Beruflich Dokumente
Kultur Dokumente
1070 Full
Hochgeladen von
Aura PalasOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
1070 Full
Hochgeladen von
Aura PalasCopyright:
Verfügbare Formate
Effect of Body Position Changes on Pulmonary Gas Exchange in Eisenmengers Syndrome
JULIO SANDOVAL, PEDRO ALVARADO, MARIA LUISA MARTNEZ-GUERRA, ARTURO GMEZ, ANDRS PALOMAR, SONIA MEZA, EFRN SANTOS, and MARTN ROSAS
Cardiopulmonary Department, Ignacio Chavez National Institute of Cardiology, Mexico City, Mexico
Preliminary studies on sleep of patients with congenital heart disease and Eisenmengers syndrome (ES) at our institution demonstrated nocturnal worsening arterial unsaturation, which appeared to be a body positionrelated phenomenon. To investigate the potential effect of body position on gas exchange in ES, we carried out a prospective study of 28 patients (mean age, 34.8 11.7 yr) with established ES due to congenital heart disease. In every patient, arterial blood gases were performed during both sitting and supine positions under three different conditions: room air, while breathing 100% oxygen, and after breathing oxygen at a flow rate of 3 L/min through nasal prongs. Alveolar oxygen pressure (PaO2) for the calculation of alveolararterial oxygen tension differences (AaPO2) was derived from the alveolar gas equation using PaCO2 and assuming R 1. We used paired t test, repeated-measures two-way ANOVA with Bonferronis test, and regression analysis. From sitting to supine position on room air, there was a significant decrease in PaO2 (from 52.5 7.5 to 47.5 5.5 mm Hg; p 0.001) and SaO2 (from 86.7 4.6 to 83.3 4.9%; p 0.001), both of which were corrected by nasal O2 (to 68.2 21 mm Hg and to 92 4%, respectively, p 0.005). PaCO2 and pH remained unchanged. The magnitude of the change in PaO2 correlated with the change in AaPO2 on room air (r 0.77; p 0.01) but not with the change in AaPO2 on 100% oxygen. It is concluded that in adult patients with ES there is a significant decrease in PaO2 and SaO2 when they change from the sitting to . the supine position. A ventilation-perfusion ( V/Q) distribution abnormality and/or a diffusion limitation phenomenon rather than an increase in true shunt may be the mechanisms responsible for this finding. The response to nasal O2 we observed warrants a trial with long-term nocturnal oxygen therapy in these patients. Sandoval J, Alvarado P, Martnez-Guerra ML, Gmez A, Palomar A, Meza S, Santos E, Rosas M. Effect of body position changes on pulmonary gas exchange in EisenAM J RESPIR CRIT CARE MED 1999;159:10701073. mengers syndrome.
Preliminary studies on sleep of patients with congenital heart disease at our institution demonstrated worsening arterial unsaturation at night in patients with Eisenmengers syndrome (ES). This worsening nocturnal unsaturation did not appear to be related to any particular stage of sleep, but rather it appeared to be a body positionrelated phenomenon. The effect of body position on gas exchange has been extensively studied and characterized in normal people (1, 2) as well as in different clinical conditions, such as obesity (3, 4), pulmonary arteriovenous fistula (5), patent foramen ovale (6), and liver disease (7, 8), but it has not been described in patients with ES. Worsening hypoxemia associated with supine position in patients with congenital heart disease and ES could be important because it might deleteriously influence the course of the pulmonary vascular remodeling and pulmonary hypertension
as well as the systemic response to hypoxia, which are characteristic of this disease. To better define this potentially deleterious phenomenon, we prospectively investigated the effect of body position changes on gas exchange in a group of adult patients with congenital heart disease and Eisenmengers syndrome.
METHODS
We studied 28 adult patients in whom the diagnosis of congenital heart disease with ES had been previously established on the basis of clinical, electrocardiography, echocardiography, pulmonary function testing, hematology, and right heart catheterization findings. None of the patients had a body weight more than 120% of the ideal (9), and all had smoked less than one cigarette or equivalent a day for less than a year of their lives. The patients were studied in a stable condition as defined by the absence of heart failure and/or respiratory infection in the 12 wk prior to the study, and most of them were born and are residents of Mexico City or places nearby (mean altitude: 2,211 568 m). All procedures were approved by our local committee for clinical investigation. They were explained to the patients, and their written consent was obtained. Arterial blood gas (ABG) measurements were performed in every patient at rest, first in the sitting and then after in the supine position, under three different and consecutive conditions (lasting 20 min each): (1) while breathing room air; (2) while breathing 100% oxygen; and (3) while breathing oxygen through nasal
(Received in original form December 12, 1996 and in revised form October 12, 1998) Correspondence and requests for reprints should be addressed to Julio Sandoval, M.D., F.A.C.C., Chief, Cardiopulmonary Department, Instituto Nacional de Cardiologa Ignacio Chvez, Juan Badiano No. 1, Tlalpan 14080, Mxico D.F., Mexico. E-mail: sandoval@compuserve.com.mx Am J Respir Crit Care Med Vol 159. pp 10701073, 1999 Internet address: www.atsjournals.org
Sandoval, Alvarado, Martnez-Guerra, et al.: Gas Exchange in Eisenmengers Syndrome
prongs at a rate of 3 L/min. A fraction of inspired oxygen (FIO2) of 1.0 was provided through a non-rebreathing system that included a twoway valve (model 1400; Hans-Rudolph, Kansas City, MO) and a large-capacity Douglas bag. Arterial blood samples were withdrawn from a radial artery catheter and immediately analyzed in a gas analyzer (model 1306; Instrumentation Laboratories, Lexington, MA). Great care was taken to obtain the blood sample anaerobically, and also to calibrate the blood gas electrode at high PO2. In patients with an isolated patent ductus arteriosus defect, the blood samples for ABG measurements were taken from the dorsalis pedis artery. Alveolar PO2 for the calculation of the alveolararterial oxygen tension differences (AaPO2) was derived from the alveolar gas equation (10) as PaO2 [(PB 47) FIO2] PaCO2/R, where PaO2 is the alveolar oxygen pressure and PB is the measured barometric pressure. R was assumed to be equal to 1. Lung diffusion capacity was not measured. For statistical analysis we used paired t test, repeated measures two-way ANOVA with Bonferronis test, and regression analysis (11). We correlated the gas exchange findings with clinical, functional, and one stanhemodynamic variables. Results are expressed as mean dard deviation (SD).
1071
capacity less than 80% predicted) and three patients had mild airway obstruction (FEV1/FVC less than 70% predicted). A combined pattern of pulmonary restriction and airway obstruction was present in the remaining two patients. Most patients had arterial hypoxemia or at least an increased AaPO2 on room air. PaCO2 was slightly elevated in only two of the patients, and the arterial pH was normal. Normal values for arterial blood gases in Mexico City are: PaO2 67.5 2.5 mm Hg; 32.2 2.5 mm Hg; pH 7.33 to 7.43 (12). As a PaCO2 group, the patients had a variable degree of secondary erythrocytosis as evident by an abnormally elevated hematocrit value of 60 7.9%, a hemoglobin level of 19 2.4 g/dl, and a red blood cell count of 6.8 million per cubic millimeter (13).
Effect of Body Position on Gas Exchange
RESULTS
Demographic, Pulmonary Function, and Hemodynamic Variables
There were 18 females and 10 males with a mean age of 34.8 11.7 yr. The spectrum of cardiac anatomic diagnosis in the studied patients was as follows: isolated ventricular septal defect (VSD 10), isolated atrial septal defect (ASD 5), isolated patent ductus arteriosus (PDA 8), and one patient had an aorto-pulmonary window (APW 1). Some of the patients had a combined cardiac abnormality; two patients had VSD plus PDA, one patient had ASD plus PDA, and one patient with PDA also had a patent foramen ovale. Pulmonary function testing had been done less than 1 yr prior to the study in 26 patients, and the results are shown in Table 1. Static and dynamic pulmonary volumes were normal in 15 of the 26 patients. Six patients had a mild to moderate degree of pulmonary restriction (vital capaticy and total lung
Results regarding the effect of body position on gas exchange are shown in Table 2. As a whole, PaO2, SaO2, and AaPO2 were significantly affected by changing from sitting to supine position as well as by the different FIO2 (two-way ANOVA), while other variables such as PaCO2 and pH remained practically unchanged. When breathing room air and changing from the sitting to the supine position, there is a significant decrease in both arterial oxygen tension and arterial oxygen saturation (paired t test; p 0.05). Less marked modifications in SaO2 occurred with the change in body position when the patients were breathing oxygen. It is important to point out that the worsening hypoxemia and arterial oxygen unsaturation that occurred in the supine position while breathing room air was corrected by the administration of oxygen by nasal prongs at a rate of 3 L/min/; from 47.5 5.5 to 68.2 21 mm Hg and from 83.3 4.9 to 91.8 4%. The magnitude of the decrease in PaO2 from sitting to supine was not the same in all patients. As illustrated in Figure 1, there is a significant negative correlation between the baseline sitting PaO2 and the magnitude of the change in PaO2 from sit0.73; p 0.01). In general, the patients ting to supine (r with a lower calculated baseline veno-arterial shunt were the ones to have a greater decrease in PaO2 with change in position. Also, the magnitude of the change in PaO2 from sitting to
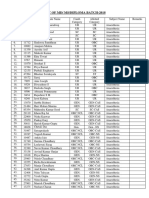
TABLE 1 PULMONARY FUNCTION AND HEMODYNAMIC DATA
Number of Patients Outside of Limits of Normality 8 9 10 5 22 3 0 23 6 8 21 0 5 21 0 21
TABLE 2 EFFECT OF BODY POSITION ON GAS EXCHANGE IN EISENMENGERS SYNDROME
Condition Sitting 52.5 33.1 7.41 86.7 80 28 190 32.4 7.41 97.9 507 317 71.7 33 7.42 93 7.7 3.7 0.02 4.5 3.7 7 131 4.4 0.04 2.6 4 130 22 4.2 0.03 4.1 Supine 47.5 33.8 7.41 83.3 79.6 32 163 32.3 7.41 97.7 507 343 68.2 34.1 7.41 91.8 5.5 3.9 0.03 4.9 4 6 110 5.2 0.04 2.4 5 109 2 4.5 0.03 4 * p Value 0.001 0.241 0.514 0.001 0.406 0.001 0.012 0.847 0.474 0.757 0.850 0.013 0.089 0.016 0.025 0.057
n Pulmonary function test VC, % predicted FEV1, % predicted FEF2575, % predicted TLC, % predicted PaO2, mm Hg PaCO2, mm Hg Arterial pH VD/VT, % Hemodynamic variables RAP, mm Hg RVEDP, mm Hg PAP, mm Hg PCWP, mm Hg CI, L/min per m2 PVRI, U/m2 SAP, mm Hg Rp/Rs 26 26 23 22 26 26 26 26 21 21 21 11 21 21 21 21
Mean 79 73.5 58 92 54 32.5 7.40 34 4.3 6.5 74.5 6 3.54 23.5 82.5 0.92
SD 20 19 24 18 9 4.5 0.03 24 3.8 4.5 16 4 1.22 9.7 7.5 0.21
Definition of abbreviations: CI cardiac index; PAP mean pulmonary artery pressure; PCWP pulmonary capillary wedge pressure; PVRI pulmonary vascular resistance index; RAP right atrial pressure; Rp/Rs pulmonary/systemic resistance ratio; RVEDP right ventricular end-diastolic pressure; SAP systemic arterial pressure; TLC total lung capacity; VC vital capacity; VD/VT physiologic dead space.
Room air: PaO2, mm Hg PaCO2, mm Hg Arterial pH SaO2, % PAO2, mm Hg AaPO2, mm Hg FIO2 100% PaO2, mm Hg PaCO2, mm Hg Arterial pH SaO2, % PAO2, mm Hg AaPO2, mm Hg Nasal O2 (3 L/min) PaO2, mm Hg PaCO2, mm Hg Arterial pH SaO2, %
Definition of abbreviations: AaPO2 inspired oxygen fraction. * ANOVA and paired t test (11).
alveolararterial oxygen pressure difference; FIO2
1072
AMERICAN JOURNAL OF RESPIRATORY AND CRITICAL CARE MEDICINE
VOL 159
1999
supine position significantly correlated with the magnitude of 0.77; the change in the AaPO2 while breathing room air (r p 0.01), but not during 100% oxygen breathing (r 0.36; p NS). The correlation between baseline sitting PaO2 and hematocrit was poor, although statistically significant (r 0.38; p 0.05). No significant correlation was found between the magnitude of the positional changes in PaO2 and arterial oxygen saturation and the other clinical, hematology, and prior (diagnostic) functional and hemodynamic variables.
DISCUSSION
It has been established that in normal subjects assumption of the supine position causes gravitational redistribution of flow and ventilation to pendant dorsal portions, often with short term favorable functional alterations in the overall V /Q ratio and the alveolar-arterial oxygen tension differences (1, 2). It has also been documented that the supine position may favorably affect gas exchange in clinical conditions such as liver cirrhosis with portal hypertension and in patent foramen ovale (68), or deleteriously as in obesity (3, 4). Although lung function has been previously studied in Eisenmengers syndrome (14, 15), we are not aware of previous studies exploring the effect of body position on gas exchange in these patients. The results of the present study showed that in adult patients with congenital heart disease and Eisenmengers syndrome there is a significant decrease in PaO2 and SaO2 when they change from the sitting to the supine position. Apart from the interest that this finding has in regard to the possible pathophysiologic mechanism involved, this deleterious effect of the supine position on gas exchange is important because it might influence the natural course of the disease, given the time that humans spend in such a position. Moreover, the potential reversibility of the supine position related worsening hypoxemia with nasal oxygen therapy may have, of course, therapeutic implications.
Pathophysiologic Mechanism
Regarding the pathophysiologic mechanism involved in this position-related worsening hypoxemia, we initially believed that the phenomenon was simply a consequence of an increase in the shunting of blood through the congenital defect as a re-
Figure 1. Change in PaO2 with supine position and its relation to baseline sitting PaO2 in 28 patients with Eisenmengers syndrome. A second order polynomial model best fit the regression of this association. The decrease in PaO2 with supine position tends to be greater in patients with relatively normal baseline sitting PaO2.
sult of the increase in venous return associated with the supine position in the presence of a fixed pulmonary vascular resis tance. Our results, however, suggest that it may be a (V/Q) abnormality phenomenon rather than an increase in shunt as the mechanism responsible for this finding. The magnitude of the decrease in PaO2 with changing position correlated with the changes in the AaPO2 on room air, but it did not correlate with the changes in AaPO2 on FIO2 1.0. It has been previously established that when patients breathe room air, the calculated AaPO2 is made up of contributions from true right-to-left shunt (intrapulmonary and intracardiac shunt), the shunt-like effect of V/Q inequality, and, to a lesser extent, from the contribution of diffusion abnormalities (16, 17). As FIO2 is increased, the degree to which lung units with low V/Q ratios and/or with diffusion abnormalities contribute to abnormal gas exchange decreases, as does their contribution to the venous admixture. When breathing 100% oxygen, the calculated AaPO2 represents only the amount of true shunt (16, 17). The correction of the supine positionrelated hypoxemia with nasal O2 also sup ports a V/Q abnormality-related phenomenon. Although veno-arterial shunt through the congenital cardiac defect is the main mechanism for hypoxemia in Eisen mengers syndrome (18), V/Q distribution abnormalities in the lungs of these patients, albeit not studied, are also likely to occur. Advanced pulmonary vascular disease resulting from Eisenmenger physiology appears to be associated with appreciable disturbance of pulmonary function, and, as in our patients, both obstructive and restrictive ventilatory defects have been demonstrated (14, 15). The precise pathogenic mechanism responsible for altered pulmonary function in patients with pulmonary hypertension is not clear. Besides the potential role of cardiac enlargement on lung volumes (19), other factors have been considered, including changes in lung compliance, presumably resulting from mechanical coupling of the vascular and air spaces as well as small airways involvement (14, 15, 20). Also, in the presence of the increased pulmonary vascular resistance and advanced pulmonary vascular lesions, such as those described in Eisenmenger syndrome (21), perfusion distribution abnormalities in the perfusion distribution are expected. To our knowledge, the V/Q distribution in the lungs of patients with Eisenmengers syndrome as well as the effect of body position changes on this V/Q distribution has not been prospectively studied, but as mentioned above, ab normalities in V/Q distribution are likely to be present in these patients and they are also likely to be modified as a result of pulmonary hemodynamic changes (i.e., changes in cardiac output and pulmonary vascular resistance with position), as it has been shown in other human models of chronic obliterative pulmonary vascular disease (22, 23). Other pathophysiologic mechanisms, such as diffusion limitation, might also explain our findings. Patients with pulmonary hypertension are expected to have a low diffusing capacity of lung for carbon monoxide (DLCO), and a further diffusion limitation factor as a result of an increase in cardiac output with changing position might explain the drop in PaO2 in this setting. Hypoxemia from low diffusion would also improve with supplemental oxygen. It is not possible in the present study to assess the contribu tion of either V/Q distribution abnormalities or diffusion limitation to this position-related worsening hypoxemia in ES patients. Accordingly, lung diffusion capacity measurements and a more precise and less invasive procedure, such as the multiple inert gas elimination technique (24), would be necessary to confirm and better define the precise role of each of these postulated mechanisms. Our results also showed that the magnitude of the decrease
Sandoval, Alvarado, Martnez-Guerra, et al.: Gas Exchange in Eisenmengers Syndrome
1073
in PaO2 in supine position inversely correlates with the baseline sitting PaO2 (Figure 1). In other words, it is in those patients with a better baseline sitting PaO2 in whom a more profound impact on PaO2 in supine position is expected. We do not have a clear explanation for this finding. It may well be only the result of statistical coupling, since PaO2 appears in both the vertical and horizontal axes. It is likely, however, that in some of the patients in whom the elevated pulmonary vascular resistance was already fixed, no modifications in pulmonary hemodynamics occurred with changing position, and as a consequence the V/Q distribution within the lung was not modified. It is in those with less advanced disease in whom a more pronounced effect of position on gas exchange is expected. It has to be stressed that our study was performed at an altitude of 2,240 m above sea level and most of the patients were natives and residents of altitude. Because of the limits of the present study, it is difficult to anticipate a similar response at sea level. It would be interesting, however, to see the behavior of gas exchange with changing position in patients with ES at sea level, where the patients should have a better baseline PaO2.
Implications of Position-related Worsening Hypoxemia in ES
References
1. Farhi, L. E. 1987. Ventilation-perfusion relationships. In L. E. Farhi and S. M. Tenney, editors. Handbook of Physiology, vol 4. Section 3: The Respiratory System. American Physiological Society, Bethesda, MD. 199215. 2. Kaneko, K., J. Milic-Emili, M. B. Dolovich, A. Dawson, and D. B. Bates. 1966. Regional distribution of ventilation and perfusion as a function of body position. J. Appl. Physiol. 21:767777. 3. Martnez-Guerra, M. L., P. Fernandez-Bonetti, J. Sandoval, and E. LupiHerrera. 1981. Efecto de la posicin corporal sobre la funcin mecnica del pulmn en el obeso. Arch. Inst. Cardiol. Mx. 51:565570. 4. Said, S. I. 1960. Abnormalities of pulmonary gas exchange in obesity. Ann. Intern. Med. 6:11211129. 5. Gaspar, J., J. Sandoval, P. Fernandez-Bonetti, and E. Lupi-Herrera. 1980. Fistula arterio-venosa pulmonar y decbito-latero-deoxia. Arch. Inst. Cardiol. Mx. 50:173177. 6. Smeenk, F. W. J. M., and P. E. Postmus. 1993. Interatrial right-to-left shunting developing after pulmonary resection in the absence of elevated right-sided heart pressures: review of the literature. Chest 103: 528531. 7. Robin, E. D., P. D. Harman, B. R. Horn, and J. Theodore. 1976. Platypnea related to orthodeoxia caused by true vascular lung shunts. N. Engl. J. Med. 294:941. 8. Robin, E. D., P. D. Laman, M. L. Goris, and J. Theodore. 1977. A shunt is (not) a shunt is (not) a shunt. Am. Rev. Respir. Dis. 115:553. 9. Lupi-Herrera, E., M. Seoane, J. Sandoval, J. M. Casanova, and D. Bialostozky. 1980. Behavior of the pulmonary circulation in the grossly obese patient: pathogenesis of pulmonary arterial hypertension at an altitude of 2,240 meters. Chest 78:553558. 10. Anthonisen, N. R., and J. A. Fleetham. 1987. Ventilation: total, alveolar, and dead space. In L. E. Farhi and S. M. Tenney, editors. Handbook of Physiology, vol 4. Section 3: The Respiratory System. American Physiological Society, Bethesda, MD. 113129. 11. Norusis, M. J. 1988. The SPSS guide to data analysis for SPSS-PC . 12. Martinez-Guerra, M. L., P. Fernandez-Bonetti, and A. Balvanera. 1973. Valores normales de algunas medidas de la funcin respiratoria en la Ciudad de Mxico. Prensa Med. Mex. 38:15. 13. Ruiz-Arguelles, G. J., L. Sanchez Medal, A. Loria, J. Piedras, and M. S. Cordova. 1980. Red cell indices in normal adults residing at altitudes from sea level to 2670 m. Am. J. Hematol. 8:265271. 14. MacArthur, C. G. C., D. Hunter, and G. J. Gibson. 1979. Ventilatory function in Eisenmenger syndrome. Thorax 34:348353. 15. Burke, C. M., A. R. Glanville, A. J. R. Morris, D. Rubin, J. A. Harvey, J. Theodore, and E. D. Robin. 1987. Pulmonary function in advanced pulmonary hypertension. Thorax 42:131135. 16. Dantzker, D. R. 1991. Pulmonary gas exchange. In D. R. Dantzker, editor. Cardiopulmonary Critical Care, 2nd ed. W.B. Saunders, Philadelphia. 2544. 17. Ayres, S. M., A. Criscitiello, and E. Grabovsky. 1964. Components of alveolar-arterial O2 difference in normal man. J. Appl. Physiol. 19:43 47. 18. Lister, G., and B. R. Pitt. 1983. Cardiopulmonary interactions in the infant with congenital cardiac disease. Clin. Chest Med. 4:219232. 19. Wiener, C. M., W. J. McKenna, M. J. Myers, J. P. Lavender, and J. M. Hughes. 1990. Left lower lobe ventilation is reduced in patients with cardiomegaly in the supine but not the prone position. Am. Rev. Respir. Dis. 141:150155. 20. Fernandez-Bonetti, P., E. Lupi-Herrera, M. L. Martinez-Guerra, R. Barrios, M. Seoane, and J. Sandoval. 1983. Peripheral airways obstruction in idiopathic pulmonary artery hypertension (primary). Chest 5:732 738. 21. Collins-Nakai, R. L., and M. Rabinovitch. 1993. Pulmonary vascular obstructive disease. Cardiol. Clin. 11:675687. 22. Dantzker, D. R., and J. S. Bower. 1979. Mechanisms of gas exchange abnormality in patients with chronic obliterative pulmonary vascular disease. J. Clin. Invest. 64:10501055. 23. Dantzker, D. R., and J. S. Bower. 1981. Pulmonary vascular tone improves VA/Q matching in obliterative pulmonary hypertension. J. Appl. Physiol. 51:607613. 24. Wagner, P. D., and R. Rodriguez-Roisin. 1991. Clinical advances in pulmonary gas exchange. Am. Rev. Respir. Dis. 143:883888. 25. Bowyer, J. J., C. M. Busst, D. M. Denison, and E. A. Shinebourne. 1986. Effect of long term oxygen treatment at home in children with pulmonary vascular disease. Br. Heart. J. 55:385390.
Whatever the mechanism, the finding of a supine position related worsening hypoxemia and its correction with nasal oxygen therapy is an important one. It is conceivable that, by adding the vasoactive component of hypoxic pulmonary vasoconstriction, nocturnal hypoxemia in these patients may negatively influence both the course of the pulmonary vascular remodeling in this disease and the level of pulmonary vascular resistance and pulmonary pressures (21, 25). Traditionally, long-term oxygen therapy has not been routinely recommended for the treatment of Eisenmengers syndrome, based on the premise that veno-arterial shunt through the congenital defect is the mechanism responsible for the hypoxemia, and therefore it would be refractory to oxygen therapy. Although this premise may still hold true, there are other circumstances, such as this supine positionrelated worsening hypoxemia, that may deleteriously contribute to the functional status of the patient; it appears to be related to factors independent from only the true veno-arterial shunt and, accordingly, to being susceptible to oxygen therapy. With the exception of one study (25), the potential benefit of long-term oxygen treatment in ES has not been prospectively evaluated. In this controlled, although non-randomized, pilot study, Bowyer and coworkers (25) showed a significant improvement in the survival of children with ES receiving domiciliary oxygen for a minimum of 12 h/d (mostly at night) for up to 5 yr. The authors attributed the survival benefit of this therapy to the relief of an additional but reversible element of pulmonary vasoconstriction. Apart from this potential and beneficial pulmonary hemodynamic effect, the relief of the deleterious systemic effects of chronic hypoxia should also be considered. In conclusion, the main finding of the present study is that changing from the sitting to supine position in patients with ES produces a small but significant decrease in PaO2 and SaO2 that is corrected by supplemental oxygen. The pathophysiologic mechanism involved, as well as the importance of this finding at sea level, remains to be defined. Likewise, the impact of this deleterious finding on the natural history of the disease and that of its correction with nocturnal long-term oxygen therapy remain to be elucidated.
Acknowledgment : The writers are indebted to Nicholas Anthonisen, M.D., for his thoughtful comments and valuable criticisms in the review of the manuscript.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Magnetic Therapy in Eastern Europe A 30 Year ReviewDokument3 SeitenMagnetic Therapy in Eastern Europe A 30 Year ReviewMichael McDonnough100% (2)
- Middle Range Theory of Chronic Sorrow PDFDokument15 SeitenMiddle Range Theory of Chronic Sorrow PDFalda100% (1)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Judet QuadricepsplastyDokument4 SeitenJudet QuadricepsplastyRakesh Kumar100% (1)
- Mats Yoga Charts PDFDokument3 SeitenMats Yoga Charts PDFGloria Lindeman75% (4)
- Ashtanga Yoga Primary SeriesDokument2 SeitenAshtanga Yoga Primary SeriesRon Pascual100% (2)
- Anaesthesiology NAGY TESZTKÖNYVDokument1.064 SeitenAnaesthesiology NAGY TESZTKÖNYVoroszgabor100% (10)
- Free Yoga Manchester Sequence ChartDokument3 SeitenFree Yoga Manchester Sequence ChartGil Eng MesquitaNoch keine Bewertungen
- Spine in Sports PDFDokument223 SeitenSpine in Sports PDFceceetvero100% (4)
- XXDokument2 SeitenXXAura PalasNoch keine Bewertungen
- Flipbook1 SNDokument291 SeitenFlipbook1 SNDavid Carrozzo100% (2)
- Dietary Aspects in Fibromyalgia Patients: Results of A Survey On Food Awareness, Allergies, and Nutritional SupplementationDokument7 SeitenDietary Aspects in Fibromyalgia Patients: Results of A Survey On Food Awareness, Allergies, and Nutritional SupplementationAura PalasNoch keine Bewertungen
- Escala SDokument1 SeiteEscala SAura PalasNoch keine Bewertungen
- Module 9 MobilityDokument174 SeitenModule 9 MobilityAura PalasNoch keine Bewertungen
- J Clin Epidemiol 2009 Menezes CostaDokument10 SeitenJ Clin Epidemiol 2009 Menezes CostaAura PalasNoch keine Bewertungen
- McGill Pain QuestionnaireDokument6 SeitenMcGill Pain Questionnairejimitkapadia100% (1)
- Dry Mouth Fact SheetDokument2 SeitenDry Mouth Fact SheetWiet SidhartaNoch keine Bewertungen
- Review in Clinical MicrosDokument103 SeitenReview in Clinical MicrosSyvelmarie Tinte100% (1)
- Methods of PrescriptionDokument4 SeitenMethods of PrescriptionGg K0% (1)
- Sms Jaipur MdMs ListDokument9 SeitenSms Jaipur MdMs ListPrabhat Kumar ShrivastavaNoch keine Bewertungen
- Essentials of Dentistry Quik Review and Examination Preparation PDFDokument327 SeitenEssentials of Dentistry Quik Review and Examination Preparation PDFpatriciatarauNoch keine Bewertungen
- Acidosis in ClvesDokument7 SeitenAcidosis in ClvesCat NeveNoch keine Bewertungen
- Shredder Capacity - Bio Medical WasteDokument3 SeitenShredder Capacity - Bio Medical WasteYasser FathiNoch keine Bewertungen
- ENGLISH FOR MIDWIFE UNIT 1 I Will Become A MidwifeDokument2 SeitenENGLISH FOR MIDWIFE UNIT 1 I Will Become A MidwifeDestyana ArabelNoch keine Bewertungen
- Lichen PlanusDokument6 SeitenLichen PlanusMerry MiraNoch keine Bewertungen
- Peripartum CardiomyopathyDokument18 SeitenPeripartum CardiomyopathyMJ WesleyNoch keine Bewertungen
- PDFDokument55 SeitenPDFYahya KhanNoch keine Bewertungen
- Ankle and Foot InjuriesDokument42 SeitenAnkle and Foot InjuriesJulius Adams100% (1)
- Basic Body Plan of Young Mammalian EmbryosDokument57 SeitenBasic Body Plan of Young Mammalian EmbryosWin DierNoch keine Bewertungen
- Pediatric Trauma: Initial Assessment and ManagementDokument29 SeitenPediatric Trauma: Initial Assessment and Managementrizky fathudinNoch keine Bewertungen
- BreastfeedingDokument13 SeitenBreastfeedingSintya AulinaNoch keine Bewertungen
- Sensory Processing DifferencesDokument42 SeitenSensory Processing Differenceselamy83% (6)
- Cranial Nerves 7-12Dokument62 SeitenCranial Nerves 7-12jangyNoch keine Bewertungen
- SoMaTom Sessions Computed Tomography November 2008Dokument79 SeitenSoMaTom Sessions Computed Tomography November 2008mojicap100% (3)
- Preoperative FastingDokument5 SeitenPreoperative FastingsilviaemohNoch keine Bewertungen
- Self LigationDokument2 SeitenSelf Ligationdavidrocks81Noch keine Bewertungen
- Brevard County Breastfeeding Resourcesjan2016Dokument2 SeitenBrevard County Breastfeeding Resourcesjan2016api-250832672Noch keine Bewertungen
- Calmine-Hine 1995 Cancer ReportDokument34 SeitenCalmine-Hine 1995 Cancer ReportShirley SpenceNoch keine Bewertungen
- Arm CurlDokument3 SeitenArm CurlNor AmalinaNoch keine Bewertungen
- Pediatric Medication Math Review Jan 2011Dokument7 SeitenPediatric Medication Math Review Jan 2011Tyrone Kent HalogNoch keine Bewertungen
- Neurofibromatosis in PregnancyDokument2 SeitenNeurofibromatosis in PregnancyDwi Wahyu AprianiNoch keine Bewertungen
- Bhutan I 2013Dokument7 SeitenBhutan I 2013marsyaNoch keine Bewertungen