Beruflich Dokumente
Kultur Dokumente
Thoracentesis
Hochgeladen von
Marivic DianoOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Thoracentesis
Hochgeladen von
Marivic DianoCopyright:
Verfügbare Formate
Prepared by: Heron Jayson E.
Bayanin BSN 3-1
Thoracentesis, Thoracocentesis or pleural tap, is an invasive procedure to remove fluid or air from the pleural space for diagnostic or therapeutic purposes. A cannula, or hollow needle, is carefully introduced into the thorax, generally after administration of local anesthesia.
Pleura Pleural space
Pneumonia,Cancer, or Congestive heart failure may cause excessive fluid to develop (pleural effusion).
Recent Surgery and Tuberculosis
To provide pleural fluid specimens to determine the cause and nature of pleural effusion To provide symptomatic relief with large pleural effusion.
Most common reasons for doing a thoracentesis : 1. New Pleural Effusion
2. Infection
3. Cancer 4. Comfort
Transudate Pleural fluid to serum total protein ratio of less than 0.5 Low white blood cell (WBC)count Low lactate dehydrogenase (LDH) enzyme level Low protein level
Transudate Congestive heart failure Nephrotic syndrome Hypoalbuminemia Cirrhosis Atelectasis trapped lung Peritoneal dialysis Superior vena cava obstruction
Exudate any fluid that filters from the circulatory system into lesions or areas of inflammation. water and the dissolved solutes of the main circulatory fluid .
Exudate hemorrhage Infection Inflammation Malignancy Iatrogenic Connective tissue disease Endocrine disorders Lymphatic disorders vs Constrictive pericarditis
Amylase greater than 160 Somogy units in the pleural fluid. acute or chronic pancreatitis pancreatic pseudocyst that has dissected or ruptured into the pleural space cancer or esophageal rupture.
Glucose less than 50% of normal serum value. rheumatoid effusion.The levels are characteristically low (<15 mg/dL). lupus effusion bacterial empyema malignancy tuberculosis esophageal rupture (Boerhaave syndrome)
Pleural Fluid pH Normal pleural fluid - pH 7.60. Below 7.30 with normal arterial blood pH has the same differential diagnosis as low pleural fluid glucose.
Triglyceride and Cholesterol Chylothorax (fluid from lymph vessels leaking into the pleural cavity) A triglyceride level over 110 mg/dl and the presence of chylomicrons indicate a chylous effusion. The appearance is generally milky but can be serous. Rupture of the thoracic duct, a result of trauma or malignancy (such aslymphoma).
Cell Count and Differential Number of WBC indication of infection. Number of RBC obvious sign of bleeding Culture and Stains A Gram stain may give a rough indication of the causative organism. A Ziehl-Neelsen stain may identify tuberculosis or other mycobacterial diseases.
Cytology Tool in identifying effusions due to malignancy. The most common causes for pleural fluid are lung cancer,metastasis and pleural mesothelioma. The latter often presents with an effusion..
PreProcedure Care
Verify a signed informed consent for the procedure. Assess knowledge and understanding of the procedure and its purpose. Preprocedure fasting or sedation is not required.
PreProcedure Care
Administer a cough suppressant if indicated. Obtain a thoracentesis tray, sterile gloves, injectable lidocaine, povidone-iodine,dressing supplies, and an extra overbed table or mayo stand.
Position the client upright,leaning forward with arms and head supported on an anchored overbed table.
PreProcedure Care
Inform the client that although local anesthesia prevents pain as the needle is inserted, a sensation of pressure may be felt.
PostProcedure Care
Monitor pulse,color,oxygen saturation,and other signs during thoracentesis.
Apply a dressing over the puncture site, and position on the unaffected side for 1 hour.
Label obtained specimen with name, date, source, and diagnosis; send specimen to the laboratory for analysis.
PostProcedure Care
During the first several hours after thoracentesis, frequently assess and document vital signs; oxygen saturation; respiratory status, including, respiratory excursion, lung sounds, cough, or hemoptysis; and puncture site for bleeding or crepitus. Obtain a chest X-ray.
Normal activities generally can be resumed after 1 hour if no evidence of pneumothorax or other complication is present.
1. Ascertain in advance that a chest x-ray has been ordered and completed and the consent form has been signed. 2. Assess the patient for allergy to the local anesthetic to be used. 3. Administer sedation if prescribed.
4. Inform the patient about the nature of the procedure and a. the importance of remaining immobile b. pressure sensations to be experienced. c. that minimal discomfort is anticipated after the procedure.
5. Position the patient comfortably with adequate supports. If possible, place the patient upright or in one of the following positions: a. Sitting on the edge of the bed with the feet supported and arms and head on a padded overthe-bed table. b. Straddling a chair with arms and head resting on the back of the chair. c. Lying on the unaffected side with the head of the bed elevated 30 to 45 degrees if unable to assume a sitting position.
6. Support and reassure the patient during procedure. a. Prepare the patient for the cold sensation of skin germicide solution and for a pressure sensation from infiltration of local anesthetic agent. b. Encourage the patient to refrain from coughing.
7. Expose the entire chest. The site for aspiration is visualized by chest x-ray and percussion. If fluid is in the pleural cavity, the thoracentesis site is determined by the chest x-ray, ultrasound scanning, and physical findings, with attention to the site of maximal dullness on percussion.
8. The procedure is performed under aseptic conditions. After the skin is cleansed, the physician uses a small-caliber needle to inject a local anesthetic slowly into the intercostal space.
9. The physician advances the thoracentesis needle with the syringe attached. When the pleural space is reached, suction may applied with the syringe. a. A 20-mL syringe with a three-way stopcock is attached to the needle( one end of the adater is attached to the needle and the other to the tubing leading to a receptacle that receives the fluid being aspirated. b. If a considerable quantity of fluid is removed the needle is held in space on the chest wall with a small hemostat
10. After the needle is withdrawn, pressure is applied over the puncture site and a small, airtight, sterile dressing is fixed in place. 11. Advise the patient that he or she will be on bed rest and a chest x-ray will be obtained after thoracentesis. 12. Record the total amount of fluid withdrawn from the procedure and document the nature of the fluid, its color and viscosity. If indicated, prepare samples of fluid for laboratory evaluation, A specimen container with formalin may be needed for a pleural biopsy.
13. Monitor the patient at intervals for increasing respiratory rate; asymmetry in respiratory movement; faintness; vertigo; tightness in chest; uncontrollable cough; blood-tinged; frothy mucus; a rapid pulse; and signs of hypoxemia.
1. Posteroanterior and lateral chest x-ray films are used to localize fluid and air in the pleural cavity and to aid in determining the puncture site. When fluid is loculated (isolated in a pocket of pleural fluid), ultrasound scans are performed to help select the best site for needle aspiration. 2. If the patient is allergic to the initially prescribed anesthetic, assessment findings provide an opportunity to use a safer anesthetic.
3. Sedation enables the patient to cooperate with the procedure and promotes relaxation. 4. An explanation helps to orient the patient to the procedure, assists the patient to mobilize resources, and provides an opportunity to ask questions and verbalize anxiety.
5. The upright position facilitates the removal of fluid that usually localizes at the base of the thorax. A position of comfort helps the patient to relax. 6. Sudden and unexpected movement, such as coughing, by the patient can traumatize the visceral pleura and lung. 7. If air is in the pleural cavity, the thoracentesis site is usually in the second or third intercostals space in the midclavicular line because air rises in the thorax.
8. An intradermal wheal is raised slowly; rapid injection causes pain. The parietal pleura is very sensitive and should be well infiltrated with anesthetic before the physician passes the thoracentesis needle through it. 9. Use of thoracentesis needle allows proper insertion.
a. When a large quantity of fluid is withdrawn a three-way stopcock serves to keep air from entering pleural cavity. b. The hemostat steadies the needle on the chest wall. Sudden pleuritic chest pain or shoulder pain may indicate that the needle point is irritating the visceral or the diaphragmatic pleura.
10. Pressure help to stop bleeding, and the airtight dressing protects the site and prevents air from entering the pleural cavity. 11. A chest x-ray verifies that there is no pneumothorax.
12. The fluid may be clear, serous, bloody, purulent, etc. 13. Pneumothorax, tension pneumothorax, subcutaneous emphysema, and pyrogenic infection are complications of a thoracentesis. Pulmonary edema or cardiac distress ca occur after a sudden shift in mediastinal contents when large amounts of fluid are aspirated.
Das könnte Ihnen auch gefallen
- THORACENTESISDokument14 SeitenTHORACENTESISKatherine Jeanne RosalNoch keine Bewertungen
- Checklist Thoracentesis (Charisse) ADokument6 SeitenChecklist Thoracentesis (Charisse) ARonel UsitaNoch keine Bewertungen
- ThoracentesisDokument9 SeitenThoracentesisPatricia G ChiuNoch keine Bewertungen
- Thoracentesis Is Also Known As Pleural Fluid AnalysisDokument3 SeitenThoracentesis Is Also Known As Pleural Fluid AnalysisJ.r. MercadoNoch keine Bewertungen
- ThoracentesisDokument12 SeitenThoracentesisAnusha Verghese0% (1)
- Thoracentesis ProDokument6 SeitenThoracentesis ProRaidis PangilinanNoch keine Bewertungen
- Thoracentesis: ProcedureDokument12 SeitenThoracentesis: Procedurealbert manievoNoch keine Bewertungen
- Ebstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandEbstein Anomaly, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- NURSING CARE OF ADULTS II: Passbooks Study GuideVon EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNoch keine Bewertungen
- Med Surg Chapter 1Dokument2 SeitenMed Surg Chapter 1Judy072100% (1)
- Interactive Quiz: Deal or No DealDokument7 SeitenInteractive Quiz: Deal or No DealShaira Jean GeminaNoch keine Bewertungen
- Chest Tube ModuleDokument37 SeitenChest Tube ModuleEdison Reyes100% (1)
- ECG Reading & InterpretationDokument52 SeitenECG Reading & InterpretationRoy Francis B. CaspeNoch keine Bewertungen
- Group 5 - Hemodialysis - Chronic Kidney FailureDokument31 SeitenGroup 5 - Hemodialysis - Chronic Kidney FailureKimberly Abella CabreraNoch keine Bewertungen
- Chapter 2 SampleDokument38 SeitenChapter 2 SampleLospa Stocazzo100% (1)
- Fundamentals Modules 1-10 Study GuidesDokument278 SeitenFundamentals Modules 1-10 Study GuidesNurseAmy100% (1)
- Assessment of The Thorax and Lungs 2014Dokument9 SeitenAssessment of The Thorax and Lungs 2014alphabennydelta4468Noch keine Bewertungen
- Icu Equipments BY: Presented Bhupender Kumar MehtoDokument35 SeitenIcu Equipments BY: Presented Bhupender Kumar Mehtobhupendermehto012Noch keine Bewertungen
- M.SC Nursing Syllabus Revised 2018 - 19-23082019-1Dokument344 SeitenM.SC Nursing Syllabus Revised 2018 - 19-23082019-1Divya ToppoNoch keine Bewertungen
- 18 NCP Ileal ConduitDokument11 Seiten18 NCP Ileal ConduitICa MarlinaNoch keine Bewertungen
- M Digestion" Absorption" EliminationDokument104 SeitenM Digestion" Absorption" EliminationChristine Carol FilipinasNoch keine Bewertungen
- Physical Assessment (Ippa)Dokument14 SeitenPhysical Assessment (Ippa)Barbara HsuNoch keine Bewertungen
- Nursing Informatics: de Lara, Denise Dominique M. Quiamco, Precious Diane S. RNDokument113 SeitenNursing Informatics: de Lara, Denise Dominique M. Quiamco, Precious Diane S. RNPrecious Diane QuiamcoNoch keine Bewertungen
- Nursing Management in Abdominal SurgeryDokument19 SeitenNursing Management in Abdominal Surgeryejguy7777100% (2)
- Perioperative Nursing CareDokument47 SeitenPerioperative Nursing CareTessa Bagus AriyantoNoch keine Bewertungen
- Nursing Care of Clients With Upper Gastrointestinal Disorder 1Dokument149 SeitenNursing Care of Clients With Upper Gastrointestinal Disorder 1Andrea TylerNoch keine Bewertungen
- Naso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringDokument12 SeitenNaso Orogastric Tube Guideline For The Care of Neonate Child or Young Person RequiringmeisygraniaNoch keine Bewertungen
- Care of Pediatric Client With Dermatologic DisorderDokument3 SeitenCare of Pediatric Client With Dermatologic DisorderAraw GabiNoch keine Bewertungen
- Fundamentals of Nursing 1Dokument6 SeitenFundamentals of Nursing 1Ruel M. BersabeNoch keine Bewertungen
- Case Study PeriopDokument3 SeitenCase Study PeriopSteve25% (4)
- Pharamacology Notes 3Dokument7 SeitenPharamacology Notes 3Martinet CalvertNoch keine Bewertungen
- Assessment of Respiratory Function Chpt.20Dokument32 SeitenAssessment of Respiratory Function Chpt.20Maricar RosasNoch keine Bewertungen
- Medication Administration - Parenteral RouteDokument3 SeitenMedication Administration - Parenteral RouteRhiz Antonio67% (3)
- GROUP 3 - CASE STUDY - TraumaDokument5 SeitenGROUP 3 - CASE STUDY - TraumaDinarkram Rabreca EculNoch keine Bewertungen
- Nursing ReviewerDokument10 SeitenNursing ReviewerChristine Hernandez100% (1)
- Patient Position PDFDokument60 SeitenPatient Position PDFDana RoxanaNoch keine Bewertungen
- Medical Surgical NursingDokument66 SeitenMedical Surgical Nursing04eden100% (3)
- 2022 Level 4 Intravenous TherapyDokument65 Seiten2022 Level 4 Intravenous TherapyBokNoch keine Bewertungen
- Cardiac SurgeryDokument35 SeitenCardiac SurgeryxxxNoch keine Bewertungen
- Pericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerDokument2 SeitenPericarditis NCLEX Review: Serous Fluid Is Between The Parietal and Visceral LayerlhenNoch keine Bewertungen
- Ethico Legal of Perioperative NursingDokument19 SeitenEthico Legal of Perioperative NursingAziil Liiza100% (1)
- ABC Dictionary of Urinary SystemDokument26 SeitenABC Dictionary of Urinary Systemaby_romero9750% (2)
- ChestTubes CareDokument21 SeitenChestTubes CareAnusha VergheseNoch keine Bewertungen
- Management of Arterial LineDokument16 SeitenManagement of Arterial LineFarcasanu Liana GeorgianaNoch keine Bewertungen
- Tracheostomy CareDokument22 SeitenTracheostomy CareHollan Galicia100% (1)
- CATHETERIZATIONDokument13 SeitenCATHETERIZATIONSarah Uy Caronan100% (1)
- Example of Nursing Care Plan (Pathophysiology)Dokument5 SeitenExample of Nursing Care Plan (Pathophysiology)Elizabeth ZamoraNoch keine Bewertungen
- Community Health Nursing Notes (Second Year)Dokument6 SeitenCommunity Health Nursing Notes (Second Year)anette katrinNoch keine Bewertungen
- ThoracentesisDokument4 SeitenThoracentesisDunathree Caranto CorcueraNoch keine Bewertungen
- Patient Positioning in Operating TheatreDokument52 SeitenPatient Positioning in Operating TheatreFatkhul AdhiatmadjaNoch keine Bewertungen
- NCM 212 - Pharmacokinetics and PharmacodynamicsDokument11 SeitenNCM 212 - Pharmacokinetics and PharmacodynamicsLYRIZZA LEA BHEA DESIATANoch keine Bewertungen
- HEC BSN 4 YearDokument254 SeitenHEC BSN 4 Yearkhizar hayatNoch keine Bewertungen
- Medical PrefixesDokument6 SeitenMedical PrefixesNasirah Nasi ImpitNoch keine Bewertungen
- Pleural Fluid Analysis: How The Test Is PerformedDokument4 SeitenPleural Fluid Analysis: How The Test Is PerformedKevin LlorenteNoch keine Bewertungen
- Periop Power PointDokument97 SeitenPeriop Power PointAldrine Albor Anyayahan INoch keine Bewertungen
- ChesttubedrainageDokument65 SeitenChesttubedrainagejerinthomasrajanNoch keine Bewertungen
- Digestive SystemDokument117 SeitenDigestive SystemKBDNoch keine Bewertungen
- Thoracentesis IntroductionDokument8 SeitenThoracentesis Introductionjyoti singhNoch keine Bewertungen
- SP42 Thoracentesis (Adult)Dokument7 SeitenSP42 Thoracentesis (Adult)Adam HuzaibyNoch keine Bewertungen
- Synthetic Approach ReportDokument20 SeitenSynthetic Approach ReportMarivic Diano100% (1)
- Return On InvestmentDokument15 SeitenReturn On InvestmentMarivic DianoNoch keine Bewertungen
- Wellness PowerpointDokument28 SeitenWellness PowerpointMarivic Diano0% (1)
- Light of HOPEDokument33 SeitenLight of HOPEMarivic DianoNoch keine Bewertungen
- BiologyDokument42 SeitenBiologyMarivic DianoNoch keine Bewertungen
- Why Did They Hide It FROM US: Remedy That Is 10,000 Times Stronger Than Chemotherapy!Dokument2 SeitenWhy Did They Hide It FROM US: Remedy That Is 10,000 Times Stronger Than Chemotherapy!Marivic DianoNoch keine Bewertungen
- Animal Tissues: Asia Technological School of Science and ArtsDokument2 SeitenAnimal Tissues: Asia Technological School of Science and ArtsMarivic DianoNoch keine Bewertungen
- Under The Guidance Of:: Dr. Sandeep Tandon Professor and Head of Dept. of PedodonticsDokument79 SeitenUnder The Guidance Of:: Dr. Sandeep Tandon Professor and Head of Dept. of PedodonticsMarivic DianoNoch keine Bewertungen
- Hospital Incident Command System (HICS) : Reported byDokument42 SeitenHospital Incident Command System (HICS) : Reported byMarivic DianoNoch keine Bewertungen
- Iv Regulation and Controlling DevicesDokument21 SeitenIv Regulation and Controlling DevicesMarivic DianoNoch keine Bewertungen
- Nurses' Perceived Job Related Stress and Job Satisfaction in Amman Private HospitalsDokument31 SeitenNurses' Perceived Job Related Stress and Job Satisfaction in Amman Private HospitalsMarivic Diano100% (1)
- Nurse To Colleagues: You Deserve A Break Today: by Tyler SmithDokument2 SeitenNurse To Colleagues: You Deserve A Break Today: by Tyler SmithMarivic DianoNoch keine Bewertungen
- Anatomy and Physiology of BVDokument16 SeitenAnatomy and Physiology of BVMarivic DianoNoch keine Bewertungen
- Suprising Truths About MotivationDokument2 SeitenSuprising Truths About MotivationMarivic DianoNoch keine Bewertungen
- Disaster Risk Management and MitigationDokument5 SeitenDisaster Risk Management and MitigationMarivic DianoNoch keine Bewertungen
- Fractures: (On Which We Will Likely Be Pimped)Dokument66 SeitenFractures: (On Which We Will Likely Be Pimped)Marivic DianoNoch keine Bewertungen
- Renal Cell Carcinoma - Nursing Considerations With The Use of Targeted TherapyDokument50 SeitenRenal Cell Carcinoma - Nursing Considerations With The Use of Targeted TherapyMarivic DianoNoch keine Bewertungen
- MeaslesDokument11 SeitenMeaslesMarivic DianoNoch keine Bewertungen
- Palliative and Terminal CareDokument78 SeitenPalliative and Terminal CareMarivic DianoNoch keine Bewertungen
- Fluid and Electrolytes Report!!Dokument20 SeitenFluid and Electrolytes Report!!Marivic DianoNoch keine Bewertungen
- Applied Clinical Anatomy: The Successful Integration of Anatomy Into Specialty-Specific Senior ElectivesDokument13 SeitenApplied Clinical Anatomy: The Successful Integration of Anatomy Into Specialty-Specific Senior ElectivesHesti AnwarNoch keine Bewertungen
- Department of Surgery Common ICD and RUVDokument2 SeitenDepartment of Surgery Common ICD and RUVAnne Lorraine BringasNoch keine Bewertungen
- NP3 Nursing Board Exam June 2007Dokument44 SeitenNP3 Nursing Board Exam June 2007rem_cen24100% (1)
- Pleural EffusionDokument2 SeitenPleural EffusionKhalid Mahmud Arifin100% (1)
- EmpyemaDokument33 SeitenEmpyemavirz23100% (1)
- Medical Surgical Nursing TionkoDokument40 SeitenMedical Surgical Nursing TionkojeshemaNoch keine Bewertungen
- Aspiration PneumoniaDokument16 SeitenAspiration PneumoniaFeni DianiNoch keine Bewertungen
- Blue Protocol. Lung Ultrasound in The Critically IllDokument12 SeitenBlue Protocol. Lung Ultrasound in The Critically IllRomina Alfonsina Decap CarrascoNoch keine Bewertungen
- Chest Tubes and ThoracentesisDokument18 SeitenChest Tubes and ThoracentesisecleptosNoch keine Bewertungen
- Pleural EffusionDokument34 SeitenPleural EffusionFazlullah HashmiNoch keine Bewertungen
- 'Batangas Medical Center Case Report by PGI Carlos H. AcuñaDokument7 Seiten'Batangas Medical Center Case Report by PGI Carlos H. AcuñaCarlos H. AcuñaNoch keine Bewertungen
- Sample Review Questions in Medical and Surgical Nursing and Sample Board Exam QuestionsDokument22 SeitenSample Review Questions in Medical and Surgical Nursing and Sample Board Exam Questionstinea nigraNoch keine Bewertungen
- 3.pleural Effusion Imaging - Overview, Radiography, Computed TomographyDokument32 Seiten3.pleural Effusion Imaging - Overview, Radiography, Computed TomographyAchmadRizaNoch keine Bewertungen
- 5 MED II 1 - PneumoniaDokument11 Seiten5 MED II 1 - PneumoniaDeann RoscomNoch keine Bewertungen
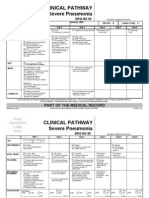
- Clinical Pathways Severe PneumoniaDokument2 SeitenClinical Pathways Severe PneumoniaaandakuNoch keine Bewertungen
- krok 2 З English 2007 2020 SURGERY+Dokument79 Seitenkrok 2 З English 2007 2020 SURGERY+Zeynep YılmaztürkNoch keine Bewertungen
- Approach To Pleural EffusionDokument46 SeitenApproach To Pleural EffusionBaskoro Tri LaksonoNoch keine Bewertungen
- Nursing Assignment 2Dokument12 SeitenNursing Assignment 2ticticNoch keine Bewertungen
- Surgery & Pediatrics SurgeryDokument111 SeitenSurgery & Pediatrics SurgeryHIMANSHU GUPTANoch keine Bewertungen
- Important Numbers For SMLEDokument3 SeitenImportant Numbers For SMLEAkpevwe EmefeNoch keine Bewertungen
- Bullets: "Victory Belongs To Those Who Are Most Persevering. Ad Majorem Dei Gloriam."Dokument15 SeitenBullets: "Victory Belongs To Those Who Are Most Persevering. Ad Majorem Dei Gloriam."Jhaylord mendozaNoch keine Bewertungen
- Prioritization, Delegation & Assignment 1-3Dokument12 SeitenPrioritization, Delegation & Assignment 1-3eric100% (2)
- Test Bank Clinical Manifestations and Assessment of Respiratory Disease Mid PartDokument24 SeitenTest Bank Clinical Manifestations and Assessment of Respiratory Disease Mid Partweekup035Noch keine Bewertungen
- Ecografia Toracica PDFDokument12 SeitenEcografia Toracica PDFCristinaLucanNoch keine Bewertungen
- filePV 31 05 232Dokument11 SeitenfilePV 31 05 232Raul Hernandez SotoNoch keine Bewertungen
- Oxygen InsuffiencyDokument21 SeitenOxygen InsuffiencyAntony Raj Culandai Swamy100% (1)
- Pathophysiology Plueral Effusion Secondary To Pneumonia: GreenDokument7 SeitenPathophysiology Plueral Effusion Secondary To Pneumonia: Greenkuro hanabusaNoch keine Bewertungen
- Report EmpyemaDokument32 SeitenReport EmpyemaMylah CruzNoch keine Bewertungen
- Thoracentesis IntroductionDokument8 SeitenThoracentesis Introductionjyoti singhNoch keine Bewertungen