Beruflich Dokumente
Kultur Dokumente
Bio 5 Notes
Hochgeladen von
kaylaisbellOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Bio 5 Notes
Hochgeladen von
kaylaisbellCopyright:
Verfügbare Formate
BIO 5: The Endocrine System 5.
1 HORMONE CHEMISTRY General hormones are the hormones released by the endocrine system. Exocrine glands release enzymes to the external environment through ducts. Endocrine glands release hormones directly into body fluids. The effects of the endocrine system tend to be slower, less direct, and longer lasting than those of the nervous system. All hormones act by binding to proteins called receptors. In general, the effects of the endocrine system are to alter metabolic activities, regulate growth and development and guide reproduction. Many endocrine glands are stimulated by neurons to secrete their hormones. Hormones exist in 3 basic chemistry types: 1. peptide hormones a. Derived from peptides b. May be large or small, and often include carbohydrate portions c. Manufactured in the rough ER d. Water soluble, and thus move freely through the blood, but have difficulty diffusing through the cell membrane of the effector (the target cell of the membrane) i. Attach to a membrane-bound receptor 1. May activate an intracellular second messenger e. Peptide hormones that you must know for the MCAT i. The anterior pituitary hormones: 1. FSH 2. LH 3. ACTH 4. hGH 5. TSH 6. Prolactin ii. The posterior pituitary hormones: 1. ADH 2. Oxytocin iii. The parathyroid hormone: PTH iv. The pancreatic hormones: 1. Glucagon 2. Insulin 2. steroid hormones a. Come only from the adrenal cortex, the gonads, or the placenta
b. Lipids: require a protein transport molecule in order to dissolve into the blood stream; they diffuse through the membrane c. Important steroid hormones for the MCAT i. The glucocorticoids and the corticoids of the adrenal cortex: 1. Cortisol 2. Aldosterone ii. The gonadal hormones: 1. Estrogen (also produced by the placenta) 2. Progesterone (also produced by the placenta) 3. Testosterone 3. tyrosine derivatives a. Thyroid hormones i. Diffuse through the membrane ii. Lipid Soluble, so they must be carried in the blood by plasma protein carriers. b. catecholamines (the adrenal medulla hormones) i. Bind to receptors on cell membrane and act through a second messenger c. Important tyrosine derivatives for the MCAT: i. The thyroid hormones: 1. T3 (triiodothyronine, contains 3 iodine atoms) 2. T4 (thyroxine, contains 4 iodine atoms) 3. Catecholamines: a. Epinephrine b. Norepinephrine 5.2 NEGATIVE FEEDBACK Endocrine glands tend to over secrete their hormones. Typically, some aspect of their effect on the target tissue will inhibit this secretion. This is an example of negative feedback **The control point of the feedback is the conduct of the effector, not the concentration of hormones.** For instance, high insulin levels do not typically create low blood glucose. Instead, high insulin levels are caused by high blood glucose and low blood glucose would cause high blood glucagon levels. 97. B ---D 98. C 99. B 100. C 101. D 102. B 103. B 104. B
5.3 SPECIFIC HORMONES AND THEIR FUNCTIONS Memorization of several major hormones, their glands, and their target tissues is required for the MCAT. In order to memorize them, you should group hormones according to the gland that secretes them. A given gland produces one of either peptide hormones, steroids, or tyrosine derivatives, but not two. The adrenal glands are really two glands. The cortext produces steroids. The medulla produces catecholamine. The thyroid is true exception. It secretes T3 and T4 which are tyrosine derivatives, and calcitonin which is a peptide. 5.4 ANTERIOR PITUITARY The anterior pituitary is located in the brain beneath the hypothalamus. The hypothalamus controls the release of the anterior pituitary hormones with releasing and inhibitory hormones of its own. The release of the releasing and inhibitory hormones is, in turn, controlled by nervous signals throughout the nervous system. The anterior pituitary releases six major hormones and several minor hormones. All of these are peptide hormones. **For the MCAT you should be familiar with the six major hormones, their target tissues, and their functions.** 1. Human Growth Hormone (hGH) a. Also called somatotropin b. Peptide c. Stimulates growth in almost all cells of the body. d. Stimulates growth by: i. Increasing episodes of mitosis ii. Increasing cell size iii. Increasing the rate of protein synthesis iv. Mobilizing fat stores. v. Increasing the use of fatty acids for energy vi. Decreasing the use of glucose. 2. Adrenocorticotropin (ACTH) a. Peptide b. Stimulates the adrenal cortex to release glucocorticoids via the second messenger system using cAMP.
3.
4. 5. 6.
c. Release of ACTH is stimulated by many types of stress. i. Glucocorticoids are stress hormones. Thyroid Stimulating Hormone (TSH) a. Also called thyrotropin b. Peptide c. Stimulates the thyroid to release T3 and T4 via the second messenger system using cAMP. d. Increases thyroid cell size, number and rate of secretion of T3 and T4 e. NOTE: T3 and T4 concentrations have a negative feedback effect on TSH release both at the anterior pituitary and the hypothalamus. Follicle-Stimulating Hormone (FSH) Luteinizing Hormone (LH) Prolactin a. Peptide b. Promotes lactation by the breasts. c. The reason that milk is not normally produced before birth is due to the inhibitory effects of milk production by progesterone and estrogen. d. Although the hypothalamus has a stimulatory effect on the release of all other anterior pituitary hormones, it mainly inhibits the release of prolactin. e. The act of suckling, which stimulates the hypothalamus to stimulate the anterior pituitary to release Prolactin, inhibits the menstrual cycle. f. The milk production effect of prolactin should be distinguished from the milk ejection effect of oxytocin.
5.5 POSTERIOR PITUITARY The posterior pituitary is also called the neurohypophysis because it is composed mainly of support tissue for nerve endings extending from the hypothalamus. The hormones oxytocin and ADH are synthesized in the neural cell bodies of the hypothalamus and transported down axons into the posterior pituitary where they are released into the blood. 1. Oxytocin a. Small peptide b. Increases uterine contractions during pregnancy c. Causes milk to be ejected from the breasts 2. ADH a. Also called vasopressin b. Small peptide c. Causes collecting ducts of the kidneys to become permeable to water reducing the amount of urine and concentrating the urine. d. Also increases blood pressure. e. Coffee and beer are ADH blockers that increase urine volume. 5.6 ADRENAL CORTEX The adrenal glands are located on top of the kidneys.
Generally, they are separated into the adrenal cortex and the adrenal medulla. The adrenal cortex is the outside portion of the gland. Secretes only steroid hormones. Two types of steroid hormones produced by the adrenal cortex: 1. Mineral corticoids a. Affect the electrolyte balance in the bloodstream 2. Glucocorticoids a. Increase blood glucose concentration b. Have an even greater effect on protein and fat metabolism. 3. Also secretes a small amount of sex hormones (significant in the female, but not the male). Must know the following: 1. Aldosterone a. Steroid i. Mineral corticoid b. Acts in the distal convoluted tubule and the collecting duct to increase Na+ and Clreabsorption and K+ and H+ secretion c. Creates a net gain in particles in the plasma, which results in an eventual increase in blood pressure. d. Has the same effect, but to a lesser extent on the sweat glands, salivary glands, and the intestines. e. FOR THE MCAT, the main effect t of aldosterone is the Na+ absorption and the K+ secretion in the collecting tubule of the kidney i. The increase in blood pressure is a secondary effect. 2. Cortisol a. Steroid i. Glucocorticoid b. Increases blood glucose levels by stimulating gluconeogenesis in the liver. i. Gluconeogenesis is the creation of glucose and glycogen, mainly in the liver, from amino acids, glycerol, and/or lactic acid c. Degrades adipose tissue to fatty acids to be used for cellular energy. d. Causes a moderate decrease in the use of glucose by the cells. e. Causes the degradation of nonhepatic proteins, a decrease of nonhepatic amino acids and a corresponding increase in liver and plasma proteins and amino acids. f. Is a stress hormone i. The benefit of excess cortisol under stressful situations is not fully understood. g. Cortisol also diminishes the capacity of the immune system to fight infection 3. Catecholamines- tyrosine derivatives synthesized in the adrenal medulla a. Epinephrine and Norephinephrine i. Also called adrenaline and noradrenaline
ii. Effects on target tissues are similar to the effects in the parasympathetic nervous system, but they last much longer iii. Vasoconstrictors (constrict blood vessels) of most internal organs and skin, but are vasodilators of skeletal muscle (increase blood flow) iv. Because of their fight or flight response, they are also considered stress hormones. 5.7 THYROID HORMONES The thyroid is located along the trachea just in front of the larynx. Thyroid hormones: 1. T3 and T4 a. Very similar in effect (No distinction will be made on the MCAT, unless it is thoroughly explained in a passage) b. T3 contains 3 iodine atoms, T4 contains 4 iodine atoms c. Both hormones are lipid soluble tyrosine derivatives i. Diffuse through the lipid bilayer ii. Act in the nucleus of the cells of their effector. d. General effect is to increase the basal metabolic rate (the resting metabolic rate) e. Thyroid hormone secretion is regulated by TSH 2. Calcitonin a. Large Peptide hormone released by the thyroid gland b. Slightly decreases blood calcium by decreasing osteoclast activity and number c. Calcium levels can be effectively controlled in humans in the absence of calcitonin 5.8 PANCREAS (ISLETS OF LANGERHANS) The pancreas acts as both an endocrine and exocrine gland. For the MCAT, the two important endocrine hormones released into the blood by the pancreas are: 1. Insulin a. b. c. d.
Peptide Hormone Released by the cells of the pancreas Associated with energy abundance in the form of high energy nutrients in the blood Released in the blood when blood levels of carbohydrates or proteins are high i. Affects carbohydrate, fat and protein metabolism ii. In the presence of insulin, 1. carbohydrates are stored as glycogen in the liver and muscles 2. Fats are stored in the adipose tissue 3. Amino acids are taken up by the cells of the body and made into proteins e. Insulin bind to a membrane receptor and makes the cell highly permeable to glucose and amino acids 2. Glucagon a. Peptide hormone
b. Released by the cells of the pancreas c. Effects are nearly opposite those of insulin d. Stimulates glycogenolysis (the breakdown of glycogen) and gluconeogenesis in the liver e. Acts via the second messenger system of cAMP f. In higher concentrations, glucagon breaks down adipose tissue, increasing the fatty acid levels in the blood. g. Net effect: to raise blood glucose levels 3. Somatostatin (not likely to be on the MCAT) a. Released by the -cells of the pancreas b. Inhibits both insulin and glucagon c. Role may be to extend the period of time over which nutrients are absorbed 5.9 PARATHYROID There are four small parathyroid glands attached to the back of the thyroid. The parathyroid glands release parathyroid hormone 1. Parathyroid Hormone a. Peptide Hormone b. Increases blood calcium i. Increases osteocyte absorption of calcium and phosphate from the bone and stimulates proliferation of osteoclasts c. Increases renal calcium reabsorption and renal phosphate excretion d. Increases calcium and phosphate uptake from the gut e. PTH secretion is regulated by the calcium ion plasma concentration i. The parathyroid glands shrink or grow accordingly 5.10 REPRODUCTION Except for FSH, LH, and HCG, which are peptides, the reproductive hormones discussed are steroids released from the testes, ovaries and placenta. 5.11 THE MALE REPRODUCTIVE SYSYTEM Should know the basic anatomy of the male and female reproductive systems. The male gonads are called the testes. Production of sperm occurs in the seminiferous tubules of the testes. Spermatagonia located in the seminiferous tubules arise from epithelial tisse to become spermatocytes, spermatids, and then spermatozoa. Sertoli cells stimulated by FSH surround and nurture the spermatocyte and spermatids.
Secrete inhibin, a peptide hormone (actually a glycoprotein) which acts on the pituitary gland to inhibit FSH secretion Leydig cells, located in the interstitium between the tubules release testosterone when stimulated by LH. Testosterone 1. The primary androgen (male sex hormone) and stimulates the germ cells to become sperm. 2. Responsible for the development of secondary sex characteristics a. Pubic Hair b. Enlargement of the larynx c. Growth of the penis and seminal vesicles 3. Helps to initiate the growth spurt at puberty 4. Stimulates close of the epiphyses of the long bones, ending growth in stature.
The spermatid has the characteristics of a typical cell. As it becomes a spermatozoon, it loses its cytoplasm and forms the 1. Head a. Composed of the nuclear material and the acrosome.
i. The acrosome contains lysosome-like enzymes for penetrating the egg during fertilization. 2. Midpiece a. Contains many mitochondria to provide energy for movement of the tail. 3. Tail Only the nuclear portion of the sperm enters the egg. Once freed into the tubule lumen, the spermatozoon is carried to the epididymus to mature. Upon ejaculation, spermatozoa are propelled through the vas deferens into the urethra and out of the penis. Semen is the complete mixture of spermatozoa and fluid that leaves the penis upon ejaculation. Semen is composed of fluid from the seminal vesicles, the prostate and the bulbourethral glands (also called Cowpers glands) Spermatozoa become activated for fertilization in a process called capacitation which takes place in the vagina. 5.12 THE FEMALE REPRODUCTIVE SYSTEM Oogenesis begins in the ovaries of the fetus. All of the eggs of the female are arrested as primary oocytes at birth. At puberty, FSH stimulates the growth of granulosa cells around the primary oocyte. The granulosa cells secrete a viscous substance around the egg called the zona pellucida. The structure at this stage is called a primary follicle. Next, theca cells differentiate from the interstitial tissue and grow around the follicle to form a secondary follicle. Upon stimulation by LH, theca cells secrete androgen, which is converted to estradiol (a type of estrogen) by the granulosa cells in the presence of FSH and secreted into the blood. The estradiol is a steroid hormone that prepares the uterine wall for pregnancy. The follicle grows and bulges from the ovary. Typically, estradiol inhibits secretion of LH by the anterior pituitary; however, just before ovulation (the bursting of the follicle), the estradiol level rises rapidly, actually causing a dramatic increase in LH secretion. This increase is called the luteal surge.
The luteal surge results from a positive feedback loop of rising estrogen levels which increase LH levels, which increase estrogen. The luteal surge causes the follicle to burst, releasing the egg (now a secondary oocyte) into the body cavity. The egg is swept into the Fallopian (uterine) tube or oviduct by the fimbriae. The remaining portion of the follicle is left behind to become the corpus luteum. The corpus luteum secretes estradiol and progesterone throughout pregnancy, or in the case of no pregnancy, for about two weeks until the corpus luteum degrades into the corpus albicans. This cycle repeats itself approximately every 28 days after puberty unless pregnancy occurs. This cycle is called the menstrual cycle. With each menstrual cycle, several primordial oocytes may begin the process, but, normally, only one completes the development to ovulation. The cycle is divided into three stages: 1. The follicular phase a. Begins with the development of the follicle and ends at ovulation 2. The luteal phase a. Begins at ovulation and ends with the degeneration of the corpus luteum into the corpus albicans 3. Flow a. Shedding of the uterine lining lasting approximately 5 days
5.13 FERTILIZATION AND EMBRYOLOGY Once in the Fallopian tube, the egg is swept toward the uterus by cilia. Fertilization normally takes place in the Fallopian tubes. The enzymes of the acrosome of a sperm are released upon contact with the egg and digest a path for the sperm through the granulosa cells and the zona pellucida. The cell membranes of the sperm head and the oocyte fuse upon contact and the sperm nucleus enters the cytoplasm of the oocyte. The entry of the sperm causes the cortical reaction, which prevents other sperm from fertilizing the same egg. Now the oocyte goes through the second meiotic division to become an ovum and releases a second polar body. Fertilization occurs when the nuclei of the sperm and the ovum fuse to form the zygote. Cleavage begins when the zygote is still in the Fallopian tube. The zygote goes through many cycles of mitosis. When the zygote is composed of 8 or more cells, it is called a morula.
The embryo at this stage does not grow during cleavage. The first 8 cells formed by cleavage are equivalent in size and shape and are said to be totipotent, meaning that they have the potential to express any of their genes. Any one of these cells at this stage could produce a complete individual. The cells of the morula continue to divide for four days forming a hollow ball filled with fluid. This fluid filled ball is called a blastocyst. It is the blastocyst that lodges in the uterus in a process called implantation on about the 5th to 7th day after ovulation. The blastocyst is made up of embryonic stem cells, which have the ability to develop into most of the types of cells in the human body. Upon implantation, the female is said to be pregnant. Upon implantation, the egg begins secreting a peptide hormone called human chorionic gonadotropic (HCG). HCG prevents the degeneration of the corpus luteum, and maintains it secretion of estrogen and progesterone. HCG in the blood and urine of the mother is the first outward sign of pregnancy. A placenta is formed from the tissue of the egg and the mother and takes over the job of hormone secretion. The placenta reaches full development by the end of the first trimester and begins secreting its own estrogen and progesterone while lowering its secretion of HCG. As the embryo develops past the 8 cells stage, the cells become different from each other due to cell-tocell interactions. The process where a cell becomes committed to a specialized developmental path is called determination. Cells become determined to give rise to a particular tissue early on. The specialization that occurs at the end of the development forming a specialized tissue cell is called differentiation. The fate of a cell is typically determined early on, but that same cell usually doesnt differentiate into a specialized tissue cell until much later at the end of the developmental process.
Recent research has shown that the fate of even a fully differentiated cell can be altered given the proper conditions. The formation of the gastrula occurs in the second week after fertilization in a process called gastrulation. Cells begin to slowly move about the embryo for the first time. In mammals, a primitive streak is formed, which is analogous to the blastopore in aquatic vertebrates. Cells destined to become mesoderm migrate into the primitive streak. During gastrulation, three primary germ layers are formed: 1. The ectoderm a. Develop in to the outer coverings of the body such as the outer layers of skin, nails, and tooth enamel b. Develop into the cells of the nervous system and sense organs 2. The mesoderm a. everything in between (muscle, bones, etc.) 3. The endoderm a. Develops into the lining of the digestive tract and into much of the liver and pancreas In the third week, the gastrula develops into a neurula in a process called neurulation. In neurulation, the notochord (made from the mesoderm) induces the overlying ectoderm to thicken and form the neural plate. The notochord eventually degenerates, while a neural tube forms from the neural plate to become the spinal cord, brain and most of the nervous system. **For the MCAT, you must know that INDUCTION OCCURS WHEN ONE TYPE OF CELL AFFECTS THE DIRECTION OF DIFFERENTIATION OF ANOTHER CELL TYPE** Part of normal cell development is programmed cell death or apoptosis. Apoptosis is essential for development of the nervous system, operation of the immune system, and destruction of tissue between fingers and toes to create normal hands and feet in humans. Damaged cells may undergo apoptosis as well. Failure to do so may result in cancer.
Apoptosis is a complicated process in humans, but it is basically regulated by protein activity as opposed to regulation at the transcription of translation level. The proteins involved in apoptosis are present, but inactive, in a normal healthy cell. In mammals, mitochondria play an important role in apoptosis.
GLAND Anterior Pituitary
HORMONE hGH ACTH FSH LH
TSH Prolactin Oxytocin ADH Adrenal Cortex Aldosterone
Posterior Pituitary
Cortisol Testosterone Adrenal Medulla Epinephrine Norepinephrine T3 and T4 Calcitonin PH Insulin
Thyroid Parathyroid Pancreas
Glucagon Ovaries Estrogen Progesterone Testes Placenta Testosterone HCG
Estrogens Progesterone
EFFECTS Growth of nearly all cells Stimulates adrenal cortex Growth of follicles in female; sperm production in male Causes ovulation; stimulates estrogen and testosterone secretion Stimulates release of T3 and T4 in the thyroid Promotes milk production Milk ejection and uterine contraction Water absorption by the kidney; Increase blood pressure Reduces Na+ excretion; increases K+ excretion; raises blood pressure Increases blood levels of carbohydrates, proteins and fats Secondary sex characteristics; closing of epiphyseal plates Stimulates sympathetic actions Stimulates parasympathetic actions Increases basal metabolic rate Lowers blood calcium Raises blood calcium Promotes entry of glucose into cells, decreasing glucose blood level Increases gluconeogenesis, increasing glucose blood level Growth of mother sex organs; causes LH surge Prepares and maintains uterus for pregnancy Secondary sex characteristics; closing of epiphyseal plates Stimulates corpus luteum to grow and release estrogen and progesterone Growth of mother sex organs; causes LH surge Prepares and maintains uterus for pregnancy
Das könnte Ihnen auch gefallen
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Concepts Regarding Function of The Stomatognathic System: John R. Thompson, D.D.S., M .S.D ., M .S., ChicagoDokument12 SeitenConcepts Regarding Function of The Stomatognathic System: John R. Thompson, D.D.S., M .S.D ., M .S., Chicagoblogger bloggerNoch keine Bewertungen
- Dental Codes-Auth Requirement UCSLS Codes - V1R0Dokument32 SeitenDental Codes-Auth Requirement UCSLS Codes - V1R0American Aesthetic MCNoch keine Bewertungen
- 1-Eruption of TeethDokument9 Seiten1-Eruption of TeethAhmed AbdNoch keine Bewertungen
- Oesophagus Maag DuodenographyDokument49 SeitenOesophagus Maag DuodenographyEvan DionesiaNoch keine Bewertungen
- Hypertension PathophysiologyDokument1 SeiteHypertension PathophysiologyTiffany Blanca Evangelista RaiNoch keine Bewertungen
- Veterinary AcupunctureDokument19 SeitenVeterinary AcupuncturekinezildiNoch keine Bewertungen
- Apraxia PDFDokument13 SeitenApraxia PDFAndré CantanhedeNoch keine Bewertungen
- Pes 2023Dokument1 SeitePes 2023dr_yasserNoch keine Bewertungen
- Anatomy of Major Salivary GlandsDokument46 SeitenAnatomy of Major Salivary Glandswaniya irumNoch keine Bewertungen
- Absen Pembacaan Refarat Dan Lapsus Suci RamadhaniDokument2 SeitenAbsen Pembacaan Refarat Dan Lapsus Suci Ramadhanisuci ramadhaniNoch keine Bewertungen
- Adrenal Medulla HormonesDokument57 SeitenAdrenal Medulla HormonesnikkitingNoch keine Bewertungen
- MODUL 1 FKG UnairDokument61 SeitenMODUL 1 FKG UnairLaurensia NovenNoch keine Bewertungen
- Visual Pathway Anatomy and PhysiologyDokument70 SeitenVisual Pathway Anatomy and Physiologylovelots1234Noch keine Bewertungen
- Koordinasi Badan Panduan GuruDokument3 SeitenKoordinasi Badan Panduan GuruNor Hamizah OmarNoch keine Bewertungen
- Understanding Joints and ArticulationsDokument26 SeitenUnderstanding Joints and Articulationsragnarok meroNoch keine Bewertungen
- Surface Anatomy of The HeartDokument5 SeitenSurface Anatomy of The HeartEglNoch keine Bewertungen
- Anatomy & Physiology of the Digestive SystemDokument7 SeitenAnatomy & Physiology of the Digestive SystemNicole Ken AgdanaNoch keine Bewertungen
- Secretory Functions of GITDokument24 SeitenSecretory Functions of GITDr.Nusrat TariqNoch keine Bewertungen
- 2018 Dental Fee Guide PDFDokument1 Seite2018 Dental Fee Guide PDFLarryNoch keine Bewertungen
- AP Biology Chapter 42 Circulatory and RespirationDokument36 SeitenAP Biology Chapter 42 Circulatory and RespirationSang Hoon KimNoch keine Bewertungen
- Blood Is A Body Fluid in Human and Other Animals That Delivers Necessary Substances Such AsDokument24 SeitenBlood Is A Body Fluid in Human and Other Animals That Delivers Necessary Substances Such AsPaulo DanielNoch keine Bewertungen
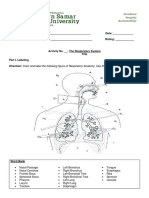
- The Respiratory System ActivityDokument4 SeitenThe Respiratory System ActivityVina DiscarNoch keine Bewertungen
- Endocrine System - outlINEDokument4 SeitenEndocrine System - outlINERalph NilloNoch keine Bewertungen
- Occluion ConceptsDokument15 SeitenOccluion ConceptsImran CassimNoch keine Bewertungen
- Neurofunctional Blueprints Transcripts For Tempe, January 2015 PDFDokument82 SeitenNeurofunctional Blueprints Transcripts For Tempe, January 2015 PDFAnonymous oCjRxyBP100% (3)
- Occlusal Forms and Philosophies in Full Mouth Rehabilitation: A Literature ReviewDokument5 SeitenOcclusal Forms and Philosophies in Full Mouth Rehabilitation: A Literature ReviewSkAliHassanNoch keine Bewertungen
- Seven Plus One Lymph HealingDokument3 SeitenSeven Plus One Lymph HealingAnonymous hndaj8zCA50% (2)
- Practice: Failures in Implant DentistryDokument7 SeitenPractice: Failures in Implant DentistryDrMarkHoganNoch keine Bewertungen
- Classifying Partial EdentulismDokument37 SeitenClassifying Partial EdentulismSangeetha BommineniNoch keine Bewertungen
- New Conservative Approach to Treating Worn TeethDokument32 SeitenNew Conservative Approach to Treating Worn TeethHektor Hak100% (1)