Beruflich Dokumente
Kultur Dokumente
181 Lec 8
Hochgeladen von
sayednourOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
181 Lec 8
Hochgeladen von
sayednourCopyright:
Verfügbare Formate
OPIATES
Psych 181: Dr. Anagnostaras
Lecture 8
Opioids
Opiates
alkaloids found in the opium poppy
(Papaver somniferum)
[Gk. opion = poppy juice]
Opioids
compounds with opiate-like actions,
including, but not confined to opiates (e.g.,
synthetic, endogenous opioids)
Types of opioids
1. Naturally-
occurring
opium
sap from
opium poppy
Two major active
alkaloids
morphine
codeine
Morphine
Morpheus (god of Dreams)
-son of Hypnos
~ 10% of opium
by weight
HO O OH
N CH3
H
Morphine
Codeine
methylmorphine
~ 0.5% of
opium
2. Semi-synthetics
2. Semi-synthetics
Heroin
diacetylmorphine
addition of two acetyl groups to morphine
~ 10x more potent than morphine
pharmacological effect usually thought to
be identical to morphine
in brain: heroin > morphine
(new data suggest morphine and heroin
may have different actions; 1999)
Semi-synthetic analgesics
Hydromorphone (Dilaudid)
Hydrocodone (Hycodan, Vicodin)
Oxycodone (Percodan, Oxycontin)
3. Synthetics
Phenylpiperidines
Fentanyl china white
Carfentanil (Wildnil)
Meperidine (Demerol)
(MPPP)
Methadone & Congeners
Methadone (Dolophine)
Propoxyphene (Darvon)
Benzomorphans
Pentazocine (Talwin)
N CH3
CH2 C O
O
CH3
Pethidine
(Meperidine)
N
H
(CH3)2
Methadone
CH2 C
O
CH3
H3C
Analgesic potency
Analgesic
potency
Mild to moderate pain
Moderately severe pain
Severe pain
codeine, propoxyphene (Darvon)
meperdine (Demerol)
heroin, hydromorphone (Dilaudid)
"Perc-a-pop"
QuickTime and a
TIFF (Uncompressed) decompressor
are needed to see this picture.
4. Opioid antagonists
naloxone (Narcan)
naltrexone
Suboxone (buprenorphine + naloxone)
5. Endogenous opioids
Enkephalins, endorphins and dynorphins
Morphine & codeine?
History of use - opium
Since recorded history
Ingredient in all
sorts of medicinal
preparations
History of use - morphine
Soldiers disease
History of use
Ads for heroin
Major effects
Analgesia
Relief of pain in absence of impairment in
other sensory modalities
Euphoria - Pleasure
Produce sense of well being, reduce
anxiety, positive feelings
Other effects
Nausea & vomiting
Respiratory depression
Miosis (opposite of mydriasis)
Gastrointestinal effects
Cough Suppression
Motor effects
Effects of repeated administration
Tolerance,
withdrawal &
sensitization
Tolerance and withdrawal
20
10
0
1 4 6 24 72
6 4 24 72 1
8
6
4
2
0
Naltrexone
Morphine
Control
Time (hr)
B
e
h
a
v
i
o
r
a
l
w
i
t
h
d
r
a
w
a
l
s
c
o
r
e
L
C
u
n
i
t
a
c
t
i
v
i
t
y
12.18
Sensitization
Psychomotor stimulant effects
Rewarding effects
(conditioned place preference)
Mechanisms of action
Primary action on opioid receptors located in
CNS +/or periphery
Different effects due to action at
Different receptor subtypes
Receptors in different locations
Endogenous opioids
Production of
Classical transmitter
Peptide transmitter
(1) Synthesizing
enzymes
(2) Storage
vesicles
Axonal transport of
(1) Synthesizing
enzymes
(2) Storage
vesicles
Axonal transport of
(1) Storage
vesicles
Supply by
(1) Axonal transport
+ storage
(2) New synthesis
(3) Reuptake
Release
Release
Supply by
(1) Axonal transport
+ storage
Production of
(1) Peptide
(precursor)
(3) Converting
enzymes
(2) Storage
vesicles
11.4
Post-translational
processing
Translation
Opioid peptide gene families
Three different gene families
Proopiomelanocortin (POMC)
Proenkephalin
Prodynorphin (proenkephalin B)
Proopiomelanocortin
Proenkephalin
Prodynorphin
Signal NH2
Signal NH2
Signal NH2
g-MSH
o-MSH |-LPH CLIP
|-MSH |-Endorphin ACTH
COOH
(Arg6 Gly7 Leu8)
5 6 7 1 2 3 4
COOH
o-Neoendorphin
Dyn A Dyn B
|-Neoendorphin
COOH
Met-enk
(Arg6 Phe7)
Met-enk
12.5
Precursor gene families
Proopiomelanocortin (POMC)
-endorphin
ACTH, melanocortin SH
Proenkephalin -> Enkephalins
met-enkephalin & 2 extended met-enk
leu-enkephalin
Prodynorphine - forms of leu-enkephalin
Dynorphins, A and B
Neoendorphins, and |
Differential distribution
Endorphins
discrete
hypothalamic - endocrine related
Enkephalins and Dynorphins
wide distribution, local circuit and short
axon projections
Opioid
receptors
Opioid receptors
Subtype Preferred Ligand
Mu () Morphine & endorphins
Delta (o) Enkephalins
Kappa (k) Ketocyclazocine & dynorphins
Each subtype has subtypes
Opioid receptors
Cellular actions
G protein coupled receptors
inhibitory
Adenylyl
cyclase
ATP
cAMP
Protein
kinase A
| |
o o
Gs Gi
Opioid receptor
12.4
Negatively-coupled
Role in drug action
Analgesia
Dorsal
horn
Ventral
horn
Dorsal root
(sensory)
Ventral root
(motor)
4.2
Spinal actions
Dorsal horn
of spinal cord
primary pain
afferents
Sensory
neuron
Projection
neuron
Spinal
cord
+
Analgesia
Spinal actions
inhibit incoming pain signals
Opioid receptor
12.8
Analgesia
Supraspinal actions
12.10
Diencephalon
Brain area Descending pathways
Midbrain
Rostroventral
medial
medulla (RVM)
Spinal cord
NR NP
DLPT LC
PAG
Dorsal horn
PVG
Analgesia
Supraspinal actions
12.10
Diencephalon
Brain area Descending pathways
Midbrain
Rostroventral
medial
medulla (RVM)
Spinal cord
NR NP
DLPT LC
PAG
Dorsal horn
PVG
Stimulation >
analgesia and
inhibit cells in
dorsal horn
Analgesia
Supraspinal actions
12.10
Diencephalon
Brain area Descending pathways
Midbrain
Rostroventral
medial
medulla (RVM)
Spinal cord
NR NP
DLPT LC
PAG
Dorsal horn
PVG
Lesion > block analgesia
to systemic or local
morphine
Analgesia
Supraspinal actions
1 sites seem most important
Specific blockade of 1 shifts dose-
response curve for morphine analgesia up
to 12 fold to right
Analgesia
Heroin vs. Morphine
difference pharmacokinetic?
recent evidence for different receptors
- MOR-1 knockouts
Analgesia - MOR1 knockouts
A
n
a
l
g
e
s
i
a
(
%
)
Schuller et al., Nature Neurosci. (1999)
heroin > 6-acetyl-
morphine in vivo
Morphine, but
not heroin,
analgesia
abolished in
Mor1 knockout
mice
Reinforcing effects
Reinforcing effects
All classical opioid drugs of abuse have a
preference for sites (e.g., morphine, heroin,
methadone, fentanyl etc.)
o may contribute, but little known
k compounds are not self-administered
psychomimetic and aversive in humans
Opioid/DA interaction
Intra-VTA opioid support SA and CPP
DA antagonist or 6-OHDA lesion impair SA
DA antagonist into VTA or ACC impair SA
Mechanism
compounds:
Increase DA cell firing
Increase DA release in ACC
Accompanied by locomotor activation
Model for reinforcing effects
Site of action
VTA accumbens DA system
DA
|-endorphin
GABA
Ventral
tegmental
area (VTA)
Nucleus
accumbens
Ventral
pallidum
Mesolimbic
dopamine
u
12.16
Disinhibition
compounds
Decrease DA cell firing
Decrease DA release
Decrease locomotion
Respiratory depression
2 sites?
Specific 1 antagonist (naloxonazine) shifts
analgesia dose - response curve for morphine
to right
Not shift dose-response curve for:
elevation of pCo2
depression of pO2
Respiratory neurons in medulla in region of n.
solitary tract
Gastrointestinal effects
and k sites
In stomach, small and large intestine
Decreased motility
Common bioassay > ability to inhibit
intestinal contractions
MOR Knockouts
Morphine has affinity for all opioid receptor
subtypes (much stronger for mu)
Evidence for site of action from
pharmacological experiments with drugs that
may act at multiple sites
Which effects due to action at which receptpr
subtypes?
MOR Knockouts (MOR -/-)
Morphine effect
Spinal analgesia Abolished
Supraspinal analgesia Abolished
Reward Abolished
Withdrawal Abolished
Respiratory depression Abolished
Inhibition GI motility Abolished
Psychoactivating effect Abolished
(all effects maintained in DOR-/- and KOR-/-)
Brigitte L. Kieffer, Opioids: first lessons from knockout mice,
Trends in Pharmacological Sciences, 20 (1999) 19-26.
The Politics of Pain
and Pain Management
Introduction
Prevalence
Pain accounts for 80% of all medical
complaints (30% debilitated at some time)
Pain is patient's #1 reason why they fear
disease
Pain affects 90% of patients with terminal
disease (50% of ambulatory patients)
Obstacles for treatment
Fearpatient, prescriber
Social and Legal obstacles
Lack of education
Political and Social Obstacles
Overstated abuse potential of opiate drugs
has been a serious obstacle to pain
treatment
Pain patients have been a casualty of the
war on drugs
No field to study pain until the 1970s
(opiate receptor cloned)
Very little formal training on pain
management as part of medical school
curriculum (often 1 hour)
Politics of pain
Most doctors misinformed about the
addictiveness of therapeutic opiates (e.g.,
vicodin v heroin or significance of routes
of administration in addiction)
Even when habit-forming this addiction
outweighed thinking about patient's
quality of life.
Fear of reprisals on license by DEA a major
issue
Drug companies avoided new opiates
Politics of pain
Pain patients looked down upon for
complaining about pain (especially chronic
pain)
Pain treated as a valuable diagnostic indicator
by doctors "don't want to cover up the pain"
(even chronic neuropathic pain)
Politics of pain
Revolution in pain management had multifaceted
roots- began in 1970s
conference on Pain formed unified field to
study Pain, 1977 - American Pain Society
(www.ampainsoc.org) 28-3600
discovery of endogenous opioids
activism by Bonica, Liebeskind, etc.
revolt by San Francisco cancer doctors
Centers for Pain Management Policy (e.g.,
Wisconsin)
Politics of pain
Several states enacted legislation to protect
doctors and patients (e.g., California's "pain
patients bill of rights")
Softening of war on drugs by Clinton
administration
Doctor's take back their rights
(Doctor's make medical decisions)
Medical marijuana acts
Politics of pain
In cancer was clear need to treat pain
outweighed any addiction
It became clear most pain patients either
didn't become addicted at all or developed
mild dependence
Pain management clinics have appeared all
over the place (including Emory)
Still many obstacles to adequate pain
management, e.g., patient access is still very
low and too many drug side-effects
Many obstacles remain
Still difficult for patients to get treatment
triplicate prescriptions
cannot be called in
cannot be refilled
policing by DEA
few experts in pain
strong slow-release drugs are expensive
pain patients often poor, uninsured, and
cannot travel or work
What is Pain?
Medical Definition
Pain is an unpleasant sensory and emotional
experience associated with actual or potential
tissue damage or described in terms of such
damage
International Association for the Study of Pain,
1979
Operative Definition
Pain is whatever the experiencing person says it
is, existing whenever he/she says it does.
patient's appearance can be very deceptive
What is Pain?
Current definitions of pain don't work well
for:
children who can't speak or even older
ones who can't express themselves well
those who are mute or mentally ill
animals
those who hide their pain
emphasis on pain behaviors emerging
Reflection tells me that I am so far from
being able to define pain, of which I
here write, that the attempt could serve
no useful purpose. Pain, like similar
subjective things, is known to us by
experience and described by
illustration.
Pain is a perception, nociception
is the sensation
Thomas Lewis. Pain.
New York, The MacMillan Company, 1942.
NOCICEPTION
PAIN
SUFFERING
PAIN BEHAVIOR
Definitions
Nociception: Potentially tissue
damaging thermal, mechanical or
chemical energy impinging upon
specialized nerve endings of A-o and C
fibers.
Pain: Perceived nociceptive input to
the nervous system.
Pain can occur without nociception!
Pain syndromes without
nociception
Thalamic syndrome Phantom limb pain
Tic douloureux Arachnoiditis
Postherpetic neuralgia Atypical facial pain
Postparaplegia pain Nerve root avulsion pain
Postthoracotomy pain Neuropathic pain
Pain is a major cause of
suffering!
Suffering: Negative affective
response generated in higher nervous
system regions in response to pain and
other situations including fear, anxiety,
isolation, depression, etc.
Pain behavior
All forms of behavior generated by
the individual that are commonly
understood to reflect the presence
of nociception; for example,
grimacing, saying ouch, limping,
lying down, taking medicines,
seeking health care, refusal to work.
Types of Pain
Nociceptive Pain
Stimulation of somatic and visceral
peripheral nociceptors by stimuli that
damage tissue
Neuropathic Pain
Pain resulting from non-inflammatory
dysfunction of the peripheral/central
nervous system in the absence of
stimuli
Neuropathic Pain
Prevalence
General population 0.6-1%
Causes
Compression/infilitration of nerves by:
Tumors
Nerve Trauma secondary to procedures
Nervous System Injury
E.g., phantom-limb pain, neuralgia
back injury, post-surgical pain
Types of Pain
Transient Pain
Studied extensively in man and animals
Does not involve tissue damage
Activation of nociceptors in resting state
Not clinically relevant, save for procedural
pain such as venipuncture, LP
Types of Pain
Acute Pain
Activation of nociceptors in region of
tissue damage
Nociceptor function is altered by tissue
changes
Healing processes can eliminate tissue
damage; nociceptor function returns to
baseline
Types of Pain
Chronic Pain
Activation of nociceptors in region of tissue
damage
Nociceptor function is altered by tissue
damage; CNS adapts permanently
Body cannot heal injury, or damage to
nervous system
Organic cause unknown and untreatable
(often iatrogenic)
Chronic pain is a special problem
Chronic Pain
Associated with a social stigma
people expect you to get over illness
"get back to work"
associated with a lot of hiding of pain
Debilitating and depressing producing lots of
psychological problems
Especially poorly treated
lack of expertise and desire to treat by docs
lack of effective treatment
Afferent pain transmission
Afferent fibers go to the CNS transmitting
nociceptive message from trauma to
dorsal horn of spinal cord
A alpha, A beta, A gamma, A delta, B, or C
Nociceptive transmission takes place in
the A delta fibers (well-localized pain); C
fibers (persistent pain)
Transduction of nociception
Conversion of stimuli into electrical action
potential
What types of stimuli?
Heat or cold (e.g. radiation damage)
Pressure (e.g. tumor infiltration into
bone)
Chemical (e.g. chemotherapy)
Peripheral Nociceptors
What is a nociceptor?
Not spontaneously active
Level of stimulation must exceed threshold
Sensitization produces hyperalgesia
Tissue damage changes the sensitivity
Sensitization is manifested as:
Decreased threshold
Increased intensity-prolonged firing
Spontaneous activity
Pain Theories and
Pathways
Spinal cord transmissionspinothalamic
tract carries pain impulses; the lateral
pathway (sharp, localized pain), the vental
pathway (dull, nonlocalized pain)
Pathways merge in thalamus and connect in
cortex
Ant Cingulate cortexpain perception area
Types of Peripheral Nerve Fibers
A Fibers (Fast Transmission)
Alpha - Proprioception (Muscles & Joints)
Beta - Mechanoreception (Cutaneous
Tissue)
Delta - Primary nociceptive neurons
C Fibers (Slow Transmission)
Primary nociceptive neurons
Neuronal Activities in Normal
States
Stimulus Pri Afferent Sensation
Low Intensity A-Beta Innocuous
High Intensity A-Delta/C Pain
(nociception)
Neuronal Activities in Pain States
Stimulus Pri Afferent Sensation
Low Intensity A-Beta Pain
(allodynia)
High Intensity A-Delta/C Hyperalgesia
Pain Theories and
Pathways
Clusters of opiate receptors throughout
ascending and descending pain pathways
endogenous opioids also in brain
Opiate receptors-- (1 and 2), o (delta),
k (kappa), (o. sigma and c.epsilon)
1 are primarily responsible for analgesic
effects (but maybe also o. k. c)
Opioid (Narcotic)
analgesics
Morphine
Meperidine (Demerol)
Codeine (Tylenol-3)
Hydromorphone (Dilaudid)
Hydrocodone and acetaminophen (Vicodin)
Methadone (Dolophine)
Fentanyl, alfentanil, sufentanil, remifentanil
(e.g., sublimaze & duragesic)
Oxycodone (Percodan)
Oxycodone and acetaminiphen (Percocet)
Propoxyphene (Darvon)
Opioids
Inhibit the transmission of pain impulses in
sensory pathways in the spinal cord
Reduce cortical responses all over the brain
Alter behavioral responses to pain
Tolerance & dependence may develop, not
necessary a sign of abuse or addiction
Opioids
Despite reports of abuse vast majority of
pain patients use chronically without
addiction or dependence
Long-acting much better than short-acting
(prevents on-off and sensitization)
ATC (around-the-clock) preferable to PRN
Non-narcotic analgesics
Salicylates (aspirinhistorically there
were several derivatives)
Aniline derivatives (Tylenol-
acetaminophen)
Non-steroidal anti-inflammatory
agents (NSAIDS)
NSAIDs
COX 1 & COX 2 inhibitors
ibuprofen (Motrin, Advil)
naproxen (Aleve)
diclofenac (Voltaren)
indomethacin (Indocin)
ketorolac (Toradol)
sulindac (Clinoril)
mefanamic (Ponstel)
piroxicam (Feldene)
flurbiprofen (Ansaid)
ketoprofen (Orudis)
Selective COX 2
inhibitors
celocoxib (Celebrex)
rofecoxib (Vioxx)
valdecoxib (Bextra)
Celebrex & Vioxx
Aspirin and most commonly used NSAIDs
nonselectively inhibit COX 1 and COX 2
COX 2 agents have a lower incidence of
the ulcerogenic side effects (they increase
the risk of heart attack, stroke, and
clotting disorders, however)
Identified by genetic screen of aspirin
side effects include headache
Therapeutic effects of
NSAIDs
Antipyretic
Analgesic--low to moderate pain intensity; lack
unwanted CNS effects of opioids
Antiinflammatory
Side effects still include ulcers, blood-thinning.
and sensitivity
Only aspirin proven to show anti-MI effects and
still in its own category
Aniline derivatives
Acetaminophen (Tylenol)
Centrally mediated hypothalamic
stimulation to alter pain perception
Clinical useanalgesic, weak antipyretic
No action as anti-inflammatory
Overdosage is associated with hepatic
necrosis/must be treated within 10 hours -
SERIOUS PROBLEM
Pain adjuvants
Tricyclic antidepressants and SSRIs
Anticonvulsants
Corticosteroids
Muscle relaxants
Capsaicin
Local anesthetics (lidocaine, benzocaine)
Non-pharmacologic therapies
NMDA receptor antagonists (ketamine, DXM, CPP)
Patient-controlled analgesia/epidural analgesia
Clinical applications
Review history (drug abuse, allergy)
Assess level of function and pain level
Monitor patient pain relief, tolerance
Level of function after treatment
Surgical treatment of chronic pain is a last
resort (exception = pumps, stimulators,
rhizotomy), usually makes things worse
Das könnte Ihnen auch gefallen
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Manual Mmpi 2 PDFDokument3 SeitenManual Mmpi 2 PDFSana Sajid17% (12)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Basavaraj-Colour Therapy PDFDokument144 SeitenBasavaraj-Colour Therapy PDFTanuku Net86% (14)
- 4 Hypovolemic ShockDokument21 Seiten4 Hypovolemic Shocksayednour100% (4)
- What Robotic Re-Embodiment Reveals About Virtual Re-EmbodimentDokument17 SeitenWhat Robotic Re-Embodiment Reveals About Virtual Re-Embodimentherac12Noch keine Bewertungen
- Fluid Electrolytes and Acid Base BalanceDokument108 SeitenFluid Electrolytes and Acid Base BalancesayednourNoch keine Bewertungen
- Basics of Laser Orthopedic ViewDokument24 SeitenBasics of Laser Orthopedic ViewsayednourNoch keine Bewertungen
- Assessment of Suitability For Lung Resection: Gerard Gould FRCA Adrian Pearce FRCADokument4 SeitenAssessment of Suitability For Lung Resection: Gerard Gould FRCA Adrian Pearce FRCAsayednourNoch keine Bewertungen
- Anesthesia in The FutureDokument11 SeitenAnesthesia in The FuturesayednourNoch keine Bewertungen
- An Overview of Therapeutic Plasma ExchangeDokument65 SeitenAn Overview of Therapeutic Plasma ExchangesayednourNoch keine Bewertungen
- General Anesthesia For Cesarean SectionDokument33 SeitenGeneral Anesthesia For Cesarean Sectionsayednour100% (2)
- AnestheticsDokument34 SeitenAnestheticssayednourNoch keine Bewertungen
- 166 Serotonin SyndromeDokument5 Seiten166 Serotonin SyndromesayednourNoch keine Bewertungen
- 1 Plasmapheresis - 1Dokument61 Seiten1 Plasmapheresis - 1sayednour100% (1)
- Plasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?Dokument4 SeitenPlasma Exchange For Heparin-Induced Thrombocytopenia: Is There Enough Evidence?sayednourNoch keine Bewertungen
- Adrenal CrisisDokument27 SeitenAdrenal CrisissayednourNoch keine Bewertungen
- Nitric Oxide An Overview: Salwa Hassan Teama M.D. NCI. Cairo UniversityDokument31 SeitenNitric Oxide An Overview: Salwa Hassan Teama M.D. NCI. Cairo Universitysayednour100% (1)
- Review Mechanisms of Glucocorticoid-Induced Myopathy: O Schakman, H Gilson and J P ThissenDokument10 SeitenReview Mechanisms of Glucocorticoid-Induced Myopathy: O Schakman, H Gilson and J P ThissensayednourNoch keine Bewertungen
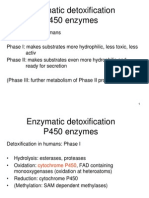
- Enzymatic Detoxification P450 EnzymesDokument22 SeitenEnzymatic Detoxification P450 EnzymessayednourNoch keine Bewertungen
- Cohort StudyDokument31 SeitenCohort Studysayednour50% (2)
- Tony Chang, MD Tuesday Conference September 6, 2005Dokument75 SeitenTony Chang, MD Tuesday Conference September 6, 2005sayednourNoch keine Bewertungen
- Developmental Genetics and Pharmacogeneticsdoc4301Dokument8 SeitenDevelopmental Genetics and Pharmacogeneticsdoc4301sayednourNoch keine Bewertungen
- 8 Plasma Derivatives ProductsDokument12 Seiten8 Plasma Derivatives ProductssayednourNoch keine Bewertungen
- 185 Anaesthesia in Pregnancy For Non Obstetric SurgeryDokument9 Seiten185 Anaesthesia in Pregnancy For Non Obstetric SurgeryaangrohmananiaNoch keine Bewertungen
- Hennebert's SignDokument3 SeitenHennebert's SignatmhyaNoch keine Bewertungen
- Selina Solutions For Class 10 Biology Chapter 11 Sense OrgansDokument19 SeitenSelina Solutions For Class 10 Biology Chapter 11 Sense OrgansParardha DharNoch keine Bewertungen
- Intelligence Testing On WISCDokument60 SeitenIntelligence Testing On WISCSangeeta ParabNoch keine Bewertungen
- Coordination & Response 5 QP PDFDokument6 SeitenCoordination & Response 5 QP PDFJeffrey PiggottNoch keine Bewertungen
- Neuroimaging Advances in Holoprosencephaly: Re Ning The Spectrum of The Midline MalformationDokument13 SeitenNeuroimaging Advances in Holoprosencephaly: Re Ning The Spectrum of The Midline Malformationfamiliesforhope100% (1)
- Bipolar PowerpointDokument10 SeitenBipolar PowerpointRAYMIND MIRANDANoch keine Bewertungen
- CHAPTER 1the Mind-Brain RelationshipDokument23 SeitenCHAPTER 1the Mind-Brain RelationshipRain Simonette GuanNoch keine Bewertungen
- CgassDokument3 SeitenCgassComan CristinaNoch keine Bewertungen
- Neurofilament Light Chain Gaetani2019Dokument12 SeitenNeurofilament Light Chain Gaetani2019eastareaNoch keine Bewertungen
- Nursing Care PlanDokument3 SeitenNursing Care Plansarah hanaNoch keine Bewertungen
- C9apstudy GuideDokument37 SeitenC9apstudy GuidejqtdNoch keine Bewertungen
- 단어시험 (Day 4~6)Dokument15 Seiten단어시험 (Day 4~6)qkrwldnjs0314Noch keine Bewertungen
- Thigmonasty 1Dokument3 SeitenThigmonasty 1BeaNoch keine Bewertungen
- Neuropsychology 2 BetDokument11 SeitenNeuropsychology 2 BetMike TemboNoch keine Bewertungen
- SSR Disability Services CentreDokument3 SeitenSSR Disability Services CentreIrshaad Ally Ashrafi GolapkhanNoch keine Bewertungen
- CIDP UpToDateDokument7 SeitenCIDP UpToDatesvd2009Noch keine Bewertungen
- Full Test Bank For Essentials of Psychology 7Th Edition Douglas A Bernstein PDF Docx Full Chapter ChapterDokument36 SeitenFull Test Bank For Essentials of Psychology 7Th Edition Douglas A Bernstein PDF Docx Full Chapter Chapterbethmcneilysgbzqkpnw100% (11)
- Philip Kosovrasti - Resource GuideDokument9 SeitenPhilip Kosovrasti - Resource Guideapi-340370776Noch keine Bewertungen
- Midterms Reviewer Ana 2Dokument8 SeitenMidterms Reviewer Ana 2Ais WallensteinNoch keine Bewertungen
- Blue BrainDokument19 SeitenBlue BrainDanielle HoltNoch keine Bewertungen
- Anatomy of The Eye WorksheetDokument1 SeiteAnatomy of The Eye WorksheetIrfan ArifNoch keine Bewertungen
- Morning Report: Departement of Neurology m28 Muhammadiyah Lamongan HospitalDokument19 SeitenMorning Report: Departement of Neurology m28 Muhammadiyah Lamongan HospitalratnaNoch keine Bewertungen
- Dopamine D3 Receptor - A Neglected Participant in Parkinson Disease Pathogenesis and Treatment?Dokument45 SeitenDopamine D3 Receptor - A Neglected Participant in Parkinson Disease Pathogenesis and Treatment?Daniel TorresNoch keine Bewertungen
- PTSD and Cognitive Processing Therapy Presented by Patricia A. Resick, PHD, AbppDokument28 SeitenPTSD and Cognitive Processing Therapy Presented by Patricia A. Resick, PHD, AbppDardo Arreche100% (2)
- A Metacognitive Therapy For Anxiety Disorders - Buddhist Psychology Applied (2002 Cognitive and B PDFDokument7 SeitenA Metacognitive Therapy For Anxiety Disorders - Buddhist Psychology Applied (2002 Cognitive and B PDFclaudiaghergariNoch keine Bewertungen
- Pathological Demand Avoidance and The DSM-5: A Rebuttal To Judy EatonDokument4 SeitenPathological Demand Avoidance and The DSM-5: A Rebuttal To Judy EatonyeyesNoch keine Bewertungen
- Vielight Inventors Notes For Neuro Alpha and Neuro Gamma 2017Dokument17 SeitenVielight Inventors Notes For Neuro Alpha and Neuro Gamma 2017arexixNoch keine Bewertungen