized as therapeutic agents [4]. The problem of microbial resistance is growing and the outlook for the use of antimicrobial drugs in the future is still uncertain. Therefore, actions must be taken to reduce this problem, for example, to control the use of antibiotic, develop research to better understand the genetic mechanisms of resistance and to continue studies to develop new drugs, either synthetic or natural. The ultimate goal is to offer appropriate and efficient antimicrobial drugs to the patient. Over the past twenty years, there has been a lot of interest in the investigation of natural materials as sources of new antibacterial agents [5, 6]. Different extracts from traditional medicinal plants have been tested. Many reports have show the effectiveness of traditional herbs against microorganisms, as a result, plants are one of the bedrocks for modern medicine to attain new principles [7]. The increasing interest on traditional ethno medicine may lead to discovery of novel therapeutic agents. Medicinal plants are finding their way into pharmaceuticals, neutralceuticals, cosmetics and food supplements. In this regard, plants have given western pharmacopoeia about
Corresponding Author: Dr. S. Satish, Department of Studies in Microbiology, Herbal Drug Technology Laboratory, University of Mysore, Manasagangotri, Mysore-570 006, Karnataka, India
267
World Appl. Sci. J., 5 (3): 267-271, 2008
7000 different pharmaceutically important compounds and a number of top-selling drugs of modern time, e.g. quinine, artemisinin, taxol, camptothecin, etc. [8]. Until natural products have been approved as new antibacterial drugs, there is an urgent need to identify novel substances active towards highly resistant pathogens [9, 10]. Biomolecules of plant origin appear to be one of the alternatives for the control of these antibiotic resistant human pathogens [11]. Hence, more studies pertaining to the use of plants as therapeutic agents should be emphasized, especially those related to the control of antibiotic resistant microbes. The objective of this research was to evaluate the potentiality of plant extracts on standard microorganism strains as well as on the multi-drug resistant bacteria. MATERIALS AND METHODS Selection of Medicinal Plants for the Study: Five medicinal plants viz. Boerhaavia diffusa, Cassia auriculata, Cassia Lantana, Eclipta alba and Tinospora cardiofolia were selected based on ethanomedical importance. Healthy, disease free leaves of selected plants were collected in around Mysore, Mysore District, Karnataka (India) were used for the preparation of aqueous and solvent extracts. Test Microorganisms: Authentic pure cultures of human pathogenic bacteria like Bacillus cereus, Bacillus subtilis, Escherichia coli, Klebsiella sp., Proteus mirabilis, Pseudomonas aeruginosa, Salmonella typhi, Shigella sp., Staphylococcus aureus and Yersinia enterocolitica, were obtained from Department Microbiology, Mysore Medical College and Research Institute, Rajiv Gandhi University, Mysore, India. PREPARATION OF EXTRACTS Grinding of the Selected Plant Materials: After drying at 37C for 24 h the plant material was ground in a grinding machine (Thomas Wiley laboratory mill, model # 4, screen size-1mm) made for the laboratory. Exposure to direct sunlight was avoided to prevent the loss of active components. Preparation of Leaf Aqueous Extract: Fifty grams of selected fresh leaf materials was macerated with 50 ml of sterile distilled water in a grinding machine (Thomas Wiley laboratory mill, model # 4, screen size-1mm) for about 10-15 min. The macerate was first filtered through
double layer muslin cloth then centrifuged at 3500 rpm for 30 min. The supernatant was filtered through. Whatman No. 1 filter paper and sterilized at 120C for 30 minutes. The extracts were preserved aseptically at 5C for further use [12]. Preparation of Leaf Solvent Extract: Thoroughly washed selected plant leaf materials were dried in shade and then powdered with the help of grinding machine. 50 grams of shade dried powder was filled in the thimble and extracted with 150 ml of methanol successively up to 48 h. The solvent extracts were concentrated separately under reduced pressure [13]. Extract from this method was then weighed and stored at 22C in desiccators until further use. After complete solvent evaporation, one gram of each concentrated solvent extracts were dissolved in 9 ml of methanol and used for antibacterial assays. ANTIBACTERIAL ACTIVITY ASSAY Antibacterial activity of aqueous and solvent extracts of all the selected plant extracts was determined by the cup diffusion method on nutrient agar medium [14]. Both the aqueous and solvent extracts of plants were screened for the antibacterial assay. Aqueous Extract: The organism to be tested was inoculated into sterile nutrient agar. After incubation period of 24 h at 37C, a loop of inoculum was transferred into 5 ml of nutrient broth and incubated for 2 h at 37C which served as fresh suspension inoculum. Five wells (5 mm diameter) were made in sterile nutrient agar plate using cork borer (one in the center and four wells at the corner) and inoculum containing 106 CFU/ml of test bacteria were spread on solid plates with the help of sterile swab moistened with the bacterial suspension. Then 50 l of aqueous extract of all the leaves were placed in the wells made in inoculated plates. The treatment also includes 50 l of sterilized distilled water as control. All the plates were incubated for 24 h at 37C and zone of inhibition if any around the well were measured in millimeter (mm). For each treatment six replicates were maintained. Solvent Extract: One gram of all the selected plant leaf extract were dissolved in 9ml of methanol. The sterile nutrient agar medium in Petridishes was uniformly smeared with test culture. Well (5 mm) were made in each petridish to which 50 l of solvent extracts dissolved in methanol were added. For each treatment six replicates were maintained. Methanol served as control.
268
World Appl. Sci. J., 5 (3): 267-271, 2008
RESULTS The antibacterial activity of aqueous and methanol extracts of selected plants against human pathogenic bacteria both Gram-positive and Gram-negative bacteria are presented in Table 1. Activity was analyzed at 50 l of aqueous extract. Only three plant species viz., Boerhaavia diffusa, Tinospora cardiofolia and Eclipta alba showed antibacterial activity. Cassia auriculata and Cassia Lantana did not show much significant activity. The results revealed that among ten pathogenic bacteria, only Staphylococcus aureus was susceptible for Boerhaavia diffusa followed by Bacillus megaterium and Streptococus faecalis by Tinospora cardiofolia and Eclipta alba respectively. Among the tested pathogens only Staphylococcus aureus belongs to Gram-positive bacteria showed maximum inhibition. However, at the test concentration of the plant extracts produced wider zones of inhibition for S. aureus, Bacillus megaterium, Streptococus faecalis and B. substilis when compared to the zones of inhibition of the gram-negative isolates. Table 1 indicates that the selected plant extracts inhibited the growth of all the tested microorganisms with the exception. The extracts showed significant antibacterial activity against Staphylococcus aureus, Bacillus megaterium and Streptococus faecalis. In Boerhaavia diffusa maximum inhibition was observed in Staphylococcus aureus followed by Bacillus megaterium and Bacillus cereus respectively at 50 l concentration. It also observed that still it exerts some degree of sensitivity on Gram-negative bacteria also. In case of Tinospora cardiofolia and Eclipta alba similar results were obtained. Both the plant extracts were
highly sensitive for Gram-positive bacteria. Even though they showed maximum inhibition for Gram-positive bacteria, the extracts still exerts significant inhibition against Gram-negative bacteria like Escherichia coli, Pseudomonas aeruginosa and Yersinia enterocolitica respectively. The results has been showed that, Salmonella typhi and Pseudomonas aeruginosa is less sensitive for all tested plant extracts, where as other Gram-negative bacteria showed some degree of susceptible for extract of all selected plants. However, Cassia auriculata and Cassia lantana showed lesser zone of inhibition in all tested pathogenic bacteria, when compared to the zones of inhibition of other plant extracts. The data revealed that significant inhibitory activity was observed in three important selected plants of methanol extracts. DISCUSSION Recently, much attention has been directed toward plant extracts and biologically active compounds isolated from popular plant species. The use of medicinal plants plays a vital role in covering the basic health needs in developing countries and these plants may offer a new source of antibacterial, antifungal and antiviral agents with significant activity against infective microorganisms [15, 16]. On the basis of the result obtained in this present investigation, we conclude that the methanol extract of Boerhaavia diffusa, Tinospora cardiofolia and Eclipta alba leaves had significant in vitro antimicrobial activity. This implied that the gram-positive bacteria were more susceptible to the extract than the gram-negative bacteria. Possibly because of the presence of outer
Table 1: Antibacterial activity of aqueous and methanol extracts of selected plant leaves and antibiotic against some human pathogenic bacteria at 50 l. (Zone of inhibition measured in mm) Zone of inhibition (mm) --------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------Boerhaavia diffusa Human pathogenic bacteria Bacillus subtilis Bacillus cereus Bacillus megaterium Escherichia coli Klebsiella pneumoniae Pseudomonas aeruginosa Salmonella typhi Staphylococcus aureus Streptococcus faecalis Yersinia enterocolitica ----------------------------Aqueous 8.830.30 9.730.32 00.000.00 8.000.00 10.000.00 9.000.00 8.500.22 13.830.30 8.83 0.30 9.16 0.30 Methanol 18.030.30 19.200.60 20.500.25 13.130.30 10.160.60 11.230.46 12.630.60 23.13 0.30 13.50 0.25 10.75 0.30 Cassia auriculata -----------------------------Aqueous 00.000.00 00.000.00 00.000.00 6.000.00 00.000.00 00.000.00 00.000.00 Methanol 7.830.22 7.000.00 9.000.00 8.500.22 00.000.00 11.330.30 10.830.30 Cassia lantana ---------------------------Aqueous 6.500.22 00.000.00 00.000.00 7.330.30 00.000.00 8.000.00 00.000.00 7.930.22 Methanol 11.160.30 9.830.30 10.000.00 7.000.00 00.000.00 9.530.30 7.930.22 18.83 0.60 9.22 0.42 8.50 0.22 Eclipta alba ---------------------------Aqueous 7.830.22 8.160.60 9.000.00 10.500.22 9.000.00 10.83 0.30 10.000.00 11.16 0.30 11.83 0.60 9.16 0.30 Methanol 19.330.30 17.230.60 19.230.30 17.450.22 16.160.60 14.000.00 16.000.00 20.83 0.60 18.000.00 15.25 0.40 Tinospora cardiofolia -------------------------------------------------------Aqueous 9.160.60 8.830.30 12.500.22 7.160.42 8.000.00 7.000.00 7.160.42 10.16 0.30 11.00 0.00 10.25 0.30 Methanol Kanamycin ( 30 l) 19.830.30 18.860.60 22.160.30 21.760.30 13.50 0.22 15.670.47 10.000.00 20.20 0.60 22.50 0.40 16.50 0.22 41.670.27 33.500.27 30.330.27 39.270.27 31.330.27 30.500.25 33.000.00 25.50 0.47 35.50 0.00 25.50 0.27
9.46 0.60 12.13 0.30 00.000.00 00.000.00
7.16 0.42 00.000.00 6.50 0.22 00.000.00
Values are the mean of three replicates standard error. P<0.05
269
World Appl. Sci. J., 5 (3): 267-271, 2008
membrane that serves as an effective barrier in gramnegative species [17, 18]. In addition, since the zone of inhibition is almost equal to the standard, it shows that the test organisms are sensitive to the plant extract. S. aureus was the most susceptible bacterium, an observation that may be attributed to the presence of single membrane of the organism which makes it more accessible to permeation by active principles of the extract of Boerhaavia diffusa. In contrast, Salmonella typhi and P. aeruginosa showed the least susceptibility to the extract. This may be due to the fact that P. aeruginosa has intrinsic resistance from a restrictive outer membrane barrier and transenvelope multidrug resistance pumps (MDRs). The results of present research highlights, the fact that the organic solvent extracts exhibited greater antimicrobial activity because the antimicrobial principles were either polar or non-polar and they were extracted only through the organic solvent medium [3, 19 ]. The present observation suggests that the organic solvent extraction was suitable to verify the antimicrobial properties of medicinal plants and they supported by many investigators [20-23]. The present study justifies the claimed uses of Boerhaavia diffusa, Tinospora cardiofolia and Eclipta alba in the traditional system of medicine to treat various infectious diseases caused by the microbes. This study also encourages cultivation of the highly valuable plant in large-scale to increase the economic status of cultivars in the country. The obtained results may provide a support to use of the plant in traditional medicine. Based on this, further chemical and pharmacological investigations to isolate and identify minor chemical constituents in Boerhaavia diffusa, Tinospora cardiofolia and Eclipta alba and to screen other potential bioactivities may be recommended. ACKNOWLEDGMENT
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12. The authors are thankful to the Department of Studies in Botany, Department of Studies in Microbiology, University of Mysore for providing facilities and the DST for providing financial support. REFERENCES 1. Salau, A.O. and O.M. Odeleye, 2007. Antimicrobial activity of Mucuna pruriens on selected Bacteria. African J. Biotechnol., 6(18): 2091-2092.
13. 14.
Gutmann, L., D. Billot-Klein, R. Williamson, F.W. Goldstein, J. Mounier, J.F. Acar and E. Collatz, 1988. Mutation of Salmonella paratyphi A conferring cross-resistance to several groups of antibiotics by decreased permeability and loss of invasiveness. Antimicrob. Agents Chemothe 32: 195-201. Mohanasundari, C., D. Natarajan, K. Srinivasan, S.A. Umamaheswari and A. Ramachandran, 2007. Antibacterial properties of Passiflora foetida L. -a common exotic medicinal plant. African J. Botechnol., 6(23): 2650-2653. Cohen, M.L., 1992. Epidemiology of drug resistance: implications for a postantimicrobialera. Science, 257: 1050-1055, Werner, F., P. Okemo and R. Ansorg, 1999. Antibacterial activity of East African Medicinal plants. J. Ethnopharmacol., 60: 79-84. Samy, R.P. and S. Ignacimuthu, 2000. Antibacterial activity of some folklore medicinal plants used by tribals in Western Ghats of India. J. Ethnopharmacol., 69: 63-71. Evans, C.E., A. Banso and O.A. Samuel, 2002. Efficacy of some nupe medicinal plants against Salmonella typhi: an in vitro study. J. Ethnopharmacol., 80: 21-24. Tshibangu, J.N., K. Chifundera, R. Kaminsky, A.D. Wright and G.M. Konig, 2002. Screening of African medicinal plants for antimicrobial and enzyme inhibitory activity. J. Ethnopharmacol., 80: 25-35. Recio, M.C., 1989. A review of some antimicrobial compounds isolated from medicinal plants reported in the literature 1978-1988. Phytother. Res., 3: 117-125. Cragg, G.M., D.J. Newman and K.M. Snader, 1997. Natural products in drug discovery and development. J. Nat. Prod., 60: 52-60. Raghavendra, M.P., S. Satish and K.A. Raveesha, 2006. Phytochemical analysis and antibacterial activity of Oxalis corniculata; a known medicinal plant. Myscience 1(1): 72-78. Gupta, V.P., Govindaiah and R.K. Datta, 1996. Plant extracts: a non-chemical approach to control Fusarium diseases of mulberry. Current Sci., 71: 406-409. Harborne, J.B., 1992. Phytochemical methods. Chapman and Hall publications, London, pp: 7-8. Satish, S., K.A. Raveesha and G.R. Janardhana, 1999. Antibacterial avtivity of plant extracts on phytopathogenic Xanthomonas compestris Pathovars. Letters in Applied Microbiology, 28: 145-147.
270
World Appl. Sci. J., 5 (3): 267-271, 2008
15. Munoz-Mingarro, D., N. Acero, F. Llinares, J.M. Pozuelo, A. Galan de and J.A. Mera Vicenten, 2003. Biological activity of extracts from Catalpa bignonioides Walt. (Bignoniaceae). J. Ethonopharmacol., 87: 163-167. 16. Coelho de Souza, G., A.P.S. Haas, G.L. Von Poser, E.E.S. Schapoval and E. Elisabetsky, 2004. Ethnopharmacological studies of antimicrobial remedies in the south of Brazil. J. Ethnopharmacol., 90: 135-43. 17. Nikaido, H., 1999. Microdermatology: Cell surface in the interaction of microbes with the external world. J. Bacteriol., 181: 4-8. 18. Adesokan, A.A., M.A. Akanji and M.T. Yakubu, 2007. Antibacterial potentials of aqueous extract of Enantia chlorantha stem bark African J. Biotechnol., 6(22): 2502-2505. 19. Britto, J.S., 2001. Comparative antibacterial activity study of Solanum incanum L. J. Swamy Bot. Club., 18: 81-82.
20. Krishna, K.T., C.E. Ranjini, V.K. Sasidharan, 1997. Antibacterial and antifungal activity of secondary metabolities from some medicinal and other common plant species. J. Life Sci., 2: 14-19. 21. Singh, I. and V.P. Singh, 2000. Antifungal properties of aqueous and organic solution extracts of seed plants against Aspergillus flavus and A. niger. Phytomorphol., 50: 151-157. 22. Natarajan, E., S. Senthilkumar, F.T. Xavier and V. Kalaiselvi, 2003. Antibacterial activities of leaf extracts of Alangium salviifolium. J. Trop. Med. Plants, 4: 9-13. 23. Natarajan, D., J.S. Britto, K. Srinivasan, N. Nagamurugan, C. Mohanasundari and G. Perumal, 2005. Anti-bacterial activity of Euphorbia fusiformis- a rare medicinal herb. J. Ethnopharmacol., 102: 123-126.
271
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Tyron Butson (Order #37627400)Dokument74 SeitenTyron Butson (Order #37627400)tyron100% (2)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- New Installation Procedures - 2Dokument156 SeitenNew Installation Procedures - 2w00kkk100% (2)
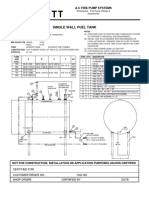
- Single Wall Fuel Tank: FP 2.7 A-C Fire Pump SystemsDokument1 SeiteSingle Wall Fuel Tank: FP 2.7 A-C Fire Pump Systemsricardo cardosoNoch keine Bewertungen
- Railway RRB Group D Book PDFDokument368 SeitenRailway RRB Group D Book PDFAshish mishraNoch keine Bewertungen
- QSK45 60 oil change intervalDokument35 SeitenQSK45 60 oil change intervalHingga Setiawan Bin SuhadiNoch keine Bewertungen
- 04 Dasmarinas Vs Reyes GR No 108229Dokument2 Seiten04 Dasmarinas Vs Reyes GR No 108229Victoria Melissa Cortejos PulidoNoch keine Bewertungen
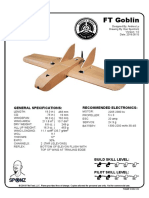
- FT Goblin Full SizeDokument7 SeitenFT Goblin Full SizeDeakon Frost100% (1)
- Leg Wri FInal ExamDokument15 SeitenLeg Wri FInal ExamGillian CalpitoNoch keine Bewertungen
- Welding MapDokument5 SeitenWelding MapDjuangNoch keine Bewertungen
- Quezon City Department of The Building OfficialDokument2 SeitenQuezon City Department of The Building OfficialBrightNotes86% (7)
- Server LogDokument5 SeitenServer LogVlad CiubotariuNoch keine Bewertungen
- Dissolved Oxygen Primary Prod Activity1Dokument7 SeitenDissolved Oxygen Primary Prod Activity1api-235617848Noch keine Bewertungen
- Analytical DataDokument176 SeitenAnalytical DataAsep KusnaliNoch keine Bewertungen
- Weka Tutorial 2Dokument50 SeitenWeka Tutorial 2Fikri FarisNoch keine Bewertungen
- Iitk Syllabus PDFDokument520 SeitenIitk Syllabus PDFcombatps1Noch keine Bewertungen
- SE Myth of SoftwareDokument3 SeitenSE Myth of SoftwarePrakash PaudelNoch keine Bewertungen
- Distribution of Laptop (Ha-Meem Textiles Zone)Dokument3 SeitenDistribution of Laptop (Ha-Meem Textiles Zone)Begum Nazmun Nahar Juthi MozumderNoch keine Bewertungen
- Proposal Semister ProjectDokument7 SeitenProposal Semister ProjectMuket AgmasNoch keine Bewertungen
- EWAIRDokument1 SeiteEWAIRKissy AndarzaNoch keine Bewertungen
- 3 Course Contents IIIBDokument5 Seiten3 Course Contents IIIBshahabNoch keine Bewertungen
- MATH2070 Computer Project: Organise Porject FoldDokument4 SeitenMATH2070 Computer Project: Organise Porject FoldAbdul Muqsait KenyeNoch keine Bewertungen
- Conplast SP430 0407Dokument4 SeitenConplast SP430 0407Harz IndNoch keine Bewertungen
- 3) Stages of Group Development - To StudsDokument15 Seiten3) Stages of Group Development - To StudsDhannesh SweetAngelNoch keine Bewertungen
- Ieee Research Papers On Software Testing PDFDokument5 SeitenIeee Research Papers On Software Testing PDFfvgjcq6a100% (1)
- Ten Golden Rules of LobbyingDokument1 SeiteTen Golden Rules of LobbyingChaibde DeNoch keine Bewertungen
- Siemens Documentation - Modeling ComponentsDokument1 SeiteSiemens Documentation - Modeling ComponentsanupNoch keine Bewertungen
- ABBBADokument151 SeitenABBBAJeremy MaraveNoch keine Bewertungen
- De Thi Chuyen Hai Duong 2014 2015 Tieng AnhDokument4 SeitenDe Thi Chuyen Hai Duong 2014 2015 Tieng AnhHuong NguyenNoch keine Bewertungen
- The Human Resource Department of GIK InstituteDokument1 SeiteThe Human Resource Department of GIK InstitutexandercageNoch keine Bewertungen
- Discretionary Lending Power Updated Sep 2012Dokument28 SeitenDiscretionary Lending Power Updated Sep 2012akranjan888Noch keine Bewertungen