Beruflich Dokumente
Kultur Dokumente
ABL p210, p190 and p230 Fusion Genes in 250 Mexican Patients With Chronic Myeloid Leukaemia (CML) - ARANA-TREJO 2022
Hochgeladen von
Angel Lugo TrampeOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
ABL p210, p190 and p230 Fusion Genes in 250 Mexican Patients With Chronic Myeloid Leukaemia (CML) - ARANA-TREJO 2022
Hochgeladen von
Angel Lugo TrampeCopyright:
Verfügbare Formate
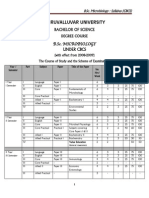
Clin. Lab. Haem.
2002, 24, 145150
BCR/ABL p210, p190 and p230 fusion genes in 250 Mexican patients with chronic myeloid leukaemia (CML)
*Genetica, Hospital General de Mexico, O.D. Facultad de Medicina, UNAM. Mexico D.F., Hematologa Hospital Regional #1 Gabriel Mancera, IMSS. Mexico D.F., Hospital de Especialidades CMNO, IMSS Guadalajara, Jal., Hospital Especialidades #25, IMSS Monterrey, N.L., Hospital de Especialidades CMN SXXI, IMSS. Mexico D.F., **Hospital de Especialidades #71, IMSS. Torreon, Coahuila, Hospital Angeles de las Lomas, S.A. and Biotecnologa, Grupo Roche/Sintex, S.A de C.V., Mexico
R.M. ARANA-TREJO*, E. RUIZ SANCHEZ*, G. IGNACIO-IBARRA, E. BAEZ DE LA FUENTE, O. GARCES, E. GOMEZ MORALES, M. CASTRO GRANADOS**, R. OVILLA MARTINEZ, M.E. RUBIO-BORJA, L. SOLIS ANAYA, P. HERRERA, J. DELGADO LLAMAS, S. KOFMAN* Summary
There are two major forms of the BCR/ABL fusion gene, involving ABL exon 2, but including different exons of BCR gene. The transcripts b2a2 or b3a2 code for a p210 protein. Another fusion gene leads to the expression of an e1a2 transcript, which codes for a p190 protein. Another, less common fusion gene is c3a2[e19a2], which encodes a p230 protein. The incidence of one or the other rearrangement in chronic myeloid leukaemia (CML) patients varies in different reported series. This study was designed to determine the frequency of coexpresion of the p210, p190 and p230 transcripts in 250 Mexican patients with CML. We performed nested and multiplex reverse transcriptase polymerase chain reaction (RT-PCR) on bone marrow samples from adult patients and found that all cases were positive for some type of BCR/ABL rearrangement. In 226 (90.4%) patients it was p210, while the remaining 9.6% showed coexpression or one of the transcripts of p190/p210/p230. In 7% of patients with p210 expression there are both isoforms (b3a2/b2a2), presumably the result of alternative splicing. The rate of coexpression of the p190/p210 transcripts was 5%, which is much lower than in other reports. This may be due to the technical factors. These patients had high platelet counts, marked splenomegaly and chromosomal abnormalities in addition to Ph. Other types of coexpression seen were p210/p230 and p190/p210/p230, in patients with high-risk clinical factors. Our study conrms the occurrence of coexpression of different BCR/ABL transcripts, although the rate (9.6%) was much lower than has been reported in other populations. This may reect either the sensitivity of the detection techniques used or the possibility of genetic differences between the populations studied. Coexpression may be due to alternative splicing or to phenotypic variation, with clinical courses different from classical CML. BCR-ABL, CML, alternative splicing, p210, p190, p230
Keywords
Accepted for publication 7 February 2002 Correspondence: R.M. Arana Trejo, Genetica, Hospital General de Mexico, Dr Balmis #148, Col. Doctores Mexico, D.F. C.P. 06726, Mexico. Fax: 01(55)5761-93-71; E-mail: aranat@prodigy.net.mx 2002 Blackwell Science Limited
145
146
BCR/ABL in CML Mexican patients
Introduction
The molecular consequence of t(9; 22)(q34;q11) is the formation of two hybrid genes: BCR/ABL on the Ph chromosome and ABL/BCR on 9q+ (Kurzrock, Gutterman & Talpaz, 1988; van Dongen et al., 1999). The BCR/ABL fusion protein can vary from 190 kDa to 230 kDa, depending on the site of the breakpoint in the BCR gene. In the vast majority of chronic myeloid leukaemia (CML) cases, as well as in 30% of adult acute lymphoblastic leukaemia chromosome Philadelphia positive (Ph + ALL) and 20% of childhood Ph+ ALL, the breakpoints in the BCR gene are found within the M-bcr region (Melo, 1996; Emilia et al., 1997; Giovanni et al., 1997; Parziale et al., 2000). This is a 5.8Kb region spanning 5 exons named b1 to b5, now known to be exons 1216 of the BCR gene. All CML patients have their breakpoints in the 2.9 kb region between BCR exons 13 and 15 [b2 and b4], that fuse to the large intron between ABL exons 1b and 2b. This results in a hybrid BCR/ABL transcript of 8.5 kb, containing either BCR exon b2 or b3 and ABL exon 2 [a2]. This mRNA encodes the 210 kDa BCR/ABL protein [p210BCR/ABL.]. The majority of CML patients have transcripts with b3a2 (55%) or b2a2 (40%) junctions; in 5% of the cases, both b3a2 and b2a2 transcripts can be formed as a result of alternative splicing (Okamoto et al., 1997; Lichty et al., 1998). In two thirds of ALL cases and in rare cases of CML and acute myeloid leukaemia (AML), the breakpoint in BCR falls further upstream, in the long (54.4 kb) intron between the two alternative exons e2 and e2, known as the minor bcr [m-bcr]. Under these circumstances, exon e1 and e2 are removed by splicing. The hybrid BCR/ABL transcript contains an e1a2 junction, and is translated into a smaller 190-kDa BCR/ABL fusion protein [p190BCR/ABL.] (Okamoto et al., 1997; Lemes et al., 1999; Li et al., 1999; van Dongen et al., 1999). In some cases, Ph+ CML displays a larger BCR/ABL fusion transcript, resulting from a fusion between the BCR exon 19 (originally named c3) and ABL exon 2. This is caused by a breakpoint in the micro breakpoint cluster region (u-bcr) between BCR exon 19 and 20. This BCR/ABL fusion gene encodes a large 230 kDa BCR/ABL protein [p230BCR/ABL.] (Pane et al., 1996; Mittre et al., 1997; Haskovec et al., 1998). This study was designed to determine the frequency of coexpression of the BCR/ABL rearrangement in 250 Mexican patients with CML. We interpreted the detection of two or more p190, p210 or p230 encoding transcripts in the same patient sample as coexpression.
Methods
Patients and samples Bone marrow samples from 250 patients with a referring diagnosis of CML were obtained for cytogenetics and molecular studies. The patients were diagnosed and treated at various centres in Mexico between January 1997 and March 2001. The median age was 40 years (range 1680 years), 48% were female and 52% were male. Seven patients were in accelerated phase, 20 were in blast crisis and the remaining 223 were in chronic phase at time of molecular testing. The patients were categorized according to phase (chronic, accelerated or blast crisis) and according to Sokal risk (low, intermediate and high risk) (Sokal et al., 1984; Cortes et al., 1997; Hasford et al., 1998). Cytogenetics Chromosomal studies were done on bone marrow cells using the direct technique or after 24 h culture in vitro, without stimulation (Rooney & Czepulkowski, 1992). The chromosomes were identied using a GTG-banding technique and 1530 metaphases were analysed (Junis, Sawyer & Ball, 1978). The karyotypes were reported according to the ISCN nomenclature (ISCN & Mitelman, 1995). Metaphases for cytogenetic study were obtained from only 215 patients. RNA extraction Bone marrow samples were diluted in a NH4Cl: Tris solution to lyse the red cells and the white cell fraction was pelleted and washed once in PBS. Total RNA was extracted from the white cell pellets using the acid guanidinium thiocyanate-phenol-chloroform extraction method. The quality of RNA was evaluated in denaturing electrophoretic gels (Chomczynski & Sachi, 1987; van Dongen et al., 1999). Reverse transcriptase-PCR Total RNA was reversed transcribed according to standard protocols. The BCR/ABL rearrangement was amplied using multiplex and nested polymerase chain reactions (PCR). The primers were designed for p190, p210 and p230 and permit the detection of junctions e1a2, b2a2, b3a2 and c3a2. The PCR products were visualized using agarose gel electrophoresis with ethidium bromide staining. In the multiplex PCR, the bands should be as follows: 808 bp, normal BCR; 481 bp, e1a2; 385 bp and/or
2002 Blackwell Science Ltd., Clin. Lab. Haem., 24, 145150
R.M. Arana Trejo et al.
147
310 bp, b3a2 and b2a2, respectively. An amplied product from the BCR gene is the only band detected in BCR/ABL negative patients. The presence of this band indicates that the quality of the RNA and the efciency of cDNA synthesis were good; absence of this band indicates procedural failure. In the nested PCR, the bands should be 458 bp (b3a2), 383 bp (b2a2), 444 bp (e1a2) or 580 (c3a2/e19a2) (Cross, Lin & Goldman, 1994; Cotter, 1996; Kidd & Lion, 1997; Burmeister et al., 2000).
Results
Cytogenetic studies were carried out in 215 of the 230 patients studied (86%), demonstrating t(9; 22)(q34;q11) as the sole cytogenetic abnormality in 157 patients and additional chromosomal abnormalities in 58 patients (27%). These secondary aberrations were mainly hyperdiploidy, +8, +9, i(17q), hypodiploidy, del (7q) and del (6q). For screening the BCR/ABL mRNA transcripts, we used multiplex PCR to detect several kinds of rearrangements simultaneously with BCR transcripts as internal controls in a single reaction. This method enables the reliable detection of typical p210 transcripts, such b2a2 or b3a2,
and atypical types, such as transcripts lacking ABL exon a2 (b2a3 and b3a2), or p190BCR/ABL. transcripts, such as e1a2. By using nested RT-PCR with two pairs of primers corresponding to appropriate BCR and ABL exons in two rounds of amplication, we could detect transcripts at levels as low as 110 copies in 1056 normal cells and could conrm the presence of the p190, p210 and p230 BCR/ABL transcripts observed in the multiplex RT-PCR reaction (Figures 1 and 2). Using RT-PCR, the majority of the patients (226/250, 90.4%) expressed one of the p210BCR/ABL. rearrangements (b3a2 or b2a2), while the rest (24/250, 9.6%) had coexpression of one of the transcripts of p190/p210/p230 (Table 2). Of the cases positive for p210, 48% corresponded to the b2a2 type, 35% to b3a2 and 7% coexpressed both transcripts (b2a2/b3a2). The median age for all of the cases was over 40 years, while for patients expressing both b3a2/b2a2, the median age was 51. Table 1 shows clinical data for the patients according to BCR/ABL transcript type. Four patients (2%) were negative for rearrangements in the larger and smaller BCR (M-BCR/p210 and m-BCR/ p190) regions, but positive for e19a2 or c3a2 in the p230 (u-BCR) transcript. Clinical data for these patients corres-
Figure 1. Multiplex PCR. Line M: 100pb marker; lines 1 and 5: Ph-positive CML with b3a2 BCR/ABL (385pb); line 2 and 4: Ph-positive CML with b2a2 BCR/ABL CML (310pb); line 3: Ph-positive CML with both b3a2/b2a2 transcripts; line 6: control Ph-negative BCR/ABL-negative; line 7: H2O negative control. Lines 16 present the 808pb band product from the BCR gene and indicate the quality of the RNA and efciency of the cDNA synthesis.
Figure 2. Nested RT-PCR. Line 100pb molecular marker; lines b3a2/b2a2 Ph-positive CML with both p210BCR/ABL. transcripts (458pb and 383pb); lines b3a2: Ph-positive CML with M-BCR (458pb); lines e1a2: Ph-positive CML with p190BCR/ABL. transcripts (444pb); line e19a2: Ph-positive CML with p230BCR/ABL. transcripts (580pb); line C-: H2O negative control.
Table 1. Incidence of the rearrangements of BCR/ABL and Sokal risk Rearreglo BCR/ABL P210 P190/p210 P230 P210/p230 P190/p210/p230 Total Case [%] 226 [90.4%] 16 [6.4%] 4 [1.6%] 2 [0.8%] 2 [0.8%] 250 # Patients with sokal Score 190/226 12/16 2/4 2/2 2/2 208/250 (83%) Sokal low 73 2 Sokal intermediate 61 6 Sokal high 56 4 2 2 2 66 (32%)
75 (36%)
67 (32%)
2002 Blackwell Science Ltd., Clin. Lab. Haem., 24, 145150
148
BCR/ABL in CML Mexican patients
ponded to classical CML, with leukocytosis and thrombocytosis (means: 320 109/l and 865 109/l, respectively), their ages ranging from 38 to 59 years. Using cytogenetic techniques, only two patients had t(9; 22), while in two other patients, hyperdiploid metaphases were seen with a double Ph chromosome, indicating disease progression. These patients were classied as high risk by Sokals score. Co-expression of p190 and p210 rearrangements was detected in 16 cases (6%). These patients had high WBC and platelet counts (means: 400 109/l and 690 109/l, respectively) and a high percentage had chromosomal abnormalities in addition to Ph. Another four patients coexpressed transcripts BCR/ABL: two were p230/p210 positive and two others were positive for a combination of p190/p210/p230, detected by nested RT-PCR. These cases were diagnosed as chronic-phase CML, with cytogenetic abnormalities in addition to t(9; 22) and high risk clinical data, based on Sokals score.
30
21
Intermediate
30
26
*Sokal Risk
Low
***Other Ph abnormality
12 (325)
12 (118)
5 (122)
12 (325)
Marrow blast (%)
7 (510)
6 (58)
15 (220)
Spleen (cms)
14 (1018)
23/109 (21%) 15/75 (20%) 5/12 (42%) 8/11 (73%) 3/4 (75%) 2/2 (100%) 2/2 (100%)
58/215 (27%)***
75/208 36%
40
30
67/208 32%
66/208 32%
High
34
Discussion
In this study we found a low incidence of p190, p210 and p230 BCR/ABL fusion gene coexpression (9.6%), although these were very heterogeneous. In 90.4% of the cases, only fusion involving the M-BCR region was seen, corresponding to p210, although 7% had both b3a2 and b2a2 isoforms, supporting the hypothesis of alternative splicing of the primary transcript. We did not observe signicant differences between the three different M-BCR breakpoint groups with respect to the clinical ndings, although the group expressing both transcripts (b3a2/ b2a2) had a mean age of 51, while those expressing b3a2 and b2a2 were on the average, below 40 years. Based on clinical risk, the majority fell within low and intermediate risk groups. In 1.6% of the cases (4/250), the breakpoint position varied within the u-BCR region (c3a2 or e19a2), producing the p230 protein. This is associated with the neutrophilic CML or the CML with thrombocytopenia phenotype, considered high risk, based on Sokals criteria. Cases with these rearrangements often show marked thrombocytopenia and splenomegaly. This junction (e19a2) was rst studied because of a discrepancy between cytogenetic ndings, showing Ph positivity in all cases, and the multiplex and nested RT-PCR ndings, showing no rearrangement of the M-BCR or m-BCR regions. The rate of coexpression of the p190 and p210 transcripts was 5%, which is much lower than that reported in other series. This may be due to the techniques used, although we cannot disregard ethnic differences.
2002 Blackwell Science Ltd., Clin. Lab. Haem., 24, 145150
690 (3501500)
481 (1001200)
467 (364570)
413 (18907)
865 (8401090)
b2a2 [p210] b3a2 [p210] b3a2/b2a2 [p210] e1a2/b3a2/b2a2 [p190/p210] c3a2 [e19a2] [p230] c3a2/b3a2 [p230/p210] e1a2/b2a2/c3a2 [p190/p210/p230]
Total
*Sokal ratio was calculated for 208 patients; ***Only 215 patients had a cytogenetic study.
PLTS (109/l)
399 (340462)
195 (12800)
217 (21773)
158 (120207)
WBC (109/l)
320 (240400)
340 258
474 44 (4345) 2 (1) 250 40 129/121 1/1
56/64
Gender (M/F)
51/37
10/8
9/7
2/2
Table 2. Patients data and BCR/ABL rearrangement
Median age (year) (range)
40 (1679)
38 (1780)
51 (2966)
32 (2446)
120 (48)
88 (35)
18 (7)
16 (6)
Rearrangement BCR/ABL
n (%)
2 (1)
4 (2)
49 (4256)
49 (3859)
0/2
540
R.M. Arana Trejo et al.
149
The sensitivity of the primer combinations used in our multiplex PCR give a sensitivity of between 103 and 104. This increases in the nested PCR to between 105 and 106. In spite of this sensitivity, the expression level of the p190 transcript is much lower than that of the p210 transcript, limiting its detectability. With respect to the clinical ndings, patients coexpressing both transcripts had high WBC counts and the majority fell within the intermediate or high risk groups when compared with those expressing only p210 transcripts, as reported in other series. Patients who were p190/p210-positive had high platelet counts, marked splenomegaly and chromosomal abnormalities additional to Ph in 60% of cases. The majority were hyperdiploid karyotypes, with more than 50 chromosomes, more typical of a lymphoid-type blastic phase CML than an atypical presentation. In view of the apparent lack of association with any clinical feature of either CML or ALL, the presence of e1a2 transcripts in p210BCR/ABL. CML is probably of no pathogenetic signicance. However, coexpression of these rearrangements should be considered a high-risk criterion, even in the absence of disease progression symptomatology. Other types of coexpression seen were b3a2/ c3a2[p210/p230] in two patients with high risk clinical features and complex karyotypes. Another two patients coexpressing the three transcripts (e19a2/b2a2/c3a2) were considered at high risk, with high WBC and platelet counts and 34% blasts in bone marrow. These patients were given Ara-C for remission induction and interferon for maintenance. They died 6 months and 9 months later, owing to disease activity. These atypical coexpression cases with high-risk clinical features may reect the existence of several leukaemic cell lines with different BCR/ABL transcript expression, rather than alternative splicing. Size differences in BCR/ABL transcripts can reect variations in the sites of breakage/fusion and may also result from alternative splicing between BCR and ABL and within BCR itself. The normal ABL gene is composed of 11 exons, including exons Ia and Ib. These exons can be alternatively spliced and this ability is maintained in the BCR/ABL fusion gene. Indeed, even in CML containing breaks within M-BCR, splicing can occasionally result in a transcript with an e1a2 or e19a2 junction in addition to transcripts with a b2a2 or b3a2 junction. Our study conrms the occurrence of coexpression in different BCR/ABL transcripts, although at a much lower rate (9.6%) than has been reported in other populations. This may reect differences in the sensitivity between the detection techniques used, or possible genetic differences between the populations studied. Co-expression may be
2002 Blackwell Science Ltd., Clin. Lab. Haem., 24, 145150
due to alternative splicing or to phenotypic variation, with clinical courses different from classical CML.
Acknowledgements
This work was supported by the Department of Biotech nology, Group Roche/Sintex, S.A. de C.V. Mexico, Mexico.
References
Burmeister T., Maurer J., Aivado M., Elmaagacli A.H., Grunebach F., Held K.R., HeB G., Hochhaus A., Hoppner W., Lentes K.U., Lubbert M., Schafer K.L., Schafhausen P., Schmidt C.A., Schuler F., Seeger K., Seelig R., Thiede C., Veihmann S., Weber C., Wilhelm S., Christmann A., Clement J.H., Ebener U., Enczmann J., Leo R., Schleuning M., Schoch R. & Thiel E. (2000) Quality assurance in RT-PCR-based BCR/ABL diagnostics results of an interlaboratory test and a standardization approach. Leukemia 14, 18501856. Chomczynski P. & Sachi N. (1987) Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-choroform extraction. Analytical Biochemistry 162, 156159. Cortes J., Kantarjian H., Giralt S. & Talpaz M. (1997) Natural history staging of chronic myelogenous leukemia. Baillieres Clinical Haematology 10 (2), 277290. Cross N. (1996) Detection of BCR-ABL in hematological malignancies by RT-PCR. In: Methods in Molecular Medicine: Molecular Diagnosis of Cancer (ed. F.E. Cotter), pp 2535. Humara Press Inc., USA. Cross N., Lin F. & Goldman J.M. (1994) An optimized multiplex polymerase chain reaction for detection of BCR/ABL fusion mRNAs in hematological disorders. Leukemia 8, 186 189. van Dongen J.J.M., Macintyre E.A., Gabert J.A., Saglio G., Gottardi E., Rambaldi A., Dotti G., Griesinger F., Parreira A., Ga meiro P., Gonzalez Diaz M., Malec M., Langerak A.W., San Miguel J.F. & Biondi A. (1999) Standardized RT-PCR analisis of fusion gene transcripts from chromosome aberrations in acute leukemia for detection of minimal residual disease. Report of the BIOMED-1 concerted action: investigation of minimal residual disease in acute leukemia. Leukemia 13, 19011928. Emilia G., Luppi M., Marasca R. & Torelli G. (1997) Relationship between BCR/ABL fusion proteins and leukemia phenotype. Blood 89, 3889 (letter). Giovanni E., Luppi M., Marasca R. & Torelli G. (1997) Relationship between BCR/ABL fusion proteins and leukemia phenotype. Blood 89, 3889 (letter). Hasford J., Markus P., Hehlmann R., Allan C.N., Baccarani M., Kluin-Nelemans C.J., Alimena G., Steegmann J.L. & Ansari H. (1998) A new prognostic score for survival of patients with chronic myeloid leukemia treated with interferon alfa. Journal of the National Cancer Institute 90, 850858. Haskovec C., Ponzetto C., Polak J., Maritano D., Serra A., Klamova H., Cermak J. & Saglio G. (1998) P230 BCR/ABL protein may be associated with an acute leukemia phenotype. British Journal of Haematology 103, 11041108. ISCN (1995) An International System for Human Cytogenetic Nomenclature (ed. F. Mitelman). Karger, Basel.
150
BCR/ABL in CML Mexican patients
Junis J.J., Sawyer J.R. & Ball D.W. (1978) The characterization of high resolution G banded chromosomes of man. Chromosoma 67, 293307. Kidd V. & Lion T. (1997) Debate round table: appropriate controls for RT-PCR. Leukemia 11, 871881. Kurzrock R., Gutterman J.U. & Talpaz M. (1988) The molecular genetics of Philadelphia chromosome-positive leukemias. New England Journal of Medicine 319, 990998. Lemes A., Gomez T., de la Iglesia S., Matutes E. & Molero T. (1999) P190 BCR/ABL rearrangement in chronic myeloid leukemia and acute lymphoblastic leukemia. Cancer Genetics Cytogenetics 113, 100102. Li S., Ilaria R., Million R., Daley G. & Van-Etten R. (1999) The p190, 210 and p230 forms of the BCR/ABL oncogene induce a similar chronic myeloid leukemialike syndrome in mice but different lymphoid leukemogenic activity. Journal of Experimental Medicine 189, 13991412. Lichty B., Keating A., Callum J., Yee K., Croxford R., Corpus G., Nwachukwu B., Kim P., Guo J. & Kamel-Reid S. (1998) Expression of p210 and p190 BCR-ABL due to alternative splicing in chronic myelogenous leukemia. British Journal of Haematology 103, 711715. Melo J. (1996) The diversity of BCR/ABL fusion proteins and their relationship to leukemia phenotype. Blood 88, 23752384.
Mittre H., Leymaire P., Macro M. & Leporrier M. (1997) A new case of chronic myeloid leukemia with c3/a2 BCR/ABL junction. Is it really a distinct disease? Blood 89, 42394241 (letter). Okamoto K., Karasawa M., Sakai H., Ogura H., Morita K. & Naruse T. (1997) A novel acute lymphoid leukemia type BCR/ ABL transcript in chronic myelogenous leukemia. British Journal of Haematology 96, 611613. Pane F., Frigeri F., Sindona M., Luciano L., Ferrara F., Cimino R., Meloni G., Saglio G., Salvatore F. & Rotoli B. (1996) Neutrophilic chronic myeloid leukemia: a distinct disease with a specic molecular marker (BCR/ABL with C3/A2 junction). Blood 88, 24102414. Parziale M., Tiribelli D., DeMicheli E., Gottardi A., Serra P., Scaravaglio G., Volpe E., Giugliano D., Cilloni G., Rege Cambrin A. & Saglio G. (2000) BCR/ABL hybrid transcripts and leukemia phenotype. In: Chronic Myeloid Leukemia (eds. A.M. Carella & J.M. Goldman, European School of Hematology [ESH]). Hopital Saint-Louis, Paris, France. Rooney D.E. & Czepulkowski B.H. (1992) Human Cytogenetics. Volume II. Malignancy and Aquired Abnormalities. A Practical Approach, pp. 293. IRL Press Oxford, USA. Sokal J.E., Cox E.B., Baccarani M., Tura S., Gomez G.A. & Robertson J.E. (1984) Prognostic discrimination in good-risk chronic granulocytic leukemia. Blood 63, 789799.
2002 Blackwell Science Ltd., Clin. Lab. Haem., 24, 145150
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Mrcog Part1Dokument7 SeitenMrcog Part1Yogeshwari Pardeshi100% (3)
- Reproductive Ecology of The Peruvian Earless Toad Rhinella Yunga (Amphibia, Bufonidae) With Descriptions of Calls, Tadpole, and Female CompetitionDokument12 SeitenReproductive Ecology of The Peruvian Earless Toad Rhinella Yunga (Amphibia, Bufonidae) With Descriptions of Calls, Tadpole, and Female CompetitionOlly Quinteros MuñozNoch keine Bewertungen
- Section G: Vocabulary Cloze: Read The Passage Carefully, and Fill in The Blanks With The Words Provided in The BoxDokument1 SeiteSection G: Vocabulary Cloze: Read The Passage Carefully, and Fill in The Blanks With The Words Provided in The BoxNitya Nurul FadilahNoch keine Bewertungen
- Quiz On Prokaryotic DiversityDokument1 SeiteQuiz On Prokaryotic DiversityIbarra, Rachel B.Noch keine Bewertungen
- W. James Kent - BLAT-The BLAST-Like Alignment ToolDokument10 SeitenW. James Kent - BLAT-The BLAST-Like Alignment ToolYopghm698Noch keine Bewertungen
- B.sc. MicrobiologyDokument56 SeitenB.sc. MicrobiologysruthyaNoch keine Bewertungen
- How To Concieve A BoyDokument32 SeitenHow To Concieve A Boyrelativelabs2075Noch keine Bewertungen
- Avian Metapneumovirus ClassificationDokument7 SeitenAvian Metapneumovirus ClassificationRezaNoch keine Bewertungen
- Biophysics Assignment2 2k19ep042 Hrithik KalkalDokument4 SeitenBiophysics Assignment2 2k19ep042 Hrithik KalkalHarsh Raj EP-037Noch keine Bewertungen
- ChlorophytaDokument13 SeitenChlorophytamandow85Noch keine Bewertungen
- Resources 11 00015 v2Dokument20 SeitenResources 11 00015 v2Gina M LópezNoch keine Bewertungen
- Illustrated Laboratory Activity 6 Test For Nucleic AcidsDokument2 SeitenIllustrated Laboratory Activity 6 Test For Nucleic AcidsAlthea Aubrey AgbayaniNoch keine Bewertungen
- Regulation of Endocrine System PhysiologyDokument169 SeitenRegulation of Endocrine System PhysiologyCriss CristinaNoch keine Bewertungen
- Basics of CentrifugationDokument10 SeitenBasics of Centrifugationramar.r.k9256Noch keine Bewertungen
- Bio 345 Evolution ASU Module 4 Cooperation - Sociality - PVLDokument23 SeitenBio 345 Evolution ASU Module 4 Cooperation - Sociality - PVLTiffanieNoch keine Bewertungen
- Antimicrobial Activity of Honey and PropolisDokument36 SeitenAntimicrobial Activity of Honey and PropolisEuler Mendoza100% (1)
- Differences Between Benign and Malignant TumorsDokument4 SeitenDifferences Between Benign and Malignant TumorsMitreswaran SelvakumaranNoch keine Bewertungen
- c3 Molecular Genetics Unit PlanDokument20 Seitenc3 Molecular Genetics Unit Planapi-477617112Noch keine Bewertungen
- Cell Structure and Function PDFDokument15 SeitenCell Structure and Function PDFAbdul RahmanNoch keine Bewertungen
- Pharmacology IDokument82 SeitenPharmacology IMelanieNoch keine Bewertungen
- Status of Biological Diversity in Malaysia and Threat Assessment of Plant Species in MalaysiaDokument298 SeitenStatus of Biological Diversity in Malaysia and Threat Assessment of Plant Species in MalaysiaCR MamRe Garingging100% (1)
- Bio P2 PDFDokument264 SeitenBio P2 PDFMaaz AdeelNoch keine Bewertungen
- G9 Science Q1 Week 3 4 Non Mendelian Patterns of InheritanDokument26 SeitenG9 Science Q1 Week 3 4 Non Mendelian Patterns of InheritanSandra Lee LigsaNoch keine Bewertungen
- Syllabus 1-2Dokument32 SeitenSyllabus 1-2hopeworld893Noch keine Bewertungen
- 2020 School of Medicine Textbooks MED1100, MED1200, MED2100, MED2200 Prescribed Author, Title, Edition PrescribedDokument4 Seiten2020 School of Medicine Textbooks MED1100, MED1200, MED2100, MED2200 Prescribed Author, Title, Edition PrescribedRobertNoch keine Bewertungen
- Click Here for Taxonomy Questions and AnswersDokument3 SeitenClick Here for Taxonomy Questions and AnswersSylvester Asare100% (1)
- 1-Cell Organelles WS 2016 KEYDokument2 Seiten1-Cell Organelles WS 2016 KEYElvin Hoyo-a Logroño100% (2)
- Microorganisms As BiofertilizerDokument16 SeitenMicroorganisms As Biofertilizersivaram888Noch keine Bewertungen
- COVID 19 Vaccine or Death VaccineDokument10 SeitenCOVID 19 Vaccine or Death VaccinejanzafarNoch keine Bewertungen
- Activity No. 3: Structure of A Cell and MitosisDokument9 SeitenActivity No. 3: Structure of A Cell and MitosisEricka GenoveNoch keine Bewertungen