Beruflich Dokumente
Kultur Dokumente
Blood Vessels
Hochgeladen von
Mark DukshteinOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Blood Vessels
Hochgeladen von
Mark DukshteinCopyright:
Verfügbare Formate
1. Arteriosclerosis hard arteries, due to thickening a.
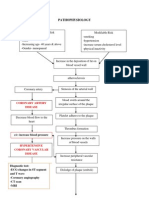
Atherosclerosis intimal plaque that obstructs blood flow; consists of a necrotic lipid core (cholesterol) with a fibromuscular cap i. Often undergoes dystrophic calcification in the wall of muscular arteries (i.e uterine and radial arteries) ii. Endothelial cell damage of muscular and elastic arteries (large and medium sized) iii. MCL: abdominal aorta > coronary artery > popliteal artery > internal carotid artery iv. Risk factors 1. Hypertension, hypercholesterolemia (LDL bad, HDL good), smoking, and diabetes 2. Age, gender, and genetics v. Cell response to endothelial injury 1. Hyperplasia of medial smooth muscle cells 2. Damage to endothelium allows lipids to leak into the intima (mainly cholesterol) 3. Lipids are oxidized and then consumed by macrophages resulting in foam cells 4. Inflammation and healing leads to deposition of ECM and proliferation of SMC vi. Progression 1. Endothelial Cell dysfunction macrophage and LDL accum foam cell fatty streaks SMC migration (involves PDGF and TGF-B) fibrous plaque atheromas 2. Fibrous plaque becomes dystropically calcified and ulcerated 3. Disrupted plaques may extrude underlying necrotic material leading to vessel thrombosis a. Marker = C-reactive protein
vii. Complications 1. Stenosis of medium vessels impaired blood flow and ischemia leading to: a. Peripheral vascular disease (lower extremity artery popliteal); increased risk of gangrene i. Pain in the butt and when walking (claudication) b. Angina acute MI coronary artery c. Vessel thrombosis i. Acute MI coronary artery ii. Stroke internal carotid artery, MCA iii. Ischemic bowel disease sup. mesenteric d. Hypertension renal artery atherosclerosis may activate the renin-angiotensin-aldosterone e. Vessel weakness abd. Aortic aneurysm
b. Arteriolosclerosis narrowing of small arterioles; thickening and loss of elasticity i. Hyaline caused by proteins leaking into the vessel wall and occludes the lumen 1. Diabetes mellitus proteins in basement membrane 2. Hypertension increased intraluminal pressure pushes plasma proteins into the vessel wall
3. Results in end-organ ischemia; produces glomerular scarring that slowly progresses to chronic renal failure ii. Hyperplastic thickening of vessel wall by smooth muscle cell hyperplasia (onion skin appearing) in malignant hypertension (~ 200/120 mm Hg) 1. May lead to fibrinoid necrosis of the vessel wall with hemorrhage 2. Classically causes acute renal failure with a characteristic flea-bitten appearance
c. Monckeberg medial calcific sclerosis calcification in the media of muscular (medium-sized) arteries (radial or ulnar) non-obstructive; pipestem arteries; seen on X-ray or mammography
2. Hypertension increased blood pressure; pulmonary or systemic circulation; systemic HTN = pressure > 140/90 (normal < 120/80)
a. Primary (95%) aka essential related to increased CO or TPR i. Risk factors: age, race, obesity, stress, lack of physical activity, and high-salt diet ii. Role of sodium in HTN: excess Na increases plasma volume increases stroke volume and systolic blood pressure 1. Produces vasoconstriction of TPR arterioles increases diastolic blood pressure iii. BP = CO x PR (peripheral resistance)
b. Secondary (5%) MCC is renovascular HTN (renal artery stenosis) caused by atherosclerosis (elderly males) and fibromuscular dysplasia (young females) 3. Aneurysm due to weakening of the vessel wall, followed by dilation and a tendency to rupture. a. True bounded by arterial wall components or the attenuated wall of the heart (atherosclerotic, syphilitic, and congenital vascular aneurysms) b. False breach in the vascular wall leading to an extravascular hematoma that freely communicates with the intravascular space (pulsating hematoma) i.e post-MI rupture contained by a pericardial adhesion, or a leak at the anastomosis of a vascular graft
c. Two important disorders that predispose to aortic aneurysms atherosclerosis (abdominal aortic aneurysms) and HTN (ascending aorta) d. Sequelae rupture, obstruction, embolism, compression (ureter, spine) e. MC clinical factor affecting aneurysm growth blood pressure f. Abdominal aortic aneurysms usually located below the renal artery orifices, but above the aortic bifurcation; balloon-like dilation i. Primarily due to atherosclerosis; classically seen in male smokers > 60 years old with HTN 1. Atheroscl. Increases the diffusion barrier to the media, resulting in atrophy (thinning) and weakness of the vessel wall ii. Lumen fills with atheromatous debris and blood clots, increased MMP production iii. Usually aysmptomatic iv. Major complication is rupture (> 5cm in diameter); presents with triad of HYPOtension, pulsatile abd. mass, and flank (back) pain g. Thoracic aneurysms balloon-like dilation of the thoracic aorta i. Seen in tertiary syphilis; endarteritis of the vasa vasorum results in luminal narrowing, decreased flow, and atrophy of the vessel wall tree-bark appearance of the aorta
ii. MC complication: aortic valve insufficiency iii. Other complications: compression of mediastinal structures (airway or esophagus), thrombosis/embolism, cough, pain h. Mycotic aneurysm vessel wall weakening due to an infection; originate either from embolization of a septic embolus (complication of infective endocarditis) or direct infection; thrombosis and rupture are possible complications i. Syphilitic aneurysm complication of tertiary syphilis; usually occurs in men 40-55 years old; vasculitis = endarteritis obliterans i. Classic: plasma cells present in vessel wall
ii. Vessel ischemia of the medial tissue leads to dilation of the aorta and aortic valve ring iii. Aortic valve regurgitation (problem in closing the aortic valve, which closes in diastole, blood leaks back into the ventricle) bounding pulses iv. Brassy cough left recurrent laryngeal nerve is stretched j. Berry aneurysm of cerebral arteries look at goljan k. Aortic dissection intimal tear with dissection of blood through media of the aortic wall (opened aorta) i. Occurs in the proximal 10cm of the aorta with preexisting weakness of the media ii. MCC is HTN (men 40-60 years old); also associated with CT disorders in young people (marfan, ehlers-danlos syndrome) iii. Hypertension hyaline arteriosclerosis of the vasa vasorum; decreased flow causes atrophy of the media iv. Marfan and EDS medial necrosis v. Cystic medial degeneration elastic tissue fragmentation, matrix maerial collects in areas of fragmentation in the tunica media 1. Risk factors increase in wall stress (HTN, pregnancy) vi. Clinical findings acute onset of severe retrosternal chest pain radiating to the back; aortic valve regurgitation (radiograph or ECG shows widening of the aortic valve root); loss of the upper extremity pulse (compression of subclavian artery) weakness of the CT in the media cystic
vii. Type A proximal (ascending aorta); B- descending aorta (distal) viii. X-ray of the abdomen double barrel aorta; may be confused for acute MI ix. Complications: pericardial tamponade (MCC of death), rupture with fatal hemorrhage, and obstruction of branching arteries (coronary or renal) with resultant end-organ ischemia 4. Vasculitis inflammation of the blood vessel wall a. Arterial wall endothelial intima, smooth muscle media, and CT adventitia b. Immune complexes antineutrophil cytoplasmic antibodies (ANCA) directed against enzymes found within the azurophil or neutrophils in monocytes and endothelial cells i. C-ANCA cytoplasmic location ii. P-ANCA perinuclear and is usually specific for myeloperoxidase c. Clinical features i. Inflammation, fever, fatigue, weight loss, and myalgia ii. Organ ischemia due to luminal narrowing or thrombosis of the inflamed vessels d. Large-vessel Vasculitis involves aorta & its major branches i. Temporal (giant cell) arteritis MC form of systemic vasculitis in adults artery is palpable 1. Granulomatous vasc. that involves carotid artery 2. Presents as unilateral headache (temporal artery), visual disturbances (ophthalmic artery), and pain when chewing. Flu-like symptoms with joint and muscle pain (polymyalgia rheumatica); ESR elevated 3. Affected arteries develop nodular thickenings with reduction of the lumen (may become thrombosed);
fragmentation of the internal elastic lamina
4. Treat with corticosteroids; risk of blindness without ii. Takayasu arteritis pulseless disease; involves the aortic arch at branch points; in asian females younger than 50 1. ESR is elevated, treat with corticosteroids 2. Fever, arthritis, night sweats, myalgia, skin nodules, ocular disturbances e. Medium-vessel vasculitis involves muscular arteries that supply organs i. Polyarteritis nodosa (PAN) necrotizing vasculitis involving often renal, coronary, and mesenteric arteries; spares pulmonary arteries (lungs) 1. Segmental, transmural (all layers of blood vessel), necrotizing (fibrinoid) inflammation 2. Vessels at all stages of acute and chronic inflammation (neutrophils, eosinphils, and mononuclear cells) a. String of pearls appearance 3. Presents in young adults as HTN (renal artery), abdominal pain with melena (mesenteric artery), neurologic disturbances, and skin lesions (cutaneous nodules) 4. Associated with HBsAg (~30% with HBV antigen)
5. Treat with corticosteroids and cyclophosphamide ii. Kawasaki disease Asian children < 4 years old involving coronary arteries; aka mucocutaneous lymph node syndrome; strawberry tongue 1. Nonspecific signs including fever, conjunctivitis, erythematous rash of palms and soles, and enlarged cervical LN 2. Coronary artery involvement is common and leads to risk for thrombosis with MI and aneurysm with rupture 3. Abnormal ECG 4. Treat with aspirin and IV gammaglobulin; avoid corticosteroids because danger of vessel rupture iii. Buerger Disease thromboangiitis obliterans; seen in heavy smokers 1. Necrotizing vasculitis involving digits 2. Presents with ulceration, gangrene, and Raynaud phenomenon; tibial and radial arteries MC involved 3. Thrombosis of the lumen, which may undergo organization and recanalization; thrombus contains small microabscesses with a central focus of neutrophils surrounded by granulomatous inflammation f. Small-vessel vasculitis involves arterioles, capillaries, and venules i. Microscopic Polyangiitis aka hypersensitivity or leukocytoclastic vasculitis an immunologic reaction to an Ag such as penicillin, bacteria, heterologous proteins, and tumor Ag 1. Necrotizing vasculitis involving multiple organs (especially lung and kidney)
2. Presents as palpable purpura involving the skin, or involvement of the mucous membranes, lungs, brain, heart, GIT, kidneys, and muscle 3. Clinical features are hemoptysis with bilateral nodular lung infiltrates, arthralgia, abdominal pain, hematuria (due to rapidly progressive glomerulonephritis), and proteinuria 4. Skin biopsy is diagnostic; microscopically there is fragmentation of neutrophils; Serum p-ANCA Ab ii. Churg-Strauss syndrome necrotizing granulomatous inflammation with eosinophils involving multiple organs, especially lungs and heart (similar to PAN) 1. Asthma and peripheral eosinophilia are often present; allergic rhinitis 2. p-ANCA Ab iii. Wegener granulomatosis necrotizing vasculitis 1. Acute necrotizing granulomas of URT, LRT 2. Necrotizing or granulomatous vasculitis affecting small to medium-sized vessels in lungs and upper airways 3. Renal disease in the form of focal necrotizing, often crescentic glomerulitis 4. Middle-aged man with sinusitis or nasopharyngeal ulceration, hemoptysis with bilateral nodular lung infiltrates, and hematuria 5. Serum c-ANCA Ab increased
6. Biopsy reveals large necrotizing granulomas with adjacent necrotizing vasculitis
7. Treat: corticosteroids, cyclophosphamide iv. Henoch-Schonlein Purpura vasculitis due to IgA immune complex deposition; MC vasculitis in children 1. Palpable purpura on butt and legs, GI pain and bleeding, and hematuria (IgA nephropathy); usually follows a URT infection 2. Polyarthritis and nephropathy v. Cryoglobulinemia involving skin, GIT, renal vessels 1. Seen in adults, associated with HCV 2. Cryoglobulins Ig s that gel at cold temperature 3. Palpable purpura, acral cyanosis of nose and ears, and Raynaud s 5. Raynaud decreased blood flow to the skin due to arteriolar vasospasm in
response to cold temperature or emotional stress (primary-disease) a. MC in fingers and toes; affects small vessels b. Phenomenon when secondary to a mixed CT disease, SLE, or CREST 6. Varicose veins dilated, tortuous superficial veins due to chronically increased venous pressure. Predisposes to poor wound healing and varicose ulcers a. MCL Superficial saphenous veins b. Causes of superficial varicosities: valve incompetence (reversal of blood flow) exacerbated by pregnancy, prolonged standing, obesity, advanced age; Secondary to deep vein thrombosis
c. Microscopy: variations in the thickness of the vein wall caused by dilation in some areas and hypertrophy of the SM and subintimal fibrosis in others i. Elastic tissue degeneration and spotty calcifications within the media phlebosclerosis d. Sequelae edema, stasis dermatitis, and varicose ulcers; embolism rare 7. Thrombophlebitis inflammation; pain and tenderness along the course of a superficial vein related to a blood clot or thrombus 8. Phlebothrombosis thrombosis of a vein without inflammation a. Caused by stasis of blood flow, hypercoagulability (antithrombin III deficiency) b. MCL deep vein of the calf c. Swelling, pain on dorsiflexion, pitting edema distal to thrombosis 9. Superior vena cava syndrome compression of SVC by primary lung tumor (usually small cell carcinoma, bronchogenic CA, or mediastinal lymphoma) a. Puffiness and blue discoloration of the face, arms, and shoulders (Dusky cyanosis) 10. IVC syndrome secondary to neoplasms (HCC, RCC), thrombus from hepatic, renal, or lower extremity veins, AAA, gravid uterus a. marked lower extremity edema, distenion of veins, and massive proteinuria 11. Lymphatic disorders lymphatic vessels have incomplete basement membranes, which predisposes them to infection and tumor invasion a. Acute lymphangitis inflammation red streak, usually due to cellulitis b. Secondary or obstructive lymphedema accumulation of interstitial fluid behind a blockage of previously normal lymph i. Result from malignant tumors, surgical procedures (radial mastectomy), post irradiation fibrosis; peau d orange (increased deposition of interstitial CT with tissue expansion)
c. Chylous effusions (pleural cavity) caused by rupture of obstructed, dilated lymphatics into the pericardium, pleural cavity, or peritoneum, due to obstruction by an infiltrating tumor mass; damage to thoracic duct 12. Vascular tumors derived from endothelial cells or from cells that support and/or surround blood vessels a. Hemangioma benign tumor comprised of blood vessels; commonly presents at birth i. Strawberry benign capillary hemangioma of infancy. Initially grows with the child, then regresses during childhood 1. Occurs in the skin, subcutaneous tissues, and mucous membranes of lips and tongue ii. Cherry benign cavernous hemangioma of the elderly. DOES NOT REGRESS. Frequency increases with age 1. Characterized by large, dilated vascular channels; less well circumscribed, locally destructive iii. Pyogenic granuloma- lobular capillary hemangioma 1. Can ulcerate and bleed; oral cavity MC, regress 2. Rapidly growing exophytic red nodule attached by a stalk to the skin and gingival or oral mucosa a. Associated with trauma and pregnancy b. Cystic hygroma cavernous lymphangioma of the head and neck. Associated with turner syndrome i. Distinguished from capillary channels only by the absence of blood cells c. Glomus tumor benign, painful, red-blue tumor under fingernails. Arises from modified smooth muscles of the glomus body (involved in thermoregulation) d. Vascular ectasias lesions characterized by localized dilation of preexisting vessels creates a small focal red lesion i. Nevus Flammeus ordinary birthmark (MC form of ectasia)
1. Flat lesion on the head of neck, ranging from light pink to deep purple 2. Port-wine stain no tendency to fade; distribution of the trigeminal nerve may be associated with SturgeWeber syndrome ii. Hereditary Hemorrhagic Telangiectasia (Osler-WeberRendu Disease) present from birth, widely distributed over the skin and oral mucous membranes; occasionally, these lesions rupture, causing epistaxis (nosebleeds), GI bleeding, or hematuria iii. Bacillary angiomatosis benign capillary skin papules found in AIDS patient; Caused by Bartonella henselae infections. Frequently mistaken for Kaposi s sarcoma 1. Stimulates VEGF production e. Kaposi Sarcoma endothelial malignancy of the skin associated with HHV-8 and HIV i. Presents as purple patches, plaques, and nodules on the skin; may involve visceral organs ii. Seen in older eastern European males tumor remains localized to skin iii. Microscopic: dilated, irregular, and angulated blood vessels lined by plump spindle cells with lymphocytes, plasma cells, and hemosiderin macrophages iv. Markers for diagnosis: Factor VIII or CD-31 f. Angiosarcoma highly lethal malignant proliferation of endothelial cells; MC in liver associated with exposure to polyvinyl chloride i. may not look vascular at all; severe atypia
Das könnte Ihnen auch gefallen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Physical Fitness Short Note (SPSC 1011) Unit One 1. 1. Concepts of Physical Fitness1 1.1. 1. Meanings and Definitions of Physical FitnessDokument62 SeitenPhysical Fitness Short Note (SPSC 1011) Unit One 1. 1. Concepts of Physical Fitness1 1.1. 1. Meanings and Definitions of Physical Fitnesseyob astatkeNoch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Handbook of Indexing Techniques A Guide For Beginn... - (Chapter 3 Writing The Index)Dokument16 SeitenHandbook of Indexing Techniques A Guide For Beginn... - (Chapter 3 Writing The Index)joseph jaalaNoch keine Bewertungen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Practice of Interventional Radiology - Valji (2012)Dokument753 SeitenThe Practice of Interventional Radiology - Valji (2012)Nar Rungrojanarak75% (4)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- KROK Part - II PDFDokument99 SeitenKROK Part - II PDFPiravi 19Noch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Nutrition and Biotechnology in Heart Disease and CancerDokument266 SeitenNutrition and Biotechnology in Heart Disease and CancerGeorge CiucaNoch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- GRE Practice TestDokument47 SeitenGRE Practice TestVincent YuNoch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Lesson 9 HIS Hospital Information SystemDokument36 SeitenLesson 9 HIS Hospital Information SystemKauline Joseph C. BrionesNoch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- ARTERISCLEROSISDokument46 SeitenARTERISCLEROSISAdilla Edi AriefNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Atherosklerosis, Artheriosklerosis Dan Kelainan VaskulerDokument66 SeitenAtherosklerosis, Artheriosklerosis Dan Kelainan VaskulerOlivia Chandra DeviNoch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- BSN - 4C: PresentorsDokument52 SeitenBSN - 4C: PresentorsHanya Bint Potawan100% (1)
- Finite Element Analysis For Fatigue Behaviour of A Self-Expanding NitinolDokument10 SeitenFinite Element Analysis For Fatigue Behaviour of A Self-Expanding NitinolhanNoch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Pasmedicine 2019Dokument183 SeitenPasmedicine 2019Ibrahim FoondunNoch keine Bewertungen
- Atherosclerotic Cardiovascular DiseaseDokument68 SeitenAtherosclerotic Cardiovascular DiseaseMarisa Adytia Adha100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- CT BR SureSubtraction CT DSADokument11 SeitenCT BR SureSubtraction CT DSAWALVRadiologyNoch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- 003 Pathology MCQ ACEM Primary CardiovascularDokument5 Seiten003 Pathology MCQ ACEM Primary Cardiovascularbmhsh100% (2)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Kaya ChikitsaDokument37 SeitenKaya ChikitsaGAURAV100% (1)
- Research Proposal Preventing Cardiovasular Disease FinalDokument12 SeitenResearch Proposal Preventing Cardiovasular Disease Finalapi-581022439Noch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- (Traves D. Crabtree) BRS Surgical Specialties PDFDokument254 Seiten(Traves D. Crabtree) BRS Surgical Specialties PDFCosmin Alexa100% (2)
- DB13 - Pathophysiology of AtherosclerosisDokument2 SeitenDB13 - Pathophysiology of Atherosclerosisi_vhie03Noch keine Bewertungen
- Circulatory System REVIEWERDokument6 SeitenCirculatory System REVIEWERClyde BaltazarNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- A Review On The Biomechanics of Coronary ArteriesDokument62 SeitenA Review On The Biomechanics of Coronary ArteriesAbhishek KarmakarNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- HCVD Cad Cva InfarctionDokument2 SeitenHCVD Cad Cva InfarctionPamela DomingoNoch keine Bewertungen
- Safety Reports Series: Radiation Protection in Newer Medical Imaging Techniques: Cardiac CTDokument30 SeitenSafety Reports Series: Radiation Protection in Newer Medical Imaging Techniques: Cardiac CTjiar001Noch keine Bewertungen
- Clinical Spectrum of Atherosclerotic Heart DiseaseDokument50 SeitenClinical Spectrum of Atherosclerotic Heart Diseaseadamu mohammadNoch keine Bewertungen
- Textbook of Stroke Medicine, 2E (2013)Dokument426 SeitenTextbook of Stroke Medicine, 2E (2013)Liviu IacobNoch keine Bewertungen
- NUR100 Sherpath CH 45 Nutrition ImbalanceDokument4 SeitenNUR100 Sherpath CH 45 Nutrition Imbalancecaloy2345caloyNoch keine Bewertungen
- CT CalscoringDokument7 SeitenCT CalscoringPrem Kumar BNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Ischemic Heart Disease (IHD)Dokument55 SeitenIschemic Heart Disease (IHD)rameshbmc100% (5)
- AtherosclerosisDokument27 SeitenAtherosclerosisAnonymous wesmz90Oh1Noch keine Bewertungen
- New Concepts On The Pathophysiology of Acute Coronary SyndromeDokument11 SeitenNew Concepts On The Pathophysiology of Acute Coronary SyndromeLuis GuerraNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)