Beruflich Dokumente
Kultur Dokumente
The Heart
Hochgeladen von
Michael SamaniegoOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
The Heart
Hochgeladen von
Michael SamaniegoCopyright:
Verfügbare Formate
Cardiovascular System:
THE HEART
MICHAEL ANTHONY D. SAMANIEGO, RM, RN UPM-SHS
The heart produces the force that causes blood circulation.
Functions of the Heart
The heart is approximately the size of a closed fist and is shaped like a blunt cone.
It is in the mediastinum.
Size, Shape, and Location of the Heart
Mediastinum
The heart consists of two atria and two ventricles.
Anatomy of the Heart
Sometimes called auricles Refers to a chamber in which blood enters the heart The right atrium receives deoxygenated blood from the superior vena cava, inferior vena cava andcoronary sinus. The left atrium receives oxygenated blood from the left and right pulmonary veins
The Atria
collect and expel blood received from an atrium towards the peripheral beds within the body and lungs the right ventricle pumps blood into the pulmonary circulation to/for the lungs, the left ventricle pumps blood into the systemic circulation through the aorta (systemic circulation)
The Ventricles
The pericardium is a sac that surrounds the heart and consists of the fibrous pericardium and the serous pericardium.
The fibrous pericardium helps hold the heart in place.
The serous pericardium reduces friction as the heart beats.
Pericardium
The parietal pericardium lines the fibrous pericardium.
The visceral pericardium lines the exterior surface of the heart.
Serous Pericardium
lies between the parietal and visceral pericardium and is filled with pericardial fluid.
Pericardial cavity
The heart wall has three layers:
The outer epicardium (visceral pericardium) which provides
protection against the friction of rubbing organs.
The middle myocardium is responsible for contraction. The inner endocardium which reduces the friction resulting from bloods passing through the heart.
Heart Wall
Each atrium has a flap called the auricle. The coronary sulcus separates the atria from the ventricles.
The interventricular grooves separate the right and left ventricles.
The inferior and superior vena cava and the coronary sinus enter the right atrium. The four pulmonary veins enter the left atrium
External Anatomy & Coronary Circulation
The pulmonary trunk exits the right ventricle, and the aorta exits the left ventricle.
Coronary arteries branch off the aorta to supply the heart.
Blood returns from the heart tissues to the right atrium through the coronary sinus and cardiac veins.
Pulmonary trunk/artery
The interatrial septum separates the atria from each other
The interventricular septum separates the ventricles.
The tricuspid valve separates the right atrium and ventricle. The bicuspid valve separates the left atrium and ventricle.
Heart Chambers & the Valves
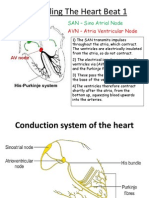
The SA node and the AV node are in the right atrium. The AV node is connected to the bundle branches in the interventricular septum by the AV bundle. The bundle branches give rise to Purkinje fibers, which supply the ventricles.
Conducting System of the Heart
The SA node initiates action potentials, which spread across the atria and cause them to contract. Action potentials are slowed in the AV node, allowing the atria to contract and blood to move into the ventricles. Then, the action potentials travel through the AV bundles and bundle branches to the Purkinje fibers, causing the ventricles to contract, starting at the apex.
a diagnostic tool that measures and records the electrical activity of the heart in exquisite detail. Interpretation of these details allows diagnosis of a wide range of heart conditions.
ELECTROCARDIOGRAM (ECG)
The ECG records only the electrical activities of the heart.
Depolarization of the atria produces the P wave.
Depolarization of the ventricles produces the QRS complex.
Repolarization of the atria occurs during the QRS complex. Repolarization of the ventricles produces the T wave.
The cardiac cycle is repetitive contraction and relaxation of the heart chambers. Blood moves through the circulatory system from areas of higher pressure to areas of lower pressure. Contraction of the heart produces the pressure.
Cardiac cycle
Although the heart is contracting, during the period of isovolumic contraction ventricular volume doesnt change because all the heart valves are closed. During the period of ejection, the semilunar valves open, and blood is ejected from the heart. Although the heart is relaxing, during the period of isovolumic relaxation, ventricular volume doesnt change because all the heart valves are closed.
Five Periods of Cardiac Cycle
Passive ventricular filling results when blood flows from the higher pressure in the veins and atria to the lower pressure in the relaxed ventricles. Active ventricular filling results when the atria contract and pump blood into the ventricles.
Contraction of the ventricles closes the AV valves, opens the semilunar valves, and ejects blood from the heart. The volume of blood in a ventricle just before it contracts is the end-diastolic volume. The volume of blood after contraction is the endsystolic volume
Events Occurring In Ventricular Systole
Relaxation of the ventricles results in closing of the semilunar valves, opening of the AV valves, and the movement of blood into the ventricles. Most ventricular filling occurs when blood flows from the higher pressure in the veins and atria to the lower pressure in the relaxed ventricles. Contraction of the atria completes ventricular filling. Events Occurring during Ventricular Diastole
Closure of the atrioventricular valves produces the first heart sound. Closure of the semilunar valves produces the second heart sound.
Heart Sounds
Murmurs an abnormal heart sounds Incompetent valve a gurgling or swishing sound after the valve closes caused by movement of blood in a direction opposite to normal results in turbulence. Stenosed - valves have an abnormally narrow opening and also produce abnormal heart sounds.
Abnormal Heart Sounds
Mean arterial pressure is the average blood pressure in the aorta. Adequate blood pressure is necessary to ensure delivery of blood to the tissues. Mean arterial pressure is proportional to cardiac output (amount of blood pumped by the heart per minute) times peripheral resistance (total resistance to blood flow through blood vessels).
Mean Arterial Pressure
Cardiac output is equal to stroke volume times heart rate. Stroke volume, the amount of blood pumped by the heart per beat, is equal to end-diastolic volume minus end-systolic volume. Venous return is the amount of blood returning to the heart.
Increased venous return increases stroke volume by increasing end-diastolic volume. Cardiac reserve is the difference between resting and exercising cardiac output.
Intrinsic Regulation 1. Venous return is the amount of blood that returns to the heart during each cardiac cycle. 2. Starlings law of the heart describes the relationship between preload and the stroke volume of the heart. An increased preload causes the cardiac muscle fibers to contract with a greater force and produce a greater stroke volume.
Regulation of the Heart
1. The cardioregulatory center in the medulla oblongata regulates the parasympathetic and sympathetic nervous control of the heart. 2. Parasympathetic control
It is supplied by the vagus nerve. It decreases heart rate. Postganglionic neurons secrete acetylcholine, which increases membrane permeability to K, producing hyperpolarization of the membrane
Extrinsic Regulation
It is supplied by the cardiac nerves. It increases heart rate and the force of contraction (stroke volume).
Postganglionic neurons secrete norepinephrine, which increases membrane permeability to Na and Ca2and produces depolarization of the membrane.
Sympathetic control
Epinephrine and norepinephrine are released into the blood from the adrenal medulla as a result of sympathetic stimulation. Epinephrine and norepinephrine increase the rate and force of heart contraction.
Baroreceptors monitor blood pressure. In response to a decrease in blood pressure, the baroreceptor reflexes increase sympathetic stimulation and decrease parasympathetic stimulation of the heart, resulting in an increase in heart rate and force of contraction.
Effect of Blood Pressure
Heart rate increases when body temperature increases It decreases when body temperature decreases.
Effect of Body temperature
Aging results in gradual changes in the function of the heart which are minor under resting conditions but are more significant during exercise. Hypertrophy of the left ventricle is a common agerelated condition.
The maximum heart rate decreases and by age 85 the cardiac output may be decreased by 3060%.
Effects of Aging on the Heart
Dr. Carmen N. Firmo
There is an increased tendency for valves to function abnormally and for arrhythmias to occur. An increased oxygen consumption, required to pump the same amount of blood, makes agerelated coronary artery disease more severe. Exercise improves the functional capacity of the heart at all ages.
Dr. Carmen N. Firmo
Endocarditis- is inflammation of the endocardium. Myocarditis- is inflammation of the myocardium and can lead to heart failure.
Pericarditis - is inflammation of the pericardium.
Rheumatic heart disease - can result from a streptococcal infection in young people.
Conditions and Diseases Affecting the Heart
Dr. Carmen N. Firmo
Coronary heart disease reduces the amount of blood that the coronary arteries are able to deliver to the myocardium. Infarct caused by inadequate blood flow , an area of damaged cardiac tissue.
Congenital heart disease is the result of abnormal development of the heart.
Dr. Carmen N. Firmo
Septal defect - is a hole in a septum between the left and right sides of the heart. Patent ductus arteriosus - results when a blood vessel called the ductus arteriosus, which is present in the fetus, fails to close after birth. Stenosis of a heart valve - is a narrowed opening through one of the heart valves.
Congenital Heart Disease
Dr. Carmen N. Firmo
Cyanosis- is a symptom of inadequate heart function in babies suffering from congenital heart disease. Heart failure is the result of progressive weakening of the heart muscle and the failure of the heart to pump blood effectively.
Dr. Carmen N. Firmo
Das könnte Ihnen auch gefallen
- Simple Office SpirometryDokument42 SeitenSimple Office SpirometryRoberto Merza III100% (4)
- Cardiovascular System PhysiologyDokument109 SeitenCardiovascular System PhysiologyKing kakaNoch keine Bewertungen
- Cardiology Mcq's Part - 1Dokument31 SeitenCardiology Mcq's Part - 1aymenNoch keine Bewertungen
- Heart Muscle: The Heart As A Pump and FunctionDokument4 SeitenHeart Muscle: The Heart As A Pump and Functionmcwnotes100% (1)
- Heart DiseaseDokument38 SeitenHeart DiseaseDr.Sunil KumarNoch keine Bewertungen
- Blood Vessel (Student)Dokument148 SeitenBlood Vessel (Student)Jerkin Razhed PostanesNoch keine Bewertungen
- Anatomy and Physiology II Course OutcomesDokument50 SeitenAnatomy and Physiology II Course OutcomesShirley LourdesNoch keine Bewertungen
- IMD - Step-Up To USMLE Step 3 - Chapter 1 - CardiologyDokument124 SeitenIMD - Step-Up To USMLE Step 3 - Chapter 1 - CardiologyAly SherifNoch keine Bewertungen
- Anatomy of Cardiovascular SystemDokument23 SeitenAnatomy of Cardiovascular SystemElvira Wisakhadewi100% (1)
- The MyocardiumDokument8 SeitenThe MyocardiumKyrene San Pedro RosalesNoch keine Bewertungen
- Anatomy of Larynx Lecture 7Dokument21 SeitenAnatomy of Larynx Lecture 7sallykamareddine100% (1)
- AP Chapter 16BDokument35 SeitenAP Chapter 16BJay Patel100% (1)
- Cardiovascular Physiology Case 9Dokument50 SeitenCardiovascular Physiology Case 9Kim AcostaNoch keine Bewertungen
- CVS Lect 6 Blood Pressure, PathophysiologyDokument13 SeitenCVS Lect 6 Blood Pressure, PathophysiologySherwan R Shal100% (5)
- 29744226: Cerebral Pathophysiology in Extracorporeal Membrane Oxygenation Pitfalls in Daily Clinical ManagementDokument11 Seiten29744226: Cerebral Pathophysiology in Extracorporeal Membrane Oxygenation Pitfalls in Daily Clinical ManagementEward Rod SalNoch keine Bewertungen
- Cardiac Cycle: Prepared By: Mineshkumar Prajapati Roll No: 05 Biomedical Science (2021-22)Dokument21 SeitenCardiac Cycle: Prepared By: Mineshkumar Prajapati Roll No: 05 Biomedical Science (2021-22)minesh prajapatiNoch keine Bewertungen
- Fetal CirculationDokument20 SeitenFetal CirculationMuhyeeSalaIdjadNoch keine Bewertungen
- Circulatory System - Part 2 4-8-14 For BBDokument23 SeitenCirculatory System - Part 2 4-8-14 For BBroman7dbNoch keine Bewertungen
- Left Sided & Right Sided Heart FailureDokument29 SeitenLeft Sided & Right Sided Heart FailureRachelle Ayn100% (3)
- Endocrine Notes - All in One FileDokument182 SeitenEndocrine Notes - All in One FilekjNoch keine Bewertungen
- Heart Blood HistoDokument53 SeitenHeart Blood HistoAnonymous 52lBinNoch keine Bewertungen
- ANS Pharmacology-Cholinergic AgentsDokument55 SeitenANS Pharmacology-Cholinergic AgentsMarc Imhotep Cray, M.D.Noch keine Bewertungen
- Coronary Artery DiseaseDokument33 SeitenCoronary Artery DiseaseAlma Rifa'Ana LiskaNoch keine Bewertungen
- Cardiovascular NotesDokument20 SeitenCardiovascular NotesJus ThomNoch keine Bewertungen
- DELNIDODokument32 SeitenDELNIDOsarwansyahNoch keine Bewertungen
- Bio Rev CardsDokument21 SeitenBio Rev CardsTamannaBhatiaNoch keine Bewertungen
- A Practical Approach To Clinical Echocardiography (2014) (PDF) PDFDokument423 SeitenA Practical Approach To Clinical Echocardiography (2014) (PDF) PDFDiana Loloiu67% (3)
- Medication AdministrationDokument66 SeitenMedication AdministrationMichael Samaniego100% (4)
- NAGA COLLEGE FOUNDATION ANATOMY & PHYSIOLOGY LABORATORYDokument4 SeitenNAGA COLLEGE FOUNDATION ANATOMY & PHYSIOLOGY LABORATORYPado100% (1)
- Circulatory SystemDokument304 SeitenCirculatory Systemyapyihao2100% (1)
- The Heart: Anatomy, Chambers, Circulation & ValvesDokument14 SeitenThe Heart: Anatomy, Chambers, Circulation & ValvesGary Bowen100% (1)
- Cardiac PhysiologyDokument102 SeitenCardiac PhysiologyPeter Larsen100% (1)
- A Brief Look at Renal AnatomyDokument15 SeitenA Brief Look at Renal AnatomyKristina De Peralta Willy100% (1)
- How Bloodis Propelled Throughthe Hum An Ci Rcula To Ry Sy StemDokument5 SeitenHow Bloodis Propelled Throughthe Hum An Ci Rcula To Ry Sy Stemridwan100% (1)
- 250 Questions For The MRCPCH Part 2Dokument250 Seiten250 Questions For The MRCPCH Part 2doctor aabiNoch keine Bewertungen
- Cardiac Output: Dr. AthulyaDokument29 SeitenCardiac Output: Dr. AthulyaamrendraNoch keine Bewertungen
- Describe The Factors Affecting Cardiac OutputDokument6 SeitenDescribe The Factors Affecting Cardiac OutputSis SukarnoNoch keine Bewertungen
- Lecture 6 Cardiovascular: Vascular System - The HemodynamicsDokument70 SeitenLecture 6 Cardiovascular: Vascular System - The HemodynamicsAndreea ŞtefănescuNoch keine Bewertungen
- Cardiovascular PhysiologyDokument49 SeitenCardiovascular PhysiologyAndreea ŞtefănescuNoch keine Bewertungen
- 2 Cardiovascular System: Describe The Systemic Circulation in The Body and Give Its ImportanceDokument28 Seiten2 Cardiovascular System: Describe The Systemic Circulation in The Body and Give Its ImportanceBhavin ChangelaNoch keine Bewertungen
- Cardiovascular Blood VesselsDokument12 SeitenCardiovascular Blood VesselswatuwaitingforNoch keine Bewertungen
- Cvs PathoDokument36 SeitenCvs PathoISRAELNoch keine Bewertungen
- Cardio Vascular SystemDokument22 SeitenCardio Vascular SystemdeborahNoch keine Bewertungen
- Hemodynamics: DR Axelle Saverettiar Mbbs Physiology Department SSR Medical CollegeDokument31 SeitenHemodynamics: DR Axelle Saverettiar Mbbs Physiology Department SSR Medical CollegeÑäd ÉèmNoch keine Bewertungen
- Cardiovascular Physiology: Cardiac Output, Blood Flow ControlsDokument33 SeitenCardiovascular Physiology: Cardiac Output, Blood Flow ControlsLuiz Jorge MendonçaNoch keine Bewertungen
- Chapter 15 - Cardiovascular SystemDokument89 SeitenChapter 15 - Cardiovascular SystemOliver Namyalo100% (1)
- Cardiac Cycle: Mechanical Event and Their Electrical and Clinical CorrelationDokument28 SeitenCardiac Cycle: Mechanical Event and Their Electrical and Clinical Correlationhawas muhammed100% (1)
- Coronary Circulation: Dr. Syma RizwanDokument34 SeitenCoronary Circulation: Dr. Syma RizwanAttiqaQureshiNoch keine Bewertungen
- The Cardiac Cycle: Chapter 19Dokument62 SeitenThe Cardiac Cycle: Chapter 19BishwambherNoch keine Bewertungen
- OutputDokument12 SeitenOutputzenishzalamNoch keine Bewertungen
- Frank-Starling LawDokument5 SeitenFrank-Starling LawNTA UGC-NETNoch keine Bewertungen
- Functional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionDokument186 SeitenFunctional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionBery Agana F. PurbaNoch keine Bewertungen
- Cardiac CycleDokument29 SeitenCardiac CycleRussell Suter100% (1)
- Bio Physio NuggetsDokument141 SeitenBio Physio NuggetsUjjwal PyakurelNoch keine Bewertungen
- The Circulatory System BookletDokument30 SeitenThe Circulatory System BookletTroy CampbellNoch keine Bewertungen
- QOch 11 Studyguide QODokument16 SeitenQOch 11 Studyguide QOHenry HoNoch keine Bewertungen
- L9 PDFDokument22 SeitenL9 PDFMiles HuiNoch keine Bewertungen
- Stroke Volume and Cardiac OutputDokument2 SeitenStroke Volume and Cardiac OutputDennifer MadayagNoch keine Bewertungen
- Mechanical Properties of The Heart IDokument30 SeitenMechanical Properties of The Heart ISeba W WolfNoch keine Bewertungen
- Cardiac Output Regulation and MeasurementDokument18 SeitenCardiac Output Regulation and MeasurementGauravSinghNoch keine Bewertungen
- Renal Physiology: Tubular ProcessingDokument6 SeitenRenal Physiology: Tubular ProcessingUloko ChristopherNoch keine Bewertungen
- FLOWCHARTDokument1 SeiteFLOWCHARTPatrick FormosoNoch keine Bewertungen
- Anatomy and Physiology - Kidney - ForDokument3 SeitenAnatomy and Physiology - Kidney - ForKristelle ModalesNoch keine Bewertungen
- Austin Journal of Clinical CardiologyDokument15 SeitenAustin Journal of Clinical CardiologyAustin Publishing GroupNoch keine Bewertungen
- 3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumDokument3 Seiten3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumAebee Alcaraz100% (1)
- Lect 75control of Tissue Blood FlowDokument23 SeitenLect 75control of Tissue Blood FlowEl FaroukNoch keine Bewertungen
- Circulation NotesDokument2 SeitenCirculation NotesBhkti MittalNoch keine Bewertungen
- Cardio Notes 1Dokument8 SeitenCardio Notes 1Lindsay Grace MandarioNoch keine Bewertungen
- 3.1A-Bolton 2007Dokument10 Seiten3.1A-Bolton 2007Michael SamaniegoNoch keine Bewertungen
- Chess Set-Up and RulesDokument28 SeitenChess Set-Up and RulesMichael SamaniegoNoch keine Bewertungen
- Icatt / ImciDokument8 SeitenIcatt / ImciMichael SamaniegoNoch keine Bewertungen
- MeralcoDokument1 SeiteMeralcoMichael SamaniegoNoch keine Bewertungen
- Threeconversations ExercisesDokument3 SeitenThreeconversations ExercisesMichael SamaniegoNoch keine Bewertungen
- AppraisalDokument32 SeitenAppraisalMichael SamaniegoNoch keine Bewertungen
- Effective LeadershipDokument200 SeitenEffective LeadershipMohd Otibi100% (1)
- Nervous SystemDokument63 SeitenNervous SystemMichael SamaniegoNoch keine Bewertungen
- Chapter 056Dokument19 SeitenChapter 056Michael SamaniegoNoch keine Bewertungen
- L & M in Nursing - ConflictDokument26 SeitenL & M in Nursing - ConflictMichael SamaniegoNoch keine Bewertungen
- Review BulletsDokument19 SeitenReview BulletsMichael SamaniegoNoch keine Bewertungen
- Teenage PregnancyDokument2 SeitenTeenage PregnancyMichael SamaniegoNoch keine Bewertungen
- Case 27 (LC Fix)Dokument14 SeitenCase 27 (LC Fix)galih suharno0% (1)
- The main components and functions of the human circulatory systemDokument1 SeiteThe main components and functions of the human circulatory systemMominul HaqueNoch keine Bewertungen
- Heart and Circulatory SystemDokument5 SeitenHeart and Circulatory SystemBryent GawNoch keine Bewertungen
- Vieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMDokument17 SeitenVieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMFranciscoNoch keine Bewertungen
- Kami Export - Circulatory System Study Questions WorksheetDokument2 SeitenKami Export - Circulatory System Study Questions WorksheetEshrat TushyNoch keine Bewertungen
- Drug Study and LaboratoryDokument13 SeitenDrug Study and LaboratoryGEOMHAI CATBAGANNoch keine Bewertungen
- Cardiac Conduction System Power Point PresentationDokument30 SeitenCardiac Conduction System Power Point PresentationAaya AdelNoch keine Bewertungen
- Kami Export - Hamad Alsayer - Gizmo Circulatory System PDFDokument4 SeitenKami Export - Hamad Alsayer - Gizmo Circulatory System PDFbratlyNoch keine Bewertungen
- 7th Lecture Physics of Cardiovascular System1Dokument12 Seiten7th Lecture Physics of Cardiovascular System1Asfoor gake1Noch keine Bewertungen
- The Cardiovascular System: Prepared by Patty Bostwick-Taylor, Florence-Darlington Technical CollegeDokument125 SeitenThe Cardiovascular System: Prepared by Patty Bostwick-Taylor, Florence-Darlington Technical Collegedomo domoNoch keine Bewertungen
- Anatomical Dissection GuideDokument4 SeitenAnatomical Dissection GuideLidy HigueraNoch keine Bewertungen
- The Circulatory System BookletDokument30 SeitenThe Circulatory System BookletTroy CampbellNoch keine Bewertungen
- Arrows Consele PDFDokument221 SeitenArrows Consele PDFIsai Lara OsoriaNoch keine Bewertungen
- Aortic ValveDokument8 SeitenAortic ValveIfeanyichukwu OgbonnayaNoch keine Bewertungen
- Using The Surface Electrocardiogram To Localization of Idiopathic Ventricular TachycardiaDokument12 SeitenUsing The Surface Electrocardiogram To Localization of Idiopathic Ventricular TachycardiaNavojit ChowdhuryNoch keine Bewertungen
- Anatomy For Beginners 2 - CirculationDokument18 SeitenAnatomy For Beginners 2 - CirculationDefy R PradentyNoch keine Bewertungen
- Basic Principle, Operation and Maintenance: Aqeel Ahmed KhanDokument18 SeitenBasic Principle, Operation and Maintenance: Aqeel Ahmed KhanchanlalNoch keine Bewertungen
- Embryology MCQ Exam: Cardiovascular & Neural DevelopmentDokument6 SeitenEmbryology MCQ Exam: Cardiovascular & Neural DevelopmentTofik MohammedNoch keine Bewertungen
- CIRCULATORY SYSTEMDokument6 SeitenCIRCULATORY SYSTEMJanelleNoch keine Bewertungen
- HS70A Reference Manual En-UsDokument280 SeitenHS70A Reference Manual En-UsVamsi ReddyNoch keine Bewertungen
- Acute and Chronic Response To Exercise in Athletes The "Supernormal Heart No Ovlidar 2017Dokument21 SeitenAcute and Chronic Response To Exercise in Athletes The "Supernormal Heart No Ovlidar 2017Cristian YanezNoch keine Bewertungen
- BioK QQ 6.2 QPDokument2 SeitenBioK QQ 6.2 QPesteban1013264503Noch keine Bewertungen