Beruflich Dokumente
Kultur Dokumente
Case Pre.. Cushing Syndrome
Hochgeladen von
dee_day_8Originalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Case Pre.. Cushing Syndrome
Hochgeladen von
dee_day_8Copyright:
Verfügbare Formate
SUBMITTED BY: MUSTAPHA, NAJIEFAH P. SUBMITTED TO: PLAZA, CHARLIE C.
RN, MN,MAN
INTRODUCTION What is Cushing Syndrome? >Cushings syndrome is a hormonal disorder caused by prolonged exposure of the bodys tissues to high levels of the hormone cortisol. Sometimes called hypercortisolism, Cushings syndrome is relatively rare and most commonly affects adults aged 20 to 50. People who are obese and have type 2 diabetes, along with poorly controlled blood glucose and high blood pressure, have an increased risk of developing the disorder. >result from excessive rather than deficient, adrenocortical activity ANATOMY AND PHYSIOLOGY Each person has 2 adrenal glands, one attached to the upper portion of the kidney. Each adrenal gland is in reality, two endocrine glands with separate, independent functions. ADRENAL MEDULLA >Located at the centre of the glands secretes catecholamines >fxn as part of the autonomic nervous system. Stimulation of paraganglionic sympathetic nerve fibers, which travels directly to the cells of the adrenal medulla, causes release of catecholamine hormones (epinephrine and norepinephrine). 90% of epinephrine is secreted. >catecholamine regulates metabolic pathways to promote catabolism of stored fuels to meet caloric needs from endogenous sources. >the major effects of epinephrine is for fight or flight response. secretion of epinephrine causes decreased blood flow to tissues that are not needed in emergency situations, and increases blood flow to tissues that are important for effective fight or flight, such as cardiac and skeletal muscle.
>catecholamines also induce the release of free fatty acid, increased the basal metabolic rate and elevate the blood glucose level. ADRENAL CORTEX >adrenocortical secretions make it possible for the body to adapt to stress at all kinds. THREE TYPES OF STEROID HORMONES PRODUCED BY ADRENAL CORTEX 1. GLUCOCORTICOID >prototype of which is hydrocortisone secretion results in elevated blood glucose level >secreted in response to the release of adrenocorticotropic hormone from the anterior lobe of the pituitary gland. 2. MINERALOCORTICOID >exert a major effect in electrolyte metabolism. Act principally in renal tubular and gastrointestinal epithelium to cause increased sodium ion absorption in exchange for secretion of potassium ions or hydrogen ions. >ACTH only minimally influences aldosterone secretion, is primarily secreted in response to the presence of angiotensin II in the blood stream.
3. ADRENAL SEX HORMONE >or androgens is the third major type of steroid hormone secreted by the adrenal cortex, exerts effect similar to those of male sex hormones. May also secretes small amount of estrogen.
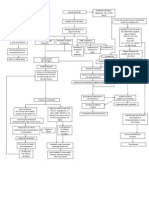
PATHOPHYSIOLGY OF CUSHIING SYMDROME ETIOLOGY >use of corticosteroid medication >hyperplasia of adrenal cortex >tumor of the pituitary gland >ectopic production of ACTH by malignancies (bronchogenic carcinoma) cause production of ACTH that stimulates the adrenal cortex to increased its hormone secretion
mineralocorticoid sodium retention potassium
glucocorticoids cortisol BUFFALO HUMP- due to steroid level
Fluid retentionEdema/anasarca
glucose/ hyperglycemia moonface- due to cortisol level Tronchal obesity supraclavicular area due to fat deposit
Hypertension
CHF
heavy trunk & relatively thin extremitiesDue to massive protein catabolism
Sex hormone
immune pattern susceptibility to infection
skeletal problem
dematologic problem
Virilism- characterized By appearance of Masculine traits & Recession of feminine traits
osteoporosis
thin fragile, easily traumatized ecchymosis, strea develops
impaired wound healing
muscle wasting
psychiatric problem
hirsutism
kyphosis backache psychoses
breast atrophy constipation clitoris enlargement` libido depression/distress, mood alteration
Menstrual cease
Voice deepen
ASSESSMENT AND DIAGNOSTIC FINDINGS No single lab test is perfect and usually several are needed. The three most common tests used to diagnose Cushings syndrome are the 24-hour urinary free cortisol test, measurement of midnight plasma cortisol or late-night salivary cortisol, and the low-dose dexamethasone suppression test. Another test, the dexamethasone-corticotropin-releasing hormone test, may be needed to distinguish Cushings syndrome from other causes of excess cortisol.
24-hour urinary free cortisol level. In this test, a persons urine is collected several times over a 24-hour period and tested for cortisol. Levels higher than 50 to 100 micrograms a day for an adult suggest Cushings syndrome. The normal upper limit varies in different laboratories, depending on which measurement technique is used. Midnight plasma cortisol and late-night salivary cortisol measurements. The midnight plasma cortisol test measures cortisol concentrations in the blood. Cortisol production is normally suppressed at night, but in Cushings syndrome, this suppression doesnt occur. If the cortisol level is more than 50 nanomoles per liter (nmol/L), Cushings syndrome is suspected. The test generally requires a 48-hour hospital stay to avoid falsely elevated cortisol levels due to stress. However, a late-night or bedtime saliva sample can be obtained at home, then tested to determine the cortisol level. Diagnostic ranges vary, depending on the measurement technique used.
Low-dose dexamethasone suppression test (LDDST). In the LDDST, a person is given a low dose of dexamethasone, a synthetic glucocorticoid, by mouth every 6 hours for 2 days. Urine is collected before dexamethasone is administered and several times on each day of the test. A modified LDDST uses a onetime overnight dose. Cortisol and other glucocorticoids signal the pituitary to release less ACTH, so the normal response after taking dexamethasone is a drop in blood and urine cortisol levels. If cortisol levels do not drop, Cushings syndrome is suspected. The LDDST may not show a drop in cortisol levels in people with depression, alcoholism, high estrogen levels, acute illness, or stress, falsely indicating Cushings syndrome. On the other hand, drugs such as phenytoin and phenobarbital may cause cortisol levels to drop, falsely indicating that Cushings is not present in people who actually have the syndrome. For this reason, physicians usually advise their patients to stop taking these drugs at least 1 week before the test.
Dexamethasone-corticotropin-releasing hormone (CRH) test. Some people have high cortisol levels but do not develop the progressive effects of Cushings syndrome, such as muscle weakness, fractures, and thinning of the skin. These people may have pseudo-Cushings syndrome, a condition sometimes found in people who have depression or anxiety disorders, drink excess alcohol, have poorly controlled diabetes, or are severely obese. Pseudo-Cushings does not have the same long-term effects on health as Cushings syndrome and does not require treatment directed at the endocrine glands. The dexamethasone-CRH test rapidly distinguishes pseudo-Cushings from mild cases of Cushings. This test combines the LDDST and a CRH stimulation test. In the CRH stimulation test, an injection of CRH causes the pituitary to secrete ACTH. Pretreatment with dexamethasone prevents CRH from causing an increase in cortisol in people with pseudo-Cushings. Elevations of cortisol during this test suggest Cushings syndrome.
TREATMENT When Cushing's syndrome results from an ACTH-producing tumor of the pituitary gland (Cushing's disease), treatment may include surgery, radiation, or medication to lower cortisol levels. Surgical removal of a small, well-defined pituitary adenoma is called transsphenoidal adenomectomy. The pituitary is located at the base of the brain. It is possible to access this area through the gums above the upper front teeth or the nose. Using special instruments, the surgeon makes an incision in one of these areas . The incision is extended through the sphenoid sinus, allowing the surgeon to see and remove the adenoma with an endoscope (a thin, lighted tube with a camera). This type of surgery permanently cures Cushing's syndrome in 60 to 70 percent of people. Sometimes a tumor cannot be identified; in these cases, half of the pituitary gland may be removed (hemihypophysectomy) or 85 to 90 percent of the pituitary gland may be removed (subtotal hypophysectomy) to be certain that the tumor has been removed. Surgical removal of half or more of the pituitary gland can reduce pituitary function and interfere with ovulation (in women) and sperm production (in men). Lifelong hormone replacement is often necessary after surgery. Radiation Radiation can be a useful treatment when pituitary tumors cannot be completely removed by surgery. Radiation of pituitary tumors reduces cortisol levels in about half of adults and most children with Cushing's disease. Because this cortisol-lowering effect takes time (3 to 12 months), medications that lower adrenal cortisol production may
be given while waiting for the effects of radiation. These medications include ketoconazole, metyrapone, and aminoglutethimide. Adrenalectomy Surgical removal of the adrenal glands (adrenalectomy) is a final measure that may be recommended if other treatments are not successful. Adrenalectomy stops excess cortisol production but requires that you begin lifelong daily glucocorticoid and mineralocorticoid replacement therapy.
NURSING DIAGNOSIS Risk for infection related to altered protein metabolism and inflammatory response
PLANNING >decreased risk of infection >improved skin integrity
INTERVENTION RATIONALE >tell the pt. to avoid >the nurse frequent unnecessary exposure assess the pt. for to infection. subtle signs of infection, because he anti-inflammatory effects of corticosteroids may mask the common signs of inflammation and infection. >stress proper hand washing by all care giver bet. Therapies of the pt >monitor clients visitor >to prevent cross contamination of the pt.
>to prevent any transmission of any respiratory illness >To prevent any occurrence of infection >to prevent the risk for any nosocomial infection
>promote reverse isolation >instruct client to have daily mouth care, include use of aseptic mouth wash >maintain sterile technique for all
>to prevent associated infection
NURSING DIAGNOSIS Risk for injury related to weakness
PLANNING >decreased risk for injury >demonstrate behaviours, lifestyle changes to reduce risk factor and protect self for injury
INTERVENTION >note client age, gender, developmental stage, decision making, ability, level of cognition/competence. >assess mood, coping abilities, and personality style >assess clients muscle strength, gross and fine motor coordination >provide environment of safety
RATIONALE >affects client ability to protect self from harm
>may result in careless/increased risktaking without consideration of consequences >to identify risk for falls
>To prevent any unusual accident
NURSING DIAGNOSIS Self-care deficit related to weakness, fatigue, muscle wasting
PLANNING >identify individual areas of weakness / needs. >perform self-care activities within level of own ability.
INTERVENTION >determine age/developmental issues >determine individual strengths and skills of the client >assisting client with ADL >provide privacy and equipment within easy reach during personal care >collaboration with physical therapist in rehabilitation >identify energy saving activities
RATIONALE >affecting individual ability to participate in own care.
>to have an idea of what the client can do >to prevent further fatigue >to prevent any complication that may arise
>to identify the pt. improvement >to prevent any further weakness and fatigue
Das könnte Ihnen auch gefallen
- Med Surg - Endocrine System QuestionsDokument7 SeitenMed Surg - Endocrine System QuestionsKrizia R. Pingke100% (8)
- Neuroendocrinology ACTIVITYDokument2 SeitenNeuroendocrinology ACTIVITYElizer Mario Pre Raboy100% (1)
- Physical Therapy Amputee Assessment FormDokument4 SeitenPhysical Therapy Amputee Assessment FormTopaz CompanyNoch keine Bewertungen
- A Disease Study of Cushing's DiseaseDokument13 SeitenA Disease Study of Cushing's DiseaseKristine AlejandroNoch keine Bewertungen
- CROHNSDokument2 SeitenCROHNSAlvin Germo Pasuquin100% (1)
- Pathophysiology of DMDokument4 SeitenPathophysiology of DMNicole Louise N. VillanuevaNoch keine Bewertungen
- Acute Myocardial InfarctionDokument20 SeitenAcute Myocardial InfarctionDavid Christian CalmaNoch keine Bewertungen
- Cholecystitis Case PresDokument103 SeitenCholecystitis Case PresAnton LaurencianaNoch keine Bewertungen
- Addison's DiseaseDokument15 SeitenAddison's DiseaseRonald A. Ogania50% (4)
- Acute Glomerulonephritis: Mohd Zamir Ghouse 060100848Dokument40 SeitenAcute Glomerulonephritis: Mohd Zamir Ghouse 060100848zamirsg100% (1)
- Medical Surgical Nursing Nclex Questions Onco1Dokument12 SeitenMedical Surgical Nursing Nclex Questions Onco1dee_day_8100% (2)
- Medical Surgical Nursing Nclex Questions Endo2Dokument9 SeitenMedical Surgical Nursing Nclex Questions Endo2dee_day_8Noch keine Bewertungen
- Nursing Care Plan GoiterDokument3 SeitenNursing Care Plan Goiterdee_day_8100% (4)
- UW ObjectivesDokument220 SeitenUW ObjectivesRaymond Bernatowicz100% (2)
- Mod 9 Basic ExtricationDokument3 SeitenMod 9 Basic Extricationrez1987Noch keine Bewertungen
- Botox EbookDokument15 SeitenBotox Ebookdoraemon100% (2)
- Critical Care Nursing AssignmentDokument13 SeitenCritical Care Nursing Assignmentiqmal irfamimi50% (2)
- Cushing's SyndromeDokument24 SeitenCushing's SyndromeUdtjeVanDerJeyk100% (1)
- Liver CirrhosisDokument60 SeitenLiver CirrhosisCamilla Zharine P. BantaNoch keine Bewertungen
- Acute and Chronic CholecystitisDokument10 SeitenAcute and Chronic Cholecystitisissam_1994Noch keine Bewertungen
- Acute PancreatitisDokument20 SeitenAcute PancreatitisMariquita BuenafeNoch keine Bewertungen
- Liver Cirrhosis: A Case Study OnDokument31 SeitenLiver Cirrhosis: A Case Study OnCharmaine del RosarioNoch keine Bewertungen
- Cushing's SyndromeDokument25 SeitenCushing's SyndromeRose Ann Del MundoNoch keine Bewertungen
- Nephrotic SyndromeDokument61 SeitenNephrotic SyndromeRanah Julia Garchitorena AyoNoch keine Bewertungen
- Crohns Disease Ebp Case Study PresentationDokument23 SeitenCrohns Disease Ebp Case Study Presentationapi-253093073Noch keine Bewertungen
- Burn Ctu 312 - 2Dokument1 SeiteBurn Ctu 312 - 2Shaira Ann CalambaNoch keine Bewertungen
- Case Study About Rectal CADokument11 SeitenCase Study About Rectal CACantiga Vhadz0% (1)
- Case Study Acute PancreatitisDokument62 SeitenCase Study Acute PancreatitisAilyne A. CleofeNoch keine Bewertungen
- DB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaDokument5 SeitenDB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaNeil Alcazaren かわいいNoch keine Bewertungen
- Case PresentationDokument31 SeitenCase PresentationYogaPratayogaMNoch keine Bewertungen
- Case Study - Septic ShockDokument16 SeitenCase Study - Septic ShockIrene Mae Villanueva Ariola100% (2)
- Presentation Liver CirrhosisDokument26 SeitenPresentation Liver CirrhosisFaye Dominique Roxas PalmaresNoch keine Bewertungen
- Septic Shock Student Case StudyDokument6 SeitenSeptic Shock Student Case StudyJenn GallowayNoch keine Bewertungen
- Ductal Carcinoma Case StudyDokument72 SeitenDuctal Carcinoma Case StudyRayjundie EstradaNoch keine Bewertungen
- NON-ALCOHOLIC FATTY LIVEr DISEASE (NAFLD) - NASHDokument4 SeitenNON-ALCOHOLIC FATTY LIVEr DISEASE (NAFLD) - NASHJason FooNoch keine Bewertungen
- Upper GI BleedingDokument70 SeitenUpper GI BleedingMia MusNoch keine Bewertungen
- Pathophysiology of Diabetes Mellitus Type 2Dokument1 SeitePathophysiology of Diabetes Mellitus Type 2faula rocamora100% (3)
- Diagram of Pathophysiology CancerDokument5 SeitenDiagram of Pathophysiology CancerKristaMaeC.Lazo0% (3)
- Cushing's SyndromeDokument5 SeitenCushing's SyndromesummerduskNoch keine Bewertungen
- Pancreatitis: (Alterations in Metabolic and Endocrine Functions)Dokument7 SeitenPancreatitis: (Alterations in Metabolic and Endocrine Functions)Jorie Roco0% (1)
- DkaDokument29 SeitenDkaShadowSpectre0Noch keine Bewertungen
- Liver CancerDokument1 SeiteLiver CancerTarantado67% (3)
- Prostate CancerDokument6 SeitenProstate CancerfheisanzNoch keine Bewertungen
- GOUT Case StudyDokument3 SeitenGOUT Case StudySunshine_Bacla_42750% (1)
- Chronic GlomerulonephritisDokument8 SeitenChronic GlomerulonephritisDaniel CornerNoch keine Bewertungen
- Concept Map CushingDokument4 SeitenConcept Map CushingCrystal Leigh Malunes Dagting100% (1)
- Case Study Cushing Syndrome 1Dokument5 SeitenCase Study Cushing Syndrome 1Selena Marie100% (1)
- Pathophysiology Hemor CVADokument4 SeitenPathophysiology Hemor CVAMatthew Emmanuel M. Martinez100% (2)
- Glaucoma Case StudyDokument5 SeitenGlaucoma Case StudyEdgel QuidolesNoch keine Bewertungen
- Pancretic Cancer Case Study - BurkeDokument52 SeitenPancretic Cancer Case Study - Burkeapi-282999254Noch keine Bewertungen
- Stevens Johnson Syndrome CASEDokument53 SeitenStevens Johnson Syndrome CASEKathrina CraveNoch keine Bewertungen
- Dengue Case StudyDokument16 SeitenDengue Case StudyJayselle FelipeNoch keine Bewertungen
- (Olfu) Pediatrics Case Study: Post Streptococcal Glomerulo Nephritis (PSGN)Dokument20 Seiten(Olfu) Pediatrics Case Study: Post Streptococcal Glomerulo Nephritis (PSGN)MikaCasimiroBalunanNoch keine Bewertungen
- Our Lady of Fatima University - Valenzuela Campus College of NursingDokument29 SeitenOur Lady of Fatima University - Valenzuela Campus College of NursingMary Shine GonidaNoch keine Bewertungen
- InTech-Diabetic Foot and GangreneDokument25 SeitenInTech-Diabetic Foot and GangrenePutu Reza Sandhya PratamaNoch keine Bewertungen
- Case Study H MOLEDokument11 SeitenCase Study H MOLEHomework PingNoch keine Bewertungen
- Diabetes PathoDokument2 SeitenDiabetes Pathodrewcel100% (1)
- Acute PancreatitisDokument11 SeitenAcute PancreatitisShara SampangNoch keine Bewertungen
- Acute Glomerulonephritis Case StudyDokument12 SeitenAcute Glomerulonephritis Case Study19lyon92100% (6)
- Systemic Lupus ErythematosusDokument89 SeitenSystemic Lupus ErythematosusIke RilleraNoch keine Bewertungen
- NCP AgnDokument2 SeitenNCP Agnj3nann3Noch keine Bewertungen
- CholelithiasisDokument3 SeitenCholelithiasisMIlanSagittarius0% (1)
- Stevens Johnson SyndromeDokument6 SeitenStevens Johnson SyndromeAudrey LeonarNoch keine Bewertungen
- Pa Tho Physiology of OsteoporosisDokument2 SeitenPa Tho Physiology of Osteoporosisjcam_o9Noch keine Bewertungen
- Adrenal DisordersDokument48 SeitenAdrenal DisordersMubeenUrRehmanNoch keine Bewertungen
- Acute Liver FailureDokument3 SeitenAcute Liver FailureElisabeth F. OjhaNoch keine Bewertungen
- Acute PancreatitisDokument7 SeitenAcute PancreatitisVytheeshwaran Vedagiri100% (9)
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- Rheumatic Fever: Causes, Tests, and Treatment OptionsVon EverandRheumatic Fever: Causes, Tests, and Treatment OptionsNoch keine Bewertungen
- Medical Surgical Nursing Nclex Questions Neuro2Dokument12 SeitenMedical Surgical Nursing Nclex Questions Neuro2dee_day_8Noch keine Bewertungen
- Onco 1Dokument8 SeitenOnco 1novice_023Noch keine Bewertungen
- Medical Surgical Nursing Nclex QuestionsDokument82 SeitenMedical Surgical Nursing Nclex Questionsdee_day_893% (14)
- Medical Surgical Nursing Nclex Questions Neuro1Dokument13 SeitenMedical Surgical Nursing Nclex Questions Neuro1dee_day_80% (1)
- Medical Surgical Nursing Nclex Questions GUDokument10 SeitenMedical Surgical Nursing Nclex Questions GUdee_day_8100% (1)
- Medical Surgical Nursing Nclex Questions Integu2Dokument12 SeitenMedical Surgical Nursing Nclex Questions Integu2dee_day_8100% (2)
- Medical Surgical Nursing Nclex questionsGI1Dokument11 SeitenMedical Surgical Nursing Nclex questionsGI1dee_day_8100% (2)
- Medical Surgical Nursing Nclex Questions Integu1Dokument12 SeitenMedical Surgical Nursing Nclex Questions Integu1dee_day_8100% (1)
- Medical Surgical Nursing Nclex Questions7Dokument7 SeitenMedical Surgical Nursing Nclex Questions7dee_day_8Noch keine Bewertungen
- Nursing Resource Unit Oral MedicationDokument3 SeitenNursing Resource Unit Oral Medicationdee_day_8Noch keine Bewertungen
- Nursing Resource Unit Taking Vital SignsDokument3 SeitenNursing Resource Unit Taking Vital Signsdee_day_8Noch keine Bewertungen
- Medical Surgical Nursing Nclex Questions 5Dokument18 SeitenMedical Surgical Nursing Nclex Questions 5dee_day_8Noch keine Bewertungen
- Ms QuestionsDokument16 SeitenMs QuestionsnursejoyNoch keine Bewertungen
- Nursing Resource Unit Postpartum CareDokument4 SeitenNursing Resource Unit Postpartum Caredee_day_8Noch keine Bewertungen
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDokument3 SeitenAssessment Nursing Diagnosis Planning Intervention Rationale Evaluationdee_day_8Noch keine Bewertungen
- SNC TuberculosisDokument19 SeitenSNC TuberculosisFabricio NuñezNoch keine Bewertungen
- Complications of Plaster Cast PATIENT LEAFLETDokument6 SeitenComplications of Plaster Cast PATIENT LEAFLETRadiyan MeidhiyantoNoch keine Bewertungen
- The Drug Discovery Process: Studies of Disease MechanismsDokument7 SeitenThe Drug Discovery Process: Studies of Disease MechanismsSajanMaharjanNoch keine Bewertungen
- Splenic InfarctionDokument20 SeitenSplenic InfarctionMộtHaiBaNoch keine Bewertungen
- Basic Principles of RhinoplastyDokument21 SeitenBasic Principles of Rhinoplastydrbantm100% (2)
- Mechanisms Case StudyDokument13 SeitenMechanisms Case Studyshane_tin143Noch keine Bewertungen
- StrokeDokument22 SeitenStrokeAlex GasnasNoch keine Bewertungen
- Counselling in Infertility Individual Couple and Group InterventionsDokument7 SeitenCounselling in Infertility Individual Couple and Group InterventionsEliza Martin100% (1)
- Kerangka GrafikDokument1 SeiteKerangka GrafikQeis RamadhanNoch keine Bewertungen
- 2016 - 13 - Fleming - Lagged Syndesmotic Fixation - Our Clinical ExperienceDokument8 Seiten2016 - 13 - Fleming - Lagged Syndesmotic Fixation - Our Clinical ExperienceJacob DoughertyNoch keine Bewertungen
- CHN 1 Skills ModuleDokument31 SeitenCHN 1 Skills ModuleGia Espinosa OcbeñaNoch keine Bewertungen
- USMLE 2013 BulletinDokument41 SeitenUSMLE 2013 BulletinKarachibreezeNoch keine Bewertungen
- Transcutaneous Electrical Nerve Stimulation (TENS) - To PrintDokument22 SeitenTranscutaneous Electrical Nerve Stimulation (TENS) - To PrintRajesh Shan100% (1)
- Mackenzie Renee Rotella CV FNP 2016Dokument2 SeitenMackenzie Renee Rotella CV FNP 2016api-311611085Noch keine Bewertungen
- 14 23gowrisankarTONGUETHRUSTHABIT Areview.Dokument11 Seiten14 23gowrisankarTONGUETHRUSTHABIT Areview.ranaNoch keine Bewertungen
- Potter: Fundamentals of Nursing, 8 EditionDokument2 SeitenPotter: Fundamentals of Nursing, 8 Editionsammm9960% (1)
- Drug StudyDokument7 SeitenDrug StudyGladys NacionNoch keine Bewertungen
- Crutchwalking QuizDokument2 SeitenCrutchwalking QuizflorenzoNoch keine Bewertungen
- Hypertension in pregnancy-ACOG 2013-1 PDFDokument100 SeitenHypertension in pregnancy-ACOG 2013-1 PDFrabinreaganNoch keine Bewertungen
- The Neutral Zone: Concept and Technique: 10.5005/jp-Journals-10026-1010 Review ArticleDokument6 SeitenThe Neutral Zone: Concept and Technique: 10.5005/jp-Journals-10026-1010 Review ArticleAndres FernandezNoch keine Bewertungen
- Pro DrugDokument4 SeitenPro DrugIbnu SinaNoch keine Bewertungen
- Smiths Fluid Warmer - General Technical ManualDokument131 SeitenSmiths Fluid Warmer - General Technical Manualmeet_vaghaniNoch keine Bewertungen
- 1452 A. Lacson St. Sta. Cruz, Manila College of Nursing: The Family Clinic, Inc. - CollegesDokument1 Seite1452 A. Lacson St. Sta. Cruz, Manila College of Nursing: The Family Clinic, Inc. - CollegesCatherine MetraNoch keine Bewertungen
- PTSD Women Combat VeteransDokument6 SeitenPTSD Women Combat VeteransMisty JaneNoch keine Bewertungen
- Pancreatitis Acute - StatPearls - NCBI BookshelfDokument6 SeitenPancreatitis Acute - StatPearls - NCBI BookshelfJosé Jefferson Da SilvaNoch keine Bewertungen