Beruflich Dokumente
Kultur Dokumente
LVH Articulo
Hochgeladen von
Nani BernstorffOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
LVH Articulo
Hochgeladen von
Nani BernstorffCopyright:
Verfügbare Formate
reVieW
CME CREDIT
EDUCATIONAL OBJECTIVE: Readers will consider screening for left ventricular hypertrophy in their hypertensive patients
Michael a. BauMl, MD
Department of Internal Medicine, Cleveland Clinic
DonalD a. unDerwooD, MD
Department of Cardiovascular Medicine, Cleveland Clinic
Left ventricular hypertrophy: An overlooked cardiovascular risk factor
AbstrAct
Left ventricular hypertrophy (LVH) is common in hypertensive patients, and it increases the risk of myocardial infarction, stroke, and death. Recent evidence indicates it is a modifiable risk factor that is not entirely dependent on blood pressure control. The authors review its pathogenesis, diagnosis, and treatment.
ventricular hypertrophy (LVH) Left overall mortality in hypertensive pastrongly predicts cardiovascular morbidity and tients.17 Antihypertensive treatment that causes LVH to regress decreases the rates of adverse cardiovascular events and improves survival, independent of how much the blood pressure is lowered.811 It is clinically important to recognize that LVH is a modifiable risk factor and that management is more complex than just blood pressure control. This paper reviews the definition of LVH, compares the diagnostic tests for it, and discusses the current evidence-based approach to managing this dangerous risk factor. A CHRONICALLY ELEVATED CARDIAC WORKLOAD CAusEs LVH LVH is an abnormal increase in the mass of the left ventricular myocardium caused by a chronically increased workload on the heart.12 This most commonly results from the heart pumping against an elevated afterload, as in hypertension and aortic stenosis. Another notable cause is increased filling of the left ventricle (ie, diastolic overload), which is the underlying mechanism for LVH in patients with aortic or mitral regurgitation and dilated cardiomyopathy. Coronary artery disease can also play a role in the pathogenesis of LVH, as the normal myocardium attempts to compensate for the ischemic or infarcted tissue.13 A key component in the development of LVH is myocardial fibrosis (FIGURE 1), which
VOLUME 77 NUMBER 6 JUNE 2010
Key Points
LVH is caused by a chronically increased cardiac workload, most commonly from hypertension. Ideally, all hypertensive patients should undergo echocardiography to screen for LVH, using the calculated left ventricular mass index. Electrocardiography is too insensitive to be used alone to screen for LVH. In hypertensive patients, initial therapy of LVH should consist of an angiotensin II receptor blocker or an angiotensin-converting enzyme inhibitor. Treatment-induced regression of LVH improves cardiovascular outcomes independent of blood pressure. Further study is necessary to examine the utility of following the left ventricular mass index as a treatment goal.
doi:10.3949/ccjm.77a.09158
CLEVEL A N D C L I N I C J O U R N A L O F M E D I C I N E
381
Left VentricuLAr HyPertroPHy
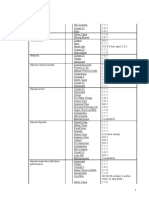
TABLE 1
common electrocardiographic criteria for the diagnosis of left ventricular hypertrophy (LVH)
Cornell voltage criteria SV3 + RaVL 2.0 mV (28 mm) in men SV3 + RaVL 2.8 mV (20 mm) in women (some variations use a lower cutoff value in men) Cornell product criteria SV3 + RaVL (+8 in women a) x QRS duration 2,440 mm ms sokolow-Lyon voltage criteria SV1 + RV5 or RV6 3.5 mV (35 mm) b or RaVL 1.1 mV (11 mm) Romhilt-Estes point score system (a score 5 is diagnostic of LVH, a score of 4 is probable LVH) Voltage criteria (3 points): Any S or R in limb leads 20 mm SV1, SV2, RV5, or RV6 30 mm ST-T wave changes of LVH (3 points, 1 point on digitalis) Left atrial abnormality (3 points): Terminal component of the P wave in V1 1 mm and 40 ms Left axis deviation (2 points): QRS axis of 30 degrees or more negative Prolonged QRS duration (1 point): 90 ms Delayed intrinsicoid deflection time (1 point): 50 ms in V5 or V6
A modification of +6 instead of +8 in women may be more accurate and was used in the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) study10 b A cutoff value of 38 mm has also been used, eg, in the LIFE study
a
for treating LVH, as we will discuss later in this review. Genetics also play an important role in the pathogenesis of LVH. Mutations in genes encoding sarcomeric proteins have a direct causal relationship in patients with hypertrophic cardiomyopathy.16 In addition, there appears to be a genetic predisposition that causes some patients with mild hypertension to develop LVH while others do not.17,18 DIAGNOsIs BY ELECTROCARDIOGRAPHY, ECHOCARDIOGRAPHY, OR mRI LVH can be detected by electrocardiography (FIGURE 2), echocardiography (FIGURE 3), or cardiac magnetic resonance imaging (MRI) (FIGURE 4). Each has unique advantages and disadvantages. Electrocardiography is specific, but not sensitive Electrocardiography is the cheapest and most readily available of the three tests for LVH. While its specificity is acceptably high, its clinical utility is limited by its very low sensitivity.19,20 Many different criteria for electrocardiographic LVH have been proposed over the years. Most use the voltage in one or more leads, with or without additional factors such as QRS duration, secondary ST-T wave abnormalities, or left atrial abnormalities. The most well known electrocardiographic criteria are the Cornell voltage,21 the Cornell product,22 the Sokolow-Lyon index,23 and the Romhilt-Estes point score system (tablE 1).24 A systematic review of 21 studies,19 published in 2007, found that all the criteria were less sensitive than specific: Cornell voltagemedian sensitivity 15%, median specificity 96% Cornell productmedian sensitivity 19.5%, median specificity 91% Sokolow-Lyon voltagemedian sensitivity 21%, median specificity 89% Romhilt-Estes point scoremedian sensitivity 17%, median specificity 95%. Of note, the ranges of the published values were extremely broad. For example, the ranges in sensitivity were:
compromises cardiac function.14 The fibrosis is initially manifested by diastolic dysfunction, although systolic dysfunction also occurs with progressive disease. The development of myocardial fibrosis appears to be pathophysiologically linked to the renin-angiotensin-aldosterone system. Specifically, there is evidence that angiotensin II has a profibrotic effect on the myocardium of hypertensive patients.15 This may explain why angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are among the most potent agents
382
CLEVELAND CLINIC JOURNAL OF MEDICINE
VOLUME 77 N U M B E R 6
JUNE 2010
bAumL And underWood
M left ventricular hypertrophy and fibrosis
Left ventricular hypertrophy (LVH) is a response to a chronically increased workload on the heart. A key component is myocardial fibrosis, which has been linked to the renin-angiotensin-aldosterone system. This observation may explain why angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers are among the most potent agents for treating LVH.
Normal
Left ventricular hypertrophy
CCF
2010
myocardial fibrosis
Medical illustrator Ross Papalardo; histology images courtesy of E. Rene Rodriguez, MD, and Carmela Tan, MD, Department of Anatomic Pathology, Cleveland Clinic
FIGURE 1
Cornell voltage2% to 41% Cornell product8% to 32% Sokolow-Lyon voltage4% to 51% Romhilt-Estes point score0% to 41%. While the studies with the extreme values may have had issues of small sample size or poor study quality, the wide range in values may primarily be the result of diverse study populations as well as different validation
methods and cutoff values to define LVH. Regardless, the overall message of high specificity and low sensitivity is indisputable. Electrocardiography is insensitive for diagnosing LVH because it relies on measuring the electrical activity of the heart by electrodes on the surface of the skin to predict the left ventricular mass. The intracardiac electrical activity is problematic to measure exterVOLUME 77 NUMBER 6 JUNE 2010
CLEVEL A N D C L I N I C J O U R N A L O F M E D I C I N E
383
Left VentricuLAr HyPertroPHy
the left ventricular mass index should be used to diagnose LVH in most patients
FIGURE 2. This electrocardiogram from a 62-year-old woman shows left ventricular hypertrophy by the Cornell voltage criteria, the Cornell product criteria, the Sokolow-Lyon voltage criteria, and the Romhilt-Estes point score system.
nally because the measurements are affected by everything between the myocardium and the electrodes, most notably fat, fluid, and air. Because of this effect, electrocardiography underdiagnoses LVH in patients with obesity, pleural effusions, pericardial effusions, anasarca, or chronic obstructive pulmonary disease. In addition, the diagnosis of LVH by electrocardiography is strongly influenced by age and ethnicity.2526 While electrocardiography is not sensitive and cannot be used to rule out LVH, it still has a role in its diagnosis and management. In the landmark Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) study, regression of LVH (diagnosed electrocardiographically by the Sokolow-Lyon index or the Cornell product criteria) in response to losartan (Cozaar) improved cardiovascular outcomes independent of blood pressure.10 Based on this, it is reasonable that all hypertensive patients and other patients at risk of LVH who
VOLUME 77 N U M B E R 6
undergo electrocardiography be screened with these two criteria. Echocardiography is the test of choice Echocardiography, if available, should be the test of choice to assess for LVH. It is much more sensitive than electrocardiography and can also detect other abnormalities such as left ventricular dysfunction and valvular disease. This test uses transthoracic or transesophageal ultrasonography to measure the left ventricular end-diastolic diameter, posterior wall thickness, and interventricular septum thickness. From these measurements and the patients height and weight, the left ventricular mass index can be calculated.27 Several different cutoff values for the left ventricular mass index have been proposed; the LIFE study used values of > 104 g/m2 in women and > 116 g/m2 in men to define LVH.
384
CLEVELAND CLINIC JOURNAL OF MEDICINE
JUNE 2010
bAumL And underWood
When using echocardiography to assess for LVH, it is imperative that the left ventricular mass index be used and not just the left ventricular wall thickness, as often happens in clinical practice. This is necessary because diagnosis by wall thickness alone is not a good indicator of LVH, with a concordance between wall thickness and a left ventricular mass index of only 60%.28 In addition, wall thickness tends to underestimate LVH in women and overestimate it in men. Is echocardiography cost-effective? Despite its clear advantages, an important consideration about echocardiography as a screening test for all hypertensive patients is its cost. A suggested way to reduce cost is to measure the left ventricular mass index only.29 A limited echocardiographic examination is much less expensive than a complete twodimensional echocardiogram ($255 vs $431 per the 2009 Medicare Ambulatory Payment Classification30) and should be the examination performed if the patient has no other clinical indication for echocardiography. Another way to control cost is to stratify patients by risk and to do echocardiography only in those who would benefit most from it. Based on the prevalence of LVH, one study concluded that echocardiography is most costeffective in men 50 years or older.31 Further study is necessary to more precisely define the cost-effectiveness of echocardiographic screening for LVH in terms of potentially preventable cardiovascular morbidity and death. Cardiac mRI: The costly gold standard Cardiac MRI is the gold standard test for LVH, as it is even more accurate and reproducible than echocardiography.32 It can precisely estimate a patient's left ventricular mass and assess for other structural cardiac abnormalities. MRIs use, however, is severely restricted in clinical practice due to its high cost and limited availability. While it may never be used for general screening for LVH, it certainly has a role in clinical research and for assessing cardiac anatomy in special clinical situations.
IVSd
lVIDd PWtd
FIGURE 3. An echocardiogram performed in a 68-year-old man being evaluated for uncontrolled hypertension and symptoms of congestive heart failure. Left ventricular hypertrophy is diagnosed by an elevated left ventricular mass index, which is calculated from the intraventricular septal thickness (IVSd), posterior wall thickness (PWTd), and left ventricular end-diastolic internal diameter (LVIDd).
TREATmENT sHOuLD INCLuDE AN ACE INHIBITOR OR ARB Once LVH has been diagnosed, the next step is to decide on an appropriate treatment plan. While the choice of therapy will always depend on other comorbidities, a 2003 metaanalysis of antihypertensive medications in the treatment of LVH (controlling for the degree of blood pressure lowering) showed that ARBs were the most efficacious class of agents for reducing the left ventricular mass.33 Specifically, ARBs decreased the mass by 13%, followed by calcium-channel blockers at 11%, ACE inhibitors at 10%, diuretics at 8%, and beta-blockers at 6%. In pairwise comparison, ARBs, calciumchannel blockers, and ACE inhibitors were all significantly more effective in reducing the left ventricular mass than beta-blockers. As previously discussed, LVH appears to be pathophysiologically linked to myocardial fibrosis and the renin-angiotensin-aldosterone system. For this reason and based on the data
VOLUME 77 NUMBER 6 JUNE 2010
CLEVEL A N D C L I N I C J O U R N A L O F M E D I C I N E
385
Left VentricuLAr HyPertroPHy
FIGURE 4. This magnetic resonance image, which also demonstrates concentric left ventricular hypertrophy, was performed in the same 68-year-old man due to suspicion of an infiltrative myocardial disorder.
also been shown to decrease the incidence of diabetes mellitus,34 atrial fibrillation,35 and hospitalizations for heart failure.36 The LIFE study also examined the prognostic implications of treating LVH detected by echocardiography. In this prospective cohort substudy, patients who had a lower left ventricular mass index during treatment with antihypertensive drugs had lower rates of cardiovascular morbidity and all-cause mortality, independent of the effects of blood pressure and treatment used.11 These results suggest that there may be a role not only for treating LVH, but also for monitoring for a reduction in the left ventricular mass index as a goal of therapy (similar to the way hemoglobin A1c is used in diabetic patients). If the index is used in this way, one could potentially adjust the dose of current drugs, switch classes, or add an additional drug based on a persistently elevated left ventricular mass index in order to optimize the patient's overall cardiovascular risk. A randomized controlled trial of therapy directed by the mass index vs conventional therapy of LVH would be necessary to assess the clinical utility of this approach. RECOmmENDATIONs LVH is a common and potentially modifiable cardiovascular risk factor often overlooked in clinical practice. Ideally, all hypertensive patients should be screened with echocardiography to look for LVH, using the calculated left ventricular mass index rather than wall thickness alone to make the diagnosis. While electrocardiography is specific and also has prognostic implications, it is not sensitive enough to be used alone to screen for LVH. Once the diagnosis of LVH is made, the initial therapy should be an ARB or an ACE inhibitor. Response to therapy can be assessed by monitoring for a reduction in left ventricular mass index or regression of electrocardiographic LVH. Treatment-induced regression of LVH decreases adverse cardiovascular events and improves overall survival. When modifying medications in hypertensive patients, it is important to remember that the treatment of LVH is not synonymous with blood pressure control.
presented above regarding the degree of LVH regression, ACE inhibitors or ARBs should be used as the first-line agents for LVH unless they are contraindicated in the individual patient. The LIFE study The LIFE study offers the strongest evidence that treating LVH is beneficial. It showed that in hypertensive patients with electrocardiographic LVH by the Cornell product or Sokolow-Lyon criteria, treatment with antihypertensive drugs that resulted in less-severe LVH on electrocardiography was associated with lower rates of cardiovascular morbidity and death, independent of the blood pressure achieved or the drug used.10 The end point in this study was a composite of stroke, myocardial infarction, and cardiovascular death. Regression of electrocardiographic LVH in hypertensive patients has
386
CLEVELAND CLINIC JOURNAL OF MEDICINE
VOLUME 77 N U M B E R 6
JUNE 2010
bAumL And underWood
REFERENCEs
1. Casale PN, Devereux Rb, Milner M, et al. Value of echocardiographic measurement of left ventricular mass in predicting cardiovascular morbid events in hypertensive men. Ann Intern Med 1986; 105:173178. 2. levy D, Garrison RJ, Savage DD, Kannel Wb, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 1990; 322:15611566. 3. Koren MJ, Devereux Rb, Casale PN, Savage DD, laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med 1991; 114:345352. 4. Verdecchia P, Carini G, Circo a, et al; MaVI (Massa Ventricolare sinistra nellIpertensione) Study Group. Left ventricular mass and cardiovascular morbidity in essential hypertension: the MAVI study. J Am Coll Cardiol 2001; 38:18291835. 5. Haider aW, larson MG, benjamin EJ, levy D. Increased left ventricular mass and hypertrophy are associated with increased risk for sudden death. J Am Coll Cardiol 1998; 32:14541459. 6. Verdecchia P, Porcellati C, Reboldi G, et al. Left ventricular hypertrophy as an independent predictor of acute cerebrovascular events in essential hypertension. Circulation 2001; 104:2039 2044. 7. Schillaci G, Verdecchia P, Porcellati C, Cuccurullo O, Cosco C, Perticone F. Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension 2000; 35:580586. 8. Verdecchia P, Schillaci G, borgioni C, et al. Prognostic significance of serial changes in left ventricular mass in essential hypertension. Circulation 1998; 97:4854. 9. Mathew J, Sleight P, lonn E, et al; Heart Outcomes Prevention Evaluation (HOPE) Investigators. Reduction of cardiovascular risk by regression of electrocardiographic markers of left ventricular hypertrophy by the angiotensin-converting enzyme inhibitor ramipril. Circulation 2001; 104:16151621. 10. Okin PM, Devereux Rb, Jern S, et al; lIFE Study Investigators. Regression of electrocardiographic left ventricular hypertrophy during antihypertensive treatment and the prediction of major cardiovascular events. JAMA 2004; 292:23432349. 11. Devereux Rb, Wachtell K, Gerdts E, et al. Prognostic significance of left ventricular mass change during treatment of hypertension. JAMA 2004; 292:23502356. 12. lorell bH, Carabello ba. Left ventricular hypertrophy: pathogenesis, detection, and prognosis. Circulation 2000; 102:470479. 13. Zabalgoitia M, berning J, Koren MJ, et al; lIFE Study Investigators. Impact of coronary artery disease on left ventricular systolic function and geometry in hypertensive patients with left ventricular hypertrophy (the LIFE study). Am J Cardiol 2001; 88:646650. 14. Weber Kt, Janicki JS, Pick R, Capasso J, anversa P. Myocardial fibrosis and pathologic hypertrophy in the rat with renovascular hypertension. Am J Cardiol 1990; 65:1G7G. 15. Gonzlez a, lpez b, Querejeta R, Dez J. Regulation of myocardial fibrillar collagen by angiotensin II. A role in hypertensive heart disease? J Mol Cell Cardiol 2002; 34:15851593. 16. Maron bJ. Hypertrophic cardiomyopathy: a systematic review. JAMA 2002; 287:13081320. 17. liebson PR, Grandits G, Prineas R, et al. Echocardiographic correlates of left ventricular structure among 844 mildly hypertensive men and women in the Treatment of Mild Hypertension Study (TOMHS). Circulation 1993; 87:476486. 18. Martinez Ma, Sancho t, armada E, et al; Vascular Risk Working Group Grupo Monitorizacon ambulatoria de la Presin arterial (MaPa)-Madrid. Prevalence of left ventricular hypertrophy in patients with mild hypertension in primary care: impact of echocardiography on cardiovascular risk stratification. Am J Hypertens 2003; 16:556563. 19. Pewsner D, Jni P, Egger M, battaglia M, Sundstrm J, bachmann 20. 21.
22.
23.
24. 25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
lM. Accuracy of electrocardiography in diagnosis of left ventricular hypertrophy in arterial hypertension: systematic review. BMJ 2007; 335:711. Devereux Rb. Is the electrocardiogram still useful for detection of left ventricular hypertrophy? Circulation 1990; 81:11441146. Casale PN, Devereux Rb, Kligfield P, et al. Electrocardiographic detection of left ventricular hypertrophy: development and prospective validation of improved criteria. J Am Coll Cardiol 1985; 6:572580. Molloy tJ, Okin PM, Devereux Rb, Kligfield P. Electrocardiographic detection of left ventricular hypertrophy by the simple QRS voltage-duration product. J Am Coll Cardiol 1992; 20:11801186. Sokolow M, lyon tP. The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J 1949; 37:161186. Romhilt DW, Estes EH Jr. A point-score system for the ECG diagnosis of left ventricular hypertrophy. Am Heart J 1968; 75:752758. levy D, labib Sb, anderson KM, Christiansen JC, Kannel Wb, Castelli WP. Determinants of sensitivity and specificity of electrocardiographic criteria for left ventricular hypertrophy. Circulation 1990; 81:815820. Okin PM, Wright Jt, Nieminen MS, et al. Ethnic differences in electrocardiographic criteria for left ventricular hypertrophy: the LIFE study. Losartan Intervention For Endpoint. Am J Hypertens 2002; 15:663671. Devereux Rb, alonso DR, lutas EM, et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986; 57:450458. leibowitz D, Planer D, ben-Ibgi F, Rott D, Weiss at, bursztyn M. Measurement of wall thickness alone does not accurately assess the presence of left ventricular hypertrophy. Clin Exp Hypertens 2007; 29:119125. black HR, Weltin G, Jaffe CC. The limited echocardiogram: a modification of standard echocardiography for use in the routine evaluation of patients with systemic hypertension. Am J Cardiol 1991; 67:10271030. american Society of Echocardiography Coding and Reimbursement Newsletter, January 2009. http://www.asecho.org/files/public /CodingnewsJan09.pdf. Accessed May 13, 2010. Cuspidi C, Meani S, Valerio C, Fusi V, Sala C, Zanchetti a. Left ventricular hypertrophy and cardiovascular risk stratification: impact and cost-effectiveness of echocardiography in recently diagnosed essential hypertensives. J Hypertens 2006; 24:16711677. bottini Pb, Carr aa, Prisant lM, Flickinger FW, allison JD, Gottdiener JS. Magnetic resonance imaging compared to echocardiography to assess left ventricular mass in the hypertensive patient. Am J Hypertens 1995; 8:221228. Klingbeil aU, Schneider M, Martus P, Messerli FH, Schmieder RE. A meta-analysis of the effects of treatment on left ventricular mass in essential hypertension. Am J Med 2003; 115:4146. Okin PM, Devereux Rb, Harris KE, et al; lIFE Study Investigators. In-treatment resolution or absence of electrocardiographic left ventricular hypertrophy is associated with decreased incidence of new-onset diabetes mellitus in hypertensive patients: the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) Study. Hypertension 2007; 50:984990. Okin PM, Wachtell K, Devereux Rb, et al. Regression of electrocardiographic left ventricular hypertrophy and decreased incidence of new-onset atrial fibrillation in patients with hypertension. JAMA 2006; 296:12421248. Okin PM, Devereux Rb, Harris KE, et al; lIFE Study Investigators. Regression of electrocardiographic left ventricular hypertrophy is associated with less hospitalization for heart failure in hypertensive patients. Ann Intern Med 2007; 147:311319.
ADDRESS: Michael A. Bauml, MD, Department of Internal Medicine, NA10, Cleveland Clinic, 9500 Euclid Avenue, Cleveland, OH, 44195; email: baumlm@ccf.org.
VOLUME 77 NUMBER 6 JUNE 2010
CLEVEL A N D C L I N I C J O U R N A L O F M E D I C I N E
387
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Varaah KavachDokument7 SeitenVaraah KavachBalagei Nagarajan100% (1)
- Calculation of The Current Transformer Accuracy Limit FactorDokument14 SeitenCalculation of The Current Transformer Accuracy Limit FactorWeiKiat Goh67% (3)
- 2018 Statin in The Treatment of Patients With Myocardial InfarctionDokument4 Seiten2018 Statin in The Treatment of Patients With Myocardial InfarctionNani BernstorffNoch keine Bewertungen
- 2020 Precision Anticoagulation MedicineDokument314 Seiten2020 Precision Anticoagulation MedicineNani Bernstorff100% (1)
- 2019 Anticoagulant Reversal Strategies in The Emergency Department SettingDokument16 Seiten2019 Anticoagulant Reversal Strategies in The Emergency Department SettingNani BernstorffNoch keine Bewertungen
- Statin HipertensiDokument12 SeitenStatin HipertensiAlifianiii KartikaNoch keine Bewertungen
- 2019 Anticoagulant Reversal Strategies in The Emergency Department SettingDokument16 Seiten2019 Anticoagulant Reversal Strategies in The Emergency Department SettingNani BernstorffNoch keine Bewertungen
- 2018 Anticoagulation in Acute Coronary Syndrome-State of The ArtDokument25 Seiten2018 Anticoagulation in Acute Coronary Syndrome-State of The ArtNani BernstorffNoch keine Bewertungen
- 2017 High-Dose Atorvastatin Versus Moderate Dose On Early Vascular Protection After ST-elevation Myocardial InfarctionDokument10 Seiten2017 High-Dose Atorvastatin Versus Moderate Dose On Early Vascular Protection After ST-elevation Myocardial InfarctionNani BernstorffNoch keine Bewertungen
- 2018 Anticoagulation in Acute Coronary Syndrome-State of The ArtDokument25 Seiten2018 Anticoagulation in Acute Coronary Syndrome-State of The ArtNani BernstorffNoch keine Bewertungen
- Statin HipertensiDokument12 SeitenStatin HipertensiAlifianiii KartikaNoch keine Bewertungen
- 2018 Anticoagulation in Acute Coronary Syndrome-State of The ArtDokument25 Seiten2018 Anticoagulation in Acute Coronary Syndrome-State of The ArtNani BernstorffNoch keine Bewertungen
- 2018 Statin in The Treatment of Patients With Myocardial InfarctionDokument4 Seiten2018 Statin in The Treatment of Patients With Myocardial InfarctionNani BernstorffNoch keine Bewertungen
- 1300 Status Epilepticus Guideline NouriDokument2 Seiten1300 Status Epilepticus Guideline NouriNani BernstorffNoch keine Bewertungen
- 2017 High-Dose Atorvastatin Versus Moderate Dose On Early Vascular Protection After ST-elevation Myocardial InfarctionDokument10 Seiten2017 High-Dose Atorvastatin Versus Moderate Dose On Early Vascular Protection After ST-elevation Myocardial InfarctionNani BernstorffNoch keine Bewertungen
- Anticoagulant Therapy For Acute Coronary SyndromesDokument6 SeitenAnticoagulant Therapy For Acute Coronary SyndromesAtrik Pristica DianiNoch keine Bewertungen
- CHEST Crisis HipertensivasDokument14 SeitenCHEST Crisis HipertensivasNani BernstorffNoch keine Bewertungen
- 2017 Antithrombotic Therapy To Reduce Ischemic Events in ACS Undergoing PCIDokument10 Seiten2017 Antithrombotic Therapy To Reduce Ischemic Events in ACS Undergoing PCINani BernstorffNoch keine Bewertungen
- 2015 Pleiotropic Effects of Statins On The Cardiovascular SystemDokument15 Seiten2015 Pleiotropic Effects of Statins On The Cardiovascular SystemNani BernstorffNoch keine Bewertungen
- Arbe2018 PDFDokument6 SeitenArbe2018 PDFNani BernstorffNoch keine Bewertungen
- Monk - Way of The Elements RevisedDokument3 SeitenMonk - Way of The Elements Revisedluigipokeboy0% (1)
- Thesis 1-15Dokument15 SeitenThesis 1-15hewelirNoch keine Bewertungen
- 520L0586 MMF044Dokument48 Seiten520L0586 MMF044vendas servicosNoch keine Bewertungen
- General Anaesthesia MCQsDokument5 SeitenGeneral Anaesthesia MCQsWasi Khan100% (3)
- AdPoe The Hunting of The HareDokument2 SeitenAdPoe The Hunting of The HarePI CubingNoch keine Bewertungen
- Module 12. Big Issues Lesson 12a. Reading. Pages 140-141: No Words TranslationDokument4 SeitenModule 12. Big Issues Lesson 12a. Reading. Pages 140-141: No Words TranslationLeonardo Perez AlegriaNoch keine Bewertungen
- With EU Stage V Engine Installed: 200 HP (149 KW) / 2,200 RPMDokument4 SeitenWith EU Stage V Engine Installed: 200 HP (149 KW) / 2,200 RPMSara Sarmiento EcheverryNoch keine Bewertungen
- Important Notice 38-2021 Dated 24-03-2021 Available Seats Foreign National Spon INI CET PG Courses July 2021Dokument3 SeitenImportant Notice 38-2021 Dated 24-03-2021 Available Seats Foreign National Spon INI CET PG Courses July 2021Priyobrata KonjengbamNoch keine Bewertungen
- Lab Centre of Pressure Ecw341Dokument4 SeitenLab Centre of Pressure Ecw341danialNoch keine Bewertungen
- Neet Code W Question Paper AkashDokument21 SeitenNeet Code W Question Paper AkashGlen PintoNoch keine Bewertungen
- Eoi QAMDokument6 SeitenEoi QAMPeeyush SachanNoch keine Bewertungen
- Macleod - 1974 - Lucian's Knowledge of TheophrastusDokument2 SeitenMacleod - 1974 - Lucian's Knowledge of TheophrastusSIMONE BLAIRNoch keine Bewertungen
- Ansible Automation SA Technical Deck Q2FY19Dokument43 SeitenAnsible Automation SA Technical Deck Q2FY19daniel_vp21Noch keine Bewertungen
- Cold N Brew MenuDokument3 SeitenCold N Brew MenuRizki FitriaNoch keine Bewertungen
- Production Technology of Dragon FruitDokument6 SeitenProduction Technology of Dragon FruitAbhinash MoirangthemNoch keine Bewertungen
- 1 Introduction To Microsoft VirtualizationDokument36 Seiten1 Introduction To Microsoft VirtualizationRavinder KantNoch keine Bewertungen
- 100 Yer PM PPM 0605Dokument40 Seiten100 Yer PM PPM 0605biplabpal2009Noch keine Bewertungen
- Magneto-Convective Non-Newtonian Nanofluid With Momentum and Temperature Dependent Slip Flow From A Permeable Stretching Sheet With Porous Medium and Chemical ReactionDokument18 SeitenMagneto-Convective Non-Newtonian Nanofluid With Momentum and Temperature Dependent Slip Flow From A Permeable Stretching Sheet With Porous Medium and Chemical ReactionIOSRjournalNoch keine Bewertungen
- Disa Match: A Match You Can Count OnDokument8 SeitenDisa Match: A Match You Can Count OngNoch keine Bewertungen
- ONGC Buyout GOI's Entire 51.11% Stake in HPCLDokument4 SeitenONGC Buyout GOI's Entire 51.11% Stake in HPCLArpan AroraNoch keine Bewertungen
- BHLP Year Long Plan Required English Medium 2023 24 Batch Final 991676721629413Dokument3 SeitenBHLP Year Long Plan Required English Medium 2023 24 Batch Final 991676721629413A V GamingNoch keine Bewertungen
- K&J Magnetics - Demagnetization CurvesDokument4 SeitenK&J Magnetics - Demagnetization CurvessubbannachrsNoch keine Bewertungen
- En LF Drivers 10nw76 8Dokument3 SeitenEn LF Drivers 10nw76 8ChrisNoch keine Bewertungen
- Tutorial 2Dokument2 SeitenTutorial 2Adam HakimiNoch keine Bewertungen
- Primakuro Catalogue Preview16-MinDokument10 SeitenPrimakuro Catalogue Preview16-MinElizabeth LukitoNoch keine Bewertungen
- BLANCHARD-The Debate Over Laissez Faire, 1880-1914Dokument304 SeitenBLANCHARD-The Debate Over Laissez Faire, 1880-1914fantasmaNoch keine Bewertungen
- Afectiuni Si SimptomeDokument22 SeitenAfectiuni Si SimptomeIOANA_ROX_DRNoch keine Bewertungen
- Suneet Narayan Singh (Updated CV), NDokument4 SeitenSuneet Narayan Singh (Updated CV), Nnishant gajeraNoch keine Bewertungen