Beruflich Dokumente
Kultur Dokumente
Rhino Sinusitis Guidelines
Hochgeladen von
Navin NagarajOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Rhino Sinusitis Guidelines
Hochgeladen von
Navin NagarajCopyright:
Verfügbare Formate
COMMENTARY Open Access
Canadian guidelines for rhinosinusitis: practical
tools for the busy clinician
Shaun Kilty
Abstract
Acute bacterial rhinosinusitis (ABRS) and chronic rhinosinusitis (CRS) frequently present in clinical practice.
Guidelines for management of these conditions have been published extensively in the past. However, a set of
guidelines that addressed issues specific to the Canadian environment while offering clear guidance for first-line
clinicians was needed, and resulted in the recent publication of Canadian clinical practice guidelines for ABRS and
CRS. In addition to addressing issues specific to Canadian physicians, the presented guidelines are applicable
internationally, and offer single algorithms for the diagnosis and management of ABRS and CRS, as well as expert
opinion in areas that do not have an extensive evidence base. This commentary presents major points from the
guidelines, as well as the intended impact of the guidelines on clinical practice.
See guidelines at: http://www.aacijournal.com/content/7/1/2
Introduction
The first comprehensive Canadian clinical practice guide-
lines for acute bacterial rhinosinusitis (ABRS) and chronic
rhinosinusitis (CRS) have recently been co-published in
Allergy Asthma Clin Immunol [1] and in J Otolaryngol
Head Neck Surg [2]. Although rhinosinusitis guidelines
have been issued by European and American medical
societies over the last few years [3-6], and guidance for the
Canadian environment has appeared [7,8], the current
Canadian guidelines mark the first time that comprehen-
sive guidelines covering both ABRS and CRS appear, with
a focus on addressing issues specific to the Canadian
healthcare environment.
The term rhinosinusitis is used to denote inflamma-
tion of the sinus and nasal passages, which often occur
simultaneously due to their close location and shared
respiratory epithelium. Rhinosinusitis is common and
increasing in prevalence worldwide. It is associated with
a significant burden on healthcare services, quality of
patients lives, and lost patient productivity. The preva-
lence of acute rhinosinusitis increased from 11% (or 26
million) of American adults in 2006 [9] to nearly 13%
(over 29 million) in 2009 [10]. Nearly 7 years ago, the
economic burden of the cost of treatment was estimated
at 6 billion dollars annually in the United States [11].
Clearly, as rhinosinusitis continues to affect more indivi-
duals, the impact on patient lives and total costs will
also continue to rise.
Discussion
Because ABRS and CRS have different pathologies and
thus management strategies, it is critical that clinicians
understand these differences so appropriate treatment
can be started. However, analysis of Canadian prescrip-
tion data demonstrated nearly identical prescribing
habits for patients with ABRS and for those with CRS
[12], highlighting that differences in the treatment of
these distinct conditions were not fully appreciated. The
Canadian guidelines provide easy-to-read and practical
recommendations to assist clinicians who face patients
with symptoms of rhinosinusitis in everyday practice.
These guidelines provide specific updates on a variety of
topics, including diagnostic symptom duration and
severity, choice of treatment, appropriate testing, and
antimicrobial resistance issues, in addition to providing
useful diagnostic tools. An overview of the diagnostic
and treatment algorithms is presented in Figure 1.
ABRS diagnosis
The diagnosis of ABRS requires the duration of appro-
priate symptoms be greater than 7 days. Prior guidelines
suggest 5 days with worsening symptoms or 10 days of
persistent symptoms as the lower end of duration [3], or
Correspondence: kiltysj@gmail.com
Department of Otolaryngology-Head and Neck Surgery, The Ottawa Hospital,
University of Ottawa, ON, Canada
Kilty BMC Ear, Nose and Throat Disorders 2012, 12:1
http://www.biomedcentral.com/1472-6815/12/1
2012 Kilty; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
symptoms that persist more than 10 days after viral
symptoms present, or worsen within 10 days of initial
improvement [5]. Although symptoms of viral infections
may linger, they reach peak severity by 3 days [13,14].
Thus, the current guidelines recommend that ABRS be
considered for symptoms lasting longer than 7 days
without improvement, or for symptoms that worsens
after 5 to 7 days, or for symptoms that persist after 10
days.
A unique offering of these guidelines is the mnemonic,
PODS, to assist clinicians in recalling the major symp-
toms of ABRS. PODS stands for facial Pain/pressure/
fullness, nasal Obstruction, nasal purulence/postnasal
Discharge, and Smell alterations (hyposmia/anosmia).
For a diagnosis, at least 2 of these major symptoms
must be present, one of which must be O (obstruction)
or D (discharge). To my knowledge, this is the first set
of guidelines offering such a mnemonic for the major
diagnostic criteria of ABRS, which should help clinicians
quickly assess the information that is needed for a diag-
nosis. The guidelines also provide a discussion of pre-
diction rules that describe symptoms whose cumulative
presence increases the likelihood of bacterial infection.
In the absence of diagnostic tests, ABRS diagnosis relies
on clinical symptoms coupled with duration despite
challenges in the accuracy and specificity of signs and
symptoms.
ABRS treatment
Symptom severity plays a role in determining appropri-
ate therapeutic intervention. Previous guidelines have
defined symptom severity either on scores from a visual
analogue score [3] or based upon temperature and pain
severity [5]. The Canadian guidelines base severity by
the degree to which symptoms impair the patient. Thus,
low severity is defined as easily tolerated symptoms,
moderate severity reflects steady symptoms that are tol-
erable, and severe severity indicates that symptoms are
difficult to tolerate or interfere with sleep or daily activ-
ities. This approach does not depend on the presence of
fever, which is not included as a major symptom of
ABRS. Symptom severity is then used to determine ther-
apeutic intervention. For symptoms that are mild to
moderate in intensity, the guidelines recommend the
M
S
A8kS CkS
C C
D D
S S
C C
C C
D D
S S
S
D
WK^
C1
u C8Sn C8Sn
d
C8Sn C8Sn
lnCS
S
A
C
M M S
lnCS
l
M M S
lnCS
A
A 1MSMx
CuS C u
lnCS
A
l
S C8S
Figure 1 Overview of algorithms for ABRS and CRS.
Kilty BMC Ear, Nose and Throat Disorders 2012, 12:1
http://www.biomedcentral.com/1472-6815/12/1
Page 2 of 5
use of intranasal corticosteroids (INCS)but not antibio-
ticsas a first step in treatment. In mild to moderate
severity illness, antibiotics are reserved for patients who
fail to respond to INCS after 3 days and whose symp-
toms continue for more than 7 days. For patients pre-
senting with severe illness, INCS and antibiotics are
recommended in combination as a first step in treat-
ment. This approach thus reserves antibiotics for clear
cases of ABRS that are not resolving spontaneously.
In general, amoxicillin remains the first-line choice for
ABRS, with trimethoprim/sulfamethoxazole (TMP/SMX)
or macrolides recommended for individuals with b-lactam
allergy. However, antibiotic choice depends upon other
considerations as well, including local antimicrobial resis-
tance patterns, patient risk of resistance, and risk of com-
plications of failure due to underlying disease. For patients
with risk of resistance or complications of first-line failure,
a second-line agent (amoxicillin/clavulanic acid combina-
tions, fluoroquinolones) is recommended.
CRS diagnosis
A useful mnemonic for quick recall of major symptoms
of CRS is CPODS, standing for facial Congestion/fullness,
facial Pain/pressure, nasal Obstruction/blockage, nasal
Drainage, and Smell dysfunction (hyposmia/anosmia). At
least two of the CPODS symptoms must be present for 8
to 12 weeks, along with documented inflammation of the
nasal mucosa or paranasal sinuses. The duration of
symptoms for diagnosis has generally been proposed as
12 weeks [3,5]. However, Canadian guidelines align with
others in recommending an 8 week minimum for CRS
diagnosis [15]. The guidelines also highlight the insis-
tence of clinical or radiologic evidence in addition to
clinical symptoms in order to make a diagnosis of CRS.
Hence, a diagnosis requires the presence of 2 or more
CPODS, present for 8 to 12 weeks, plus objective evi-
dence using either endoscopy or computed tomography.
A recent study of EP3OS symptom criteria confirmed by
endoscopy reported moderate reliability of symptom-
based diagnosis for CRS, and found stability between
geographic regions [16]. These findings concur with an
earlier study that found that endoscopy was critical to
increase the specificity, and positive and negative predic-
tive values for symptom-based diagnosis of CRS [17].
Although symptom-based diagnosis had poor specificity
by itself, diagnostic accuracy improved dramatically when
combined with an objective finding (odds ratio for CRS
improved from 1.1 to 4.6 [95% CI, 2.3-9.2]).
The presence or absence of nasal polyps is used to
further categorize disease. The presence of bilateral
polyps in the middle meatus characterizes CRS with
nasal polyps (CRSwNP), while the lack of polyps consti-
tutes CRS without nasal polyps (CRSsNP). The guide-
lines provide detailed description of the physical
examination, including adequate tools for visual rhino-
scopy assessments and description of clinical signs,
which should provide clinicians with a better under-
standing of useful signs and symptoms.
CRS treatment
Because CRS is primarily an inflammatory disease with
unknown contributions from bacteria, cytokines, leuko-
cytes, and tissue remodeling, treatment is based upon
use of INCS as monotherapy or as adjunct therapy with
antibiotics. Before initiating one of these treatments,
predisposing and contributing conditions should be
identified and treated. Conditions that are thought to
contribute to CRS include allergic rhinitis, asthma, cili-
ary dysfunction, immune dysfunction, lost ostia patency,
aspirin-exacerbated respiratory disease, and cystic
fibrosis.
Nasal or oral corticosteroids are used with or without
antibiotics for initial treatment of CRSsNP. When pre-
scribed, antibiotics should be a second-line agent with
broad-spectrum coverage (ie, amoxicillin-clavulanic acid
inhibitors, fluoroquinolones) and duration of therapy
should be longer than for ABRS.
For CRSwNP, a course of topical INCS and short
courses of oral steroids are used. Antibiotics are not
recommended for CRSwNP unless there are symptoms
suggesting infection.
Role of antibiotics
These guidelines discuss concerns of increasing rates of
antibiotic resistance, with the emergence of penicillin,
macrolide, and multi-drug resistant S. pneumoniae. Ele-
vated rates of b-lactamase-producing H. influenzae and
M. catarrhalis have also been reported, with conse-
quences for antibiotic choice. Although antibiotic resis-
tance rates increased between 1988 and 2005, some rates
have stabilized in the 5-year period between 2000 and
2005, including rates for ciprofloxacin, penicillin, and
TMP/SMX resistance [18,19]. However, resistance rates
continue to increase for erythromycin and tetracycline,
and penicillin nonsusceptibility remains elevated. Resis-
tance and nonsusceptibility rates also showed regional
differences. Similar patterns of variable and growing anti-
biotic resistance are of global concern, with the World
Health Organization dedicating World Health Day 2011
to the topic of antimicrobial resistance. Because of the
trends in resistance rates, guidelines advise judicious use
of antibiotic therapy and awareness of related issues, with
appropriate selection of therapy for clinical situation.
Ancillary therapy, testing, and prevention
Saline irrigation has emerged in these guidelines as a
strong recommendation from the experts despite limited
evidence. This expert endorsement is in line with the
Kilty BMC Ear, Nose and Throat Disorders 2012, 12:1
http://www.biomedcentral.com/1472-6815/12/1
Page 3 of 5
increased recognition of the benefits of saline therapy
over the last 5 to10 years in the management of sinona-
sal disease. Multiple studies report the benefit of saline
irrigation in patients with CRS [20-22], ARS [23], and in
allergic, acute and chronic rhinosinusitis [24]. The use
of saline irrigation as adjunct therapy is primarily based
upon reported symptomatic improvement and its good
safety profile.
The expert panel endorsed allergy testing in cases of
recurrent episodes of ABRS or for CRS as a potential
contributing condition to these diseases. Indeed, studies
have reported that over half of patients with recurrent
ARS or with CRS tested positive for allergies [25,26].
Whether allergy treatment helps minimize symptoms in
these cases is not known, but knowledge and avoidance
of identified allergens remains a prudent approach none
the less.
Prevention of illness is a recommendation. The impor-
tance of hand washing is highlighted as fundamental to
reduce viral transmission and prevent the development
of ABRS and acute exacerbations of CRS. Although stu-
dies are lacking, the expert recommendation strongly
encourages educating patients regarding strategies to
reduce the likelihood of contracting a viral illness.
Guideline rationale and method
The Canadian clinical practice guidelines for acute and
chronic rhinosinusitis were designed foremost to be a
valuable tool for first-line clinicians, particularly primary
care providers. As such, the guidelines are evidence
based, make specific recommendations, and comprehen-
sively address both ABRS and CRS in single algorithms
for each, while also providing the practitioner with the
opinion of clinical experts.
Previous Canadian guidelines were either outdated or
did not provide guidance for practitioners in best prac-
tices management of patients with ABRS or CRS. The
current guidelines present strategies relevant for Cana-
dian practitioners to negotiate the unique aspects of
their healthcare system, while remaining sufficiently
general to benefit an international audience. Thus, in
situations that might arise in the Canadian healthcare
system, such as delays in obtaining a computed tomo-
graphy scan or specialist referral, action points during
this waiting period are presented. However, the state-
ments and discussions throughout the document focus
on aspects central to ABRS and CRS, and apply in any
healthcare environment. Advances in the pathobiology
of these disease entities are discussed, along with the
current status of treatment options.
The guidelines were constructed using an evidence-
based strategy and present an evidence strength rating,
plus a second rating that reflects the endorsement level
of the multidisciplinary group of experts who represent
medical fields involved in treating this multifaceted con-
dition. This latter rating is particularly useful in areas
where rigorous trials are lacking in quality or number.
The guidelines were further reviewed and endorsed by
the Association of Medical Microbiology and Infectious
Disease Canada, Canadian Society of Allergy and Clini-
cal Immunology, Canadian Society of Otolaryngology-
Head and Neck Surgery (CSO-HNS), Canadian Associa-
tion of Emergency Physicians, and the Family Physicians
Airways Group of Canada.
The Canadian guidelines provide clear definitions and
discussion of ABRS and CRS. The diagnostic and treat-
ment flow diagrams are complete, providing detail and
ease of flow within a single algorithm for ABRS and for
CRS. The guidelines were designed to improve the
usability for general practitioners and family medicine
physicians. In addition, these guidelines provide current,
clear information for the optimal management of CRS-a
disease entity for which advances in understanding its
pathobiology and effective management strategies con-
tinue to evolve. The steps involved in the diagnosis,
management, and referral of ABRS and CRS, coupled
with strength of recommendation ratings, should help
arm general practitioners with the information necessary
to improve the management of their patients with symp-
toms of rhinosinusitis.
Conclusion
The knowledge base of ABRS and CRS pathology and
management continues to grow and evolve as the role
of pathogens are discerned, antimicrobial resistance
rates change, and treatment strategies are improved.
The Canadian guidelines recognize this changing envir-
onment and provide a solid foundation for future devel-
opments. The guidelines are a much-needed user-
friendly tool for busy physicians who want to quickly
grasp the appropriate methods of diagnosis and manage-
ment of ABRS and CRS. The inclusion of mnemonic
devices to aid in diagnosis, succinct algorithms for each
disease entity, and expert opinion to aid where studies
are lacking create a new level of utility for rhinosinusitis
guidelines. Physicians who desire to understand the cur-
rent state of the pathologies and treatment approaches
for ABRS and CRS will benefit from these guidelines,
and as an extension, their patients will benefit as well.
List of abbreviations
ABRS: acute bacterial rhinosinusitis; CRS: chronic rhinosinusitis; INCS:
intranasal corticosteroids; TMP/SMX: trimethoprim/sulfamethoxazole.
Acknowledgements and funding
The author thanks Lynne Isbell, PhD for editorial assistance, which was
funded by CSO-HNS.
Kilty BMC Ear, Nose and Throat Disorders 2012, 12:1
http://www.biomedcentral.com/1472-6815/12/1
Page 4 of 5
Competing interests
The author declares that they have no competing interests.
Received: 25 March 2011 Accepted: 1 February 2012
Published: 1 February 2012
References
1. Desrosiers M, Evans GA, Keith PK, Wright ED, Kaplan A, Bouchard J,
Ciavarella A, Doyle PW, Javer AR, Leith ES, et al: Canadian clinical practice
guidelines for acute and chronic rhinosinusitis. Allergy Asthma Clin
Immunol 7:2.
2. Desrosiers M, Evans GA, Keith PK, Wright ED, Kaplan A, Bouchard J,
Ciavarella A, Doyle PW, Javer AR, Leith ES, et al: Canadian clinical practice
guidelines for acute and chronic rhinosinusitis. J Otolaryngol Head Neck
Surg 2011, 40(Suppl 2):S99-193.
3. Fokkens W, Lund V, Mullol J: European position paper on rhinosinusitis
and nasal polyps 2007. Rhinol Suppl 2007, 1-136.
4. Scadding GK, Durham SR, Mirakian R, Jones NS, Leech SC, Farooque S,
Ryan D, Walker SM, Clark AT, Dixon TA, et al: BSACI guidelines for the
management of allergic and non-allergic rhinitis. Clin Exp Allergy 2008,
38:19-42.
5. Rosenfeld RM, Andes D, Bhattacharyya N, Cheung D, Eisenberg S,
Ganiats TG, Gelzer A, Hamilos D, Haydon RC, Hudgins PA, et al: Clinical
practice guideline: adult sinusitis. Otolaryngol Head Neck Surg 2007, 137:
S1-31.
6. Scadding GK, Durham SR, Mirakian R, Jones NS, Drake-Lee AB, Ryan D,
Dixon TA, Huber PA, Nasser SM: BSACI guidelines for the management of
rhinosinusitis and nasal polyposis. Clin Exp Allergy 2008, 38:260-275.
7. Desrosiers M, Frenkiel S, Hamid QA, Low D, Small P, Carr S, Hawke M,
Kirkpatrick D, Lavigne F, Mandell L, et al: Acute bacterial sinusitis in adults:
management in the primary care setting. J Otolaryngol 2002, 31(Suppl
2):2S2-14.
8. Diagnosis and management of acute bacterial sinusitis: adults. 2008
Update. [http://www.topalbertadoctors.org/cpgs.php?sid=15&cpg_cats=56].
9. Pleis J, Lucas J: Summary health statistics for U.S. adults: National Health
Interview Survey, 2007. National Center for Health Statistics. Vital Health
Stat 2009, 10.
10. Pleis JR, Ward BW, Lucas JW: Summary health statistics for U.S. adults:
National Health Interview Survey, 2009. Hyattsville, MD: National Center
for Health Statistics; 2010, Series 10, No. 249.
11. Anand VK: Epidemiology and economic impact of rhinosinusitis. Ann Otol
Rhinol Laryngol Suppl 2004, 193:3-5.
12. IMS Health: Canadian Disease and Therapeutic Index (CDTI) database.
2006.
13. Gwaltney JM Jr, Hendley JO, Patrie JT: Symptom severity patterns in
experimental common colds and their usefulness in timing onset of
illness in natural colds. Clin Infect Dis 2003, 36:714-723.
14. Gwaltney JM Jr: Rhinovirus infection of the normal human airway. Am J
Respir Crit Care Med 1995, 152:S36-39.
15. Slavin RG, Spector SL, Bernstein IL, Kaliner MA, Kennedy DW, Virant FS,
Wald ER, Khan DA, Blessing-Moore J, Lang DM, et al: The diagnosis and
management of sinusitis: a practice parameter update. J Allergy Clin
Immunol 2005, 116:S13-47.
16. Tomassen P, Newson RB, Hoffmans R, Lotvall J, Cardell LO,
Gunnbjornsdottir M, Thilsing T, Matricardi P, Kramer U, Makowska JS, et al:
Reliability of EP3OS symptom criteria and nasal endoscopy in the
assessment of chronic rhinosinusitisa GA(2) LEN study. Allergy 2011,
66:556-561.
17. Bhattacharyya N, Lee LN: Evaluating the diagnosis of chronic
rhinosinusitis based on clinical guidelines and endoscopy. Otolaryngol
Head Neck Surg 2010, 143:147-151.
18. Green K, McGreer A, Church D, Weiss K, Davidson R, Hoban D, Kibsey P,
Kuhn M, Toye B, Pong-Porter S, et al: Trends in antimicrobial resistance in
Canadian strains of Streptococcus pneumoniae, 1988-2003. 43rd Annual
Interscience Conference on Antimicrobial Agents and Chemotherapy 9/14/2003
Chicago; 2003.
19. Green K, Pong-Porter S, Plevneshi A, McGeer A, Low EE, Canadian Bacterial
Surveillance Network: Trends in antimicrobial prescribing and
pneumococcal resistance, Canada, 1993-2005. 46th Annual Interscience
Conference on Antimicrobial Agents and Chemotherapy 9/27/2006 San
Francisco; 2006.
20. Pynnonen MA, Mukerji SS, Kim HM, Adams ME, Terrell JE: Nasal saline for
chronic sinonasal symptoms: a randomized controlled trial. Arch
Otolaryngol Head Neck Surg 2007, 133:1115-1120.
21. Harvey R, Hannan SA, Badia L, Scadding G: Nasal saline irrigations for the
symptoms of chronic rhinosinusitis. Cochrane Database Syst Rev 2007,
CD006394.
22. Ottaviano G, Marioni G, Staffieri C, Giacomelli L, Marchese-Ragona R,
Bertolin A, Staffieri A: Effects of sulfurous, salty, bromic, iodic thermal
water nasal irrigations in nonallergic chronic rhinosinusitis: a
prospective, randomized, double-blind, clinical, and cytological study.
Am J Otolaryngol 2011, 32:235-239.
23. Hauptman G, Ryan MW: The effect of saline solutions on nasal patency
and mucociliary clearance in rhinosinusitis patients. Otolaryngol Head
Neck Surg 2007, 137:815-821.
24. Ural A, Oktemer TK, Kizil Y, Ileri F, Uslu S: Impact of isotonic and
hypertonic saline solutions on mucociliary activity in various nasal
pathologies: clinical study. J Laryngol Otol 2009, 123:517-521.
25. Emanuel IA, Shah SB: Chronic rhinosinusitis: allergy and sinus computed
tomography relationships. Otolaryngol Head Neck Surg 2000, 123:687-691.
26. Alho OP, Karttunen R, Karttunen TJ: Nasal mucosa in natural colds: effects
of allergic rhinitis and susceptibility to recurrent sinusitis. Clin Exp
Immunol 2004, 137:366-372.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1472-6815/12/1/prepub
doi:10.1186/1472-6815-12-1
Cite this article as: Kilty: Canadian guidelines for rhinosinusitis: practical
tools for the busy clinician. BMC Ear, Nose and Throat Disorders 2012 12:1.
Submit your next manuscript to BioMed Central
and take full advantage of:
Convenient online submission
Thorough peer review
No space constraints or color gure charges
Immediate publication on acceptance
Inclusion in PubMed, CAS, Scopus and Google Scholar
Research which is freely available for redistribution
Submit your manuscript at
www.biomedcentral.com/submit
Kilty BMC Ear, Nose and Throat Disorders 2012, 12:1
http://www.biomedcentral.com/1472-6815/12/1
Page 5 of 5
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Anatomy and Physiology of PlacentaDokument5 SeitenAnatomy and Physiology of PlacentaAdrianne Basa100% (1)
- Guidelines For Prescribing EyeglassesDokument18 SeitenGuidelines For Prescribing Eyeglassesratujelita100% (1)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
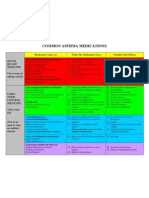
- Common Asthma MedicationsDokument1 SeiteCommon Asthma MedicationsHeart of the Valley, Pediatric CardiologyNoch keine Bewertungen
- Tall StatureDokument24 SeitenTall StaturedianmutiaNoch keine Bewertungen
- Closed Chain Exercises: Dominic S. Adolfo, PTRPDokument56 SeitenClosed Chain Exercises: Dominic S. Adolfo, PTRPEric Carlos YumulNoch keine Bewertungen
- SAMPLE FDAR CHARTING PainDokument1 SeiteSAMPLE FDAR CHARTING Painjpm100% (1)
- Prenatal CareDokument3 SeitenPrenatal CareYolanda Dwi OktaviyaniNoch keine Bewertungen
- Therapeutic CommunicationDokument82 SeitenTherapeutic CommunicationYvette Vallejo100% (2)
- HI KPI GuidelinesDokument65 SeitenHI KPI Guidelinesi_kostadinovicNoch keine Bewertungen
- MC-55-157-001 - 1-E Asg-120u Ug PDFDokument56 SeitenMC-55-157-001 - 1-E Asg-120u Ug PDFSiti NurhadijahNoch keine Bewertungen
- FY 1 Antimicrobial PrescriptionDokument10 SeitenFY 1 Antimicrobial Prescriptiongus_lionsNoch keine Bewertungen
- TITLE-class Diagram For Hospital Management SystemDokument2 SeitenTITLE-class Diagram For Hospital Management SystemShivam JhaNoch keine Bewertungen
- Boy: - 2. Bus: - 3. Box: - 4. Mouse: - 5. Child: - 6. BabyDokument3 SeitenBoy: - 2. Bus: - 3. Box: - 4. Mouse: - 5. Child: - 6. BabyMurni Abu BakarNoch keine Bewertungen
- Asthalin InhalerDokument5 SeitenAsthalin InhalerRajib MandalNoch keine Bewertungen
- Drug Studies (Levodopa, Ropinirole, Rivastigmine Tatrate, Glucerna)Dokument12 SeitenDrug Studies (Levodopa, Ropinirole, Rivastigmine Tatrate, Glucerna)KBDNoch keine Bewertungen
- Ulcerative Colitis 1. Chief ComplaintDokument5 SeitenUlcerative Colitis 1. Chief Complaintdrnareshkumar3281Noch keine Bewertungen
- Post Partum HemorrhageDokument40 SeitenPost Partum HemorrhageGita GirsangNoch keine Bewertungen
- Ch02 Costing Out Nursing ServicesDokument26 SeitenCh02 Costing Out Nursing ServicesRicardo CanalesNoch keine Bewertungen
- Comfort Room PDFDokument1 SeiteComfort Room PDFPixaaaNoch keine Bewertungen
- MSN FP6216 ForsythKathryn Assessment4 2Dokument6 SeitenMSN FP6216 ForsythKathryn Assessment4 2NbiNoch keine Bewertungen
- What Documents Do You Need After A Blood Transfusion?: BT Checklist 1Dokument5 SeitenWhat Documents Do You Need After A Blood Transfusion?: BT Checklist 1Edelweiss Marie CayetanoNoch keine Bewertungen
- Cleft Lip and PalateDokument2 SeitenCleft Lip and PalateTracy100% (1)
- Dentinogenesis ImperfectaDokument4 SeitenDentinogenesis Imperfectamirfanulhaq100% (1)
- Koo Quay Keong V Ooi Peng Jin London Lucien (2016) 5 SLR 0130Dokument16 SeitenKoo Quay Keong V Ooi Peng Jin London Lucien (2016) 5 SLR 0130a b cNoch keine Bewertungen
- Cerumen Management PDFDokument10 SeitenCerumen Management PDFHimawan WidyatmikoNoch keine Bewertungen
- Manual of Basic Techniques For A Health Laboratory (Part1) - WHODokument114 SeitenManual of Basic Techniques For A Health Laboratory (Part1) - WHOcholinchuchuNoch keine Bewertungen
- Times Leader 03-17-2013Dokument77 SeitenTimes Leader 03-17-2013The Times LeaderNoch keine Bewertungen
- GLUMODokument8 SeitenGLUMOZhayree R.Noch keine Bewertungen
- Cesarean SectionDokument73 SeitenCesarean Sectionkalsoom sahibzadaNoch keine Bewertungen
- Clostridium Difficile Infection and Fecal BacteriotherapyDokument9 SeitenClostridium Difficile Infection and Fecal BacteriotherapyAnonymous nEC4alrPjGNoch keine Bewertungen