Beruflich Dokumente
Kultur Dokumente
Cardio, Otis, Ortho, and GI Drug Lists
Hochgeladen von
Jodi Gugel DeMarrowOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Cardio, Otis, Ortho, and GI Drug Lists
Hochgeladen von
Jodi Gugel DeMarrowCopyright:
Verfügbare Formate
Cardiovascular Drugs Toprol (Lopressor) Zestril (lisinopril) Cozaar (losartan) Cardizem Digoxin Amiodorone Nitroglycerin Heparin, Coumadin Lasix
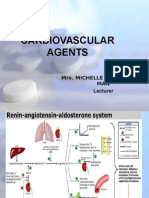
Aldosterone Coumadin antidote Heparin antidote Heparin blood labs Coumadin blood labs Contraindications for anticoagulants HDL norms LDL norms Rabdomylosis Beta-Blockers Beta-Blocker implications Beta-Blocker Prototype ACE-Inhibitor Prototype Angiotensin II Receptor Blockers (ARBs) Prototype Calcium Channel Blocker Prototype Cardiac Glycoside Prototype Antiarrythmic Prototype Nitrate Prototype Anticoagulants Prototypes Diuretic Prototype Potassium sparing diuretic Vitamin K Protamine Sulfate PTT PT/INR Hemophilia, liver disease, bone marrow disorders, ASA, Plavix, lovenox >40 <100 Muscle breakdown that can cause kidney failure; watch for with hyperlipidemic agents Blocks vasoconstriction; most drugs end in ol; causes decreased heart rate Contraindicated in COPD; may mask hypoglycemic reaction(lack of sweating); hold if HR<60; can cause fluid build-up, watch in CHF Blocks conversion of angiotensinI to II, therefore not moving to aldosterone thus releasing Na and water causing less volume but increasing potassium; most end in il Withhold from poor renal function, watch BUN creatinine; used for HTN,CHF and MI Renal insufficiency, cough, angina, cardiac arrhythmias due to potassium imbalances Bind angiotensin II receptors in bvs to prevent vasoconstriction; used for those intolerant to ACE to treat HTN usually with other meds; ex: Diovan Cozaar, Avapro, Atacand; many end in sartan Dizziness, headache,cough,muscle weakness (Na and K imbalances) alopecia Only PO; caution with liver and kidney disease; use with caution if on phenobarbital Slow movement of Ca into cardiac and smooth muscle thus causing vasodilation decreasing bp and cardiac workload; ex: Norvasc (BP), Cardizem(A-fib),Calan, Cardene
ACE Inhibitors
ACE Inhibitor implications ACE side effects ARBs
ARB side effects ARB implications Calcium Channel Blockers
Ca Channel Blocker side effects Ca Channel implications
Digoxin therapeutic range Dig toxicity Cardiac Glycoside implications Antiarrythmics
Antiarrythmic side effects Antiarrythmic implications
Nitrates side effects Nitrates Nitrate implications
Thrombolytics Thrombolytic contraindications
Bradycardia, heart blocks, dizziness, orthostatic hypotension. PO or IV;extended release form for HTN;interacts with grapefruit juice; blocks enzymes in small intestine 0.8-2.0 Yellow halo around objects, heacache, drowsiness <60hold; watch e-lytes: increase Ca, decreased K, decreased Mg;antidote to dig toxicity:digibind Class III block K channel which prolongs repolarization slowing down the rate and conduction of heart;ex: Amiodorone and betapace May produce vasodilation, hypotension and arrhythmias (bradycardia) First line treatment for ventricular fib and ventricular tachycardia; load patient with IV than PO; must be in glass container with filter; long half life>30days; no grapefruit juice Severe hypotension; headache, dizziness,skine redness with patch Reduces cardiac workload by vasodilation IV,sublingual,transdermal(gloves!); burns under tongue;take one every 5 minutes with a max of 3;rapid absorption; carried in dark bottle Clot busters; all IV Post-op; ulcers and GI bleeding; CVa within 2 months; trauma; uncontrolled HTN; liver disease; pregnancy
GI Drugs Antispasmodics Bentyl Antidiarrheals Lomotil Laxatives Metamucil Milk of Magnesia; Magnesium Citrate Dulcolax Colace Peptic ulcers PUD GERD Antacid Interactions Decrease muscle tone, reduce mobility of GI tract Antispasmodic Decrease GI mobility Antidiarrheal Bulk forming; chemical stimulant; lubricant Bulk forming Osmotic-pulls in water Stimulates peristalsis Stool softener-pulls in water and fats Dark tarry stools H. pylori infection Esophageal stricture; improper working of lower esophageal sphincter Alters drug absorption; do not give within 1-2 hours of other meds
Zollinger-Ellison Syndrome
Excessive acid production-H2 receptor antagonist used to treat Proton Pump Inhibitors Increased anticholinergic effects when used with antihistamines and antidepressants Stomach infection due to acid killing bacteria Narrow angle glaucoma; GI obstruction Stimulates hydrochloric acid Cause parietal cells to release more hydrochloric acid
Use when H2 blockers ineffective Antispasmodic interactions Long term use of Proton Pump Inihibitors Contraindications for antidiarrheals Gastrin H2 receptors
What is Glaucoma Disease of the major nerve of vision What is the cause of Glaucoma Usually related to elevated pressure in the eye (intraocular pressure) Also build up of the aqueous humor is the most common cause What is the goal in treatment Reduce IOP, Increase drainage of aqueous humor, decrease production of aqueous How do the anticholingeric work -Miosis, increase the rate of the fluid that leaves the eye, encourage the small muscles inside your eye to work harder. SE- Blurred vision, HA, bradycardia How is sympathomimetics work -Diviverfrin reduces the amount of fluid in the eye, which decreases the pressure. Stimulates the dilator muscle in results mydriasis, increase drainage decrease pressure SE- Ocular burning, lacrimation (tears) How do Beta blockers work?
-Decrease production of aqueous humor SE- Ocular burning, blurred vision, bronchospasms, arrhythmias What side effects are you worried about for each? See above How do you properly instill eye drops and ear drops? -wash hands -tilt head back slightly & pull down lower eyelid to create a small pocket -gently press on the intracanthus for 30 to 60 -Do not allow dropper tip to touch any surface, including the eyes or hands
Das könnte Ihnen auch gefallen
- Pharmacotherapy of Hypertention TerbaruDokument45 SeitenPharmacotherapy of Hypertention TerbarulisaNoch keine Bewertungen
- Pharmacology Chapter 42 p-3Dokument19 SeitenPharmacology Chapter 42 p-3sho bartNoch keine Bewertungen
- Antihypertensive Pharmacologic Agents: Nr33 K Burger, Msed, MSN, RN, CneDokument28 SeitenAntihypertensive Pharmacologic Agents: Nr33 K Burger, Msed, MSN, RN, CneLopez JoeNoch keine Bewertungen
- CHF Drugs Guide: Key Medications for Treating Congestive Heart FailureDokument21 SeitenCHF Drugs Guide: Key Medications for Treating Congestive Heart Failuremohsen mirdamadiNoch keine Bewertungen
- 09 Diuretics UpdDokument42 Seiten09 Diuretics UpdYeni Chie Aneuk TuleutNoch keine Bewertungen
- Drug ListsDokument10 SeitenDrug ListsAmber Merritt100% (1)
- Cardiac Med ChartsDokument6 SeitenCardiac Med ChartsNursingSchoolNotes100% (15)
- Cardiotonic DrugsDokument67 SeitenCardiotonic DrugsLady Mae Ramos100% (1)
- Pharma Medications ListDokument35 SeitenPharma Medications ListCalvin Keith YadaoNoch keine Bewertungen
- Pharmacology: Unit VIIIDokument92 SeitenPharmacology: Unit VIIIChristian Laraya AlayonNoch keine Bewertungen
- Cardiology Review: HTN: Julia Akaah M.DDokument40 SeitenCardiology Review: HTN: Julia Akaah M.DJose LunaNoch keine Bewertungen
- Meds #1 NotesDokument4 SeitenMeds #1 NotesAnh TrinhNoch keine Bewertungen
- DiureticsDokument28 SeitenDiureticsmohsen mirdamadiNoch keine Bewertungen
- 1 Antihypertensive DrugsDokument14 Seiten1 Antihypertensive DrugsReda SoNoch keine Bewertungen
- Cardiovascular Pharmacology OutlineDokument11 SeitenCardiovascular Pharmacology OutlineLhay de OcampoNoch keine Bewertungen
- Cardiac DrugsDokument8 SeitenCardiac Drugsdawggj100% (2)
- DBP: Diastolic Blood Pressure SBP: Systolic Blood PressureDokument7 SeitenDBP: Diastolic Blood Pressure SBP: Systolic Blood PressureM. JoyceNoch keine Bewertungen
- Cardiovascular Agents: Mrs. Michelle A. Iduria, RN, MAN LecturerDokument131 SeitenCardiovascular Agents: Mrs. Michelle A. Iduria, RN, MAN LecturerNiala AlmarioNoch keine Bewertungen
- Drugs for Hypertension 2023 (1)Dokument19 SeitenDrugs for Hypertension 2023 (1)aguilarjanicaNoch keine Bewertungen
- Cardiac MedsDokument7 SeitenCardiac MedsMary Fair DelcidNoch keine Bewertungen
- Drugs Used in HF IIDokument40 SeitenDrugs Used in HF IIJamal LudinNoch keine Bewertungen
- Pharmacology RCR1 RenalDokument6 SeitenPharmacology RCR1 RenaleamcrawleyNoch keine Bewertungen
- Diuretics: DR Mozna TalpurDokument33 SeitenDiuretics: DR Mozna TalpurShahid HameedNoch keine Bewertungen
- Obat Gagal Jantung N Anti AnginaDokument42 SeitenObat Gagal Jantung N Anti AnginaAyu Devi YantiNoch keine Bewertungen
- Drugs WorksheetDokument16 SeitenDrugs Worksheetninja-2001Noch keine Bewertungen
- Hypertension: Classification, Effects and TherapyDokument35 SeitenHypertension: Classification, Effects and TherapyDevi Septiani D3-2019Noch keine Bewertungen
- Sympatholytic DrugsDokument20 SeitenSympatholytic DrugsAudrey Beatrice Reyes100% (1)
- Cardiovascular Agents PDFDokument118 SeitenCardiovascular Agents PDFgherlethrNoch keine Bewertungen
- Cholinergic System: e CarbamatesDokument26 SeitenCholinergic System: e CarbamatesAcai BoncaiNoch keine Bewertungen
- Cardio Winter BreakDokument13 SeitenCardio Winter Breakmadhungry34Noch keine Bewertungen
- CVS PharmacologyDokument60 SeitenCVS PharmacologyGølà Sèèñàà–baale irraaNoch keine Bewertungen
- Congestive Heart Failure ReportDokument6 SeitenCongestive Heart Failure ReportSunshine_Bacla_4275100% (1)
- AntiHypertensives (Autosaved)Dokument64 SeitenAntiHypertensives (Autosaved)UsamaNoch keine Bewertungen
- Topic - Diuretics: Submitted By, Group - 07Dokument28 SeitenTopic - Diuretics: Submitted By, Group - 07Arvi KhanNoch keine Bewertungen
- Antiplatelet and Proton Pump Inhibitor Drug Study SummaryDokument9 SeitenAntiplatelet and Proton Pump Inhibitor Drug Study SummaryrocketwapNoch keine Bewertungen
- ACE Inhibitors: Medications To Control Blood PressureDokument3 SeitenACE Inhibitors: Medications To Control Blood PressurekNoch keine Bewertungen
- DRUG THERAPY FOR HEART FAILUREDokument40 SeitenDRUG THERAPY FOR HEART FAILURENiteesh Kumar SharmaNoch keine Bewertungen
- Anti Hypertensive DrugsDokument46 SeitenAnti Hypertensive DrugsShabaka KashataNoch keine Bewertungen
- Understanding Hypertension: Causes, Symptoms, TreatmentDokument16 SeitenUnderstanding Hypertension: Causes, Symptoms, TreatmentJheanAlphonsineT.MeansNoch keine Bewertungen
- Drugs Acting On Cardiovascular SystemDokument81 SeitenDrugs Acting On Cardiovascular SystemevaNoch keine Bewertungen
- 10-11 Treatment of HypertensionDokument11 Seiten10-11 Treatment of HypertensionHanif GandohNoch keine Bewertungen
- Anti-Anginal Drugs ExplainedDokument19 SeitenAnti-Anginal Drugs ExplainedAnusha ZubairNoch keine Bewertungen
- Set 4c16c8b0Dokument4 SeitenSet 4c16c8b0davidvpnNoch keine Bewertungen
- HTNDokument15 SeitenHTNNatukunda DianahNoch keine Bewertungen
- Antianginal Drugs: Roger Joseph Ii R. Jecino, M.DDokument31 SeitenAntianginal Drugs: Roger Joseph Ii R. Jecino, M.DFranz Earl Niño AlbesaNoch keine Bewertungen
- Anti Hypertensive 20191211Dokument35 SeitenAnti Hypertensive 20191211helloitsmenadNoch keine Bewertungen
- Congestive Heart Failure: CardiacDokument36 SeitenCongestive Heart Failure: CardiacHUZAIFA YAMAANNoch keine Bewertungen
- Anoosha Roll#21Dokument19 SeitenAnoosha Roll#21Anusha ZubairNoch keine Bewertungen
- Drugs For Congestive Heart FailureDokument46 SeitenDrugs For Congestive Heart Failuresultan khabeeb100% (1)
- Drug Presentation On Anti-Hypertensive: All India Institute of Medical and Science New Delhi 2021-2022Dokument12 SeitenDrug Presentation On Anti-Hypertensive: All India Institute of Medical and Science New Delhi 2021-2022Priya SinghNoch keine Bewertungen
- Antihypertensive Drugs: Dr/Azza Baraka Prof of Clinical Pharmacology Faculty of Medicine Alexandria UniversityDokument71 SeitenAntihypertensive Drugs: Dr/Azza Baraka Prof of Clinical Pharmacology Faculty of Medicine Alexandria UniversityMoonAIRNoch keine Bewertungen
- Cardiovascular Drugs Coronary Arteries: Myocardial InfarctionDokument1 SeiteCardiovascular Drugs Coronary Arteries: Myocardial Infarctionsharu4291Noch keine Bewertungen
- HypertensionDokument54 SeitenHypertensionBadri KarkiNoch keine Bewertungen
- Hypertension Guide: Causes, Types, Symptoms, TreatmentDokument10 SeitenHypertension Guide: Causes, Types, Symptoms, TreatmentHarold CapidosNoch keine Bewertungen
- HTNDokument54 SeitenHTNapi-232466940Noch keine Bewertungen
- Department of Clinical Pharmacology: Pharmacotherapy of Chronic Ischemic Heart DiseaseDokument84 SeitenDepartment of Clinical Pharmacology: Pharmacotherapy of Chronic Ischemic Heart DiseasePatty ReyesNoch keine Bewertungen
- Bihs PDFDokument4 SeitenBihs PDFFredrikus Lay Berkh MansNoch keine Bewertungen
- A Simple Guide to Hypertension and Heart DiseasesVon EverandA Simple Guide to Hypertension and Heart DiseasesBewertung: 5 von 5 Sternen5/5 (1)
- Statement of The Problem: Notre Dame of Marbel University Integrated Basic EducationDokument6 SeitenStatement of The Problem: Notre Dame of Marbel University Integrated Basic Educationgab rielleNoch keine Bewertungen
- Factors Affecting English Speaking Skills of StudentsDokument18 SeitenFactors Affecting English Speaking Skills of StudentsRona Jane MirandaNoch keine Bewertungen
- Ghaziabad Resume Amresh Kumar Upadhyay Desktop EngineerDokument2 SeitenGhaziabad Resume Amresh Kumar Upadhyay Desktop EngineerRipunjay MishraNoch keine Bewertungen
- AFRICAN SYSTEMS OF KINSHIP AND MARRIAGEDokument34 SeitenAFRICAN SYSTEMS OF KINSHIP AND MARRIAGEjudassantos100% (2)
- The Five Laws of Light - Suburban ArrowsDokument206 SeitenThe Five Laws of Light - Suburban Arrowsjorge_calvo_20Noch keine Bewertungen
- Settlement of Piled Foundations Using Equivalent Raft ApproachDokument17 SeitenSettlement of Piled Foundations Using Equivalent Raft ApproachSebastian DraghiciNoch keine Bewertungen
- Tong RBD3 SheetDokument4 SeitenTong RBD3 SheetAshish GiriNoch keine Bewertungen
- Hadden Public Financial Management in Government of KosovoDokument11 SeitenHadden Public Financial Management in Government of KosovoInternational Consortium on Governmental Financial ManagementNoch keine Bewertungen
- Tax Invoice/Bill of Supply/Cash Memo: (Original For Recipient)Dokument1 SeiteTax Invoice/Bill of Supply/Cash Memo: (Original For Recipient)Pravin AwalkondeNoch keine Bewertungen
- Lesson 1 Reviewer in PmlsDokument10 SeitenLesson 1 Reviewer in PmlsCharisa Joyce AgbonNoch keine Bewertungen
- Activity 1 DIASSDokument3 SeitenActivity 1 DIASSLJ FamatiganNoch keine Bewertungen
- Mastering ArpeggiosDokument58 SeitenMastering Arpeggiospeterd87Noch keine Bewertungen
- The Highest Form of Yoga - Sant Kirpal SinghDokument9 SeitenThe Highest Form of Yoga - Sant Kirpal SinghKirpal Singh Disciple100% (2)
- MW Scenario Handbook V 12 ADokument121 SeitenMW Scenario Handbook V 12 AWilliam HamiltonNoch keine Bewertungen
- 1120 Assessment 1A - Self-Assessment and Life GoalDokument3 Seiten1120 Assessment 1A - Self-Assessment and Life GoalLia LeNoch keine Bewertungen
- RumpelstiltskinDokument7 SeitenRumpelstiltskinAndreia PintoNoch keine Bewertungen
- Will You Be There? Song ActivitiesDokument3 SeitenWill You Be There? Song ActivitieszelindaaNoch keine Bewertungen
- 2019 Batch PapersDokument21 Seiten2019 Batch PaperssaranshjainworkNoch keine Bewertungen
- Brain Chip ReportDokument30 SeitenBrain Chip Reportsrikanthkalemla100% (3)
- 1 - Nature and Dev - Intl LawDokument20 Seiten1 - Nature and Dev - Intl Lawaditya singhNoch keine Bewertungen
- 12.1 MagazineDokument44 Seiten12.1 Magazineabdelhamed aliNoch keine Bewertungen
- Adic PDFDokument25 SeitenAdic PDFDejan DeksNoch keine Bewertungen
- ModalsDokument13 SeitenModalsJose CesistaNoch keine Bewertungen
- Consent 1095 1107Dokument3 SeitenConsent 1095 1107Pervil BolanteNoch keine Bewertungen
- Poetry Recitation Competition ReportDokument7 SeitenPoetry Recitation Competition ReportmohammadNoch keine Bewertungen
- The Insanity DefenseDokument3 SeitenThe Insanity DefenseDr. Celeste Fabrie100% (2)
- ISA standards, materials, and control room conceptsDokument8 SeitenISA standards, materials, and control room conceptsGiovanniNoch keine Bewertungen
- 2Dokument5 Seiten2Frances CiaNoch keine Bewertungen
- February / March 2010Dokument16 SeitenFebruary / March 2010Instrulife OostkampNoch keine Bewertungen
- IB Theatre: The Ilussion of InclusionDokument15 SeitenIB Theatre: The Ilussion of InclusionLazar LukacNoch keine Bewertungen