Beruflich Dokumente
Kultur Dokumente
Charcot Arthropathy Treatment & Management
Hochgeladen von
Zulqarnain RamliOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Charcot Arthropathy Treatment & Management
Hochgeladen von
Zulqarnain RamliCopyright:
Verfügbare Formate
1/29/12
Charcot Arthropath Treatment & Management
Charcot Arthropath Treatment & Management
Author: Mrugeshkumar Shah, MD, MPH; Chief Editor: Jason H Calhoun, MD, FACS more... Updated: Mar 25, 2011
Medical Therap
Treatment of Charcot arthropathy is primarily nonoperative. Treatment consists of 2 phases: an acute phase and a postacute phase. Management of the acute phase includes immobilization and reduction of stress.[10] Immobilization usually is accomplished by casting. Total contact casts have been shown to allow patients to ambulate while preventing the progression of deformity. Casts must be checked weekly to evaluate for proper fit, and they should be replaced every 1-2 weeks. Patients with concomitant ulceration must have their casts changed weekly for ulcer evaluation and debridement. Serial plain radiographs should be taken approximately every month during the acute phase to evaluate progress. Casting usually is necessary for 3-6 months and is discontinued based on clinical, radiographic, and dermal thermometric signs of quiescence. Other methods of immobilization include metal braces and ankle-foot orthoses (AFOs), but they may prolong healing times. Reduction of stress is accomplished by decreasing the amount of weight bearing on the affected extremity. While total non-weight bearing (NWB) is ideal for treatment, patients are often not compliant with this treatment. Studies have shown that partial weight bearing (PWB) with assistive devices (eg, crutches, walkers) also is acceptable without compromising healing time. However, full weight bearing (FWB) in the acute phase tends to lengthen total time in the cast. Healing time varies according to the location of the disease. Pattern 1, or forefoot pathology, heals in two thirds the time of pattern 3 or pattern 4. One study revealed that the mean time in a cast is 18.5 weeks, while another study showed that the acute phase lasts 12.5 weeks. Management following the removal of the cast includes lifelong protection of the involved extremity. Patient education and professional foot care on a regular basis are integral aspects of lifelong foot protection. After cast removal, patients should wear a brace to protect the foot. Many types of braces may be used, including a patellar tendon-bearing brace, accommodative footwear with a modified AFO, a Charcot restraint orthotic walker (CROW), and a double metal upright AFO.[11] Custom footwear includes extra-depth shoes with rigid soles and a plastic or metal shank. If ulcers are present, a rocker-bottom sole can be used. Also, Plastazote inserts can be used for insensate feet. This regimen may be eliminated after 6-24 months, based on clinical, radiographic, and dermal thermographic findings. Continued use of custom footwear in the postacute phase for foot protection and support is essential. The total healing process typically takes 1-2 years. Preventing further injury, noting temperature changes, checking feet every day, reporting trauma, and receiving professional foot care also are important tenets of treatment.
Surgical Therap
Surgical procedures and techniques vary based on the location of the disease and on surgeon preference and experience with Charcot arthropathy. Surgical procedures include exostosectomy of bony prominence, osteotomy, arthrodesis, screw and plate fixation, open reduction and internal fixation, reconstructive surgery, fusion with Achilles tendon lengthening, autologous bone grafting, and amputation. Patients treated with surgery have longer healing times.[10]
emedicine.medscape.com/article/1234293-treatment#showall 1/6
1/29/12
Charcot Arthropath Treatment & Management
Surgical methods can be based on Sch n's classification system. Open reduction and internal fixation should be used for an ankle with displaced fractures. Ankle arthrodesis is necessary in patients with tibiotalar destruction. In cases in which the hindfoot has avascular necrosis of the talus, a talectomy with tibiocalcaneal fusion is necessary. Arthrodesis may be necessary for patients with hindfoot involvement. For a midfoot pattern, surgical correction of rocker-bottom deformity and osteotomies for bony prominences are used. If there is an associated hindfoot/ankle equinus contracture, then a posterior release/Achilles tendon lengthening procedure is required. For forefoot patterns, patients with bony prominences or recurrent ulcerations may need a resection arthroplasty or cheilectomy. One small study found minimally invasive arthrodesis plus gradual Charcot foot correction with the Taylor spatial frame to be an effective treatment. This technique may aid in the avoidance of incomplete deformity correction, fixation failure, infections, shortening of the foot, and the use of long-term casts or braces.[12]
Follow-up
For excellent patient education resources, visit eMedicine's Diabetes Center, Sexually Transmitted Diseases Center, and Foot, Ankle, Knee, and Hip Center. Also, see eMedicine's patient education articles Diabetic Foot Care and Syphilis.
Complications
Charcot fractures that are not identified and treated properly may progress to marked joint deformity and to skin ulceration over a bony prominence. The ulceration can result in a severe infection, which may lead to amputation of the extremity. Another complication of Charcot arthropathy is foot collapse leading to the formation of a clubfoot. Another commonly seen deformity is the rocker-bottom foot, in which collapse and inversion of the plantar arch occurs. Other complications include the ossification of ligamentous structures, the formation of intra-articular and extra-articular exostoses, the collapse of the plantar arch, and the development of osteomyelitis.
Outcome and Prognosis
Outcomes for Charcot arthropathy are based on immediate diagnosis and treatment. A more favorable outcome is elicited when joints are treated within 2 weeks of injury and when there is strict adherence to weight-bearing precautions. Location of the disease also affects outcome. Forefoot arthropathies heal in less time than midfoot, hindfoot, or ankle arthropathies. Average healing times are as follows: Ankle - Mean time, 83 days, +/- 22 days Hindfoot - Mean time, 97 days, +/- 16 days Midfoot - Mean time, 96 days, +/- 11 days Forefoot - Mean time, 55 days, +/- 17 days) Surgical treatment prolongs healing time. The extent of the injury also affects healing time. The more severe the injury, the longer it takes to heal and the greater the likelihood of permanent deformity. It generally takes 1-2 years to completely heal a Charcot joint, from the active phase to quiescence.
Future and Controversies
The current mainstay of therapy for patients with Charcot arthropathy is immobilization and NWB on the affected extremity. However, other treatment options are currently being tested. One option is the use of bisphosphonates, which are potent inhibitors of bone resorption that have minimal effect on bone formation.[13, 14] This action stops the osteoclastic activity of bone breakdown, promotes healing, and decreases local inflammation. However, only a few case reports have examined this treatment as an alternative. Another therapy that is currently being researched is low-intensity ultrasound.[15] Pulsed low-intensity ultrasound has been shown to transmit micromechanical force and strains to the fracture site and to promote bone formation.
emedicine.medscape.com/article/1234293-treatment#showall 2/6
Das könnte Ihnen auch gefallen
- Mims Doctor 2020Dokument68 SeitenMims Doctor 2020Zulqarnain RamliNoch keine Bewertungen
- Corrigendum - 210422 - Guidelines On Management of Occupational Noise-Related Hearing Disorders CMPDokument112 SeitenCorrigendum - 210422 - Guidelines On Management of Occupational Noise-Related Hearing Disorders CMPZulqarnain RamliNoch keine Bewertungen
- Corrigendum - 210422 - Guidelines On Management of Occupational Noise-Related Hearing Disorders CMPDokument112 SeitenCorrigendum - 210422 - Guidelines On Management of Occupational Noise-Related Hearing Disorders CMPZulqarnain RamliNoch keine Bewertungen
- Scaffolder Erector Medical ExaminationDokument6 SeitenScaffolder Erector Medical ExaminationZulqarnain RamliNoch keine Bewertungen
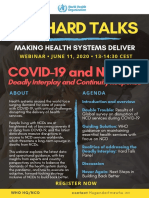
- WHO Ncd-Hard-Talks-Covid-19-And-Ncd-June2020Dokument1 SeiteWHO Ncd-Hard-Talks-Covid-19-And-Ncd-June2020Zulqarnain RamliNoch keine Bewertungen
- Medical Surveilance 2001Dokument140 SeitenMedical Surveilance 2001Mohd MustafhaNoch keine Bewertungen
- PpeDokument68 SeitenPpeoshaptss100% (1)
- Ppe Recommended PDFDokument7 SeitenPpe Recommended PDFZulqarnain RamliNoch keine Bewertungen
- Practical Obstetrics and Gynaecology Handbook For O&G Clinicians and General Practitioners - 2nd Edition (2014, World Scientific Publishing Company)Dokument843 SeitenPractical Obstetrics and Gynaecology Handbook For O&G Clinicians and General Practitioners - 2nd Edition (2014, World Scientific Publishing Company)james100% (4)
- WHO - Foodborne Disease OutbreaksDokument162 SeitenWHO - Foodborne Disease OutbreaksGabriella Breder L. LimaNoch keine Bewertungen
- Tabligh MovementDokument4 SeitenTabligh MovementZulqarnain RamliNoch keine Bewertungen
- 02 EyeanatomyDokument12 Seiten02 Eyeanatomyzafar_18325Noch keine Bewertungen
- PpeDokument68 SeitenPpeoshaptss100% (1)
- Hujjatullah BaligahDokument359 SeitenHujjatullah BaligahZulqarnain RamliNoch keine Bewertungen
- National Public Health Laboratory Test Handbook 2018 FINAL (28082018)Dokument276 SeitenNational Public Health Laboratory Test Handbook 2018 FINAL (28082018)MelvinNoch keine Bewertungen
- Ihya Ulum Al DinDokument732 SeitenIhya Ulum Al Dinwalialig100% (2)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Deep Learning Assignment 1 Solution: Name: Vivek Rana Roll No.: 1709113908Dokument5 SeitenDeep Learning Assignment 1 Solution: Name: Vivek Rana Roll No.: 1709113908vikNoch keine Bewertungen
- The Creative Bureaucracy 2Dokument45 SeitenThe Creative Bureaucracy 2IndirannaNoch keine Bewertungen
- Orpiano Vs TomasDokument2 SeitenOrpiano Vs TomasDotsNoch keine Bewertungen
- 18.CASE STUDY - Southwest AirlinesDokument23 Seiten18.CASE STUDY - Southwest AirlinesDaniel CiprianNoch keine Bewertungen
- Aron Nimzowitsch-My System & Chess Praxis-New in Chess (2016) PDFDokument1.029 SeitenAron Nimzowitsch-My System & Chess Praxis-New in Chess (2016) PDFMomin Fayzan100% (9)
- Topic Categorization Based On User Behaviour in Random Social Networks Using Firefly AlgorithmDokument5 SeitenTopic Categorization Based On User Behaviour in Random Social Networks Using Firefly AlgorithmBONFRINGNoch keine Bewertungen
- Cohort 2 Assignment Essay FinalDokument4 SeitenCohort 2 Assignment Essay Finalapi-652640066Noch keine Bewertungen
- Principles and Methods of Effective TeachingDokument5 SeitenPrinciples and Methods of Effective TeachingerikaNoch keine Bewertungen
- Contract ManagementDokument26 SeitenContract ManagementGK TiwariNoch keine Bewertungen
- HLR BasicsDokument13 SeitenHLR BasicsAyan Chakraborty75% (4)
- © The Registrar, Panjab University Chandigarh All Rights ReservedDokument99 Seiten© The Registrar, Panjab University Chandigarh All Rights Reservedshub_88Noch keine Bewertungen
- APQP TrainingDokument22 SeitenAPQP TrainingSandeep Malik100% (1)
- Tales From The Wood RPGDokument51 SeitenTales From The Wood RPGArthur Taylor100% (1)
- Financial Reporting For Financial Institutions MUTUAL FUNDS & NBFC'sDokument77 SeitenFinancial Reporting For Financial Institutions MUTUAL FUNDS & NBFC'sParvesh Aghi0% (1)
- Estoryang BinisayaDokument27 SeitenEstoryang BinisayaAngel GellaNoch keine Bewertungen
- The Meaning of LifeDokument1 SeiteThe Meaning of LifeJayas SharmaNoch keine Bewertungen
- Lesson 2 Cultural Relativism - Part 1 (Reaction Paper)Dokument2 SeitenLesson 2 Cultural Relativism - Part 1 (Reaction Paper)Bai Zaida Abid100% (1)
- A N S W e R-Accion PublicianaDokument9 SeitenA N S W e R-Accion PublicianaEdward Rey EbaoNoch keine Bewertungen
- Wdnsakn KDniend w5564Dokument8 SeitenWdnsakn KDniend w5564Jo BloNoch keine Bewertungen
- Aptitude TestDokument19 SeitenAptitude TestSANANoch keine Bewertungen
- A Skunk, A Weasel and A Rat!Dokument174 SeitenA Skunk, A Weasel and A Rat!WalliveBellair100% (1)
- Research MethodologyDokument5 SeitenResearch Methodologysonal gargNoch keine Bewertungen
- Condition Monitoring 021711 v3Dokument40 SeitenCondition Monitoring 021711 v3Kevin_INoch keine Bewertungen
- Tutorial-Midterm - CHEM 1020 General Chemistry - IB - AnsDokument71 SeitenTutorial-Midterm - CHEM 1020 General Chemistry - IB - AnsWing Chi Rainbow TamNoch keine Bewertungen
- Lesson 4 Theories of TruthDokument25 SeitenLesson 4 Theories of TruthKayeden CubacobNoch keine Bewertungen
- Spiderman EvolutionDokument14 SeitenSpiderman EvolutionLuis IvanNoch keine Bewertungen
- Presentation Management Trainee Batch VII - Mohammad Arian RahmatullahDokument8 SeitenPresentation Management Trainee Batch VII - Mohammad Arian RahmatullahMohammad Arian RahmatullahNoch keine Bewertungen
- Internal Job Posting 1213 - Corp Fin HyderabadDokument1 SeiteInternal Job Posting 1213 - Corp Fin HyderabadKalanidhiNoch keine Bewertungen
- TestDokument21 SeitenTestTri Arini TitisingtyasNoch keine Bewertungen
- Interaksi Simbolik Dalam Komunikasi BudayaDokument18 SeitenInteraksi Simbolik Dalam Komunikasi BudayaPrazzNoch keine Bewertungen