Beruflich Dokumente
Kultur Dokumente
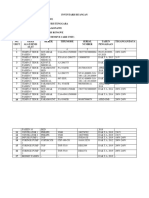
Nutrition Support Assessment
Hochgeladen von
adevasenOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Nutrition Support Assessment
Hochgeladen von
adevasenCopyright:
Verfügbare Formate
DISCLAIMER: These guidelines were prepared by the Department of Surgical Education, Orlando Regional Medical Center.
They are intended to serve as a general statement regarding appropriate patient care practices based upon the available medical literature and clinical expertise at the time of development. They should not be considered to be accepted protocol or policy, nor are intended to replace clinical judgment or dictate care of individual patients.
NUTRITIONAL ASSESSMENT IN CRITICALLY ILL PATIENTS
SUMMARY Indirect calorimetry (IC) is considered the gold standard for determination of a patients caloric needs. Controversy remains when comparing IC with weight-based equations such as the Harris-Benedict Equation (HBE). Although there is new evidence to support that the HBE may closely estimate caloric needs when multiplied by certain stress factors, there is also contradictory evidence demonstrating that the HBE can lead to either over- or underfeeding, which is associated with a multitude of complications. RECOMMENDATIONS Level 1 None Level 2 Initial estimation of caloric needs using 30 kcal/kg/day (or Harris-Benedict Equation (HBE) with appropriate stress factors) and protein needs using 1.5 gm/kg of protein per day is a reasonable and cost free alternative to indirect calorimetry (IC). Level 3 Pre-albumin is a practical and accurate marker of nutritional status due to its short half-life. The Curreri formula should be used to estimate the caloric needs of patients with burns greater than 20% total body surface area (TBSA). Indirect calorimetry (IC) and 24 hour urine urea nitrogen (UUN) studies should be utilized to determine the caloric needs of mechanically ventilated patients requiring supplemental nutrition for greater than 7 days.
INTRODUCTION Nutrition is an important, but often overlooked aspect of critical care management. During the 1990s, there was a major shift from parenteral nutrition (PN) to enteral nutrition (EN), which remains the preferred method for providing nutritional support to the critically ill given its improved patient outcome. Providing the gastrointestinal tract with nutrients directly, EN can help prevent mucosal atrophy and increased permeability with resultant decreases in bacterial translocation and priming of neutrophils and macrophages. As the importance of adequate nutrition has become evident, the ability to determine the patients caloric and protein needs in a convenient yet accurate manner has become essential. This is important not only to prevent underfeeding, but overfeeding as well. The fundamental goal of nutritional support is to meet the energy requirements of metabolic processes, to support the hypermetabolism associated with critical illness, and to minimize protein catabolism. Nutritional support begins with an estimation of the patients caloric requirements. The Harris Benedict Equation (HBE) is one of the most commonly used methods for estimating caloric needs or basal energy expenditure (BEE). It is calculated as follows:
EVIDENCE DEFINITIONS Class I: Prospective randomized controlled trial. Class II: Prospective clinical study or retrospective analysis of reliable data. Includes observational, cohort, prevalence, or case control studies. Class III: Retrospective study. Includes database or registry reviews, large series of case reports, expert opinion. Technology assessment: A technology study which does not lend itself to classification in the above-mentioned format. Devices are evaluated in terms of their accuracy, reliability, therapeutic potential, or cost effectiveness. LEVEL OF RECOMMENDATION DEFINITIONS Level 1: Convincingly justifiable based on available scientific information alone. Usually based on Class I data or strong Class II evidence if randomized testing is inappropriate. Conversely, low quality or contradictory Class I data may be insufficient to support a Level I recommendation. Level 2: Reasonably justifiable based on available scientific evidence and strongly supported by expert opinion. Usually supported by Class II data or a preponderance of Class III evidence. Level 3: Supported by available data, but scientific evidence is lacking. Generally supported by Class III data. Useful for educational purposes and in guiding future clinical research. 1 Approved 06/09/2007
Males: Females:
BEE = 66.5 + 13.8 (weight in kg) + 5 (height in cm) 6.8 (age) BEE = 655 + 9.6 (weight in kg) + 1.7 (height in cm) 4.7 (age)
These equations yield basal energy requirements that are frequently multiplied by various activity and/or stress factors to generate the patients estimated resting energy expenditure (REE): Stress Factors: Minor Surgery 1.2, Trauma 1.35, Sepsis 1.6, Major Burns 2.1 REE = BEE * stress factors Some studies have demonstrated that the use of stress factors may lead to an overestimation of the patients actual caloric needs, leading to overfeeding and unnecessary administration of nutrients. Another important consideration is the patient weight that is used for these calculations. The patients current actual body weight may be quite elevated after a period of aggressive volume resuscitation and its use in calculations could result in overestimation of caloric requirements. Ideally, an admission weight prior to initial resuscitation should be obtained. In practice, this assessment is impractical and not normally part of the primary and secondary surveys in the acutely injured patient. An accurate measurement of body weight is an arduous task in critically ill patients with bulky dressings, catheters, monitoring wires, tubes and drains. The ideal body weight (IBW) may prove useful in such circumstances and is calculated as follows: IBW (male) = 50 + (2.3 * height [in inches] -60) IBW (female) = 45.5 + (2.3 * height [in inches] -60) Obesity poses another scenario where overfeeding may result if one uses the patients actual body weight. Obesity is defined as an actual body weight that is greater than 120% above the patients IBW or a Body Mass Index (BMI) >30. For all of the above reasons, the adjusted body weight (ABW) is commonly utilized for calculating energy requirements: ABW = 0.25 * (actual weight - IBW) + IBW A more specific method that may be used to determine caloric needs in mechanically ventilated patients is to perform indirect calorimetry (IC). This is considered the gold standard for caloric assessment. A computerized metabolic cart is used to collect the patients expired gases to determine CO2 production and O2 consumption, which are used to calculate the REE using the Weir equation: REE = [VO2 (3.941) + VCO2 (1.11)] 1440 min/day IC also provides the respiratory quotient (RQ = CO2 production divided by O2 consumption) which can be further used to monitor the adequacy of nutritional support. An RQ of greater than 1.0 suggests overfeeding and lipogenesis, while an RQ = 1.0 indicates pure carbohydrate utilization. Unlike glucose metabolism, oxidation of fatty acids requires less O2 and produces less CO2. Pure fat utilization produces an RQ of 0.7 and a value of less than 0.7 suggests underfeeding and ketogenesis. Mixed substrate utilization, the desired goal of nutritional support, is suggested when the RQ value falls within the 0.8 to 0.9 range. There are several limitations to IC including the need for dedicated equipment and staff. Such measurements are costly and are for the most part limited to those patients on a mechanical ventilator. Measurements may be inaccurate in patients with conditions often encountered in the critically ill. These include patients on high levels of oxygen (Fi02 > 0.6), high positive end expiratory pressure (PEEP), air leaks (such as bronchopleural fistulae) which may limit the ability to adequately collect and analyze expired gases, and peritoneal and hemodialysis due to removal of CO2 across the membrane that is not measured by the indirect calorimeter. One must also consider the fact that these measurements are only a reflection of the short window of time during which the patient is being studied. In general, the patient
Approved 06/09/2007
selected for this study should be in a stable, steady state. The patient should also be protected from noise or other stimulation. The literature addressing the optimal method for nutritional assessment is controversial and is outlined below. It should be remembered that no specific formula has been proven to be superior to the others and that these should be considered to provide at best an estimate of the patients initial protein and caloric needs. Currently recommendations for most surgical patients are to provide approximately 25-30 kcal/kg/day through the administration of carbohydrates (70%) and lipids (30%). Protein should not be included in these energy calculations as the intent is for the protein to be incorporated into new muscle rather than metabolized into energy. Protein is the building block of life. Once hepatic glycogen stores are depleted, muscle protein is degraded to provide three carbon backbones for hepatic gluconeogenesis. Initially protein catabolism is resistant to the administration of exogenous amino acids and it takes weeks until a critically ill patient is found to be in a state of positive nitrogen balance. In addition to protein catabolism, exogenous protein is required for wound healing and to replace that lost in wounds and fistulae. The goal is to minimize the loss of lean body mass and as a general rule this requires anywhere from 1.0 to 1.5 gm/kg/day of protein depending on the degree of illness and injury. A severely burned patient may require in excess of 2.0 gm/kg/day to replace the large quantities of protein lost through their wounds. Another circumstance that one must consider is the patient with an open abdomen who may lose additional amounts of nitrogen through their open abdomen and temporary dressing. There are several ways to estimate protein requirements. One simple method is to look at the ratio of non-protein calories to grams of nitrogen. A typical post-operative patient requires a ratio of 150 carbohydrate calories to 1 gram of nitrogen to prevent the use of protein as an energy source. Critically ill subjects and burn victims may require ratios below 100. Another method is to calculate the nitrogen balance following collection of a 24 hour urine specimen: Nitrogen balance = Nitrogen intake = nitrogen intake nitrogen output total protein intake (gm / day) 6.25 gm protein / gm nitrogen UUN + 4 grams + [1.9 * (liters of abdominal fluid)]
Nitrogen output =
where UUN is urine urea nitrogen in grams of nitrogen excreted in the urine over the 24 hour period. Four grams is typically used to estimate insensible nitrogenous losses through the skin and gastrointestinal tract. This is a very crude estimate of nitrogen balance and may not be valid in the patient with large burns or wounds. Cheatham et al showed that patients with an open abdomen lose on average 1.9 gm of nitrogen per liter of abdominal fluid. In patients with temporary abdominal dressings, this needs to be added to the insensible losses to avoid overestimating nitrogen balance which would, in turn, lead to underfeeding and inadequate nutritional support (1). A patient in positive nitrogen balance excretes less nitrogen than is being consumed and is incorporating nitrogen into newly formed protein. A patient in negative nitrogen balance excretes more nitrogen than they consume and continues to degrade muscle protein for gluconeogenic precursors. Determining caloric and protein needs has been discussed above. Once this has been done, one then needs to reevaluate the particular nutritional regimen the patient is receiving. There are a number of markers easily obtained to ascertain whether or not the patient is being properly nourished. These include albumin, prealbumin, and transferrin. Albumin has a long half-life of 20 days making it a less desirable test. Transferrin, with a half life of 8-10 days is also of limited usefulness. Pre-albumin has a half-life of 2 days and has proven to be accurate in burn and trauma patients making it the best marker for nutritional monitoring. Regarding burn patients, there is a large body of literature that demonstrates the inaccuracy of the HBE and the 30 kcal/kg empiric formulas in estimating caloric needs. In the 1970s, Dr. Curreri and his
Approved 06/09/2007
colleagues developed a formula that incorporates the percentage of the body surface area burned and seems to more accurately estimate the calories necessary for a hypermetabolic post-burn response (2). The formula they developed is still in use today and is as follows: Curreri formula = 25 * body weight (kg) + 40 * % TBSA burned This formula has been found to overestimate the caloric needs in some burn patients, however, it seems to be more accurate than the other available formulas for estimating burn patient needs. The most likely reason for this is that it incorporates the percentage burn while the other equations do not.
LITERATURE REVIEW In Support Of Indirect Calorimetry A retrospective evaluation of the determination of energy needs was performed by Boulatta et al (3). They evaluated 395 patients who had undergone IC over the previous year. Average REE (from IC) was 1730 402 in the critically ill group (n=141). Compared with other equations, the HBE was most accurate in the critically ill group when multiplied by a stress factor of 1.1; however, it was only accurate in 55% of patients. In the remaining 45% of the study population, the HBE either over- or underestimated the caloric needs of the individuals. Campbell et al. performed a retrospective comparison of IC versus calculated determination of caloric needs for the critically ill using the HBE as well as the Ireton-Jones equation (4). In this study, both current body weight and ideal body weight were used for the calculated estimates. The results demonstrated that the HBE calculations differed significantly from the determinations obtained by using IC regardless of whether current body weight or ideal body weight was utilized for the calculation. Using current body weight in the HBE calculation resulted in an average caloric estimation of 77.0% 11.6% of measured resting energy expenditure (MEE) (as determined by IC) while using ideal body weight in the HBE estimated 90% 16.1% of MEE ( as determined by IC). The Ireton-Jones equation tended to overestimate the MEE (as determined by IC) with the results being 109.3%16.8% of MEE. Ahmad et al. performed a prospective trial to evaluate the REE (as determined by IC) of severely underweight hospitalized patients. They evaluated 14 patients using IC and compared the results to the BEE estimated by the HBE and also compared the IC results to a more simplistic method of providing the patient with 25 kcal/kg/day. There was a statistical difference between the measured caloric needs using IC and the calculated needs for both HBE (1032 66 kcal/day) and the 25 kcal/kg/day formula (1023 129 kcal/day) (p < 0.0001). In Support Of Calculations Davis and colleagues performed a prospective study to evaluate the need for IC in the ICU by comparing it to the HBE and other weight based calculations (6). Their study incorporated trauma and surgical patients and utilized enteral feedings in 80% of the patients. IC determined the caloric need to be 2217 540 kcal/day while the HBE (multiplied by a stress factor of 1.5) and the standard weight-based formula (30 kcal/kg/day) estimated the caloric needs to be 2339 497 kcal/day and 2276 447 kcal/day respectively. They found no statistically significant differences between IC and the HBE or the weight based calculation of 30 kcal/kg/day recommended by the American Society for Parenteral and Enteral Nutrition (ASPEN) guidelines. They concluded that IC is unnecessary. A retrospective, observational study was performed in 2004 by Alexander et al (7). They evaluated 76 adult, critically ill, ventilated patients. They compared the BEE as determined by four commonly used equations with the resting energy expenditure as determined by IC. Accuracy of the equations was determined using bias and precision calculations. The HBE, when multiplied by a stress factor of 1.2, was unbiased and precise while the Ireton-Jones equation was precise, but biased. The American College of Chest Physicians recommendation of 25 kcal/kg/day was biased and not precise. They concluded that the HBE multiplied by a stress factor of 1.2 was accurate for predicting caloric needs when compared with the results obtained from indirect calorimetry.
Approved 06/09/2007
Faisy et al performed a prospective observational study to determine an accurate method for calculating the caloric needs of the critically ill (8). They evaluated 70 patients over a one year period using IC. These results were then compared with BEE determined using the HBE. Further comparison was performed between IC and the HBE using stress factors. They found that the REE (IC) averaged 1890 404 kcal/day and the BEE determined by the HBE averaged 1399 243 kcal/day. However, when the appropriate stress factors were multiplied by the BEE, the HBE results were 1817 528 kcal/day which was not significantly different from the calculated resting energy expenditure as determined by IC. Support For Prealbumin Use In Nutritional Assessment Devota et al demonstrated that pre-albumin was a valuable and accurate marker of patient response to nutritional support (9). They evaluated 108 hospitalized patients using the detailed nutritional assessment as a reference for comparison to pre-albumin. During analysis, pre-albumin was found to be an accurate tool for assessing nutritional status. Robinson et al. performed a prospective, observational study to evaluate the usefulness of their standard nutritional screening protocol as compared with laboratory assessment using prealbumin (PAB), albumin (ALB), and retinol binding protein (RBP) (10). 335 patients were evaluated from the medical, general surgery, MICU, SICU, and bone marrow transplant services. The screening protocol utilized a questionnaire which identified 43% of the study population to be at risk for malnutrition while PAB identified 51% to be at risk. It took an average of 3 days for the nutritional assessment utilizing the questionnaires in 69% of those considered at risk while PAB took an average of 3 days to identify 94% of those considered at risk. This difference in percentages was of statistical significance therefore demonstrating the worth of PAB in evaluating ones nutritional status.
SUMMARY Nutritional assessment remains an important tool in treating critically ill patients. Accurate determination of caloric needs is essential to obtaining the full benefits of nutritional therapy and aids in preventing the problems associated with underfeeding (infection, poor healing) as well as overfeeding (failure to wean the ventilator). There is still controversy regarding what the best method is to determine how to accurately estimate the caloric needs of the critically ill patient. There is a large amount of information that spans at least thirty years regarding the use of IC in determining ones caloric needs. The use of various equations has also been studied for many years. With more and more studies demonstrating the accuracy of equations, more and more institutions are abandoning IC due to cost and convenience and instead utilizing equations to estimate initial caloric requirements. IC may, however, be of value in mechanically ventilated patients who continue to remain critically ill and require supplemental nutritional support. The literature supports utilizing prealbumin levels in patient nutritional assessment as it has a short half life compared to albumin and retinol binding protein and is relatively inexpensive. Therefore, patients requiring prolonged hospitalization should undergo nutritional evaluation using prealbumin levels. The exact frequency of these measurements has yet to be determined. The current literature supports a practice of weekly prealbumin levels.
Approved 06/09/2007
REFERENCES 1. Cheatham ML, Safcsak K, Brzezinski SJ, Lube MW. Nitrogen Balance, Protein Loss, and the Open Abdomen. Crit Care Med 2007; 35: 1-5. 2. Curreri WP, Richmond D, Marvin J, Baxter C. Dietary Requirements of the Patient with Major Burns. Journal of the American Dietary Association 1974; 65: 415-417. 3. Boullata J, Williams J, Cottrell F, Hudson L Compher C. Accurate Determination of Energy Needs in Hospitalized Patients. Journal of the American Dietetic Association. 2007; 107: 393-401. 4. Campbell CG, Zander E, Thorland W. Predicted vs Measured Energy Expenditure in Critically Ill, Underweight Patients. Nutrition in Clinical Practice. 2005; 20: 276-280. 5. Ahmad A, Duerksen DR, Nunroe S, Bistrian BR. An Evaluation of Resting Energy Expenditure in Hospitalized, Severely Underweight Patients. Nutrition. 1999; 15: 394-388. 6. Davis KA, Kinn T, Esposito TJ, Reed RL, Santaniello JM, Luchette FA. Nutritional Gain Versus Financial Gain: The Role of Metabolic Carts in the Surgical ICU. J Trauma 2006; 61: 1436-1440. 7. Alexander E, Susla, GM, Burstein AH, Brown DT, Ognibene FP. Retrospective Evaluation of Commonly Used Equations to Predict Energy Expenditure in Mechanically Ventilated Critically Ill Patients. Pharmacotherapy. 2004; 24: 1659-1667. 8. Faisy C, Guerot E, Diehl JL, Labrousse J, Fagon JY. Assessment of Resting Energy Expenditure in Mechanically Ventilated Patients. American Journal of Clinical Nutrition. 2003; 78: 241-249. 9. Devoto G, Gallo F, Marchello C, Racchi O, Garbarini R, Bonassi S, Albalustri G, Haupt E. Prealbumin Serum Concentrations as a Useful Tool in the Assessment of Malnutrition in Hospitalized Patients. Clinical Chemistry. 2006; 52: 2281-2285. 10. Robinson MK, Trujillo EB, Mogensen KM, Rounds J, McManus K, Jacobs DO. Improving Nutritional Screening of Hospitalized Patients: the Role of Prealbumin. Journal of Parenteral & Enteral Nutrition. 2004; 27: 389-395.
Approved 06/09/2007
Approved 06/09/2007
Das könnte Ihnen auch gefallen
- Ketogenic Diet in Treating Obesity And Type 2 DiabetesVon EverandKetogenic Diet in Treating Obesity And Type 2 DiabetesNoch keine Bewertungen
- Surgical Nutrition PDFDokument8 SeitenSurgical Nutrition PDFClever ImaniaNoch keine Bewertungen
- Obesity - Short Scientific Findings to Ameliorate the Body WeightVon EverandObesity - Short Scientific Findings to Ameliorate the Body WeightNoch keine Bewertungen
- Liz AssignmentsDokument13 SeitenLiz Assignmentsapi-445479317Noch keine Bewertungen
- Practical Carbohydrate Counting: A How-to-Teach Guide for Health ProfessionalsVon EverandPractical Carbohydrate Counting: A How-to-Teach Guide for Health ProfessionalsBewertung: 5 von 5 Sternen5/5 (1)
- Adecuacion de Harris BenedictDokument7 SeitenAdecuacion de Harris BenedictEsme D'silosNoch keine Bewertungen
- Nutrition in The Critically Ill PatientDokument13 SeitenNutrition in The Critically Ill PatientnainazahraNoch keine Bewertungen
- Screening and Referral: Executive Summary of RecommendationsDokument8 SeitenScreening and Referral: Executive Summary of RecommendationsJoana TavaresNoch keine Bewertungen
- Case Study 30Dokument6 SeitenCase Study 30api-276551783Noch keine Bewertungen
- Nutrition Therapy For ALI and ARDSDokument13 SeitenNutrition Therapy For ALI and ARDSAlan Espíndola Cruz100% (1)
- Feeding Critically Ill Obese 1Dokument53 SeitenFeeding Critically Ill Obese 1gianellaNoch keine Bewertungen
- Nutrition Support in Critically Ill Patients - An Overview - UpToDateDokument23 SeitenNutrition Support in Critically Ill Patients - An Overview - UpToDateduong tien truongNoch keine Bewertungen
- Post-ICU Nutrition The Neglected Side of Metabolic SupportDokument3 SeitenPost-ICU Nutrition The Neglected Side of Metabolic SupportHubert PastasNoch keine Bewertungen
- Unit 5 Assessment Sitaca Tan Viedor Yap 1Dokument12 SeitenUnit 5 Assessment Sitaca Tan Viedor Yap 1api-532152575Noch keine Bewertungen
- Chapter 6 Nutrition Care ProcessDokument17 SeitenChapter 6 Nutrition Care Processr55fsf75hpNoch keine Bewertungen
- Aspen Spinal Cord InjuryDokument8 SeitenAspen Spinal Cord InjuryLuis Javier CastroNoch keine Bewertungen
- Nutricion PerioperatoriaDokument11 SeitenNutricion PerioperatoriaAndres Neira QuezadaNoch keine Bewertungen
- MFN-005 Unit-4 PDFDokument17 SeitenMFN-005 Unit-4 PDFShubhendu ChattopadhyayNoch keine Bewertungen
- A.S.P.E.N. Clinical Guidelines Nutrition Support of Hospitalized Adult Patients With Obesity.Dokument9 SeitenA.S.P.E.N. Clinical Guidelines Nutrition Support of Hospitalized Adult Patients With Obesity.Madalina TalpauNoch keine Bewertungen
- Nutrition Therapy - ArtículoDokument7 SeitenNutrition Therapy - ArtículoNicolas Esteban Casallas MendezNoch keine Bewertungen
- Caloric Intake Data AccuracyDokument6 SeitenCaloric Intake Data AccuracylyleNoch keine Bewertungen
- Nutritional Needs of Critically Ill ChildDokument9 SeitenNutritional Needs of Critically Ill Childdaniphilip777100% (11)
- RD Competency Quiz QuestionsDokument5 SeitenRD Competency Quiz QuestionsCameron SeguraNoch keine Bewertungen
- Critical Illness: Nutrition Care ManualDokument20 SeitenCritical Illness: Nutrition Care ManualDiogo JuniorNoch keine Bewertungen
- Critical Ill PDFDokument5 SeitenCritical Ill PDFAnish H DaveNoch keine Bewertungen
- (2019) Metabolic Support Challenges With Obesity During Critical IllnessDokument8 Seiten(2019) Metabolic Support Challenges With Obesity During Critical IllnessAnna Maria Ariesta PutriNoch keine Bewertungen
- Nutrition in ICUDokument13 SeitenNutrition in ICURicky DepeNoch keine Bewertungen
- Nutrisi SepsisDokument20 SeitenNutrisi SepsisTantri SyahtiraNoch keine Bewertungen
- Near-Target Caloric Intake in Critically Ill Medical-Surgical Patients Is Associated With Adverse OutcomesDokument42 SeitenNear-Target Caloric Intake in Critically Ill Medical-Surgical Patients Is Associated With Adverse OutcomesyufapipiNoch keine Bewertungen
- Official Reprint From Uptodate ©2018 Uptodate, Inc. And/Or Its Affiliates. All Rights ReservedDokument16 SeitenOfficial Reprint From Uptodate ©2018 Uptodate, Inc. And/Or Its Affiliates. All Rights ReservedGallethiita de ChocolatiitoNoch keine Bewertungen
- Effects of Intermittent and Continuous Calorie Restriction On Body Weight and Metabolism Over 50 WK: A Randomized Controlled TrialDokument13 SeitenEffects of Intermittent and Continuous Calorie Restriction On Body Weight and Metabolism Over 50 WK: A Randomized Controlled TrialSarah OctaviaNoch keine Bewertungen
- Hypocaloric, High-Protein Nutrition Therapy For Critically Ill Patients With ObesityDokument7 SeitenHypocaloric, High-Protein Nutrition Therapy For Critically Ill Patients With ObesityStacey WoodsNoch keine Bewertungen
- Nutritional Pyramid For Post-Gastric Bypass Patients: Current StatusDokument9 SeitenNutritional Pyramid For Post-Gastric Bypass Patients: Current StatusvcaguiarNoch keine Bewertungen
- Estimating Energy Requirements ArticleDokument9 SeitenEstimating Energy Requirements ArticleyusufNoch keine Bewertungen
- Negative Impact of Hypocaloric Feeding and Energy Balance On Clinical Outcome in ICU PatientsDokument8 SeitenNegative Impact of Hypocaloric Feeding and Energy Balance On Clinical Outcome in ICU PatientsDaniela HernandezNoch keine Bewertungen
- Guia ESPEN - Tamizaje NutricionalDokument7 SeitenGuia ESPEN - Tamizaje NutricionalJudy OlivaNoch keine Bewertungen
- Nutrition Journal of Parenteral and Enteral: Less or More? Enteral Nutrition in Critically Ill Septic PatientsDokument4 SeitenNutrition Journal of Parenteral and Enteral: Less or More? Enteral Nutrition in Critically Ill Septic PatientsMarco Antonio BravoNoch keine Bewertungen
- 2018 REview NutritionTherSepsisDokument20 Seiten2018 REview NutritionTherSepsisMedicinaInternaNoch keine Bewertungen
- Nutrition in ICU: DR Rahul VarshenyDokument50 SeitenNutrition in ICU: DR Rahul VarshenyAntar InenigogNoch keine Bewertungen
- Dasar Gizi KlinikDokument69 SeitenDasar Gizi KlinikTio Muhammad Fadlillah Firstiogusran100% (2)
- !!!IJF1Dokument16 Seiten!!!IJF1Nayane NoronhaNoch keine Bewertungen
- New Microsoft Office PowerPoint PresentationDokument27 SeitenNew Microsoft Office PowerPoint PresentationDr-Iyad AljuaidiNoch keine Bewertungen
- Lesson 1 Back To Basics Estimating Energy Requirements Foradult Hospital PatientsDokument8 SeitenLesson 1 Back To Basics Estimating Energy Requirements Foradult Hospital PatientsBalireddy NeeharikaNoch keine Bewertungen
- TSWJ2012 909564Dokument6 SeitenTSWJ2012 909564Tomas Lopez RNoch keine Bewertungen
- Evidencia Científica de Dietas para Bajar de Peso Diferente Composición de Macronutrientes, Ayuno Intermitente y Dietas PopularesDokument35 SeitenEvidencia Científica de Dietas para Bajar de Peso Diferente Composición de Macronutrientes, Ayuno Intermitente y Dietas PopularesCesar Flores ValleNoch keine Bewertungen
- Nutritional AssessmentDokument8 SeitenNutritional AssessmentOutour KhNoch keine Bewertungen
- Hypocaloric Enteral NutritionDokument10 SeitenHypocaloric Enteral NutritionMario TGNoch keine Bewertungen
- 10.1007@s11154 019 09514 yDokument12 Seiten10.1007@s11154 019 09514 ysimonNoch keine Bewertungen
- 3 SkaarJ RDsInPracitce PICUDokument53 Seiten3 SkaarJ RDsInPracitce PICUIrhamna FauziahNoch keine Bewertungen
- Pi Is 1054139 X 13003157Dokument6 SeitenPi Is 1054139 X 13003157Pablo Andres Encina AbrigoNoch keine Bewertungen
- Optimal Nutrition During The Period of Mechanical Ventilation - Ccforum Article - DOC1061468Dokument11 SeitenOptimal Nutrition During The Period of Mechanical Ventilation - Ccforum Article - DOC1061468Solomon YimerNoch keine Bewertungen
- Personalized Nutrition Therapy in Critical CareDokument16 SeitenPersonalized Nutrition Therapy in Critical CareAlfredo MenaNoch keine Bewertungen
- Nutrion in ObesityDokument40 SeitenNutrion in Obesitykero R.habibNoch keine Bewertungen
- Article Review Nutrition in Critically Ill ChildDokument6 SeitenArticle Review Nutrition in Critically Ill ChildkhairachungNoch keine Bewertungen
- PIIS240545772100245XDokument5 SeitenPIIS240545772100245Xsulemi castañonNoch keine Bewertungen
- Cocca 29 101Dokument7 SeitenCocca 29 101Rasime Sevgi CenanNoch keine Bewertungen
- Adult Nutrition Guidelines For ICU PatientsDokument13 SeitenAdult Nutrition Guidelines For ICU PatientsMariana MoralesNoch keine Bewertungen
- Adult Nutrition Support HandbookDokument23 SeitenAdult Nutrition Support Handbookmajd100% (1)
- Dietary Treatments For EpilepsyDokument13 SeitenDietary Treatments For EpilepsyShahruzzaman AhmadNoch keine Bewertungen
- Topic 3 Assignment 3 Case StudyDokument8 SeitenTopic 3 Assignment 3 Case StudyErikNoch keine Bewertungen
- 02 NST Icu Intake 0007Dokument8 Seiten02 NST Icu Intake 0007anariela kityNoch keine Bewertungen
- ArpitDokument73 SeitenArpitDurgesh PushkarNoch keine Bewertungen
- Paper Telaah Jurnal Evidence Based Practice Keperawatan Kritis Dengan Judul Treatment of Patients With Severe Sepsis and Septic ShockDokument11 SeitenPaper Telaah Jurnal Evidence Based Practice Keperawatan Kritis Dengan Judul Treatment of Patients With Severe Sepsis and Septic ShockTheresia AvilaNoch keine Bewertungen
- NCM 118 - Course Time TableDokument6 SeitenNCM 118 - Course Time TableLaurence Zerna100% (1)
- Resume Dr. Akash PatelDokument8 SeitenResume Dr. Akash PatelRajvi ParmarNoch keine Bewertungen
- Emergency Laparotomy PDFDokument13 SeitenEmergency Laparotomy PDFbushra mughalNoch keine Bewertungen
- Icu (Intensive Care Unit)Dokument2 SeitenIcu (Intensive Care Unit)IrfanNoch keine Bewertungen
- Pain, Agitation and Delirium in The Intensive Care Unit: Learning ObjectivesDokument7 SeitenPain, Agitation and Delirium in The Intensive Care Unit: Learning ObjectivesVlady78Noch keine Bewertungen
- Escala PermeDokument9 SeitenEscala PermeMileniNoch keine Bewertungen
- Critical Care Environment - Design Stucture and FacilitiesDokument22 SeitenCritical Care Environment - Design Stucture and FacilitiesProf. Ramsharan MehtaNoch keine Bewertungen
- MC2021-001 2020 Ipp GP&SGDokument47 SeitenMC2021-001 2020 Ipp GP&SGRaffy BelloNoch keine Bewertungen
- Icu Scoring SystemDokument63 SeitenIcu Scoring Systemzzaw59900Noch keine Bewertungen
- Abg Interpretation Practice TestDokument9 SeitenAbg Interpretation Practice TestPatty RomeroNoch keine Bewertungen
- Mechanical Ventilation 2015Dokument18 SeitenMechanical Ventilation 2015Nauman GilaniNoch keine Bewertungen
- Oxford Textbook of Neurocritical CareDokument750 SeitenOxford Textbook of Neurocritical CareMykhailo LysianskyiNoch keine Bewertungen
- Risk FactorDokument42 SeitenRisk Factorbethelmedia100% (1)
- IPHS For 31 To 50 Bedded With Comments of Sub GroupDokument84 SeitenIPHS For 31 To 50 Bedded With Comments of Sub Groupram4uintpt50% (4)
- Diagnosis of Fluid Overload: From Conventional To Contemporary ConceptsDokument14 SeitenDiagnosis of Fluid Overload: From Conventional To Contemporary Conceptsbenitez1228Noch keine Bewertungen
- Intensive Care Unit Built Environments: A Comprehensive Literature Review (2005-2020)Dokument48 SeitenIntensive Care Unit Built Environments: A Comprehensive Literature Review (2005-2020)Indhu JayavelNoch keine Bewertungen
- Stimulasi Auditori Pada Pasien Cedera Kepala Dengan Penurunan Kesadaran Tri Wahyuni Ismoyowati Emiliana BinartiDokument6 SeitenStimulasi Auditori Pada Pasien Cedera Kepala Dengan Penurunan Kesadaran Tri Wahyuni Ismoyowati Emiliana BinartiPutri Eka MuzdhalifahNoch keine Bewertungen
- Ekstube 6Dokument8 SeitenEkstube 6Muhamad ArwaniNoch keine Bewertungen
- Acid Base BalanceDokument40 SeitenAcid Base Balancemohdmaghyreh100% (1)
- Rajivgandhi University of Health Sciences Bangalore, KarnatakaDokument19 SeitenRajivgandhi University of Health Sciences Bangalore, KarnatakaHUSSAINA BANONoch keine Bewertungen
- Bree Doran - ResumeDokument2 SeitenBree Doran - Resumeapi-546694141Noch keine Bewertungen
- 2018 Conference AbstractsDokument155 Seiten2018 Conference AbstractsBanin AbadiNoch keine Bewertungen
- Pakitang Turo: Sa Filipino 7Dokument39 SeitenPakitang Turo: Sa Filipino 7Lyth LythNoch keine Bewertungen
- Discharge GoalsDokument13 SeitenDischarge GoalsAngela Nicole MarcosNoch keine Bewertungen
- 01.03 ABG (Arterial Blood Gas) Interpretation-ROME - NRSNG Nursing CoursesDokument3 Seiten01.03 ABG (Arterial Blood Gas) Interpretation-ROME - NRSNG Nursing CoursesTurkleNoch keine Bewertungen
- Arterial Blood Gas Interpretation: Presenter-Dr. Garima Aggarwal Resident Iind Yr Department of MedicineDokument43 SeitenArterial Blood Gas Interpretation: Presenter-Dr. Garima Aggarwal Resident Iind Yr Department of Medicinefirdaus che daud100% (1)
- CMC Exam HandbookDokument18 SeitenCMC Exam HandbookNílo StárnNoch keine Bewertungen
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyVon EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyBewertung: 4.5 von 5 Sternen4.5/5 (4)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)
- Hearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIVon EverandHearts of Darkness: Serial Killers, The Behavioral Science Unit, and My Life as a Woman in the FBIBewertung: 4 von 5 Sternen4/5 (20)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsVon EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsBewertung: 4.5 von 5 Sternen4.5/5 (39)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryVon EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryBewertung: 4 von 5 Sternen4/5 (46)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingVon EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingBewertung: 4 von 5 Sternen4/5 (1138)