Beruflich Dokumente
Kultur Dokumente
Potential of Electronic Personal Health Records: Analysis
Hochgeladen von
Gareth YeungOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Potential of Electronic Personal Health Records: Analysis
Hochgeladen von
Gareth YeungCopyright:
Verfügbare Formate
ANALYSIS
Potential of electronic personal health records
Novel methods for helping patients to access and manage their personal electronic health data are emerging in the UK and internationally. Claudia Pagliari, Don Detmer, and Peter Singleton examine their potential benefits and challenges
Public demand for flexible access to health information and services is growing, encouraged by internet trends and policies promoting patient rights and empowerment.1 In parallel, unprecedented global investment in healthcare information and communication technologies has been dominated by efforts to implement electronic health records, which promise improved quality and efficiency through better maintenance and availability of patient data.2 There is considerable international interest in the potential of electronic personal health records to bridge these agendas, and NHS HealthSpace is set to become the worlds first fully national system, although its capabilities are still limited in comparison with some European and US examples. We consider the potential of electronic personal health records and factors that are likely to influence their adoption in the UK, drawing on a new report from the Nuffield Trust.3
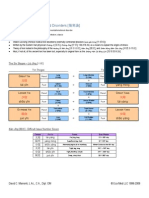
What are electronic personal health records? Although no universally agreed definition of an electronic personal health record exists,4 it has been described as an electronic application through which individuals can access, manage and share their health information in a private, secure and confidential environment.5 Models vary in the extent to which the content of the record and rights of access are controlled by the patient or the healthcare provider, the range of tools that accompany it, and their interactivity. Simpler models include patient generated health and lifestyle records that are stored and managed using personal computer or web applications, and passive access to provider held records through waiting room kiosks, the internet, or digital copy (such as on a CD or smart card). However, personal health record systems are becoming increasingly complex (box 1). Some are integrated with providers information systems to combine personal record keeping, access to current electronic health records, and a range of information and communications functions. For example, patients of the US managed care organisation Kaiser Permanente have access to HealthConnectOnline, which offers records of allergies, immunisations, future appointments, diagnoses, instructions from past visits, and laboratory results as well as allowing patients to book appointments, reorder prescriptions, and communicate with healthcare professionals by email (figure).
330
Claudia Pagliari senior lecturer in primary care, Division of Community Health Sciences (GP Section), University of Edinburgh, Edinburgh EH8 9DX Don Detmer professor of medical education, Public Health Sciences, University of Virginia, PO Box 800717, Charlottesville, VA 22908, USA Peter singleton principal research fellow, Centre for Health Informatics and Multiprofessional Education, University College London, London N19 5LW Correspondence to: C Pagliari claudia.pagliari@ed.ac.uk Accepted: 28 May 2007
Box 1 | Potential functions of electronic personal health records ccess to providers electronic clinical record (summary or A detailed)eg history, drugs, test results Personal health organiser or diaryeg clinics, doctors, tests, dates, non-prescribed treatments, scanned documents Self management supporteg care plans, graphing of symptoms, passive biofeedback, tailored instructive or motivational feedback, decision aids, or reminders Secure patient-provider communication for booking appointments, reordering prescriptions, or seeking advice (eg patient-doctor email) Links to static or interactive information about illness, treatments, or self care Links to sources of supporteg patient organisations or virtual peer networks Capture of symptom or health behaviour databy self report or objective monitoring through electronic devices (fixed or portable)
Complex online personal records are also being used in Europe. The LifeSensor product (www. us.lifesensor.com/lsn/content/e4529/index_usa. html), which is available in Germany, Switzerland, Austria, and Bulgaria, allows patients to store and manage information about their current health status, medical history, results, images, and documents and also to authorise access for selected healthcare team members or caregivers to view, add, or update
Example of portal for electronic personal health records from the US
BMJ | 18 August 2007 | VoluMe 335
ANALYSIS
Box 2 | Current UK experience with electronic personal health records Primary care Online access to the full electronic primary care record is being piloted in practices associated with a major system supplier. 7 Patients of some eligible practices also have access to online appointment booking, prescription reordering, and secure email. (www. emis-online.com/products/access/) Waiting room kiosks providing secure access to records and related patient information have been introduced in several general practices and are now available commercially (www. emis-online.com/products/health-information-portal/) Some practices have offered patients copies of their electronic record on CD or USB memory stick for several years8 Smart cards are currently being marketed, on to which patients can upload their general practice record, for a fee, and view it using personal computing software (www. healthecard.co.uk) Access to record via mobile phone and BlackBerry smart phone is also being piloted9 (www. ehiprimarycare.com/news/item.cfm?ID=2148) Secondary care Patient portals offering access to more specialised records, some with a range of additional features, exist or are being developed in several areas, including: Nephrology (www.renalpatientview.org) Paediatric intensive care (www.babylink.info/Edinburgh/BabyLink/Intro_page.aspx) Diabetes (www.dmag.org.uk/bird/aboutthisproject.asp) Maternity care (www.nhshealthquality.org/nhsqis/229.html) Patient-provider email and remote submission of symptoms to electronic health records are also being tested in both sectors
and interactivity are beginning to emerge. While most have been driven by pioneering clinical enthusiasts, commercial providers are beginning to enter this market, offering opportunities to scale up these developments for wider delivery (box 2).
What are the possible benefits and for whom? Electronic personal health records have the potential to empower patients through greater access to personal data, health information, and communications tools, which may aid self care, shared decision making, and clinical outcomes. They may increase patient safety through exposing diagnostic or drug errors, recording non-prescribed medicines or treatments, or increasing the accessibility of test results or drug alerts. They may also reduce geographical barriers to patient care and act as a point of record integration, particularly in fragmented health systems, thus improving continuity of care and efficiency.10 11 Although the number and quality of studies remains limited, existing research suggests improvements in communication and trust between patients and professionals, confidence in self care, compliance in chronic disease, and accuracy of records.12 -14 Patients particularly value online reordering of prescriptions, laboratory results, disease management plans, trend charts, drug lists, and secure messaging.5 Surveys indicate that most patients would like to be able to access their health records.5 15 16 However, the most frequent users of electronic personal health records, and those for whom the greatest benefits can be expected, are likely to be patients with long term conditions, who have the most need to track their illness and treatments, and patients experiencing episodic periods of care or treatment that generate new needs for information or communication (such as in vitro fertilisation).5 17 The emergence of mobile and wireless applications that allow remote submission of data to a shared record offer new possibilities for patient monitoring and real time decision support. Additionally, electronic records may help to promote partnership between carers and health professionals through sharing information, or allow relatives to monitor the care and progress of elderly parents or children in hospital from a distance. Factors influencing UK adoption and effectiveness Privacy and security Anxieties around security and confidentiality have been expressed in most studies of patient attitudes to personal electronic records, particularly in regard to mental and sexual health data. This does not seem to have been a barrier where access to general practice records has been tried in the UK 8 12 14; however, some patients may wish to keep sensitive information off the central NHS record (called the spine). 18 Although encryption technologies can help to prevent unauthorised access, the risk of privacy invasions may be greatest at the family level, whether the intent is supportive or malign (for example, in spousal abuse), which is difficult to control for.19 Growing experience
331
information, although the system is not directly linked to provider records. In the future, the European Union electronic health insurance card may enable patients to access their online personal health record.6 HealthSpace (www.healthspace.nhs.uk/) is a secure online personal health organiser available to all patients in England. The system was initially launched in 2003 to store health notes generated by patients. However, its functions have since increased to include selection and booking of hospital appointments; storage and charting of health indicators such as blood pressure, peak flow, or weight; a calendar with the option to generate email reminders; a database of NHS contacts; and links to online health information. By the end of next year patients will be able to access their NHS Summary Care Recorda snapshot of the general practice record documenting allergies, adverse reactions, and drug treatment. Although HealthSpace will not provide access to detailed care records, clinicians can add data to the summary record with the patients agreement. Other features under consideration include allowing patients to enter their needs or preferences, such as for wheelchair access or translators; greater use of text and email alerting; and enhanced tools for patients with chronic disease. The link with NHSDirect Online (www.nhsdirect.nhs. uk) also offers possibilities for integrating electronic consulting and education in the future. Although HealthSpace promises a national solution to electronic personal health records, it will be some time before its full potential is realised. Compatible developments are taking place independently in several UK clinical settings. These have mainly focused on providing passive access to records, although systems with additional functionality
BMJ | 18 August 2007 | VoluMe 335
ANALYSIS
of online services in other sectors and traditionally high levels of trust in healthcare professionals are likely to help ease concerns about confidentiality.
Digital divide Electronic personal health records have the potential to contribute to health inequalities through uneven internet access, although rising ownership of mobile phones and digital TV may help to ameliorate this if developers include these alternative media. Attention also needs to be paid to usability and training in order to overcome access disparities resulting from poor technical skillsfor example, among elderly people. If these problems are effectively addressed, such records may reduce healthcare exclusion through flexible access to information and services.20 Choice of model Although patients may welcome passive access to records, the greatest benefits are likely to come from multifunctional, interactive systems that are integrated with providers record systems and can support education, self care, and communication with the health service.5 However, this increased utility may decrease security, and patients will have to decide whether this risk is acceptable for them.3 It also creates an imperative for standards to ensure transparency of contributorship and access. Growing availability and use of digital health monitoring devices may create new sources of data that can be included in the record, although this information is unlikely to be beneficial unless clinicians are available to interpret and respond to it.13 In view of individuals differing requirements from an electronic personal health record and the associated security issues, HealthSpaces cautious approach to access and interactivity is appropriate. Systems offering more comprehensive patient records or interactive support tools are likely to be pursued as optional supplements to HealthSpace, ideally integrating with local general practice or disease specific records systems. It is unclear whether wholly patient managed records will be adopted because the NHS is in a unique position to create joined-up health records for all citizens, reducing the advantages of patient managed systems seen in more disaggregated healthcare systems such as in the US. The business case for personal electronic records in the UK has not been well established, and it remains to be seen which optional services patients and local care providers will be prepared to pay for. However, evidence that the UK is faring worse than comparable Western countries in meeting patients wishes for easy access to their records suggests an unmet demand.16 technical considerations Incompatability between different systems and databases remains a barrier to integrated records, although this will diminish with the adoption of consistent technology and data standards. Further work is required to ensure effective management of interactivity between patient and provider records
332
SummArY PoINtS
Online versions of personal health records that allow patients to manage their health data are emerging in the US and Europe Implementation of NHS HealthSpace is increasing awareness and provision in the UK Electronic personal health records may improve the quality, safety, and efficiency of care Key challenges include balancing security against utility and integrating diverse data sources and systems
and the balance between live and historical data. Methods of effectively managing interfaces between independent systems and HealthSpace will also need to be established.
People and organisational factors To realise their potential, electronic personal health records must be integrated within care processes. This will require efforts to develop policies, conventions, and incentives for using such records as well as changes in attitudes and expectations regarding appropriate modes of transaction and the rebalancing of information and status differentials in the doctorpatient relationship. Although no adverse effects have yet been reported in UK pilots, some patients may be distressed by what they read in their electronic health record.21 Healthcare professionals will need to be sensitive in their use of clinical terms and delay entering threatening diagnoses or test results until after speaking to the patient. Public education on the value of internet hygiene and password secrecy will also encourage more secure and appropriate use of online records. Professionals and patients should be involved in the design, development, implementation, and evaluation to generate a sense of ownership and ensure that systems meet users needs and are easy to operate. More immediately, measures to increase awareness of the potential value of personal health records to patients and the NHS are needed if these systems are to be adopted in the UK. Future priorities Current views on the value and risks of electronic records are highly polarised in the UK.22 23 Studies comparing responses to alternative models of personal health records in diverse consumer groups may help to shed light on acceptable boundaries and trade-offs and hence suggest ways of tailoring such systems to patients needs. Ethnographic studies of usage by patients with different clinical and access needs would also be of value. Evidence of the impact of electronic personal health records on clinical, safety, economic, and psychosocial outcomes is urgently required. Although research conducted in other countries is useful, implementation of technology is highly context dependent and research within the UK is essential to inform strategic decision making. As the first fully nationalised electronic personal health records system, the implementation of NHS HealthSpace offers unique opportunities to inform the evidence base on this topic.
Contributors and sources: CP chairs the Edinburgh and Lothian eHealth Research Network. DD is president and chief executive officer of the American Medical Informatics Association. PS is a senior associate of the Judge Business School, University of Cambridge, and director of Cambridge Health Informatics Limited. All are actively involved in health informatics research, with longstanding interests in electronic personal health records. CP drafted the article, with input from DD and PS. All cowrote the Nuffield Trust report on which this article draws, which was based on a workshop organised by CP and facilitated by DD with PS as rapporteur.. CP is guarantor. Funding: The Nuffield Trust.
BMJ | 18 August 2007 | VoluMe 335
ANALYSIS
Competing interests: None declared. Provenance and peer review: Not commissioned, externally peer reviewed.
1 Cayton H. Introduction. In: Better information, better choices, better health. London: Department of Health, 2004. www. dh.gov.uk/PolicyAndGuidance/PatientChoice/Choice/ BetterInformationChoicesHealth/BetterChoicesArticle/fs/ en?CONTENT_ID=4123252&chk=/BMoN%2B. 2 World Health Organization. Building foundations for ehealth: progress of member states. Geneva: WHO, 2006. www.who.int/ ehealth/resources/en. 3 Pagliari C, Detmer D, Singleton P. Electronic personal health records: emergence and implications for the UK. London: Nuffield Trust, 2007. www.nuffieldtrust.org.uk/publications/detail. asp?id=0&PRid=267. 4 National Committee on Vital and Health Statistics. Personal health records and personal health record systems: a report and recommendations. Washington: Department of Health and Human Services, 2006. www.ncvhs.hhs.gov/0602nhiirpt.pdf. 5 Connecting for Health. Connecting Americans to their healthcare. final report of the working group on policies for electronic information sharing between doctors and patients. New York: Markle Foundation, 2004. www.connectingforhealth.org/resources/final_phwg_ report1.pdf. 6 Clarke JL, Meiris DC, Nash DB. Electronic personal health records come of age. Am J Med Qual 2006;21(suppl 3):5-15S. 7 100 practices to rollout patient access on the net. E-Health Insider 2007 Feb 16. www.ehiprimarycare.com/news/item.cfm?ID=2488. 8 Harris C, Boaden R. Patient held electronic medical records at the Hadfield Medical Centre. Evaluation report. Manchester: Manchester School of Management, 2003. 9 Now doctors offer health help by text. SMS News 2004 Nov 20. http://sms-news.tm4b.com/email-446.php. 10 Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health 11 12 13
14 15 16 17 18 19 20 21 22 23
records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc 2006;13:121-6. Richards T. My illness, my record. BMJ 2007;334:510. Pyper C, Amery J, Watson M, Crook C. Patients experiences when accessing their on-line electronic patient records in primary care. Br J Gen Pract 2004;54:38-43. Ross SE, Moore LA, Earnest MA, Wittevrongel L. Providing a webbased online medical record with electronic communication capabilities to patients with congestive heart failure: randomized trial. J Med Internet Res 2004;6(2):e12. Honeyman A, Cox B, Fisher B. Potential impacts of patients access to their electronic records. Inform Primary Care 2005;13:55-60. National Programme for Information Technology. The public view on electronic health records. London: Department of Health, 2003. www. dh.gov.uk/assetRoot/04/05/50/46/04055046.pdf. Coulter A. Engaging patients in their healthcare. Oxford: Picker Institute Europe, 2006. www.pickereurope.org/Filestore/ Publications/Six_country_study_with_ISBN_web.pdf. Tuil WS, ten Hoopen AJ, Braat DD, de Vries Robbe PF, Kremer JA. Patient-centred care: using online personal medical records in IVF practice. Hum Reprod 2006;21:2955-9. Powell J, Fitton R, Fitton C. Sharing electronic health records: the patient view. Inform Primary Care 2006;14:55-7. McKinstry BH. Vulnerable people have most to lose from online access. BMJ 2007;334:599. Gustafson DH, McTavish FM, Stengle W, Ballard D, Hawkins R, Shaw BR, et al. Use and impact of ehealth system by low-income women with breast cancer. J Health Commun 2005;10(suppl 1):195-218. Bloch S, Riddell CE, Sleep TJ. Can patients safely read their psychiatric records? Implications of freedom of information legislation. Med J Aust 1994;161:665-6. Privacy GP calls records opt out pledge a decoy. E-Health Insider 2007 Mar 13. www.ehiprimarycare.com/news/item.cfm?ID=2536. Winfield W. For patients sake dont boycott e-health records. BMJ 2007;335:158.
medical education research remains the poor relation
Research into medical education is stagnating and urgently needs the resources to become more rigorous and relevant say mathew todres, Anne Stephenson, and roger Jones
The requirement that clinical practice should be based on the best available evidence has been paralleled by calls for medical education to become more evidence based.1-3 This has resulted, among other initiatives, in the establishment of the Best Evidence for Medical Education (BEME) Collaboration4 and the Campbell Collaboration, an off-shoot of the Cochrane Collaboration. The BEME initiative includes dissemination of best evidence to support medical education and the encouragement of a culture capable of nurturing more rigorous and better funded research. Evidence from the United States suggests such nurturing is much needed. In 2004, Carline analysed reports of medical education research in two major North American journals (Academic Medicine and Teaching and Learning in Medicine) and found that only a minority of studies were supported by external research grants.3 She was critical about the quality, rigour, and generalisability of most of these studies. Her concerns were echoed last year by Chen and
BMJ | 18 August 2007 | VoluMe 335
Mathew todres, research associate, Anne Stephenson, director of community education Roger Jones, Wolfson professor of general practice Department of General Practice and Primary Care, Kings College London School of Medicine, London SE11 6SP Correspondence to: R Jones roger.jones@kcl.ac.uk Accepted: 4 June 2007
colleagues,5 who advocated moving the focus of medical education research from learners to patient oriented clinical outcomes, thus increasing the relevance and its likely attractiveness to funders. A review of 290 medical education studies published during 2002 and 2003 found that only one quarter had received external funding; the median amount of
table 1 | Details of medical education research published in three journals during 2004-5
No (%) of studies (n=387) Study design Observational, cross sectional Longitudinal cohort Before and after studies Other Focus of research Undergraduate medical curriculum Continuing medical education Postgraduate medical training Other 267 (69) 31 (8) 31 (8) 58 (15) 240 (62) 85 (22) 43 (11) 19 (5) 333
Das könnte Ihnen auch gefallen
- Cognitive Informatics: Reengineering Clinical Workflow for Safer and More Efficient CareVon EverandCognitive Informatics: Reengineering Clinical Workflow for Safer and More Efficient CareKai ZhengNoch keine Bewertungen
- Health informatics: Improving patient careVon EverandHealth informatics: Improving patient careBCS, The Chartered Institute for ITBewertung: 3 von 5 Sternen3/5 (1)
- CHN 7 & 8 - E-LearningDokument66 SeitenCHN 7 & 8 - E-LearningCristina AdolfoNoch keine Bewertungen
- Text 2Dokument9 SeitenText 2Alvin Josh CalingayanNoch keine Bewertungen
- Medical Informatics Activity No.1Dokument3 SeitenMedical Informatics Activity No.1leomillmendiolaNoch keine Bewertungen
- Ways of Storing Patients' Health RecordDokument2 SeitenWays of Storing Patients' Health RecordRainer FlormataNoch keine Bewertungen
- Tihp It 012610Dokument7 SeitenTihp It 012610api-258667648Noch keine Bewertungen
- Legal and Ethical Aspects of Patient SafetyDokument11 SeitenLegal and Ethical Aspects of Patient SafetyAyesha SarwerNoch keine Bewertungen
- Benefits of Computer Use in Health Care Systems PDFDokument3 SeitenBenefits of Computer Use in Health Care Systems PDFAnonymous DlESilj50% (4)
- Order 2298121 Describe The Major Sources of The Health Data US and InterDokument2 SeitenOrder 2298121 Describe The Major Sources of The Health Data US and InterreubenNoch keine Bewertungen
- Tizon, R. - Assignment in NCM 112Dokument4 SeitenTizon, R. - Assignment in NCM 112Royce Vincent TizonNoch keine Bewertungen
- An Assessment of Manual Medical SystemDokument40 SeitenAn Assessment of Manual Medical SystemDimple SalesNoch keine Bewertungen
- Iot For PatientsDokument5 SeitenIot For PatientsSilas SuryawijayaNoch keine Bewertungen
- Compusoft, 2 (3), 65-72Dokument8 SeitenCompusoft, 2 (3), 65-72Ravi Tyagi TyagiNoch keine Bewertungen
- Jndegwa EhrDokument13 SeitenJndegwa Ehrapi-551332616Noch keine Bewertungen
- Cs5038 The Electronic Society: Lecture: EhealthDokument34 SeitenCs5038 The Electronic Society: Lecture: EhealthgopiNoch keine Bewertungen
- Nursing Informatics FinalsDokument7 SeitenNursing Informatics FinalsAlyNoch keine Bewertungen
- NCM 104 Community Health Nursing 1: Bachelor of Science in NursingDokument8 SeitenNCM 104 Community Health Nursing 1: Bachelor of Science in NursingMargarette GeresNoch keine Bewertungen
- NursingDokument11 SeitenNursingNdung'u Wa Mumbi100% (1)
- 5 Benefits of Technology in HealthcareDokument2 Seiten5 Benefits of Technology in HealthcareCHUAH TZE YEE MoeNoch keine Bewertungen
- Bari 11Dokument104 SeitenBari 11etsabayomiNoch keine Bewertungen
- Module 14Dokument5 SeitenModule 14camille nina jane navarroNoch keine Bewertungen
- Electronic Medical RecordDokument10 SeitenElectronic Medical RecordPrem Deep100% (1)
- A Tablet Computer Application For Patients To Participate in Their Hospital CareDokument8 SeitenA Tablet Computer Application For Patients To Participate in Their Hospital CareSteveEpsteinNoch keine Bewertungen
- Concept of Health Information ExchangeDokument3 SeitenConcept of Health Information ExchangeカマットダリルNoch keine Bewertungen
- Winkelman 2005Dokument9 SeitenWinkelman 2005Mathilda UllyNoch keine Bewertungen
- C C C 3 3 J JDokument30 SeitenC C C 3 3 J JmrchilliciousNoch keine Bewertungen
- Benefits of Iclinicsys in The Rural Health Unit of Lupi, Camarines SurDokument5 SeitenBenefits of Iclinicsys in The Rural Health Unit of Lupi, Camarines SurattyleoimperialNoch keine Bewertungen
- Importance of Information and Statistics in Field of Pharmacy (00000031833)Dokument7 SeitenImportance of Information and Statistics in Field of Pharmacy (00000031833)Ruien KhorNoch keine Bewertungen
- Healthcare HXZEAL2 ZD8Dokument42 SeitenHealthcare HXZEAL2 ZD8FMTech ConsultsNoch keine Bewertungen
- gjmbsv3n3spl 14Dokument25 Seitengjmbsv3n3spl 14areeb khanNoch keine Bewertungen
- Adebukola - IEEE FormatDokument8 SeitenAdebukola - IEEE FormatKelechi OdoemenaNoch keine Bewertungen
- Jurnal 1Dokument10 SeitenJurnal 1dinidinayNoch keine Bewertungen
- What Is Nursing InformaticsDokument3 SeitenWhat Is Nursing InformaticsRose JoyNoch keine Bewertungen
- Tizon, R. - Assignment in NCM 112Dokument4 SeitenTizon, R. - Assignment in NCM 112Royce Vincent TizonNoch keine Bewertungen
- Consumer and Patient Use of Computers For HealthDokument7 SeitenConsumer and Patient Use of Computers For HealthAnjo Pasiolco CanicosaNoch keine Bewertungen
- Clinical Data RepositoriesDokument5 SeitenClinical Data RepositoriesvivianschuylerNoch keine Bewertungen
- Electronic Health Record Research PaperDokument5 SeitenElectronic Health Record Research Paperef71d9gw100% (1)
- Aplikasi TI Dalam Kehidupan Sehari2Dokument20 SeitenAplikasi TI Dalam Kehidupan Sehari2Indah Dwi RiyantiNoch keine Bewertungen
- EHR Assignment Group1Dokument10 SeitenEHR Assignment Group1Abebe ChekolNoch keine Bewertungen
- Telepsychiatry in The 21 Century: Transforming Healthcare With TechnologyDokument17 SeitenTelepsychiatry in The 21 Century: Transforming Healthcare With TechnologyEngr Gaddafi Kabiru MarafaNoch keine Bewertungen
- 2009 It Medical ResearchDokument10 Seiten2009 It Medical ResearchMansoor Ali ShaikNoch keine Bewertungen
- Tablanza-Finals Activity 1 (Lab)Dokument3 SeitenTablanza-Finals Activity 1 (Lab)trust nobodyNoch keine Bewertungen
- Ncm110lec Act1Dokument14 SeitenNcm110lec Act1shahdmagrani59Noch keine Bewertungen
- Y2k Project Work On Emr (New)Dokument114 SeitenY2k Project Work On Emr (New)Otunuya Chukwudi Henry EngrNoch keine Bewertungen
- HCI 540 Final PaperDokument10 SeitenHCI 540 Final PaperJulian CorralNoch keine Bewertungen
- Health Informatics: A Roadmap For Autism Knowledge Sharing: Content/uploads/2009/04/oberleitner-Final PDFDokument4 SeitenHealth Informatics: A Roadmap For Autism Knowledge Sharing: Content/uploads/2009/04/oberleitner-Final PDFLisa_WNoch keine Bewertungen
- Review of Related LiteratureDokument6 SeitenReview of Related LiteratureSkyla FiestaNoch keine Bewertungen
- Issues in International Health Policy: Electronic Health Records: An International Perspective On "Meaningful Use"Dokument18 SeitenIssues in International Health Policy: Electronic Health Records: An International Perspective On "Meaningful Use"Sevi Cephy ONoch keine Bewertungen
- Medical Professionals Are Obligated To Protect The Data and Confidentiality of Their PatientsDokument4 SeitenMedical Professionals Are Obligated To Protect The Data and Confidentiality of Their PatientsKrishelle Kate PannigNoch keine Bewertungen
- Leakage of Electronic Medical Record - Threat To PrivacyDokument382 SeitenLeakage of Electronic Medical Record - Threat To PrivacyNandhini RaviNoch keine Bewertungen
- Ethical Practice in Telehealth and TelemedicineDokument5 SeitenEthical Practice in Telehealth and TelemedicineThaysa LimaNoch keine Bewertungen
- Contemporary Presentation CHDokument44 SeitenContemporary Presentation CHapi-546505804Noch keine Bewertungen
- Role of Information Technology in MedicineDokument7 SeitenRole of Information Technology in MedicineFahadghaznavi100% (1)
- Bnaic 2007Dokument7 SeitenBnaic 2007Perry GrootNoch keine Bewertungen
- An Assessment of Manual Medical Record System of Fr. Simpliciano Academy Inc. School Year 2018-2019Dokument66 SeitenAn Assessment of Manual Medical Record System of Fr. Simpliciano Academy Inc. School Year 2018-2019Dimple SalesNoch keine Bewertungen
- NURSING INFORMATICS Community Health ApplicationsDokument6 SeitenNURSING INFORMATICS Community Health ApplicationsThirdy Aquino100% (2)
- Electronic Health Record Literature ReviewDokument5 SeitenElectronic Health Record Literature Reviewafmzadevfeeeat100% (1)
- Group # - 1Dokument4 SeitenGroup # - 1Astra JoyNoch keine Bewertungen
- Privacy Law, Data Sharing Policies, and Medical Data: A Comparative PerspectiveDokument41 SeitenPrivacy Law, Data Sharing Policies, and Medical Data: A Comparative PerspectiveHung NguyenNoch keine Bewertungen
- New Microsoft Word DocumentDokument3 SeitenNew Microsoft Word DocumentHazim YusoffNoch keine Bewertungen
- CraniomaDokument7 SeitenCraniomaSophia BeecherNoch keine Bewertungen
- Saunders, Et Al (2017)Dokument9 SeitenSaunders, Et Al (2017)uki arrownaraNoch keine Bewertungen
- Master Techniques in Orthopaedic SurgeryDokument1.031 SeitenMaster Techniques in Orthopaedic Surgerysasa0687100% (6)
- Lesson Plan On Minor Disorders During Pregnancy Its Management 1Dokument20 SeitenLesson Plan On Minor Disorders During Pregnancy Its Management 1Bhawna Joshi100% (6)
- Krok 2 2002-2003 SurgeryDokument23 SeitenKrok 2 2002-2003 SurgeryAli ZeeshanNoch keine Bewertungen
- ABC Quality and Patient Saftey Workshop FinalDokument68 SeitenABC Quality and Patient Saftey Workshop Finalyousrazeidan1979Noch keine Bewertungen
- Introduction To HemostasisDokument16 SeitenIntroduction To HemostasisRaiza RuizNoch keine Bewertungen
- Biomedical Equipment Technology Bet1Dokument1 SeiteBiomedical Equipment Technology Bet1Rufaida HussainNoch keine Bewertungen
- DR - Neimy Novitasari. SpsDokument56 SeitenDR - Neimy Novitasari. Spscindy ramadhaniNoch keine Bewertungen
- 7 Essential Steps of CPRDokument2 Seiten7 Essential Steps of CPRBea YmsnNoch keine Bewertungen
- Impared NursesDokument11 SeitenImpared Nursesapi-240352043Noch keine Bewertungen
- 傷寒論 Shang Han LunDokument3 Seiten傷寒論 Shang Han LunDave Mainenti97% (30)
- Biology Final Exam Grade 9Dokument2 SeitenBiology Final Exam Grade 9Yesha Shah100% (1)
- Antenatal Care: Muhammad Wasil Khan and Ramsha MazharDokument55 SeitenAntenatal Care: Muhammad Wasil Khan and Ramsha MazharmarviNoch keine Bewertungen
- Kizilarslanoglu 2016Dokument7 SeitenKizilarslanoglu 2016EviNoch keine Bewertungen
- Páginas Desdepharmacotherapy Casebook 10th Ed.Dokument61 SeitenPáginas Desdepharmacotherapy Casebook 10th Ed.Glo VsNoch keine Bewertungen
- HYPOTHYROIDISMDokument11 SeitenHYPOTHYROIDISMVarun SinghNoch keine Bewertungen
- MI090717 F 2. Systemic MycosesDokument44 SeitenMI090717 F 2. Systemic Mycosesapi-19922507100% (4)
- 5,600 Residents Tested: Case SummaryDokument3 Seiten5,600 Residents Tested: Case SummaryPeterborough ExaminerNoch keine Bewertungen
- Ibuprofen 150mg + Paracetamol 500mg (Combodex)Dokument15 SeitenIbuprofen 150mg + Paracetamol 500mg (Combodex)ddandan_2Noch keine Bewertungen
- The Effect of Mangosteen (Garcinia Mangostana) Rind in The Blood Glucose Levels of Adult Patients With Type 2 Diabetes MellitusDokument4 SeitenThe Effect of Mangosteen (Garcinia Mangostana) Rind in The Blood Glucose Levels of Adult Patients With Type 2 Diabetes MellitusFiqoh Puteri FauziNoch keine Bewertungen
- Case Study.... Group-BDokument33 SeitenCase Study.... Group-BNazmul HossainNoch keine Bewertungen
- 07 - NDP Diving Emergency Assistance Plan SampleDokument2 Seiten07 - NDP Diving Emergency Assistance Plan Sample12scribd123Noch keine Bewertungen
- Devoir de Synthèse N°2 2011 2012 (Lycée Ali Bourguiba Bembla)Dokument4 SeitenDevoir de Synthèse N°2 2011 2012 (Lycée Ali Bourguiba Bembla)ferchichi halimaNoch keine Bewertungen
- BLS Aha - 2010 Refresher Course For Junior Clerks 2015Dokument28 SeitenBLS Aha - 2010 Refresher Course For Junior Clerks 2015Kalpana ShahNoch keine Bewertungen
- 1-Diabetes Package - PO2693771771-269Dokument6 Seiten1-Diabetes Package - PO2693771771-269KishoreNoch keine Bewertungen
- Objectives For Critical Care RotationDokument9 SeitenObjectives For Critical Care Rotationsteviestevie333Noch keine Bewertungen
- Guided Prep Pack - Neet Mds 2021-22Dokument13 SeitenGuided Prep Pack - Neet Mds 2021-22Annu SharmaNoch keine Bewertungen
- Diagnostic Criteria Decision Tree PDFDokument2 SeitenDiagnostic Criteria Decision Tree PDFNor Nadia ZakariaNoch keine Bewertungen