Beruflich Dokumente
Kultur Dokumente
Assr, Vemp, VNG, Oae
Hochgeladen von
Suprit SnOriginalbeschreibung:
Originaltitel
Copyright
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Assr, Vemp, VNG, Oae
Hochgeladen von
Suprit SnCopyright:
Dr.
Supreet Singh Nayyar, AFMC
2009
AUDITORY STEADY STATE RESPONSE (ASSR)
(for more topics & ppts visit www.nayyarENT.com)
Introduction A far-field evoked auditory potential test Principle Similarity to ABR o Sound stimulus converted to electrical impulse pathway EE COLI recording via electrodes on scalp Difference from ABR o Evoked using continuous rather than transient stimulation o Stimulus is amplitude or frequency modulated o Place of maximal stimulation on the cochlea is determined by the choice of carrier frequency o Continuous, sinusoidal nature of the response lends itself to analysis in frequency rather than the time domain o ASSR is converted to frequency domain using FAST FOURIER TRANSFORM (FFT) techniques. o Frequency spectrum is considerably narrower than the frequency spectrum of the tone bursts typically used to elicit the ABR o Additionally continuous rather than a transient stimulus possible to achieve higher stimulation easier to distinguish between severe and profound hearing loss Procedure Headphone,computer for analysis Electrodes o Inverting (-ve) two Ipsilateral mastoid Scalp of neck o Non inverting (+ve) Vertex o Ground Forehead Historical perspective When the ASSR was originally described, modulation frequencies of approximately 40 Hz were generally used to evoke the response, and relatively strong correlations between ASSR thresholds and audiometric thresholds were reported Initial optimism about the correlation between ASSR thresholds and audiometric thresholds waned, however, when it was noted that these responses were adversely affected by sleep and sedation Interest in ASSR was revived when research showed that these problems could be www.nayyarENT.com
1
Dr. Supreet Singh Nayyar, AFMC
2009
avoided if a modulation frequency of approximately 80 Hz rather than 40 Hz was used There have been a number of studies that have reported finding good correlations between ASSR thresholds and audiometric thresholds in both children and adults
Uses & advantages Analysis of the ASSR does not require as much training as is currently needed with ABR For estimating frequency-specific thresholds give results similar to PTA To record the ASSR in ears with no measurable ABR at the limits of the equipment Low frequency hearing loss can be recorded For evaluation of children being considered for cochlear implantation
VEMP
(for more topics & ppts visit www.nayyarENT.com) Principle : Sudden Changes in Saccular Activity Evoke Changes in Postural Tone
Anatomic and Physiologic Basis of normal saccular function
Saccule lies in a parasagittal plane Hair cells of the saccule, are polarized so that they are excited by otoconial mass displacements away from the striola, can sense accelerations up and down Only the sacculus can sense linear accelerations up or down When the head is upright in the gravitational field, the acceleration resulting from gravity (9.8 m/sec2) constantly pulls the saccular otoconial mass toward the earth Afferents in the inferior half of the saccule, whose hair cells are excited by this downward acceleration, have lower firing rates and lower sensitivities to linear accelerations than do those afferents in the upper half Afferents in the upper half are excited by relative upward acceleration of the otoconial mass, such as might occur when the head drops suddenly (e.g., when one is falling) Thus, sudden excitation of hair cells across the saccular macula would likely be interpreted by the brain as a sudden loss of postural tone (i.e., falling) The appropriate compensatory reflex would be one that activates the trunk and limb extensor muscles and relaxes the flexors to restore postural tone Accordingly, the saccular afferents project to the lateral portions of the vestibular nuclei, which give rise to the vestibulospinal tract, in contrast to the utricular afferents, which project more rostrally to areas involved in the VOR
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC
2009
Clinical Importance
Saccular excitation underlies the test of VEMP VEMPs are transient decreases in flexor muscle electromyographic (EMG) activity evoked by loud acoustic clicks or tones applied to the ear Sufficiently loud sounds applied to the ear excite saccular afferents The predicted reflexive response would include relaxation of flexor muscles EMG activity averaged over multiple acoustic stimuli from a tonically contracting flexor muscle will demonstrate a biphasic short-latency relaxation potential EMG activity can be recorded in many different flexor muscles, but SCM responses have been best described Because the saccule is the only end organ that mediates VEMP responses, absence of VEMP responses may indicate saccular dysfunction However, transmission of the VEMP acoustic stimulus is very sensitive to any cause of conductive hearing loss in the middle ear Interestingly, the preservation of VEMP responses in the face of conductive hearing loss implies an abnormally low acoustic impedance of the labyrinth, such as occurs in superior canal dehiscence syndrome or with enlarged vestibular aqueduct syndrome
Method
An intense click or tone pip is delivered to an earphone, stimulating sensory tissue (otolith organ) in the saccule This is interesting since the saccule is part of the balance system and not normally thought of as being sensitive to sound.(work on pigeons was done by pierre fluorence) Neural impulses travel from saccule up to inferior division of the vestibular nerve (cranial nerve VIII), to the lateral vestibular nucleus, to the lateral vestibulospinal tract, to the accessory nerve (XI), to the sternocleidomastoid muscle (SCM). To increase sensitivity, the head is turned away from the ear tested (right ear) and elevated to tense the SCM SCM contracts producing a large amplitude potential (compared to ABR) with positive and negative peaks at 13 and 23 ms (P13 and N23) This pathway is called the vestibulo-collic reflex. Presence of the VEMP indicates integrity of the pathway VEMPs may be abnormal (absent, low amplitude, high or enhanced amplitude, or delayed latency) in Meniere's disease, superior canal dehiscence, vestibular neuritis, multiple sclerosis, migraine, spinocerebellar degeneration. See table. If RE and LE represent the VEMP amplitude for the right and left ears, then a 30-47% asymmetry is clinically significant: Asymmetry = 100*(LE - RE)/(LE + RE)
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC
2009
The following figure illustrates a reduced response obtained from a patient with Meniere's disease (affecting the left ear):
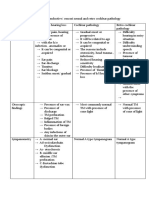
Pathology
Meniere's disease Superior canal dehiscence syndrome Neurolabyrinthitis Vestibular neuritis Migraine Spinocerebellar degeneration Multiple sclerosis Brainstem stroke Large Vestibular Acqueduct syndrome Conductive deafness
VEMP Response
Absent, reduced, enhanced Enhanced Absent, reduced Absent, reduced Absent, reduced, delayed Absent, delayed Absent, delayed Absent, delayed Enhanced reduced
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC
2009
VIDEONYSTAGMOGRAPHY (VNG) TESTING
(for more topics & ppts visit www.nayyarENT.com)
Videonystagmography (VNG) is often used in the evaluation of a patient who presents with vertigo and uses the vestibular-ocular reflex to indirectly measure vestibular function. VNG tests for nystagmus using infrared light and video technology to monitor eye movements during testing.
VNG testing is considered the new standard for testing inner ear functions over Electronystagmography (ENG), because VNG measures the movements of the eyes directly through infrared cameras, instead of measuring the mastoid muscles around the eyes with electrodes like the previous ENG version. VNG testing is more accurate, more consistent, and more comfortable for the patient. By having the patient more comfortable and relaxed, consistent and accurate test results are more easily achieved. VNG testing is used to determine if a vestibular (inner ear) disease may be causing a balance or dizziness problem, and is one of the only tests available today that can decipher between a unilateral (one ear) and bilateral (both ears) vestibular loss. VNG testing is a series of tests designed to document a persons ability to follow visual objects with their eyes and how well the eyes respond to information from the vestibular system. This test also addresses the functionality of each ear and if a vestibular deficit may be the cause of a dizziness or balance problem. To monitor the movements of the eyes, infrared goggles are placed around the eyes to record eye movements during testing. VNG testing is non-invasive, and only minor discomfort is felt by the patients during testing as a result of wearing goggles. Appointments usually last about 1.5 hours.
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC
2009
There are 4 main parts to a VNG test: 1. Occular Mobility
You will be asked to have your eyes follow objects that jump from place to place, stand still, or move smoothly. The technician will be looking for any slowness or inaccuracies in your ability to follow visual targets. This may indicate a central or neurological problem, or possibly a problem in the pathway connecting the vestibular system to the brain.
2. Optokinetic Nystagmus
2. You will be asked to view a large, continuously moving visual image to see if your eyes can appropriately track these movements. Like the occular mobility tests, the technician will be looking for any slowness or inaccuracies in your ability to follow visual targets. This may indicate a central or neurological problem, or possibly a problem in the pathway connecting the vestibular system to the brain.
3. Positional Nystagmus
The technician will move your head and body into various positions to make sure that there are no inappropriate eye movements (nystagmus), when your head is in different positions. This test is looking at your inner ear system and the condition of the endolymph fluid in your semi-circular canals. The technician is verifying that small calcium carbonate particles called otoconia are not suspended in the fluid and causing a disturbance to the flow of the fluid.
4. Caloric Testing
The technician will stimulate both of your inner ears (one at a time) with warm and then cold air. They will be monitoring the movements of your eyes using goggles to make sure that both of your ears can sense this stimulation. This test will confirm that your vestibular system for each ear is working and responding to stimulation. This test in the only test available that can decipher between a unilateral and bilateral loss.
Optokinetic Testing using Micromedical Visual Eyes System
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC
2009
Otoacoustic emissions
(for more topics & ppts visit www.nayyarENT.com)
Otoacoustic emissions are low energy sounds produced by the cochlea. They are thought to be acoustic byproducts of the outer hair cells, which are thought to underlie the amplification of the basilar membrane. Clinically, they are most often evoked using transient and distorted product stimulation. The evoking response causes outer hair cell motility which results in a mechanical wave that travels from the cochlea through the middle ear and tympanic membrane to the ear canal where it is recorded. Spontaneous emissions are not present from the cochlea when there is a greater than 25dB hearing loss. Unfortunately, they are not present in all normal ears, which does not make this the test of choice to clinically assess cochlear functioning. Transient stimuli such as clicks evoke emissions from a large portion of the cochlea. The emissions are then sampled and signal-averaged to extract them from background noise. These alternating samples are then stored in one of two memory banks and compared. Reproducibility, expressed as a percentage, is the cross correlation between these two waveforms. A reproducibility score of 50% or greater indicates that a response is present. Waveforms may vary significantly between people, but they are highly reproducible within a given individual. When hearing thresholds are better than 35dB, TEOAEs are generally present. The advantages of TEOAE are that it can separate normal from abnormal ears at 20-30dB and that it is quick. The specificity of clean, dry ears of infants is 95%. The main disadvantage is that it fails to extract responses at higher frequencies. Distorted products are additional tones which are created when two tones, f1/lower frequency & f2/higher frequency, are presented simultaneously to a healthy cochlea. The most robust DPOAE occurs at the frequency determined by the equation 2f1-f2. Due to a nonlinear process within the cochlea, the DPOAE assesses the cochlear integrity of the region near f2. When hearing thresholds are better than 50dB, DPOAEs are generally present. The main advantage is that DPOAEs can recover OAEs above 6000Hz. The transmission properties of the middle ear directly influence the OAE characteristics. The presence of a middle ear effusion, as in otitis media, affects both the forward and backward transmission. Although otitis media often eliminates OAEs, it is possible to record OAEs in some patients with middle ear effusion. OAE characteristics increase significantly over the first few days of life likely as a result of changes in the ear canal and middle ear. Small tympanic perforations will impede the forward transmission. This can usually be overcome with DPOAEs by increasing the amplitude.
www.nayyarENT.com
Dr. Supreet Singh Nayyar, AFMC
2009
Central Auditory Processing
(for more topics & ppts visit www.nayyarENT.com)
There is no accepted definition of Central Auditory Processing (CAP). In its simplest form, it is what we do with what we hear. The Task Force on CAP Consensus Development defines CAP as the auditory system mechanisms and processes responsible for the following behavioral phenomena:
Sound localization Auditory discrimination Auditory pattern recognition Temporal aspects of audition, including temporal resolution and masking Auditory performance decrements with competing and degraded acoustic signals
Deficiencies in any of these behaviors are considered central auditory processing disorders (CAPD). Results of CAPD testing have revealed clustering of test results and characteristic behaviors. These four categories are decoding, tolerance-fading memory, integration, and organization. Each of the four categories has been associated with a specific region of the brain. The Buffalo model of CAPD assessment and management takes into account the classification of CAPD as well as speech language evaluation and academic characteristics. It is important to understand that there is no one test that is sensitive enough to detect CAPD, especially in children where the variability of the tests is very wide. Therefore a battery of tests is recommended. In the Buffalo model, the CAP battery always includes the Staggered Spondaic Word (SSW) test, the Phonemic Synthesis (PS) test, a speech-in-noise (SN) test, and the masking level difference (MLD) test. Most patients will have weaknesses in more than one category and the categories are not mutually exclusive.
(for more topics & ppts visit www.nayyarENT.com)
www.nayyarENT.com
Das könnte Ihnen auch gefallen
- Snoring, A Simple Guide To The Condition, Treatment And Related ConditionsVon EverandSnoring, A Simple Guide To The Condition, Treatment And Related ConditionsNoch keine Bewertungen
- Otoacoustic Emissions From MedscapeDokument5 SeitenOtoacoustic Emissions From MedscapeMin-Joo Esther ParkNoch keine Bewertungen
- Consultant in Audiology: Passbooks Study GuideVon EverandConsultant in Audiology: Passbooks Study GuideNoch keine Bewertungen
- Assessment of HearingDokument51 SeitenAssessment of HearingSwetha PasupuletiNoch keine Bewertungen
- Audiology MaskingDokument6 SeitenAudiology MaskingRavi VarakalaNoch keine Bewertungen
- Anatomy of The Vestibular SystemDokument10 SeitenAnatomy of The Vestibular Systemmbs30689Noch keine Bewertungen
- FlashcardsDokument140 SeitenFlashcardsDoodNoch keine Bewertungen
- Interactions between the Craniomandibular System and Cervical Spine: The influence of an unilateral change of occlusion on the upper cervical range of motionVon EverandInteractions between the Craniomandibular System and Cervical Spine: The influence of an unilateral change of occlusion on the upper cervical range of motionNoch keine Bewertungen
- Slow Auditory Evoked Potentials (1 InterligneDokument8 SeitenSlow Auditory Evoked Potentials (1 Interligner.boniver524Noch keine Bewertungen
- Audiometric Testing of AdultsDokument6 SeitenAudiometric Testing of AdultssofiameNoch keine Bewertungen
- Vestibular DisordersDokument8 SeitenVestibular DisordersHilwy Al-haninNoch keine Bewertungen
- Post Laryngectomy Voice RehabilitationDokument58 SeitenPost Laryngectomy Voice RehabilitationfakeywakeyNoch keine Bewertungen
- Oae Presentation,/ Kunnampallil GejoDokument69 SeitenOae Presentation,/ Kunnampallil GejoKUNNAMPALLIL GEJO JOHN100% (1)
- Auditory Brainstem Response - ABR - in Clinical Practice PDFDokument9 SeitenAuditory Brainstem Response - ABR - in Clinical Practice PDFary wisma dewiNoch keine Bewertungen
- ASSR Thresholds PDFDokument7 SeitenASSR Thresholds PDFDaniela Garrido GonzálezNoch keine Bewertungen
- Speech AudiometryDokument9 SeitenSpeech AudiometryVarunSharmaNoch keine Bewertungen
- BPPVDokument10 SeitenBPPVRizki MaulanaNoch keine Bewertungen
- Auditory Brain Stem ImplantsDokument7 SeitenAuditory Brain Stem Implantsabirajalakshmix9395Noch keine Bewertungen
- Impedance Audiometry - Overview, Indications, ContraindicationsDokument8 SeitenImpedance Audiometry - Overview, Indications, ContraindicationsSorin AilincaiNoch keine Bewertungen
- Basic Audiology (Fred)Dokument4 SeitenBasic Audiology (Fred)Aisyah BadhrulhishamNoch keine Bewertungen
- Auditory Brainstem ResponseDokument18 SeitenAuditory Brainstem ResponseFree dataNoch keine Bewertungen
- Symptomatology and Examination of The Larynx and TracheaDokument42 SeitenSymptomatology and Examination of The Larynx and TracheaYibeltalNoch keine Bewertungen
- VEMP Guidance v1.1 20121Dokument19 SeitenVEMP Guidance v1.1 20121M. Arief PurnantaNoch keine Bewertungen
- The Use of Optokinetic Stimulation in VestibularDokument6 SeitenThe Use of Optokinetic Stimulation in Vestibularbuku fisio0% (1)
- Auditory Brainstem Evoked Response (Abr)Dokument37 SeitenAuditory Brainstem Evoked Response (Abr)Nitin Sharma100% (2)
- Mankekar - Implantablehearing Devices Other Than Cochlear ImplantsDokument119 SeitenMankekar - Implantablehearing Devices Other Than Cochlear ImplantscetristanNoch keine Bewertungen
- Peripheral Vs Central Vestibular DisordersDokument2 SeitenPeripheral Vs Central Vestibular DisordersraraNoch keine Bewertungen
- Understanding A Dizzy AdultDokument39 SeitenUnderstanding A Dizzy AdultR Srinivasa RaghavanNoch keine Bewertungen
- Revision OssiculoplastyDokument14 SeitenRevision Ossiculoplastyapi-19500641Noch keine Bewertungen
- Congenital Aural AtresiaDokument30 SeitenCongenital Aural Atresiaalrafeek1050Noch keine Bewertungen
- Auditory Pathway PDFDokument35 SeitenAuditory Pathway PDFJohnson JayarajNoch keine Bewertungen
- Vestibular Appratus: BY: Harshita YadavDokument49 SeitenVestibular Appratus: BY: Harshita YadavNitin SharmaNoch keine Bewertungen
- A Guide To TympanometryDokument17 SeitenA Guide To Tympanometryoeoe26100% (1)
- New Born Hearing FactsDokument8 SeitenNew Born Hearing FactsAhiawortor Kplorla100% (1)
- Anatomy & Physiology of Ear (Prof. Fatthi Abdel-Baki)Dokument20 SeitenAnatomy & Physiology of Ear (Prof. Fatthi Abdel-Baki)Dr-Firas Nayf Al-ThawabiaNoch keine Bewertungen
- Malignant Otitis Externa 20070821Dokument0 SeitenMalignant Otitis Externa 20070821Suci PramadianiNoch keine Bewertungen
- Larynx Removal SurgeryDokument33 SeitenLarynx Removal SurgerySwathi GNoch keine Bewertungen
- Anatomy & Physiology of Vestibular System.Dokument68 SeitenAnatomy & Physiology of Vestibular System.Prasanna DattaNoch keine Bewertungen
- TympanoplastyDokument21 SeitenTympanoplastyDr. T. BalasubramanianNoch keine Bewertungen
- Hearing Losses and Assocated CorealtesDokument3 SeitenHearing Losses and Assocated CorealtesAchu SachuNoch keine Bewertungen
- Audiology: Test at A GlanceDokument13 SeitenAudiology: Test at A Glanceabdullah hussinyNoch keine Bewertungen
- Therapeutic Management of Laryngectomy - PDF / KUNNAMPALLIL GEJO JOHNDokument31 SeitenTherapeutic Management of Laryngectomy - PDF / KUNNAMPALLIL GEJO JOHNKUNNAMPALLIL GEJO JOHNNoch keine Bewertungen
- The Effects of Earphone Use On The Incidence of Noise-Induced Hearing Loss An Empirical Study of Senior High School Students in Banda AcehDokument8 SeitenThe Effects of Earphone Use On The Incidence of Noise-Induced Hearing Loss An Empirical Study of Senior High School Students in Banda AcehInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Tplasty Cartilage Slides 080319 PDFDokument46 SeitenTplasty Cartilage Slides 080319 PDFasiyazaidiaNoch keine Bewertungen
- Genes Hearing DeafnessDokument328 SeitenGenes Hearing DeafnessjvojnicNoch keine Bewertungen
- Etiology and Diagnosis of Tinnitus - UpToDateDokument18 SeitenEtiology and Diagnosis of Tinnitus - UpToDateAdri NolascoNoch keine Bewertungen
- Management of Congenital Aural AtresiaDokument22 SeitenManagement of Congenital Aural AtresiamelaniNoch keine Bewertungen
- Hearing Disorders and Audiogram InterpretationDokument27 SeitenHearing Disorders and Audiogram InterpretationGaluhNoch keine Bewertungen
- 2022 OlfactionDokument46 Seiten2022 OlfactionRam LakshmanNoch keine Bewertungen
- Cochlear ImplantDokument33 SeitenCochlear ImplantNithiyah DevarajuNoch keine Bewertungen
- Diagnostic Audiology - 834 - Syllabus - 2015Dokument37 SeitenDiagnostic Audiology - 834 - Syllabus - 2015api-349133705Noch keine Bewertungen
- Otosclerosis Slides 061018Dokument96 SeitenOtosclerosis Slides 061018Paraguay De La Cruz JoelNoch keine Bewertungen
- ورق مذاكره PDFDokument100 Seitenورق مذاكره PDFsalamred100% (1)
- Physiology of EquilibriumDokument64 SeitenPhysiology of EquilibriumSaiNoch keine Bewertungen
- Temp Bone Trauma Slides 051012Dokument55 SeitenTemp Bone Trauma Slides 051012RaihanFarhanaNoch keine Bewertungen
- SGD 4 - Facial Nerve PalsyDokument9 SeitenSGD 4 - Facial Nerve PalsyDanang SetiajiNoch keine Bewertungen
- Temporal Bone AnatomyDokument39 SeitenTemporal Bone AnatomymizmuzNoch keine Bewertungen
- LPR by Dr. SS NayyarDokument45 SeitenLPR by Dr. SS NayyarSuprit Sn100% (1)
- Inferior Turbinate Hypertrophy PDFDokument3 SeitenInferior Turbinate Hypertrophy PDFSuprit SnNoch keine Bewertungen
- Meatoplasty in CWD PDFDokument7 SeitenMeatoplasty in CWD PDFSuprit Sn100% (1)
- EPISTAXISDokument25 SeitenEPISTAXISSuprit Sn78% (9)
- Dural Venous Sinuses PDFDokument3 SeitenDural Venous Sinuses PDFSuprit SnNoch keine Bewertungen
- Drooling PDFDokument2 SeitenDrooling PDFSuprit SnNoch keine Bewertungen
- Laryngeal Electromyography Emg Lemg PDFDokument3 SeitenLaryngeal Electromyography Emg Lemg PDFSuprit Sn50% (2)
- Thyroid StormDokument3 SeitenThyroid StormSuprit SnNoch keine Bewertungen
- Maxillary Carcinoma, Nasal Cavity and Paranasal Sinus Malignancy PDFDokument18 SeitenMaxillary Carcinoma, Nasal Cavity and Paranasal Sinus Malignancy PDFSuprit Sn100% (2)
- Deep Neck Spaces PDFDokument15 SeitenDeep Neck Spaces PDFSuprit SnNoch keine Bewertungen
- Facial Pain PDFDokument4 SeitenFacial Pain PDFSuprit SnNoch keine Bewertungen
- CSF RhinorrhoeaDokument12 SeitenCSF RhinorrhoeaSuprit Sn100% (5)
- Cochlear ImplantationDokument11 SeitenCochlear ImplantationSuprit Sn100% (3)
- Cholesteatoma Part 9 - Reconstruction of The Mastoid Cavity PDFDokument4 SeitenCholesteatoma Part 9 - Reconstruction of The Mastoid Cavity PDFSuprit SnNoch keine Bewertungen
- Cholesteatoma Part 5 Congenital Cholesteatoma PDFDokument4 SeitenCholesteatoma Part 5 Congenital Cholesteatoma PDFSuprit Sn100% (1)
- OSA Part 3Dokument10 SeitenOSA Part 3Suprit SnNoch keine Bewertungen
- Alaryngeal SpeechDokument6 SeitenAlaryngeal SpeechSuprit SnNoch keine Bewertungen
- OtosclerosisDokument9 SeitenOtosclerosisSuprit SnNoch keine Bewertungen
- Laryngopharyngeal Reflux 2Dokument25 SeitenLaryngopharyngeal Reflux 2Suprit Sn100% (1)
- Sleep Disordered Breathing (Part 4) : Obstructive Sleep Apnea in ChildrenDokument5 SeitenSleep Disordered Breathing (Part 4) : Obstructive Sleep Apnea in ChildrenSuprit SnNoch keine Bewertungen
- Anatomy and Physiology of Salivary GlandsDokument55 SeitenAnatomy and Physiology of Salivary GlandsSuprit SnNoch keine Bewertungen
- Oesophagus Foreign BodyDokument3 SeitenOesophagus Foreign BodySuprit SnNoch keine Bewertungen
- Conf PrenatalsensorydevelopmentDokument2 SeitenConf Prenatalsensorydevelopmentapi-259661638Noch keine Bewertungen
- Student's Booklet - Human Body and SensitivityDokument8 SeitenStudent's Booklet - Human Body and SensitivityRafa Rguez PerezNoch keine Bewertungen
- Creative Writing Quiz # 2 Imagery: Email AddressDokument8 SeitenCreative Writing Quiz # 2 Imagery: Email AddressJilian MeiNoch keine Bewertungen
- Full Download Essentials of Geology 10th Edition Test Bank Frederick K Lutgens PDF Full ChapterDokument36 SeitenFull Download Essentials of Geology 10th Edition Test Bank Frederick K Lutgens PDF Full Chapterstree.brooklet1wue7u100% (14)
- Case Presentation BY Dr. Prashanti Ophthalmology Ist YrDokument22 SeitenCase Presentation BY Dr. Prashanti Ophthalmology Ist YrAyushman100% (3)
- Macarsmento Metodo PlatôDokument6 SeitenMacarsmento Metodo PlatôAdriana BatistaNoch keine Bewertungen
- Colour Vision TestsDokument9 SeitenColour Vision Testsbforte09Noch keine Bewertungen
- Sir Imran SynopsisDokument13 SeitenSir Imran Synopsismethoo143Noch keine Bewertungen
- Sumi - Presentation On BlindnessDokument23 SeitenSumi - Presentation On Blindnessabhigyan priyadarshanNoch keine Bewertungen
- Poteat On Acoustic Weapons AFIO INTEL - FALL2017 Oct 26 v3Dokument2 SeitenPoteat On Acoustic Weapons AFIO INTEL - FALL2017 Oct 26 v3Jason I. PobleteNoch keine Bewertungen
- Bionic EyeDokument16 SeitenBionic Eyeavinash76350% (2)
- The Human Eye Powerpoint NotesDokument22 SeitenThe Human Eye Powerpoint Notesapi-262193618Noch keine Bewertungen
- Theories of Colour VisionDokument4 SeitenTheories of Colour VisionZumairi Tamin0% (1)
- Let's Look Together: An Interactive Picture Book For People With Alzheimer's and Other Forms of Memory Loss (Ziegler Excerpt)Dokument9 SeitenLet's Look Together: An Interactive Picture Book For People With Alzheimer's and Other Forms of Memory Loss (Ziegler Excerpt)Health Professions Press, an imprint of Paul H. Brookes Publishing Co., Inc.Noch keine Bewertungen
- Error of RefractionDokument3 SeitenError of RefractionMargot SanchezNoch keine Bewertungen
- Sensory PathwaysDokument17 SeitenSensory PathwaysNabilah Ani SofianNoch keine Bewertungen
- UIColorsDokument15 SeitenUIColorsJiNXedNoch keine Bewertungen
- Scotopic Vs PhotopicDokument12 SeitenScotopic Vs PhotopicAdolf ReyesNoch keine Bewertungen
- DIP Lec 04 - Digital Image Fundamental - I - Week 04 PDFDokument50 SeitenDIP Lec 04 - Digital Image Fundamental - I - Week 04 PDFMuhammad Ali RazaNoch keine Bewertungen
- 07 Crossed Eyes Nystagmus and AmblyopiaDokument7 Seiten07 Crossed Eyes Nystagmus and AmblyopiaMwanja MosesNoch keine Bewertungen
- Structure of EyeDokument11 SeitenStructure of EyeAKSHAT JINDALNoch keine Bewertungen
- Approach To A Case of DiplopiaDokument63 SeitenApproach To A Case of DiplopiaSriniwasNoch keine Bewertungen
- FR 15 Farnsworth and LanthonyD15 Instructions Rev 1.7 0506Dokument7 SeitenFR 15 Farnsworth and LanthonyD15 Instructions Rev 1.7 0506Muchammad Karunia Fadillah100% (1)
- Science Form 3 KSSM Chapter 1Dokument10 SeitenScience Form 3 KSSM Chapter 1Wan Shuhaimi50% (4)
- Grade 3 Q2 Science LASDokument128 SeitenGrade 3 Q2 Science LASERIC VALLENoch keine Bewertungen
- Silly Socks Preschool Learning Pack PDFDokument9 SeitenSilly Socks Preschool Learning Pack PDFaleparsantNoch keine Bewertungen
- Eye RobicsDokument28 SeitenEye RobicsIsmi Raudha0% (1)
- Masking Frequency Selectivity and The Critical BandDokument80 SeitenMasking Frequency Selectivity and The Critical Bandعلی احمدNoch keine Bewertungen
- In The Name of Holy Allah, The Most Beneficent, The Most MercifulDokument60 SeitenIn The Name of Holy Allah, The Most Beneficent, The Most MercifulSyed Jawad Raza KazmiNoch keine Bewertungen
- SL4SB U7 The Super DoctorDokument12 SeitenSL4SB U7 The Super DoctorLiane RegnardNoch keine Bewertungen
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Von EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Bewertung: 3 von 5 Sternen3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedVon EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedBewertung: 4.5 von 5 Sternen4.5/5 (82)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDVon EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDBewertung: 5 von 5 Sternen5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionVon EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionBewertung: 4 von 5 Sternen4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityVon EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityBewertung: 4 von 5 Sternen4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeVon EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeBewertung: 2 von 5 Sternen2/5 (1)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesVon EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesBewertung: 4.5 von 5 Sternen4.5/5 (1412)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsVon EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNoch keine Bewertungen
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsVon EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsBewertung: 4 von 5 Sternen4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsVon EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsBewertung: 5 von 5 Sternen5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisVon EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisBewertung: 4.5 von 5 Sternen4.5/5 (42)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaVon EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Comfort of Crows: A Backyard YearVon EverandThe Comfort of Crows: A Backyard YearBewertung: 4.5 von 5 Sternen4.5/5 (23)
- The Obesity Code: Unlocking the Secrets of Weight LossVon EverandThe Obesity Code: Unlocking the Secrets of Weight LossBewertung: 4 von 5 Sternen4/5 (6)
- Why We Die: The New Science of Aging and the Quest for ImmortalityVon EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityBewertung: 4.5 von 5 Sternen4.5/5 (6)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisVon EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisBewertung: 3.5 von 5 Sternen3.5/5 (2)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeVon EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeBewertung: 4.5 von 5 Sternen4.5/5 (254)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Von EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Bewertung: 4.5 von 5 Sternen4.5/5 (110)
- To Explain the World: The Discovery of Modern ScienceVon EverandTo Explain the World: The Discovery of Modern ScienceBewertung: 3.5 von 5 Sternen3.5/5 (51)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsVon EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsBewertung: 4.5 von 5 Sternen4.5/5 (39)
- The Marshmallow Test: Mastering Self-ControlVon EverandThe Marshmallow Test: Mastering Self-ControlBewertung: 4.5 von 5 Sternen4.5/5 (60)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingVon EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingBewertung: 4 von 5 Sternen4/5 (1138)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessVon EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessBewertung: 4.5 von 5 Sternen4.5/5 (328)