Beruflich Dokumente
Kultur Dokumente
Escherichia Coli Streptococcus Group B Haemophilus Influenzae Streptococcus Pneumoniae Neisseria Meningitides Staphylococcus Aureus
Hochgeladen von
Brent NicholsOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Escherichia Coli Streptococcus Group B Haemophilus Influenzae Streptococcus Pneumoniae Neisseria Meningitides Staphylococcus Aureus
Hochgeladen von
Brent NicholsCopyright:
Verfügbare Formate
Introduction Good morning classmates. Today we will be talking about an infectious disorder very popular among the children.
It is Meningitis. You must know that there are different types of meningitis. However, I will be talking about the most common type of this condition which is Bacterial meningitis. In this one-hour interactive discussion, I will be presenting to you concept map, which will include the pathophysiology, diagnostic exams, medical management and nursing management. Situation A: Four-year-old Donatelo was admitted to hospital due to fever, headache, neck pain and purpuric rashes on both legs. Upon assessment, the nurse asked him if theres someone in the household who is sick. Donatelo said they have a neighbor who just been admitted to the hospital because of tuberculosis. He added that 3 days prior to admission, he is afraid in light, always irritable and had one seizure episode. He believes that his previous head surgery is the reason for all the suffering he is experiencing and blames himself for the car accident. During physical examination, there Kernig and Brudzinski signs were positive. Dr. Chuca ordered a Lumbar puncture and laboratory results show: Protein= 800 g/dl .Glucose level= 38mg/dl. CSF appearance: turbid. There is an increased in the intracranial pressure thorough Intracranial pressure monitoring. WBC count= 1300/l mostly PMN. Dr. Chuca diagnosed Donatelo with Bacterial meningitis.
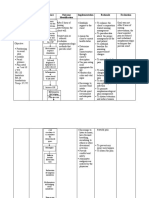
Etiologic factors: Escherichia coli Streptococcus group B Haemophilus influenzae Streptococcus pneumoniae Neisseria meningitides Staphylococcus aureus Predisposing Factors: Gender: males are more susceptible Very young age: between birth to 4 years of age Maternal factors, such as premature rupture of fetal membranes and maternal infection during the last week of pregnancy Deficiencies in the immune mechanisms Decreased leukocyte activity Immunoglobulin deficiencies Children receiving immunosuppressant drugs Lack of acquired resistance to the various etiologic organisms Preexisting CNS anomalies neurosurgical procedures or injuries sickle-cell disease Primary infections elsewhere in the body Asplenia Chronic pulmonary disease Cardiac disease Renal disease Diabetes mellitus Cerebrospinal leaks Organ transplants Signs and symptoms: Preceding respiratory or sore throat Presence of fever, chills Headache Vomiting Photophobia Stiff neck Rash Irritability Drowsiness Lethargy Muscle rigidity Seizures
Diagnostic exams Lumbar puncture (LP) - withdrawal of CSF from the subarachnoid space for analysis. It is to diagnose infection or obstruction. nursing responsibilities include proper positioning by helping child maintain position and remain still, maintaining strict asepsis, assisting with collection and transport of specimen, keeping child flat for 1 hour if ordered. Complete blood count- in meningitis, WBCs will be elevated Blood culture- done to rule out sepsis. Blood culture will be positive in cases of septicemia
Urine specific gravity- to detect oversecretion or undersecretion of antidiuretic hormone Skull X-ray examination- radiographic image of the skull that will fractures. Nursing implications include allowing a parent or family member to accompany the child since children may be afraid. If the child is unwilling or unable to stay still for the x-ray, restraint may be necessary. Computed tomography (CT)- noninvasive x-ray study that looks at tissue density and structures. Images a slice of clients tissue. It is to diagnose congenital abnormalities such as neural tube, hemorrhage, tumors, fractures. The machine is large and can be frightening to children. The procedure can be lengthy and child must remain still. If unable to do so, sedation may be necessary. Gram stain- used in determining the causative factor/ etiologic agent. Only useful to detect bacterial culture. Electroencephalogram (EEG)- measures the activity of the brain. It is to diagnose seizures and brain death. The child must remain still. If unable to do so, sedation may be necessary but should be avoided if possible because sedatives can alter the EEG reading.
Laboratory results Increased Cerebro-spinal fluid pressure (normal, 60-150 mmH20) WBC count (normal, 0-8/l): Bacteria: >1000/l (mainly PMN) Viral: 25-500/l (mainly lymphocytes) Protein (normal, 15-45 mg/dl [0.15-0.45 g/L]): Bacteria: >500mg/dl Viral: 50-500mg/dl Glucose (normal, 45-75 mg/dl [2.5-4.2 mmol/L]): Bacteria: decreased ( the bacteria feed on the glucose) Viral: normal or low Appearance of CSF Bacteria: turbid, cloudy Viral: clear or cloudy
Medical management Antibiotics Brand Name: Penicillin G Generic Name: Penicillin Action: Binds to bacterial cell wall, causing bacterial death. Nursing Responsibilities: Let the patient finish the required days and dose af the medication. Assess for clients allergies and perform skin testing before giving the medication. Corticosteroids Brand Name: Solu-Cortef Generic Name: hydrocortisone Action: Suppresses normal immune response and stops inflammatory process. Nursing Responsibilities: Provide a clean environment for the client. Isolate the patient from other patient with different disease condition to avoid the client from being infected. Analgesics Brand Name: Acetaminophen Generic Name: acetaminophen Action: Inhibits the synthesis of prostaglandins that may serve as mediator of pain and fever, primarily in the CNS. Nursing Responsibilities: Provide comfort for the patient. Provide safety and clean environment. Reduce environmental stimuli. Assess for clients level of pain. Osmotic diuretics Brand Name: Osmitrol Generic Name: mannitol Action: Increases the osmotic pressure of glomelural filtrate, thereby inhibiting reabsorption of water and electrolytes. Nursing Responsibilities: Monitor intake and output of the patient per shift. Assess for clients hydration status. Assess clients vital signs every 4 hours. Assess for the mobility and turgor of the patient.
Nursing process/ management: Assessment Explore clients current and past medical history for risk factors such as: Young age: 1 month to 5 years, with most cases in children less than 1 year of age and young adults 15 to 24 years of age Any fever or illness during pregnancy or around delivery ( for infants less than 3 months of age) Exposure to ill persons Exposure to tuberculosis Travel history History of maternal illness Recent neurosurgical procedure or head trauma Presence of a foreign body, such as shunt or a cochlear implant Immunocompromised status Close-contact living spaces such as dormitories Daycare attendance Physical Examination Observe general appearance of the client Opisthotonic position- head and neck are hyperextended to relieve discomfort. the infant may rest in this position while older child may complain of neck pain. A bulging fontanel-may be present in infant, which is often a late sign. Infant is consolable when lying still as opposed to being held. Positive Kernigs sign Positive Brudzinskis sign Presence of rash; a petechial, vesicular or macular rash may be seen. Vital signs Fluid intake and output Evaluation of lung fields and skin.
Nursing Diagnoses Altered comfort: acute pain R/T increase in intracranial pressure secondary to meningitis Risk for injury R/T reduced level of consciousness secondary to meningitis Altered thought processes R/T compression of the brain secondary to meningitis
Outcomes/ Evaluation Reduce intracranial pressure Maintaining cerebral perfusion along with treating fluid volume deficit Controlling/ preventing seizures Preventing injury that may result from altered level of consciousness or seizure activity Remain free of signs and symptoms of increased intracranial pressure Free from headache, vomiting No signs of altered level of consciousness Head circumference within normal range Absence of pain in the neck Absence of lethargy and drowsiness Adequate nutrition Intake and output will be in normal range Interrupted family processes
Interventions Initiate isolation precautions: to prevent nosocomial spread of infection. Reduction of environmental temperature and the use of cooling blankets, fans, cold compresses, and tepid baths. Avoid measures that cause shivering because it increases heat production and is therefore counterproductive as well as uncomfortable. Monitor vital signs: decreased pulse and respiratory rate and increased blood pressure or pulse pressure can indicate increased ICP. Elevate head of bed 15-30 degrees to facilitate venous return and can help to reduce ICP. Minimize environment stimuli and noise, avoid pain-producing procedures if possible: all can increase ICP. Notify MD immediately if changes in assessment are noted; early intervention is critical to prevent neurologic damage and death. Have emergency equipment ready and available: increased ICP can result in respiratory or cardiac failure. Measure specific gravity of urine: can detect an oversecretion or undersecretion of antidiuretic hormone. Assess neurologic status closely: changes in level of consciousness, signs of irritability or lethargy, changes in pupillary reaction can indicate decreased cerebral tissue perfusion. Ensure patient has patent airway and adequate oxygenation and place patient in side-lying position if possible: a patient with altered LOC may not be able to manage his secretions and is at risk for aspiration and ineffective airway clearance; providing suction and oxygenation can help ensure an open airway.
Protect patient from hurting self during seizures or changes in level of consciousness be removing environmental obstacles, easing patient to lying position, and padding side rails. With seizure activity do not insert a tongue blade or restrain patient: can lead to injury to caregiver and patient. Provide familiar sounds (voices, music): can help relieve anxiety related to changes in sensory perception, especially visual changes. Encourage nutritious diet and proper hydration according to patients preferences and ability to feed orally: to assist bodys natural defenses against infection. Teach patient/family preventive measures such as good hand washing, covering mouth and nose upon cough or sneeze, adequate disposal of used tissues: to prevent nosocomial or community spread of infection. Monitor for pain Assess patient and familys willingness to learn. Provide family with time to adjust to diagnosis: will help facilitate adjustment and ability to learn and participate in patient care. Teach in short sessions: many short sessions are found to be more helpful than one long session. Gear teaching to a level of understanding of the patient and also the family members: to ensure understanding. Provide reinforcement and rewards: help facilitate the teaching-learning process. Encourage significant others and family members to verbalize concerns related to illness, diagnosis, and prognosis: allows the nurse to identify concerns and areas where further education may be needed. Explain therapies, procedures, behaviors, and plan of care to parents: understanding the patients current status and plan of care helps decrease anxiety. Identify support system for the patient: helps nurse identify needs and resources available for coping. Collaborative Care Collaborate with physical therapy, occupational therapy: strengthen muscles and promote optimal mobility
Complications: Obstructive hydrocephalus Subdural effusions Thrombosis in meningeal veins or venous sinuses Brain abscesses Compression necrosis Deafness Blindness Weakness or paralysis of facial or other muscles of the head and neck Meningococcemia Waterhouse-friderichsen syndrome Cerebral edema and herniation Ventriculitis Hemiparesis Quadriparesis Open forum
Das könnte Ihnen auch gefallen
- Nurse Practitioner Board ReviewVon EverandNurse Practitioner Board ReviewBewertung: 5 von 5 Sternen5/5 (1)
- Neurological DisordersDokument35 SeitenNeurological DisordersUday Kumar100% (3)
- Textbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyVon EverandTextbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyNoch keine Bewertungen
- Consciousness: Alertness Cognitive PowerDokument7 SeitenConsciousness: Alertness Cognitive PowersabinNoch keine Bewertungen
- Neonatal Infections - Pathophysiology, Diagnosis, and Management 2018 PDFDokument254 SeitenNeonatal Infections - Pathophysiology, Diagnosis, and Management 2018 PDFBao NguyenNoch keine Bewertungen
- General Practitioner - Neurology MCQsDokument20 SeitenGeneral Practitioner - Neurology MCQsAsif Newaz100% (3)
- Nursing Management of PatientDokument32 SeitenNursing Management of PatientNoky KiaNoch keine Bewertungen
- Abdullahi V Pfizer Inc PDFDokument44 SeitenAbdullahi V Pfizer Inc PDFBevs DomingoNoch keine Bewertungen
- Algorithm Febrile SeizuresDokument32 SeitenAlgorithm Febrile SeizuresSilvestri Purba100% (1)
- Chapter 59: Nursing Management: Acute Intracranial Problems Lewis Et Al.: Medical-Surgical Nursing in Canada, 3rd EditionDokument14 SeitenChapter 59: Nursing Management: Acute Intracranial Problems Lewis Et Al.: Medical-Surgical Nursing in Canada, 3rd EditionlmaoheartsNoch keine Bewertungen
- Listening Jahshan OET Collection-1 PDFDokument139 SeitenListening Jahshan OET Collection-1 PDFss78% (27)
- 2017 Wise 3RD Year With KeyDokument24 Seiten2017 Wise 3RD Year With KeyAnne Lorraine BringasNoch keine Bewertungen
- Algorithm Febrile SeizuresDokument32 SeitenAlgorithm Febrile SeizuresSi Puput100% (1)
- Management of Patients With Neurologic DisordersDokument9 SeitenManagement of Patients With Neurologic DisordersJames Felix Gallano GalesNoch keine Bewertungen
- Stool Analysis and Other Body Fluid AnalysisDokument51 SeitenStool Analysis and Other Body Fluid AnalysisPutri Senna Rahayu100% (2)
- To Decrease Temperature by Means Through Evaporation and ConductionDokument11 SeitenTo Decrease Temperature by Means Through Evaporation and Conductioniaekawa100% (6)
- NURS 6531 Final Exam 2Dokument18 SeitenNURS 6531 Final Exam 2Ren PaulNoch keine Bewertungen
- SAQs PaediatricsDokument43 SeitenSAQs Paediatricss336336anl100% (1)
- Ragasa - Neurologic DisordersDokument51 SeitenRagasa - Neurologic DisordersremeroseNoch keine Bewertungen
- ENLS Meningitis and Encephalitis ProtocolDokument20 SeitenENLS Meningitis and Encephalitis ProtocolFransiskus MikaelNoch keine Bewertungen
- Rheumatic Heart DiseaseDokument14 SeitenRheumatic Heart Diseaseudaybujji100% (1)
- Neurological AssessmentDokument20 SeitenNeurological Assessmentdhanya jayan100% (1)
- Pediatric EmergencyDokument98 SeitenPediatric Emergencyian ismail100% (5)
- Listening Jahshan OET CollectionDokument194 SeitenListening Jahshan OET CollectionAKHILNoch keine Bewertungen
- Case Study MeningitisDokument20 SeitenCase Study MeningitisMitch Love100% (5)
- Hydrocephalus Lesson PlanDokument12 SeitenHydrocephalus Lesson PlanUday KumarNoch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care PlanKwini Jeyn50% (2)
- Principles of Antimicrobial TherapyDokument39 SeitenPrinciples of Antimicrobial TherapyAsthree Nur AzizahNoch keine Bewertungen
- Neurological Alterations NotesDokument12 SeitenNeurological Alterations NotesAnna TaylorNoch keine Bewertungen
- Nursing DiagnosisDokument10 SeitenNursing DiagnosisZaty ChaiyOkk100% (1)
- Care of Unconscious PatientDokument6 SeitenCare of Unconscious PatientSuparna SinghaNoch keine Bewertungen
- NCM 102 Pedia Nervous, Hema,,Renal, SkeletalDokument178 SeitenNCM 102 Pedia Nervous, Hema,,Renal, SkeletalMika SamsonNoch keine Bewertungen
- Ink NCM 110-Immunologic Response 8-23-20Dokument60 SeitenInk NCM 110-Immunologic Response 8-23-20Justin John NavarroNoch keine Bewertungen
- NewbornEmergenices2006 PDFDokument16 SeitenNewbornEmergenices2006 PDFRana SalemNoch keine Bewertungen
- Trauma in Children. Initial Assessment and ManagementDokument39 SeitenTrauma in Children. Initial Assessment and ManagementDrTushar GoswamiNoch keine Bewertungen
- Assessment and Diagnostic FindingsDokument7 SeitenAssessment and Diagnostic FindingsAlmustapha Babangida DanganiNoch keine Bewertungen
- Hypoxic Ischaemic Encepalopathy - Nicole StevensDokument38 SeitenHypoxic Ischaemic Encepalopathy - Nicole StevensAbishaNoch keine Bewertungen
- Neurological Disorders in The Pediatric Patient: Presented by Marlene Meador RN, MSN, CNEDokument57 SeitenNeurological Disorders in The Pediatric Patient: Presented by Marlene Meador RN, MSN, CNEsharepoint88Noch keine Bewertungen
- Neural Tube DefectDokument8 SeitenNeural Tube DefectReema Akberali nooraniNoch keine Bewertungen
- Huma Mir-1Dokument51 SeitenHuma Mir-1drw72409Noch keine Bewertungen
- 15yo With Lethargy and FeverDokument7 Seiten15yo With Lethargy and FeverdakewtwontonNoch keine Bewertungen
- NCP and Drug StudyDokument11 SeitenNCP and Drug StudyTonio PagaoNoch keine Bewertungen
- Simple Febrile SeizureDokument63 SeitenSimple Febrile SeizureMary Ann SacramentoNoch keine Bewertungen
- MeningitisDokument21 SeitenMeningitisSonya GodwinNoch keine Bewertungen
- Thesis On Birth AsphyxiaDokument4 SeitenThesis On Birth Asphyxiaimmkhuwhd100% (3)
- Meningitis: Coli, and Listeria Species Are The Most CommonDokument6 SeitenMeningitis: Coli, and Listeria Species Are The Most CommonSarika YadavNoch keine Bewertungen
- Guideline Summary NGC-9469: RecommendationsDokument6 SeitenGuideline Summary NGC-9469: RecommendationsIbrahim MachmudNoch keine Bewertungen
- Melbourne 14 May 2005: Case 1: Rotator Cuff InjuryDokument9 SeitenMelbourne 14 May 2005: Case 1: Rotator Cuff InjuryZweNoch keine Bewertungen
- POLIOMYELITISDokument26 SeitenPOLIOMYELITISIzhra Margate100% (1)
- Potential Complications in Unconscious PatientDokument3 SeitenPotential Complications in Unconscious PatientPandesal with EggNoch keine Bewertungen
- By Abraham Belay: Approach To ComaDokument36 SeitenBy Abraham Belay: Approach To ComaashuNoch keine Bewertungen
- HHD 9 Accident EmergencyDokument6 SeitenHHD 9 Accident Emergencymusy9999Noch keine Bewertungen
- ABC TraumaDokument27 SeitenABC TraumarikarzNoch keine Bewertungen
- Alterations in Nervous SystemDokument37 SeitenAlterations in Nervous SystemVIVIEN CONSIGNANoch keine Bewertungen
- EncephalitisDokument46 SeitenEncephalitismeenoNoch keine Bewertungen
- Prince Sultan Military College For Health SciencesDokument20 SeitenPrince Sultan Military College For Health SciencesmahaNoch keine Bewertungen
- Mechanism of TraumaDokument46 SeitenMechanism of TraumauutNoch keine Bewertungen
- 2019 IteDokument188 Seiten2019 IteBHNoch keine Bewertungen
- A 27Dokument10 SeitenA 27NestleNoch keine Bewertungen
- HYDROCEPHALUSDokument6 SeitenHYDROCEPHALUSErika CadawanNoch keine Bewertungen
- A Case Study of "Meningitis": Mary Chiles College Gastambide St. Sampaloc ManilaDokument16 SeitenA Case Study of "Meningitis": Mary Chiles College Gastambide St. Sampaloc ManilaJessa BorreNoch keine Bewertungen
- Epilepsyppt 180618175748Dokument38 SeitenEpilepsyppt 180618175748Vasu LohraNoch keine Bewertungen
- Neurology LectureDokument48 SeitenNeurology Lecturehasanatiya41Noch keine Bewertungen
- Meningitis Bacterial: EtiologyDokument22 SeitenMeningitis Bacterial: EtiologyRhima KemalaNoch keine Bewertungen
- Symptoms of Pneumonia: o o o o o o oDokument2 SeitenSymptoms of Pneumonia: o o o o o o oKathzkaMaeAgcaoiliNoch keine Bewertungen
- Neurological EmergenciesDokument47 SeitenNeurological EmergenciesStellate Repentance100% (1)
- CASEPRESDokument37 SeitenCASEPRESNathaniel GanapinNoch keine Bewertungen
- Penatalaksanaan Anestesi Pada Shaken Baby Syndrome Anesthesia Management For Shaken Baby SyndromeDokument9 SeitenPenatalaksanaan Anestesi Pada Shaken Baby Syndrome Anesthesia Management For Shaken Baby SyndromeDesta FransiscaNoch keine Bewertungen
- Care Plan Presentation On Meningitis PatientDokument20 SeitenCare Plan Presentation On Meningitis PatientDuop Jock LiemNoch keine Bewertungen
- A Normal Blood Glucose Level For Newborn Infants Is 40 MG/DL and HigherDokument8 SeitenA Normal Blood Glucose Level For Newborn Infants Is 40 MG/DL and Higherglenard-roble-1251Noch keine Bewertungen
- Ang Crocs 2Dokument59 SeitenAng Crocs 2MarufNoch keine Bewertungen
- The Neurological Exam: Mental Status ExaminationDokument13 SeitenThe Neurological Exam: Mental Status ExaminationShitaljit IromNoch keine Bewertungen
- Bacterial Meningitis in ChildrenDokument10 SeitenBacterial Meningitis in ChildrenAnny AryanyNoch keine Bewertungen
- Diagnostic Tests: Neisseria Meningitidis CapsularDokument2 SeitenDiagnostic Tests: Neisseria Meningitidis CapsularCherry Mae JasoNoch keine Bewertungen
- Infectios DiseasesDokument183 SeitenInfectios DiseasesAnonymous eson90Noch keine Bewertungen
- Clinical Aspects of Headache in HIVDokument8 SeitenClinical Aspects of Headache in HIVnatacha479Noch keine Bewertungen
- Concept Map Meningitis - TheoryDokument3 SeitenConcept Map Meningitis - Theoryapi-308767893Noch keine Bewertungen
- (10920684 - Neurosurgical Focus) Intracranial Infections - Lessons Learned From 52 Surgically Treated CasesDokument8 Seiten(10920684 - Neurosurgical Focus) Intracranial Infections - Lessons Learned From 52 Surgically Treated CasesIsmail MuhammadNoch keine Bewertungen
- Dermatology Videos by DR RihamDokument31 SeitenDermatology Videos by DR Rihamengr_shazzNoch keine Bewertungen
- Tuberculous Meningitis: A Narrative ReviewDokument10 SeitenTuberculous Meningitis: A Narrative ReviewVyom BuchNoch keine Bewertungen
- Chapter 2: Growth and DevelopmentDokument26 SeitenChapter 2: Growth and DevelopmentusamaNoch keine Bewertungen
- Manual For Lab ID, AST-Cdc, WhoDokument385 SeitenManual For Lab ID, AST-Cdc, Whopatricktiew100% (1)
- Meningitis - Introduction and ManagementDokument27 SeitenMeningitis - Introduction and ManagementAmmo KhanNoch keine Bewertungen
- Clinpharm Notes 4 TopicsDokument8 SeitenClinpharm Notes 4 TopicsALESANDRA DAWN PAYOTNoch keine Bewertungen
- Otitis Media NCPDokument3 SeitenOtitis Media NCPJames AbendanNoch keine Bewertungen
- Encephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningDokument9 SeitenEncephalitis and Aseptic Meningitis: Short-Term and Long-Term Outcome, Quality of Life and Neuropsychological FunctioningRoberto SoehartonoNoch keine Bewertungen
- Telaah JurnalDokument29 SeitenTelaah JurnalRafiqy Sa'adiy FaizunNoch keine Bewertungen
- Another DedicationDokument21 SeitenAnother DedicationFarida AdiningrumNoch keine Bewertungen
- Kernig Sign, Brudzinski Sign and Nuchal Rigidity By: PutrialishajsgDokument24 SeitenKernig Sign, Brudzinski Sign and Nuchal Rigidity By: Putrialishajsgfarah fadzilNoch keine Bewertungen