Beruflich Dokumente
Kultur Dokumente
Case Study For Cast
Hochgeladen von
Maria JuvilisaOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Case Study For Cast
Hochgeladen von
Maria JuvilisaCopyright:
Verfügbare Formate
Introduction
An orthopedic cast, body cast or surgical cast, is a shell, frequently made from plaster,encasing a limb (or, in some cases, large portions of the body) to hold a broken bone (or bones)in place until healing is confirmed. It is similar in function to a splint.
An orthopedic cast is merely a cast made traditionally from cotton bandages soaked in plaster of Paris. In a few minutes the bandages harden, forming a protective layer around an injured area, usually a broken or badly sprained bone. Sometimes the bone is reset prior to placing anorthopedic cast. The casts function will then be to hold the bone in place to heal. The orthopedic cast has been used since the 1800s. During the Crimean War, other materials that would harden into a cast were used to set broken bones. The initial orthopedic cast was not always comfortable or helpful since plaster of Paris tends to expand as it dries. If inappropriately applied, it could create a cast so tight that blood circulation was cut off to the injured area. Although it rarely caused a tourniquet effect, it could delay healing instead of promoting it. Problems with the orthopedic cast made of plaster of Paris persisted even into its most modern forms. People with an orthopedic cast are susceptible to skin infections or irritations, and have limitations associated with wearing an orthopedic cast. For example, one cannot shower or bathe with this type of cast, and it is fairly heavy.
To address problems associated with the plaster orthopedic cast, most physicians switched tofiberglass casting instead. Fiberglass casting is notably lighter, and takes less time to apply. However, skin irritation can still occur, in fact more so with fiberglass. Further, fiberglass tends to provide a slightly less comfortable fitting cast. One can still request a plaster cast, which may be provided should the physician have materials available. There have been some improvements in the fiberglass orthopedic cast. A lining called PROCEL can make a fiberglass cast totally waterproof. This can be helpful for those who must be regularly exposed to water. It is a more expensive liner and not all insurances will cover the charge. Instead of using an orthopedic cast, sometimes a physician chooses to use a removable splint or brace for certain types of broken or injured bones. These have the advantage of allowing one to remove the brace for a quick shower, or to simply air the skin. Those with chronic skin conditions may prefer them, as it is possible to apply lotion or ointment to the skin prior to putting the brace back on.
Purposes of Cast:
Immobilization Prevention/Correction of deformity
3.
For support
4.
For elevation
5. Serves as a model for artificial leg
Having a cast for treatment of a broken bone can elicit different emotions. While some are excited to have a cast, this often quickly turns into annoyance with the realization that you may have to learn to do simple activities in a new way. Fortunately, you are not the first person to have a cast, and those before you have figured out tips and tricks to make having a cast not as difficult an experience
Personal profile
Name: Angelo Benjie Vibar Address: Blk 28 Lot 5 Golden Laguna Canlalay Binan Laguna Age: 25 Sex: Male Birthday: October 7, 1985 Birthplace: Laguna Nationality: Filipino Religion Catholic Civil Status: Single Date Admitted: August 28 2011 Time Admitted: 4am Present illness: Few hours PTC, Patient while allegedly driving motorcycle when he was hit by a tricycle causing him to be thrown off hitting ground with his left lower extremity first. There was reported extreme pain and was brought to our institution. Past medical history: (-) Hypertension (-) Diabetes mellitus (-) Allergy No kidney / liver disease
Anatomy and physiology
The arm has intermuscular septa, which are extensions of the deep fasica in between the muscles. These septa divide the arm into compartments and allow the muscles to freely slide over each other when they contract. The lower half of the arm is divided by these septa into anterior (front) and posterior (back) compartments. Humerus the Arm Bone The humerus is the bone in the arm region, the largest of the bones of the upper limb. It is a long bone located in the centre of the arm, completely surrounded by muscles. Its parts are a head, neck, body and a lower end. The head of the humerus is shaped like a hemisphere that fits into the shallow glenoid cavity of the scapula (the shoulder blade) to form the shoulder joint. The body is a long and sturdy shaft that gives attachment to some of the muscles of the arm. The lower end bears prominent bony projections called epicondyles on either side. The lower end connects with the radius and the ulna, bones of the forearm, to form the elbow joint. Radius The radius is the bone of the forearm or lower arm, extending from the elbow to the wrist. This bone is relatively long and curved, extending parallel to the ulna. Like the humerus, the radius primary function includes motion of the arm and support of the arm. The radius connects to many muscles, such as the biceps, supinator, flexor digitorum superficialis, flexor pollicis longus muscles, extensor ossis metacarpi pollicis, extensor primi internodii pollicis, and the pronator teres muscles. Furthermore, the radius is found on each arm thus contributing a total of two bones to the human body skeleton. Ulna The ulna is the third and final bone of the arm. This bone runs parallel to the radius from the elbow to the wrist. Like the other arm bones, the ulna is relatively long and slightly curved. The primary function of the ulna is allowing motion and supporting the arm. An ulna exists on each arm and thus contributes two bones to the total human body skeleton. The ulna is also the site of attachment for many muscles and ligaments. Examples of muscles attaching to the ulna include the triceps brachii muscle, supinator muscle, pronator teres muscle, pronator quadratus muscle, and the flexor digitorum superficialis muscle. Anatomy of Arm Muscles While the upper part of the arm is wrapped by some of the shoulder muscles like the deltoid, the muscles that actually occupy the arm are: biceps brachii coracobrachialis brachialis triceps brachii The first three muscles occupy the front of the arm while the triceps forms the bulk of the back of the arm. While the biceps and coracobrachialis cause flexion at the shoulder joint, the triceps cause extension at the elbow. Read all about arm muscle anatomy for details about the origin and insertion, nerve supply and actions of each of these muscles.
Anatomy of Arm Nerves
The entire upper limb is supplied by nerves arising from the brachial plexus, a major nerve network formed by the cervical and first thoracic spinal nerves. Many important nerves run through the arm, some of them to supply the structures of the arm and others on their way to the forearm and hand. The nerves present in the arm. radial nerve median nerve ulnar nerve musculocutaneous nerve The musculocutaneous nerve comes from the lateral cord of the brachial plexus. After supplying the biceps, coracobrachialis and brachialis muscles of the arm, it ends up as the lateral cutaneous nerve of the forearm, the nerve for sensation of part of the forearm skin. The radial nerve arises from the posterior cord of the brachial plexus and supplies the triceps muscle in the arm before heading towards the hand. The ulnar nerve only passes through the arm and does not control any structure here. The median nerve, too, mainly supplies the muscles in the palm and fingers, but gives off branches to the arteries in the arm. Read brachial plexus anatomy for complete details about how this nerve network is formed and what nerves arise from it. Anatomy of Arm Veins and Arteries The major blood vessel in the arm is the brachial artery. This vessel is a continuation of the axillary artery and carries nutrition to all the structures in the arm through its branches. You can feel its pulsation in front of the elbow just beside the biceps tendon. In fact, it is the pulsation of this artery that is used while measuring blood pressure with a sphygmomanometer and this is why the nurse places the stethoscope on the front of the elbow. The branches of the brachial artery in the arm are: profunda brachii that runs along with the radial nerve ulnar collateral artery there are 2, the superior and inferior, supplying the arm muscles nutrient artery to the humerus supplying the arm bone There are veins accompanying every artery, for example, the brachial artery and the brachial vein, but the arrangement of veins can vary widely. The main veins in the arm are: basilic vein cephalic vein The basilic vein runs along the inner side while the cephalic vein is located along the outer edge, especially at the front of the elbow. The two veins are often connected by the median cubital vein in front of the elbow. Both these veins, along with the brachial vein, empty into the axillary vein. Arm anatomy is an important part of upper limb anatomy and includes the arm bone humerus, arm muscles, nerves of the arm, veins and arteries. http://lakshmiananth.suite101.com/arm-anatomy-anatomy-of-arm-muscles-bone-arm-nerves-arm-veins-a344028
Bones and Joints
There are 15 bones that form connections from the end of the forearm to the hand. The wrist itself contains eight small bones, called carpal bones. These bones are grouped in two rows across the wrist. The proximal row is where the wrist creases when you bend it. Beginning with the thumb-side of the wrist, the proximal row of carpal bones is made up of the scaphoid,lunate, and triquetrum. The second row of carpal bones, called the distal row, meets the proximal row a little further toward the fingers. The distal row is made up of the trapezium, trapezoid, capitate, hamate, and pisiform bones.
The proximal row of carpal bones connects the two bones of the forearm, the radius and the ulna, to the bones of the hand. The bones of the hand are called the metacarpal bones. These are the long bones that lie within the palm of the hand. The metacarpals attach to the phalanges, which are the bones in the fingers and thumb. One reason that the wrist is so complicated is because every small carpal bone forms a joint with the bone next to it. This means that what we call the wrist joint is actually made up of many small joints. Articular cartilage is the material that covers the ends of the bones of any joint. Articular cartilage can be up to onequarter of an inch thick in the large, weight-bearing joints. It is thinner in joints such as the wrist that don't support a lot of weight. Articular cartilage is white, shiny, and has a rubbery consistency. It is slippery, which allows the joint surfaces to slide against one another without causing any damage. The function of articular cartilage is to absorb shock and provide an extremely smooth surface to make motion easier. We have articular cartilage essentially everywhere that two bony surfaces move against one another, or articulate. In the wrist, articular cartilage covers the sides of all the carpals and the ends of the bones that connect from the forearm to the fingers.
Ligaments and Tendons Ligaments are soft tissue structures that connect bones to bones. The ligaments around a joint usually combine to form a <="" em="">. A joint capsule is a watertight sac that surrounds a joint and contains lubricating fluid calledsynovial fluid. In the wrist, the eight carpal bones are surrounded and supported by a joint capsule. Two important ligaments support the sides of the wrist. These are thecollateral ligaments. There are two collateral ligaments that connect the forearm to the wrist, one on each side of the wrist. As its name suggests, the ulnar collateral ligament (UCL) is on the ulnar side of the wrist. It crosses the ulnar edge (the side away from the thumb) of the wrist. It starts at the ulnar styloid, the small bump on the edge of the wrist (on the side away from the thumb) where the ulna meets the wrist joint. There are two parts to the cord-shaped UCL. One part connects to the pisiform (one of the small carpal bones) and to the transverse carpal ligament, a thick band of tissue that crosses in front of the wrist. The other goes to the triquetrum (a small carpal bone near the ulnar side of the wrist). The UCL adds support to a small disc of cartilage where the ulna meets the wrist. This structure is called thetriangular fibrocartilage complex (TFCC) and is discussed in more detail below. The UCL stabilizes the TFCC and keeps the wrist from bending too far to the side (toward the thumb). The radial collateral ligament (RCL) is on the thumb side of the wrist. It starts on the outer edge of the radius on a small bump called the radial styloid. It connects to the side of the scaphoid, the carpal bone below the thumb. The RCL prevents the wrist from bending too far to the side (away from the thumb). Just as there are many bones that form the wrist, there are many ligaments that connect to and support these bones. Injury or problems that cause these ligaments to stretch or tear can eventually lead to arthritis in the wrist. At the wrist, the end of the ulna bone of the forearm articulates with two carpal bones, the lunate and the triquetrum. A unique structure mentioned earlier, the triangular fibrocartilage complex (TFCC), sits between the ulna and these two carpal bones. The TFCC is a small cartilage pad that cushions this part of the wrist joint. It also improves the range of motion and gliding action within the wrist joint. There are several important tendons that cross the wrist. Tendons connect muscles to bone. The tendons that cross the wrist begin as muscles that start in the forearm. Those that cross the palm side of the wrist are theflexor tendons. They curl the fingers and thumb, and they bend the wrist. The flexor tendons run beneath the transverse carpal
ligament (mentioned earlier). This structure lies on the palm side of the wrist. This band of tissue keeps the flexor tendons from bowing outward when you curl your fingers, thumb, or wrist. The tendons that travel over the back of the wrist, the extensor tendons, run through a series of tunnels, called compartments. These compartments are lined with a slick substance called tenosynovium, which prevents friction as the extensor tendons glide inside their compartment.
Anatomy of Legs
The major (long) bones of the human leg are the femur (thighbone), tibia (shinbone), and fibula (the smaller, rear calf bone). Thepatella (kneecap) is the bone in front of the knee. Most of the leg skeleton has bony prominences and margins that can bepalpated, notable exceptions being the hip joint, and the neck and shaft of femur. Many of these anatomical landmarks are used to define the extent of the leg: most notably the anterior superior iliac spine, the greater trochanter, the superior margin of the medial condyle of tibia, and the medial malleolus.In the normal case, the large joints of the lower limb are aligned on a straight line which represents the mechanical longitudinal axis of the leg, the Mikulicz line. This line stretches from the hip joint (or more precisely the head of the femur), through the knee joint (the intercondylar eminence of the tibia), and down to the center of the ankle (the ankle mortise, the fork-like grip between the medial and lateral malleoli). In the tibial shaft, the mechanical and anatomical axes coincide, but in thefemoral shaft they diverge 6, resulting in the femorotibial angle of 174 in a leg with normal axial
alignment. A leg is considered straight when, with the feet brought together, both the medial malleoli of the ankle and the medial condyles of the knee are touching. Divergence from the normal femorotibial angle is called genu varumif the center of the knee joint is lateral to the mechanical axis (intermalleolar distance exceeds 3 cm), and genu valgum if it is medial to the mechanical axis (intercondylar distance exceeds 5 cm). These conditions impose unbalanced loads on the joints and stretching of either the thigh's adductors and abductors. The angle of inclination formed between the neck and shaft of the femur, the collodiaphysial angle, varies with age about 150 in the newborn, it gradually decreases to 126-128 in adults, to reach 120 in old age. Pathological changes in this angle results in abnormal posture of the leg: A small angle produces coxa vara and a large angle in coxa valga; the latter is usually combined with genu varum and coxa vara leads genu valgum. Additionally, a line drawn through the femoral neck superimposed on a line drawn through the femoral condyles forms an angle, the torsion angle, which makes it possible for flexion movements of the hip joint to be transposed into rotary movements of the femoral head. Abnormally increased torsion angles results in a limb turned inward and a decreased angle in a limb turned outward; both cases resulting in a reduced range of mobility. Thigh The muscles of the thigh can be classified into three groups according to their location: anterior and posterior muscles and the adductors (on the medial side). All adductors (see above) except gracilis insert on the femur and therefore act only on the hip joint. The majority of the thigh muscles, the "true" thigh muscles, are insert on the leg (either the tibia or the fibula) and thus act primarily on the knee joint. Functionally, the extensors lie anteriorly on the thigh and are distinguished from flexors on the posterior side. Even though the sartorius flexes the knee, it is ontogenetically considered an extensor since its displacement is secondarily.Most of the adductors act exclusively on the hip joint, so functionally they qualify as hip muscles. Of the anterior thigh muscles the largest are the four muscles of the quadriceps femoris. The central rectus femoris which is surrounded by the three vasti: The vastus intermedius, medialis, and lateralis. Rectus femoris is attached to the pelvis with two tendons, while the vasti are inserted to the femur. All four muscles unite in a common tendon inserted into the patella from where thepatellar ligament extends it down to the tibial tuberosity. Fibers from the medial and lateral vasti form two retinacula that stretch past the patella on either sides down to the condyles of the tibia. The quadriceps is the knee extensor, but the rectus femoris additionally flexes the hip joint, and articular muscle of the knee protects the articular capsule of the knee joint from being nipped during extension. Thesartorius runs superficially and obliquely down on the anterior side of the thigh, from the anterior superior iliac spine to the pes anserinus on the medial side of the knee, from where it is further extended into the crural fascia. The sartorius acts as a flexor on both the hip and knee, but, due to its oblique course, also contributes to medial rotation of the leg as one of the pes anserinus muscles (with the knee flexed), and to lateral rotation of the hip joint. There are four posterior thigh muscles. The biceps femoris has two heads: The long head has its origin on the ischial tuberositytogether with the semitendinosus and acts on two joints. The short head originates from the middle third of the linea aspera on the shaft of the femur and the lateral intermuscular septum of thigh, and acts on only one joint. These two heads unite to form the biceps which inserts on the head of the fibula. The biceps flexes the knee joint and rotates the flexed leg laterally it is the only lateral rotator of the knee and thus has to oppose all medial rotator. Additionally, the long head extends the hip joint. The semitendiosus and the semimembranosus share their origin with the long head of the biceps, and both attaches on the medial side of the proximal head of the tibia together with the gracilis and sartorius to form the pes anserinus. The semitendinosus acts on two joints; extension of the hip, flexion of the knee, and medial rotation of the leg. Distally, the semimembranosus' tendon is divided into three parts referred to as the pes anserinus profondus. Functionally, the semimembranosus is similar to the semitendinosus, and thus produces extension at the hip joint and flexion and medial rotation at the knee. Posteriorly below the knee joint, the popliteus stretches obliquely from thelateral femoral epicondyle down to the posterior surface of the tibia. The subpopliteal bursa is located deep to the muscle. Popliteus flexes the knee joint and medially rotates the leg.
Foot
With the popliteus (see above) as the single exception, all muscles in the leg are attached to the foot and, based on location, can be classified into an anterior and a posterior group separated from each others by the tibia, the fibula, and the interosseous membrane. In turn, these two groups can be subdivided into subgroups or layers the anterior group consists of the extensors and the peroneals, and the posterior group of a superficial and a deep layer. Functionally, the muscles of the leg are either extensors, responsible for the dorsiflexion of the foot, or flexors, responsible for the plantar flexion. These muscles can also classified by innervation, muscles supplied by the anterior subdivision of the plexus and those supplied by the posterior subdivision. The leg muscles acting on the foot are called theextrinsic foot muscles whilst the foot muscles located in the foot are called intrinsic. Dorsiflexion (extension) and plantar flexion occur around the transverse axis running through the ankle joint from the tip of the medial malleolus to the tip of the lateral malleolus. Pronation (eversion) and supination (inversion) occur along the oblique axis of the ankle joint.
Extrinsic Three of the anterior muscles are extensors. From its origin on the lateral surface of the tibia and the interosseus mebrane, the three-sided belly of the tibialis anterior extends down below the superior and inferior extensor retinacula to its insertion on the plantar side of the medial cuneiform bone and the fifth metatarsal bone. In the non-weight-bearing leg, the anterior tibialis dorsal flexes the foot and lifts the medial edge of the foot. In the weight-bearing leg, it pulls the leg towards the foot. The extensor digitorum longus has a wide origin stretching from the lateral condyle of the tibia down along the anterior side of the fibula, and the interosseus membrane. At the ankle, the tendon divides into four that stretch across the foot to the dorsal aponeuroses of the last phalanges of the four lateral toes. In the non-weight-bearing leg, the muscle dorsiflexes the digits and the foot, and in the weight-bearing leg acts similar to the tibialis anterior. The extensor hallucis longus has its origin on the fibula and the interosseus membrane between the two other extensors and is, similarly to the extensor digitorum, is inserted on the last phalanx of big toe ("hallux"). The muscle dorsiflexes the hallux, and acts similar to the tibialis anterior in the weight-bearing leg. Two muscles on the lateral side of the leg form the peroneal group. The peroneus longus and brevis both have their origins on the fibula and they both pass behind the lateral malleolus where their tendons pass under the peroneal retinacula. Under the foot, the longus stretches from the lateral to the medial side in a groove, thus bracing the transverse arch of the foot. The brevis is attached on the lateral side to the tuberosity of the fifth metatarsal. Together the two peroneals form the strongest pronators of the foot. The peroneus muscles are highly variable and several variants can occasionally be present. Of the posterior muscles three are in the superficial layer. The major plantar flexors, commonly referred to as the triceps surae, are the soleus, which arises on the proximal side of both leg bones, and the gastrocnemius, the two heads of which arises on the distal end of the femur. These muscles unite in a large terminal tendon, the Achilles tendon, which is attached to the posterior tubercle of thecalcaneus. The plantaris closely follows the lateral head of the gastrocnemius. Its tendon runs between those of the soleus and gastrocnemius and is embedded in the medial end of the calcaneus tendon. In the deep layer, the tibialis posterior has its origin on the interosseus membrane and the neighbouring bone areas and runs down behind the medial malleolus. Under the foot it splits into a thick medial part attached to the navicular bone and a slightly weaker lateral part inserted to the three cuneiform bones. The muscle produces simultaneous plantar flexion and supination in the non-weight-bearing leg, and approximates the heel to the calf of the leg. The flexor hallucis longus arises distally on the fibula and on the interosseus membrane from where its relatively thick muscle belly extends far distally. Its tendon extends beneath the flexor retinaculum to the sole of the foot and finally attaches on the base of the last phalanx of the hallux. It plantarflexes the hallux and assists in supination. The flexor digitorum longus, finally, has its origin on the upper part of the tibia. Its tendon runs to the sole of the foot where it forks into four terminal tendon attached to the last phalanges of the four lateral toes. It crosses the tendon of the tibialis posterior distally on the tibia, and the tendon of the flexor hallucis longus in the sole. Distally to its division, the quadratus plantae radiates into it and near the middle phalanges its tendons penetrate the tendons of the flexor digitorum brevis. In the non-weight-bearing leg, it plantar flexes the toes and foot and supinates. In the weight-bearing leg it supports the plantar arch.[21] (For the popliteus, see above.) Intrinsic The intrinsic muscles of the foot, muscles whose bellies are located in the foot proper, are either dorsal (top) or plantar (sole). On the dorsal side, two long extrinsic extensor muscles are superficial to the intrinsic muscles, and
their tendons form the dorsal aponeurosis of the toes. The short intrinsic extensors and the plantar and dorsal interossei radiates into these aponeuroses. The extensor digitorum brevis and extensor hallucis brevis have a common origin on the anterior side of the calcaneus, from where their tendons extend into the dorsal aponeuroses of digits 1-4. They act to dorsiflex these digits. The plantar muscles can be subdivided into three groups associated with three regions: those of the big digit, the little digit, and the region between these two. All these muscles are covered by the thick and dense plantar aponeurosis, which, together with two tough septa, form the spaces of the three groups. These muscles and their fatty tissue function as cushions that transmit the weight of the body downward. As a whole, the foot is a functional entity The abductor hallucis stretches along the medial edge of the foot, from the calcaneus to the base of the first phalanx of the first digit and the medial sesamoid bone. It is an abductor and a week flexor, and also helps maintain the arch of the foot. Lateral to the abductor hallucis is the flexor hallucis brevis, which originates from the medial cuneiform bone and from the tendon of the tibialis posterior. The flexor hallucis has a medial and a lateral head inserted laterally to the abductor hallucis. It is an important plantar flexor which comes into prominent use in classical ballet (i.e. for pointe work). The adductor hallucis has two heads; a stronger oblique head which arises from the cuboid and lateral cuneiform bones and the bases of the second and third metatarsals; and a transverse head which arises from the distal ends of the third-fifth metatarsals. Both heads are inserted on the lateral sesamoid bone of the first digit. The muscle acts as a tensor to the arches of the foot, but can also adduct the first digit and plantar flex its first phalanx. The opponens digiti minimi originates from the long plantar ligament and the plantar tendinous sheath of peroneus longus and is inserted on the fifth metatarsal. When present, it acts to plantar flex the fifth digit and supports the plantar arch. The flexor digiti minimi arises from the region of base of the fifth metatarsal and is inserted onto the base of the first phalanx of the fifth digit where it is usually merged with the abductor of the first digit. It acts to plantar flex the last digit. The largest and longest muscles of the little toe is the abductor digiti minimi. Stretching from the lateral process of the calcaneus, with a second attachment on the base of the fifth metatarsal, to the base of the fifth digit's first phalanx, the muscle forms the lateral edge of the sole. Except for supporting the arch, it plantar flexes the little toe and also acts as an abductor. The four lumbricales have their origin on the tendons of the flexor digitorum longus, from where they extend to the medial side of the bases of the first phalanx of digits two-five. Except for reinforcing the plantar arch, they contribute to plantar flexion and move the four digits toward the big toe. They are, in contrast to the lumbricales of the hand, rather variable, sometimes absent and sometimes more than four are present. The quadratus plantae arises with two slips from margins of the plantar surface of the calcaneus and is inserted into the tendon(s) of the flexor digitorum longus, and is known as the "plantar head" of this latter muscle. The three plantar interossei arise with their single heads on the medial side of the third-fifth metatarsals and are inserted on the bases of the first phalanges of these digits. The two heads of the four dorsal interossei arise on two adjacent metatarsals and merge in the intermediary spaces. Their distal attachment is on the bases of the proximal phalanges of the second-fourth digits. The interossei are organized with the second digit as a longitudinal axis; the plantars act as adductors and pull digits 3-5 towards the second digit; while the dorsals act as abductors. Additionally, the interossei act as plantar flexors at the metatarsophalangeal joints. Lastly, the flexor digitorum brevis arises from underneath the calcaneus to insert its tendons on the middle phalanges of digit 2-4. Because the tendons of the flexor digitorum longus run between these tendons, the brevis is sometimes called perforatus. The tendons of these two muscles are surrounded by a tendinous sheath. The brevis acts to plantar flex the middle phalanges. Pathophysiology Nursing care plan Assessme Diagnosis nt Impaired
Scientific Explaination A limitation in
Planning
Intervention Independent:
Rationale
Evaluati on
Physical Mobility related to pain/discomf ort
Independent, purposeful physical movement of the body or of one or more extremities. Physical agent Causedfracture bydamaging thetissue andbone of theleft leg fibula Lead toexperienceseverepain/dis comfort Resulted toimpairment of movement
Help client achieve mobility and start walking as soon as possible if not contraindic ated
> The longer a client is immobile , the longer it takes to regain strength ,balance, and coordinat ion >Techniqu es such as gait training, strength training, exercise to improve balance and coordinat ion can be very helpful to rehabilita te client.
Consult with Physical therapy for further evaluation, strength raining, gait training, and development of a mobility plan
Das könnte Ihnen auch gefallen
- The Sensitive Gut Harvard HealthDokument57 SeitenThe Sensitive Gut Harvard HealthDayhanna Guzman100% (7)
- The Goldfish and Its Culture. Mulertt PDFDokument190 SeitenThe Goldfish and Its Culture. Mulertt PDFjr2010peruNoch keine Bewertungen
- 3rd Lecture Morphological Changes During Maturation o Te GameteaDokument25 Seiten3rd Lecture Morphological Changes During Maturation o Te GameteaHussein Al Saedi100% (1)
- 411 419Dokument9 Seiten411 419Afif MansorNoch keine Bewertungen
- Phalanx FractureDokument46 SeitenPhalanx FractureBagas WidhiarsoNoch keine Bewertungen
- Administering Ear DropDokument2 SeitenAdministering Ear DropJenny WongNoch keine Bewertungen
- Epidemiology: Phalanges and Interphalangeal JointsDokument4 SeitenEpidemiology: Phalanges and Interphalangeal JointsHafidah RakhmatinaNoch keine Bewertungen
- BSC - 2019 - 1 - Anatomy and Physiology PDFDokument1 SeiteBSC - 2019 - 1 - Anatomy and Physiology PDFBasava VillanNoch keine Bewertungen
- The Integumentary System - The Dermis: T. RickDokument17 SeitenThe Integumentary System - The Dermis: T. Rickapi-464344582Noch keine Bewertungen
- Fracture Treatment ProtocolsDokument14 SeitenFracture Treatment ProtocolsZikrul IdyaNoch keine Bewertungen
- You Are HereDokument8 SeitenYou Are HeremthanushriNoch keine Bewertungen
- Lab 7 - The Axial and Appendicular SkeletonDokument5 SeitenLab 7 - The Axial and Appendicular Skeletonsidro123100% (3)
- Human Anatomy and Physiology: Clarito F. Concepcion Associate Professor 5 CSM, WmsuDokument48 SeitenHuman Anatomy and Physiology: Clarito F. Concepcion Associate Professor 5 CSM, WmsuScar Shadow100% (1)
- Lab 7 - Sensory SystemDokument46 SeitenLab 7 - Sensory SystemNatalie Pemberton100% (1)
- Connective TissueDokument7 SeitenConnective TissueRoy Michael Trinidad0% (1)
- The Muscular System Learning Enhancement Activity LectureDokument6 SeitenThe Muscular System Learning Enhancement Activity LectureNathaniel CornistaNoch keine Bewertungen
- Reviewer Skeletal To EndoDokument46 SeitenReviewer Skeletal To EndoSophia CaisipNoch keine Bewertungen
- Chap 18Dokument84 SeitenChap 18Virgil AnmaNoch keine Bewertungen
- Ana Phisio Lab Report.Dokument4 SeitenAna Phisio Lab Report.Diana Amor100% (1)
- AnaPhy Lesson 6 Muscular SYstemDokument7 SeitenAnaPhy Lesson 6 Muscular SYstemLM KishimotoNoch keine Bewertungen
- Musculoskeletal Anatomy and Physiology 5Dokument36 SeitenMusculoskeletal Anatomy and Physiology 5Dennis Nabor Muñoz, RN,RMNoch keine Bewertungen
- Integumentary System: Functions of SkinDokument7 SeitenIntegumentary System: Functions of SkinSoniyaJI84Noch keine Bewertungen
- Blood Anatomy and Physiology ReviewDokument20 SeitenBlood Anatomy and Physiology ReviewStacey CamilleNoch keine Bewertungen
- Musculo Care Modalities 2 PDFDokument44 SeitenMusculo Care Modalities 2 PDFAhmad FaujiNoch keine Bewertungen
- GastrointestinalDokument39 SeitenGastrointestinalالمسوول الاعلاميNoch keine Bewertungen
- Medical Terminology of Anatomical Positions - FK Undana Lsit 2016Dokument127 SeitenMedical Terminology of Anatomical Positions - FK Undana Lsit 2016Maria JozilynNoch keine Bewertungen
- Abdominal Wall Learning ObjectivesDokument7 SeitenAbdominal Wall Learning ObjectivesMadison KommorNoch keine Bewertungen
- Central Nervous SystemDokument30 SeitenCentral Nervous SystemJames Lacuesta Tabiolo100% (1)
- Urinary System Disorders Practice Quiz #1 (50 Questions)Dokument26 SeitenUrinary System Disorders Practice Quiz #1 (50 Questions)Emy TandinganNoch keine Bewertungen
- 1.1 Cell PhysiologyDokument47 Seiten1.1 Cell PhysiologyGiftNoch keine Bewertungen
- Laboratory ActivityDokument15 SeitenLaboratory ActivityChippy RabeNoch keine Bewertungen
- Introduction in Human Anatomy and PhysiologyDokument35 SeitenIntroduction in Human Anatomy and Physiologyraul nino MoranNoch keine Bewertungen
- Laboratory Activity No. 9: The Frog Respiratory SystemDokument4 SeitenLaboratory Activity No. 9: The Frog Respiratory SystemMaricris GuillermoNoch keine Bewertungen
- Pulmonary CirculationDokument16 SeitenPulmonary Circulationsajid_saiyad0% (1)
- Case Study Final FractureDokument27 SeitenCase Study Final Fracture3amabelle arevaloNoch keine Bewertungen
- Anatomy and Physiology Lab Activity 9Dokument4 SeitenAnatomy and Physiology Lab Activity 9Kylene Gayle MoralesNoch keine Bewertungen
- Theoretical Foundation of Nursing - Florence NightingaleDokument9 SeitenTheoretical Foundation of Nursing - Florence NightingaleAshley Nicole BeltranNoch keine Bewertungen
- Digestive SystemDokument41 SeitenDigestive SystemRotsen B. VelascoNoch keine Bewertungen
- D.muscular System PDFDokument8 SeitenD.muscular System PDFJohn Lawrence YbanezNoch keine Bewertungen
- Anaphy Prelims ReviewerDokument11 SeitenAnaphy Prelims ReviewerMariz Elizabeth TaytayNoch keine Bewertungen
- Frog Circulatory SystemDokument43 SeitenFrog Circulatory Systembawcock100% (5)
- Lymph SystemDokument7 SeitenLymph SystemghaiathNoch keine Bewertungen
- Assessment of AbdomenDokument99 SeitenAssessment of AbdomenKeid ReumaNoch keine Bewertungen
- Lab 1 - Asepsis and Infection Control QuestionsDokument3 SeitenLab 1 - Asepsis and Infection Control QuestionsmlomiguenNoch keine Bewertungen
- Lesson Plan Chapter OneDokument4 SeitenLesson Plan Chapter Oneapi-378592385Noch keine Bewertungen
- Animal Tissues: Epithelial TissueDokument19 SeitenAnimal Tissues: Epithelial TissueJnana YumnaNoch keine Bewertungen
- Pediatric Case StudyDokument21 SeitenPediatric Case StudyJobelle AcenaNoch keine Bewertungen
- 2.1 (B) - Role of Muscles, Ligaments & Tendons inDokument19 Seiten2.1 (B) - Role of Muscles, Ligaments & Tendons inliefeng81100% (1)
- Anatomy & Physiology - AllDokument15 SeitenAnatomy & Physiology - AllAnubhav ShuklaNoch keine Bewertungen
- Anatomy Reviewer Nervous SystemDokument4 SeitenAnatomy Reviewer Nervous SystemCristinNoch keine Bewertungen
- Human Anatomy and Physiology I Laboratory: Gross Anatomy of The Muscular SystemDokument39 SeitenHuman Anatomy and Physiology I Laboratory: Gross Anatomy of The Muscular SystemAnomalie12345Noch keine Bewertungen
- Anatomy and Physiology of BVDokument16 SeitenAnatomy and Physiology of BVMarivic DianoNoch keine Bewertungen
- Anatomy Physiology Syllabus 2016 UpdatedDokument5 SeitenAnatomy Physiology Syllabus 2016 Updateddats_idjiNoch keine Bewertungen
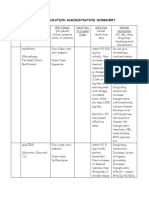
- Medication Administration WorksheetDokument6 SeitenMedication Administration WorksheetCheska CarrionNoch keine Bewertungen
- Osteomyelitis 130708212636 Phpapp01Dokument107 SeitenOsteomyelitis 130708212636 Phpapp01merikasorNoch keine Bewertungen
- EpitheliumDokument48 SeitenEpitheliumdrpankaj28100% (1)
- Cardiovascular System: K. Hariharan Iv Eee - 'B'Dokument33 SeitenCardiovascular System: K. Hariharan Iv Eee - 'B'Hari Haran100% (1)
- Spinal Cord and Spinal NervesDokument46 SeitenSpinal Cord and Spinal Nerveskombat13_708353334Noch keine Bewertungen
- Quiz Urinary Reproductive 20Dokument5 SeitenQuiz Urinary Reproductive 20estherNoch keine Bewertungen
- BSCI 1824 Anatomy and Physiology - Syllabus - 2020-2021Dokument16 SeitenBSCI 1824 Anatomy and Physiology - Syllabus - 2020-2021glennNoch keine Bewertungen
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- Hip AnatomyDokument8 SeitenHip AnatomyRusu AdrianNoch keine Bewertungen
- Shoulder AnatomyDokument150 SeitenShoulder Anatomysrinidhi2011Noch keine Bewertungen
- Chapter: Breathing and Exchange of Gases: BIOLOGY - AssignmentDokument9 SeitenChapter: Breathing and Exchange of Gases: BIOLOGY - Assignmentyogesh ahireNoch keine Bewertungen
- Digestive SystemDokument41 SeitenDigestive SystemRotsen B. VelascoNoch keine Bewertungen
- ArenavirusDokument29 SeitenArenavirusRamirez GiovarNoch keine Bewertungen
- 2804 Central Concepts January 2006 Mark SchemeDokument0 Seiten2804 Central Concepts January 2006 Mark SchemeWK SoohgNoch keine Bewertungen
- The 5 Hidden: Libido KillersDokument6 SeitenThe 5 Hidden: Libido KillersscribduserNoch keine Bewertungen
- Sanum Therapy Book Helios PDFDokument314 SeitenSanum Therapy Book Helios PDFOscarNoch keine Bewertungen
- The Nervous System, NotesDokument6 SeitenThe Nervous System, NotesnadshinkNoch keine Bewertungen
- Jurnal 4Dokument5 SeitenJurnal 4Nindita RahmaNoch keine Bewertungen
- Chapter 38 Animal DevelopmentDokument77 SeitenChapter 38 Animal Developmentmaria banunaekNoch keine Bewertungen
- Maternal QuestionsDokument7 SeitenMaternal Questionsjhae_darilayNoch keine Bewertungen
- TrapsDokument4 SeitenTrapsPatricia BrownNoch keine Bewertungen
- Farmakodinamik Nsaid 2018Dokument57 SeitenFarmakodinamik Nsaid 2018kiki rawitriNoch keine Bewertungen
- Ped Gi Handbook NaspghanDokument62 SeitenPed Gi Handbook NaspghanFernando Camara100% (1)
- Acupuncture ChartsDokument7 SeitenAcupuncture Chartsdoringrama50% (2)
- Poecilia Reticulata Domestic Breeder Tra PDFDokument18 SeitenPoecilia Reticulata Domestic Breeder Tra PDFAdrian BercanNoch keine Bewertungen
- Metodo, Entrenamiento y Principios Del ADVIA 120Dokument64 SeitenMetodo, Entrenamiento y Principios Del ADVIA 120Jaime Elias100% (3)
- 5 6057344157398073400Dokument69 Seiten5 6057344157398073400Desmiyati AdoeNoch keine Bewertungen
- Artritis Gout in Aviation MedicineDokument22 SeitenArtritis Gout in Aviation MedicineBuyungNoch keine Bewertungen
- Keyword Ideas On Hair Loss For SEODokument18 SeitenKeyword Ideas On Hair Loss For SEOChitrakarudu KalabhimaniNoch keine Bewertungen
- Neck TrianglesDokument6 SeitenNeck TrianglesJay-arh SebusaNoch keine Bewertungen
- A&P Principles of Microbiology and Human Disease (Nursing) - PowerPointDokument47 SeitenA&P Principles of Microbiology and Human Disease (Nursing) - PowerPointLinsey Bowen100% (2)
- Administering EnemaDokument35 SeitenAdministering Enemabajaoc100% (1)
- Rabies SeminarDokument73 SeitenRabies SeminarQazi Muhammad IqbalNoch keine Bewertungen
- Peter Singer Science and FreedomDokument13 SeitenPeter Singer Science and FreedomMariusz PopieluchNoch keine Bewertungen
- MannitolDokument2 SeitenMannitolJen Recto Palad86% (7)
- CR DR - Dedi Hidropneumothorax Ec TB ParuDokument38 SeitenCR DR - Dedi Hidropneumothorax Ec TB ParuBunga Listia ParamitaNoch keine Bewertungen
- Anatomy of Male Reproductive OrgansDokument18 SeitenAnatomy of Male Reproductive OrgansPutri HolmesNoch keine Bewertungen