Beruflich Dokumente
Kultur Dokumente
Protozoal Infection
Hochgeladen von
naeb_91Originalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Protozoal Infection
Hochgeladen von
naeb_91Copyright:
Verfügbare Formate
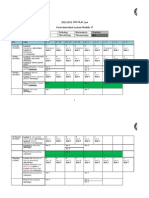
Phlum, Subphylu m geo dist
Entamoeba histolytica SM, Sarcodina
Giardia Lamblia SM, Mastigophora
Balantidium Coli Ciliophora
Isospora Belli Apicomplexa
Cryptosporidia Apicomplexa
cosmopolitan but tropical & subtropical countries > trophozoites and cysts 1rily inhabit the lumen of LI occasionally trophozoites invade mucosal crypts where the lyse tissues, feed on RBC, form ulcers fresh unstained H&E faecal smear pseudopodium w ectoplasm clearly clear ectoplasm differentiated from + endoplasm nucleus not visible + + spherical nucleus w ingested RBC -> v small central pale greenish karyosome refractile bodies + fine granular chromatin granules 20-60 lining the nuclear membrane + ingested RBC -> bluish black dics in endoplasm
cosmopolitan but tropical & subtropical countries > crypts of duodenum + upper jejunum occasionally in bile ducts and gall bladder
habitat
cosmopolitan most common in tropical zones esp philippines caecum and colon of humans, pigs, guinea pigs, rats and other mammals
cosmopolitan but tropical & subtropical > epithelial cells of distal duodenum and prox jejunum
cosmopolitan
originally para of calves but can infect man, kittens, puppies, rodents
morpho TROPHOZ OITES
30-150 o bilaterally symmetrical o pear-shaped broad antly and tapering postly o 9-21 x 5-15 o Dorsal surface convex o Ventral surface ant ovoidal concavity (sucking disc) serves as attachment to mucosa o 2 vesicular nuclei in area of sucking disc o 4 pairs of flagella + 2 sausage shaped median bodies post to sucking disc o Multiply repeated by binary fission
x 25-120
Oblong/ spheroid Ant end - peristome, either wide open OR slit like Post end - cytopyge Whole body covered w fine cilia arranged in rows 1 macronucleus - v slightly curved kidney or bean shaped - lies obliquely near middle of body - about 2/5 of length of body 1 micronucleus - much smaller - often hidden 2 contractile vacuoles ; 1 near middle of body, 1 near post end Food vacuoles contain cell fragments, starch granules, faecal debris, RBC
CYSTS
spherical / oval bodies w a hyaline refractile cyst + nuclei may not be visible OR 1-4 hyaline bodies + chromatid bodies made up of RNA -> rod shaped clear areas in cytoplasm 10-20
nuclear structure is apparent and similar to trophic form + mature cyst contains 4 visible nuclei + chromatid bodies > rod shaped + rounded edges & stain blue black
o o o o o o o
oval in shape 8 x 14 4 nuclei usually at one pole Parabasal bodies Remnants of flagella Axonemes Encystations occur when liquid faeces become dehrydrated in transit down the colon
Spheroidal / ovoidal w 40-60 diameter and thick cyst wall Macro and micro nuclei can also be seen
(mature sporulated oocyst) 20-33 x 1019 Contain 2 mature sporocyst with 4 sporozoites each
(mature oocyst + 4 naked sporozoites) 4-6 in diameter
reproducti on def. host infect. stage diag. stage mode of infection
binary fission
longitudinal binary fission
transverse fission
asexual schizogenic cycle + sexual reproduction mature sporulated oocyst
asexual schizogenic cycle + sexual reproduction mature oocyst + 4 naked sporozoites
humans mature 4 nucleated cyst *if trophozoites are swallowed, they are destroyed by gastric acidity contamination of food and drink thru : 1. Polluted water supply 2. Imperfectly washed raw vege 3. Contaminated hands esp in food handlers who are cyst passers 4. Food contaminated w vomits or excreta of flies since the cysts pass unharmed thru intestine of these insects 5. Usage of human excreta as fertilizers cysts cysts
ingestion of food or water 1. Contaminated of food and drink 2. Direct infection from man to man 3. Autoinfection 4. Mechanical transmission by house flies endemic areas : infection occurs anoorally directly from one to another epidemic areas : infection thru polluted water supplies more common in children
ingestion of cyst usually in contaminated water or food basically it is a parasite of pigs, and is esp common in ppl who are in close cntct w pigs
ingestion of water or food contaminated with mature sporulated oocysts
ingestion of mature oocysts thru: 1. Contamination of food and drink by oocysts 2. Close cntct with infected calves 3. Auto-infection 4. Direct person to person 5. Inhalation
pathogenesis
pathological changes depend on : Virulence of infective strain Host resistance Host nutritional status Bacterial infection most affected areas (dt sluggish movement of faecal material : Caecum Rt & Lt colic flexures Sigmoid colon pathogenic trophozoites secrete lytic enzyme small areas of necrosis in epithelium giving a way to penetrate (penetration) erode into deeper tissues breaking thru musc. Mucosa (reach submucosa) where the spread fan-like, multiply extensively causing lytic necrosis (when necrotic content is discharged) typical flask shaped ulcers produced, mucosa in between is healthy further progress invasion may occur thru penetration of musculosa and reaching serous coat peritonitis amoebiasis of caecum appendix amoebic appendicitis chronic infection + superadded bact infection granulomatous nodular mass (amoeboma) erosion of BV in the wall of ulcers hemorrhage amoeba carried by BV as emboli to reach liver and others
under ordinary conditions, trophozoites feed on food debris in caecum but sometimes, organism can produce proteolytic enzyme digest away epithelium ulcer ulcer mayb rounded irregular OR flask shaped + narrow neck undermining sac-like cavity in submucosa colonic ulceration lymphocytic infiltration w few polymorphnuclear cells + hemorrhage 2ry bacterial invasion may follow
distortion of intestinal villi + cellular infiltration of plasma cells, lymphocytes, eosinophils
clinical pic
ASYMPTOMATIC (major of cases, 8090%) patient is a carrier of cysts this person is in danger to himself and to others SYMPTOMATIC INTESTINAL LESION 1. Acute dysentery variable incub. period : as short as 4 days, as long as a year gradual onset except in fulminating cases where it is sudden gripping abd pain + dysentery (diarrhea + tenesmus + blood + mucus in stool) localized abd pain over caecum and pelvic colon no of motions are 4-8 per day toxemic manifestations are rare Non Dysenteric Colitis Vague abd discomfort + distention of caecum and colon + gas Diarrhea alternating w constipation may be present Amoeboma / Amoebic Granuloma
good % are asymptomatic in symptomatic cases, IP last from 1-3 weeks and present itself in diff forms: Diarrhea gradual / acute stool are offensive, pale yellow and frothy similar to lentil soup Dyspepsia epigastric pain, marked nausea, flatulence Malabsorption severe infection resembles tropical sprue : weight loss lassitude fatty stools fatty stool dt : 1. attachment of sucking disc to mucous membrane blockage of mucosal cells absorption of FA 2. inflammation of epithelial cells absorption capacity both of these conditions lead to accumulation of unabsorbed FA fatty yellow frothy stools there is also malasorption of Dxylose and vit B12
may be asymptomatic but major of cases present with 1. dysentery 2. abd colic 3. tenesmus resembling amoebic dysentery 4. intestinal perforation (fulminant case) 5. invasion of extraintestinal such as liver (rare)
1. diarrhea for several months to years + weight loss + abd colic + fever 2. bowel motions, 6-10x daily 3. soft to watery, foamy + offensive smell = malabsorption 4. profuse diarrhea + weakness + anorexia + weight loss in immunosuppress ed patients (AIDS)
1. 2. 3.
4.
low grade fever abd cramps diarrhea, self limited in person w normal immune response BUT fatal in immunocompromized patients respi infection
2.
3.
Results from repeated amoebic infection + superadded bact infection mass in abd might be misdiagnosed as carcinoma Surgical removal w/out medical treatment is fatal
1.
EXTRAINTESTINAL Amoebic Hepatitis
Results from emboli of trophozoites from LI reaching liver via portal blood no of small necrotic foci, if not treated, coalesce to form abcess Acute onset : may occur during attack of dysentery / in ppl who gave no history of amoebiasis at all Sudden rise in temp + enlarged tender liver 2. Amoebic Liver (Liver Abcess)
dt untreated amoebic hepatitis toxemic manifestations are more severe, pain becomes stabbing referred to rt shoulder and increase by coughing and inspiration and relieved by lying on rt side patient has a characteristic muddy complexion denoting toxaemia liver is enlarged and tender + marked intercostals edema over site of liver abcess may rupture into pleural cavity, lung, pericardium, stomach, rt colonic flexure, perinephric area, gall bladder or skin 3. Pulmonary Amoebiasis
Thru invasion of hepatic abcess thru diaphragm / rarely blood born 1ry infection from intestinal ulcers Manifested by dyspnea + lower chest pain + cough
4.
Cutaneous lesions
On skin covering the liver area after rupture or aspiration of an amoebic liver abcess OR perineal region in debilitated infected patients Manifested by tender swollen ulcerated area 5. Cerebral lesions
Result of blood extension from preexisting lesion in liver / lung OR direct hematogenous spread from colon May stimulate brain tumour which is usually fatal COMPLICATIONS 1. Intestinal : hemorrhage, appendicitis, amoeboma 2. Extraintestinal : amoebic hepatitis, amoebic liver, lung involvement, amoebiasis cutis, may stimulate brain tumour
Lab Diagnosis
DIRECT METHOD INTESTINAL HEPATIC 1. Stool examination 1. History and clinical Dysenteric stool (trophozoite pic of patient is visible) 2. X-ray shows upward either thru fresh saline smear displacement of OR fixed stool specimen diaphragm + reduced *refer to morpho movement + Well formed stool (cyst is sometimes a fluid visible) can be seen either thru fresh saline/iodine 3. CT scan smear OR fixed stool sample 4. Aspiration ; only if theres a large abcess 2. Sigmoidoscopy so used as for visualization of amoebic treatment, lesion and confirmation of o aspirated material is diagnosis by taking scraped viscid, choc brown, material from an ulcer thick (anchovy sauce) o trophozoites never found in pus, they are only present if aspirate is taken from edge of the abcess 5. Trophozoites can be found in sputum if liver abcess rupture into the lung
DIRECT METHOD 1. Stool examination Diarrhoeic stool, trophozoite is visible in saline smears Well formed stool, cysts are visible easily by staining w Lugols iodine solution repeated stool examination shud be done coz organisms tend to pass in stools intermittently 3 samples shud be examined routinely on alternate days in scanty infections, concentration by Zn sulphate floatation technique is of value 2. Duodenal aspiration when clinical pic is suggestive of giardial infection and repeated stool examination give ve results esp that excretion of parasite is erratic and not regular 3. Entero test capsule (string test) INDIRECT METHOD detection of FL copro Ag in stools by ELISA technique is helpful and resorted when repeated ve results of stool examination and CP is suggestive
stool examination to discover trophozoite w or w/out cystic stage
1. stool examination by simple saline / iodine smear conc techniques such as zn floatation mayb used if infection is scanty organisms are acid-fast, oocysts appear bright pink when stained w modified ZN stain 2. Blood pic eosinophilia
1. stool examination using formol ether OR Sheathers sugar flotation oocysts are better visualized when stained by modified ZN acid fast stain bright pink 2. entero test 3. intestinal biopsy 4. sputum examination
INDIRECT METHOD indirect haemagglutination test (IHAT), ELISA, and gel diffusion tests are +ve in invasive amoebiasis : acute dysentery and amoebic abcess
treatment
choice of drug depends on type of clinical presentation & site of drug action luminal amoebicides - drugs act 1rily on organisms in colonic lumen mainly cyst passers tissue/systemic amoebicides - acting on invasive stages (tissue forms) all patients w invasive disease require treatment 1stly w systemically acting compound, subsequently w luminal amoebicide to eliminate any organisms in colon 1. asymptomatic intestinal infection (cyst passers) o diloxanide furoate (furamide) non dysenteric intestinal colitis o diloxanide furoate +metronidazole o furazole (combination of diloxanide furoate and metronidazole) dysenteric intestinal colitis o bed rest + fluid and electrolyte replacement therapy o specific treatment : metronidazole accompanied by furazole hepatic abcess o hospitalization + bed rest o needle aspiration is advisablewhen size of abcess is large and when severe hepatic pain and tenderness o specific treatment : metronidazole
metronidazole (flagyl)
tetracycline dose: 500mg, 4x daily for 10 days
cotrimoxazole a comnbination of trimethoprim (TMP) + sulphamethoxazo le (SMX) each tablet made up of 160mg TMP + 800mg SMX dose : 1 tablet twice daily for 10days *in immunesuppressed pastients w persistent infection treatment shud be for life
nitazoxanide
2.
3.
4.
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Past Papers GitDokument9 SeitenPast Papers GitNur MaslinaNoch keine Bewertungen
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Module 17 Mid Term ResultsDokument7 SeitenModule 17 Mid Term Resultsnaeb_91Noch keine Bewertungen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Oral Cavity, Salivary Glands and Pharynx SkullDokument9 SeitenOral Cavity, Salivary Glands and Pharynx Skullnaeb_91Noch keine Bewertungen
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- GIT 1st Week Till 8th Week (Silap)Dokument23 SeitenGIT 1st Week Till 8th Week (Silap)naeb_91Noch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Practical Questions of The EgyptiansDokument2 SeitenPractical Questions of The Egyptiansnaeb_91Noch keine Bewertungen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- NGTDokument1 SeiteNGTnaeb_91Noch keine Bewertungen
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Part IiDokument10 SeitenPart Iinaeb_91Noch keine Bewertungen
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- GIT 1st Week Till 8th WeekDokument24 SeitenGIT 1st Week Till 8th Weeknaeb_91Noch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Recovery Position: Clinical Learning GuideDokument3 SeitenRecovery Position: Clinical Learning Guidenaeb_91Noch keine Bewertungen
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- Clinical Learning Guide Nasogastric Tube Insertion (NGT) : Before StartingDokument2 SeitenClinical Learning Guide Nasogastric Tube Insertion (NGT) : Before Startingnaeb_91Noch keine Bewertungen
- Professional Skills ScheduleDokument1 SeiteProfessional Skills Schedulenaeb_91Noch keine Bewertungen
- Cardic CompressionDokument3 SeitenCardic Compressionnaeb_91Noch keine Bewertungen
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Question GenitourinaryDokument2 SeitenQuestion Genitourinarynaeb_91Noch keine Bewertungen
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Endocrine MarksDokument1 SeiteEndocrine Marksnaeb_91Noch keine Bewertungen
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Index For Genitourinary ModuleDokument5 SeitenIndex For Genitourinary Modulenaeb_91Noch keine Bewertungen
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Index Urinary ModuleDokument5 SeitenIndex Urinary Modulenaeb_91Noch keine Bewertungen
- Index For Endocrine System ModuleDokument4 SeitenIndex For Endocrine System Modulenaeb_91Noch keine Bewertungen
- CHN TransesDokument82 SeitenCHN Transeskint manlangitNoch keine Bewertungen
- AmoebiasisDokument2 SeitenAmoebiasisJay PeeNoch keine Bewertungen
- AMOEBIASISDokument36 SeitenAMOEBIASISKhei Laqui SNNoch keine Bewertungen
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Amoebiasis: Synonym: Amoebic Dysentery HistoryDokument152 SeitenAmoebiasis: Synonym: Amoebic Dysentery HistoryMacaRonie PepeRownie del RioNoch keine Bewertungen
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Typhoid Fever: Causes, Symptoms and Nursing CareDokument122 SeitenTyphoid Fever: Causes, Symptoms and Nursing CaretishpatNoch keine Bewertungen
- Loparet Tablet 10'SDokument1 SeiteLoparet Tablet 10'SFARHEEN AZAM NoorNoch keine Bewertungen
- Senarai Penyakit-BerjangkitDokument1 SeiteSenarai Penyakit-BerjangkitMuhammad Syamil RadzuanNoch keine Bewertungen
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Diarrhoeal Diseases in NepalDokument86 SeitenDiarrhoeal Diseases in NepalBinayaNoch keine Bewertungen
- Symptoms and Causes of ColitisDokument5 SeitenSymptoms and Causes of ColitisChatrina TandiloloNoch keine Bewertungen
- "Bloody Scours": Swine DysenteryDokument29 Seiten"Bloody Scours": Swine DysenteryleaNoch keine Bewertungen
- Persistent Diarrhoea: IAP UG Teaching Slides 2015 16Dokument31 SeitenPersistent Diarrhoea: IAP UG Teaching Slides 2015 16Srujana MohanNoch keine Bewertungen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Entamoeba HistolyticaDokument2 SeitenEntamoeba HistolyticaEugenia Cindy JulianyNoch keine Bewertungen
- ParagisDokument15 SeitenParagisNeil Francel D. MangilimanNoch keine Bewertungen
- Stuart Bloom (Editor), George Webster (Editor), Daniel Marks (Editor) - Oxford Handbook of Gastroenterology & Hepatology (Oxford Medical Handbooks) - Oxford University Press (2021)Dokument1.146 SeitenStuart Bloom (Editor), George Webster (Editor), Daniel Marks (Editor) - Oxford Handbook of Gastroenterology & Hepatology (Oxford Medical Handbooks) - Oxford University Press (2021)aliakbar178Noch keine Bewertungen
- Ragama Medicine Case BookDokument391 SeitenRagama Medicine Case BookSanjaya WijesekaraNoch keine Bewertungen
- Tibb Practitioner Monograph - July 2008Dokument75 SeitenTibb Practitioner Monograph - July 2008bilalbprNoch keine Bewertungen
- Louisiana Couple Sues Pelahatchie Water Park After Daughter Allegedly Contracts E. ColiDokument9 SeitenLouisiana Couple Sues Pelahatchie Water Park After Daughter Allegedly Contracts E. ColiWLBT NewsNoch keine Bewertungen
- Maape - Bacillary DysenteryDokument7 SeitenMaape - Bacillary Dysenterylorella_abejuelaNoch keine Bewertungen
- PIDSR Manual of ProceduresDokument55 SeitenPIDSR Manual of ProceduresOrlea FranciscoNoch keine Bewertungen
- Infectious Disease Exam Questions Covering Topics Like Hepatitis, Malaria, Cholera & MoreDokument23 SeitenInfectious Disease Exam Questions Covering Topics Like Hepatitis, Malaria, Cholera & Moretarun956519Noch keine Bewertungen
- (Nelsons 21st) Acute GastroenteritisDokument21 Seiten(Nelsons 21st) Acute GastroenteritisLara Patricia TamsiNoch keine Bewertungen
- Pamphlet AmoebiasisDokument3 SeitenPamphlet AmoebiasisAristotel Cabais100% (1)
- DIARRHEADokument44 SeitenDIARRHEAKristin Masehathena BerutuNoch keine Bewertungen
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Dysentery: Causes, Symptoms and Ayurvedic ManagementDokument20 SeitenDysentery: Causes, Symptoms and Ayurvedic ManagementGaurav SinghNoch keine Bewertungen
- Ethnomedicinal plants used by Deori tribes of AssamDokument5 SeitenEthnomedicinal plants used by Deori tribes of Assammkshri_inNoch keine Bewertungen
- Acute Gastroenteritis in ChildrenDokument64 SeitenAcute Gastroenteritis in ChildrenSteven William0% (1)
- MAPEHDokument4 SeitenMAPEHDalmendozaNoch keine Bewertungen
- Acute Lower Gastrointestinal Bleeding: Evaluation and Management p206Dokument7 SeitenAcute Lower Gastrointestinal Bleeding: Evaluation and Management p206Ahmed AlhalwajiNoch keine Bewertungen
- Herbs and SpicesDokument166 SeitenHerbs and Spiceskareen samantha tamayoNoch keine Bewertungen
- Clinical Case: Csu Junior InternsDokument82 SeitenClinical Case: Csu Junior InternsAlexious Marie CalluengNoch keine Bewertungen