Beruflich Dokumente
Kultur Dokumente
ACLS and Megacode
Hochgeladen von
Mark JosephCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
ACLS and Megacode
Hochgeladen von
Mark JosephCopyright:
Verfügbare Formate
Advance Cardiovascular Life Support and Mega Code Protocol
Mark Joseph S. Tunac, RN
Changes in 2010 Update
THE QUALITY OF CHEST COMPRESSION
In basic life support, compression depth has been increased to between 5 & 6 cm.
Previous studies on both suggested that to achieve ROSC, CPP of over 15 mmHg during chest compressions are required and that the depth previously recommended of 45 cm for chest compressions was inadequate.
Minimizing of disruption in the compression sequence
Defibrillation should take a maximum period of five seconds, with charging during chest compressions.
For tracheal intubation, ten seconds hands-off time for the passage of the tube is the only point at which compressions are paused.
Pulse checks are only undertaken where there are signs suggestive of ROSC.
USE & TIMING OF DRUGS
The use and timing of drugs have been simplified.
Atropine, long given for asystole and slow PEA, is discontinued, it remains for peri-arrest management. The tracheal route of drug administration is not recommended except in neonates following the widespread introduction of intraosseous devices.
POST-RESUSCITATIO CARE
2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care
Management of Cardiac Arrest
Cardiac arrest can be caused by 4 rhythms: ventricular fibrillation (VF), pulseless ventricular tachycardia (VT), pulseless electric activity (PEA), and asystole.
VF represents disorganized electric activity, whereas pulseless VT represents organized electric activity of the ventricular myocardium. Neither generates significant forward blood flow. PEA encompasses a heterogeneous group of organized electric rhythms associated with either absence of mechanical ventricular activity or mechanical ventricular activity that is insufficient to generate a clinically detectable pulse.
Asystole ( ventricular asystole ) represents absence of detectable ventricular electric activity with or without atrial electric activity.
For VF/pulseless VT, attempted defibrillation within minutes of collapse. For victims of witnessed VF arrest, early CPR and rapid defibrillation can significantly increase the chance for survival to hospital discharge.
Other ACLS therapies such as some medications and advanced airways, although associated with an increased rate of ROSC, have not been shown to increase the rate of survival to hospital discharge.
Combination of higher quality CPR and post arrest interventions such as therapeutic hypothermia and early percutaneous coronary intervention (PCI), doesnt necessarily improves the outcome. Periodic pauses in CPR should be as brief as possible and only as necessary to assess rhythm, shock VF/VT, perform a pulse check when an organized rhythm is detected, or place an advanced airway.
Monitoring and optimizing quality of CPR is encouraged and includes:
Optimizing chest compression rate and depth, adequacy of relaxation, and minimization of pauses. Monitoring partial pressure of end-tidal CO2 [PETCO2], arterial pressure during the relaxation phase of chest compressions, or [ScvO2] when feasible.
In the absence of an advanced airway, a synchronized compression ventilation ratio of 30:2 is recommended at a compression rate of at least 100 per minute. After placement of an advanced airway, the provider performing chest compressions should deliver at least 100 compressions per minute without pauses for ventilation.
The provider delivering ventilations should give 1 breath every 6 to 8 seconds (8 to 10 breaths per minute) and should avoid delivering an excessive number of ventilations.
ADULT CARDIAC ARREST ALGORITHM
Megacode Protocol
Members of the Code Team
Team Leader Chest Compressor Airway Manager IV therapist Electrical Therapist Code Recorder
Elements of Effective Code Team
Closed loop Communication Clear Messages Clear roles and responsibilities Know ones limitation Knowledge sharing Constructive Intervention Re-evaluation and summarizing Mutual Respect
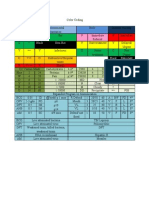
V tach / V Fib (-) Pulse
CPR
Defib
MEDS
EVAL
V tach (+) Pulse
Check BP Stable (BP> 90/60) Unstable (BP< 90/60)
MEDS
AALP
Cardiovert
100 joules
A Fib/SVT/A flutter
Check pulse and BP Stable (BP> 90/60) Unstable (BP< 90/60)
Vagal stimulation
Cardiovert
MEDS SVT 50-100 joules A fib 120-200 joules
AVID
Asystole/PEA
Check electrode and Pulse (-)
CPR
MEDS
EV
S Tach/ NSR
Check BP and Pulse Stable (BP> 90/60) Unstable (BP< 90/60)
PCC
Fast drip of Saline solution or
Dopamine Drip
S Brady
Check BP and Pulse Stable (BP> 90/60) Unstable (BP< 90/60)
PCC
ATDE
Post Cardiac Care (PCC)
PCC
Check O2 saturation
SpO2 70- 92
BVM OPA/NPA Non-Rebreather Mask at 10-15LPM
SpO2 <70
ET LMA Combitube
PCC
Insert NGT Insert IFC 12 lead or 14 lead ECG X-ray ABG and other blood works Transfer to ICU
Das könnte Ihnen auch gefallen
- ACLS Advanced Cardiovascular Life Support Provider Manual 2023Von EverandACLS Advanced Cardiovascular Life Support Provider Manual 2023Noch keine Bewertungen
- Acls MegacodeDokument8 SeitenAcls Megacodes33d_destinyNoch keine Bewertungen
- ACLS and PALS Certification Practice QuestionsDokument11 SeitenACLS and PALS Certification Practice Questionsdyah rahayu hutamiNoch keine Bewertungen
- Aha Acls Prep Packet 2020Dokument69 SeitenAha Acls Prep Packet 2020VP The Hacker100% (2)
- ACLS NotesDokument3 SeitenACLS Notessaxmanwrv0% (1)
- American Heart Association Acls Post Test AnswersDokument4 SeitenAmerican Heart Association Acls Post Test AnswersArun Jude Alphonse0% (9)
- ACLS PRETEST ANSWER KEY RHYTHM IDENTIFICATIONDokument3 SeitenACLS PRETEST ANSWER KEY RHYTHM IDENTIFICATIONaditNoch keine Bewertungen
- 15 Item ACLS Drill With RationaleDokument12 Seiten15 Item ACLS Drill With RationaleLj Ferolino100% (1)
- ACLS Practice TestDokument5 SeitenACLS Practice Testprettynpink0867% (3)
- ACLS PrecourseAssessmentDokument19 SeitenACLS PrecourseAssessmentRaiedKhaled100% (1)
- ACLS (Advanced Cardiac Life Support) Algorithms & NotesDokument4 SeitenACLS (Advanced Cardiac Life Support) Algorithms & Notesiamlucil100% (4)
- AHA ACLS Written Test: Ready To Study? Start With FlashcardsDokument8 SeitenAHA ACLS Written Test: Ready To Study? Start With FlashcardssallyNoch keine Bewertungen
- Cardiac Arrest Drugs & ProceduresDokument8 SeitenCardiac Arrest Drugs & ProceduresAstri Adel BudiarsoNoch keine Bewertungen
- ACLS Simulation ScenariosDokument14 SeitenACLS Simulation ScenariosVanessa HermioneNoch keine Bewertungen
- The Crash CartDokument39 SeitenThe Crash Cartpramod kumawat100% (1)
- CPR Class QuestionnaireDokument4 SeitenCPR Class QuestionnaireParikshit PekhaleNoch keine Bewertungen
- 2010 Integrated Updated Circulation ACLS Acute Coronary Syndromes AlgorithmDokument1 Seite2010 Integrated Updated Circulation ACLS Acute Coronary Syndromes Algorithmms_lezahNoch keine Bewertungen
- AHA ELearning ACLS Precourse Self-Assessment and Precourse WorkDokument1 SeiteAHA ELearning ACLS Precourse Self-Assessment and Precourse Work9kjsntkrzcNoch keine Bewertungen
- TestDokument11 SeitenTestzenagit123456100% (1)
- AclsDokument85 SeitenAclsJulia CostaNoch keine Bewertungen
- ACLS QuizletDokument7 SeitenACLS Quizletek.9006001Noch keine Bewertungen
- ACLS Practice Test 1Dokument6 SeitenACLS Practice Test 1tarrynwortmann5319100% (3)
- Megacode Simulator 1Dokument10 SeitenMegacode Simulator 1srimatsimhasaneshwarNoch keine Bewertungen
- ACLS Full LectureDokument47 SeitenACLS Full LectureAdhydeva Purusanti100% (3)
- Emergency DrugsDokument26 SeitenEmergency DrugsSiergs Smith GervacioNoch keine Bewertungen
- ACLS Review Guide for Cardiac Arrest Scenarios and TreatmentDokument29 SeitenACLS Review Guide for Cardiac Arrest Scenarios and TreatmentJB Reyes100% (2)
- BLS and ACLS Case ScenariosDokument35 SeitenBLS and ACLS Case ScenariosrajNoch keine Bewertungen
- Introd To ECG Code Blue Champs March 2019Dokument52 SeitenIntrod To ECG Code Blue Champs March 2019james rukenya100% (1)
- ACLS DrugDokument7 SeitenACLS DrugPhongsatorn Thunin100% (1)
- ACLS Test PrintscreenedDokument13 SeitenACLS Test Printscreenedhellfireomega67% (9)
- Cals ReviewbjvjvjDokument14 SeitenCals ReviewbjvjvjCarl Jay M Ocariza100% (1)
- Nursing Responsibilities in Handling AntibioticsDokument4 SeitenNursing Responsibilities in Handling Antibioticsrichardmd20% (1)
- ACLS Written 2006 Precourse Self AssessmentDokument14 SeitenACLS Written 2006 Precourse Self AssessmentmonickamsNoch keine Bewertungen
- ACLS Precourse Test AnswersDokument60 SeitenACLS Precourse Test AnswersTip Piraya60% (5)
- ACLS Provider Manual Supplementary MaterialDokument86 SeitenACLS Provider Manual Supplementary MaterialEma0% (2)
- Soalan MCQ Acls Fit Set BDokument3 SeitenSoalan MCQ Acls Fit Set BAnonymous 89ilBIGhrmNoch keine Bewertungen
- ACLS Rhythms Practice Test 2020 Recognition Rhythm Strips (PDF)Dokument11 SeitenACLS Rhythms Practice Test 2020 Recognition Rhythm Strips (PDF)김민길100% (2)
- ACLS Exam - A&B VersionsDokument36 SeitenACLS Exam - A&B VersionsMohamed El-sayed100% (1)
- ACLS 2020 Algorithms: American Heart Association 2020 GuidelinesDokument8 SeitenACLS 2020 Algorithms: American Heart Association 2020 GuidelinesNofi Nurina100% (4)
- ACLS Drugs: Primary Medications Used in Cardiac Arrest AlgorithmsDokument10 SeitenACLS Drugs: Primary Medications Used in Cardiac Arrest AlgorithmsChintami Octavia100% (1)
- ACLS FullMapsDokument68 SeitenACLS FullMapswong2689Noch keine Bewertungen
- ACLS Post Test (Copy) 낱말 카드 - QuizletDokument18 SeitenACLS Post Test (Copy) 낱말 카드 - Quizlet김민길Noch keine Bewertungen
- AclsDokument73 SeitenAclsKamel Hady50% (2)
- ACLS Algorithms SlideDokument26 SeitenACLS Algorithms SlidehrsoNoch keine Bewertungen
- BLS ALGORITHM As of February 2023Dokument2 SeitenBLS ALGORITHM As of February 2023Mark Jason Rodriguez, RNNoch keine Bewertungen
- ACLS ECG Rhythms & Pharmacology ReviewDokument24 SeitenACLS ECG Rhythms & Pharmacology Reviewkarenjlazarus86% (14)
- ACLS Provider Manual 2015 NotesDokument5 SeitenACLS Provider Manual 2015 Notescrystalshe93% (14)
- ACLS PrecourseAssessmentDokument19 SeitenACLS PrecourseAssessmentBrigitte Elaine81% (21)
- A Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsVon EverandA Simple Guide to Abdominal Aortic Aneurysm, Diagnosis, Treatment and Related ConditionsNoch keine Bewertungen
- Cardio Pulmonary Resuscitation (CPR) and Automated External Defibrillation (AED) Training GuideVon EverandCardio Pulmonary Resuscitation (CPR) and Automated External Defibrillation (AED) Training GuideBewertung: 5 von 5 Sternen5/5 (1)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsVon EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNoch keine Bewertungen
- Advanced Cardiovascular Life Support (ACLS)Dokument27 SeitenAdvanced Cardiovascular Life Support (ACLS)Sara Ali100% (3)
- Managing Cardiac ArrestDokument12 SeitenManaging Cardiac ArrestpunctumlacrimaleNoch keine Bewertungen
- Guidelines Adult Advanced Life SupportDokument35 SeitenGuidelines Adult Advanced Life SupportindahNoch keine Bewertungen
- Advanced Cardiac Life Support: Valentina, MD, FIHADokument34 SeitenAdvanced Cardiac Life Support: Valentina, MD, FIHAfaradibaNoch keine Bewertungen
- CPR PDFDokument37 SeitenCPR PDFArdhi AgustjikNoch keine Bewertungen
- WHATs New in CPCRDokument4 SeitenWHATs New in CPCRJessicaHernandezNoch keine Bewertungen
- Gordon PDFDokument5 SeitenGordon PDFAthena SaturdayNoch keine Bewertungen
- Virginia Avenel HendersonDokument16 SeitenVirginia Avenel HendersonMark JosephNoch keine Bewertungen
- Question 1: What Is The PR Interval in This ECG?Dokument4 SeitenQuestion 1: What Is The PR Interval in This ECG?Mark JosephNoch keine Bewertungen
- Learning French EbookDokument36 SeitenLearning French EbookDonnette Davis100% (20)
- What Is CancerDokument13 SeitenWhat Is CancerMark JosephNoch keine Bewertungen
- Surgical and Radiation TherapyDokument22 SeitenSurgical and Radiation TherapyMark JosephNoch keine Bewertungen
- CT ShowDokument17 SeitenCT ShowMark JosephNoch keine Bewertungen
- Analysis and Evaluation of TheoriesDokument9 SeitenAnalysis and Evaluation of TheoriesMark JosephNoch keine Bewertungen
- Men in NursingDokument2 SeitenMen in NursingMark JosephNoch keine Bewertungen
- In Partial Fullfilment of The Course Requirements IN MSN 104: Clinical TeachingDokument6 SeitenIn Partial Fullfilment of The Course Requirements IN MSN 104: Clinical TeachingAnish VeettiyankalNoch keine Bewertungen
- Color Coding (CHN)Dokument1 SeiteColor Coding (CHN)Mark JosephNoch keine Bewertungen
- Diabetes Mellitus: Diagnostic ExamsDokument11 SeitenDiabetes Mellitus: Diagnostic ExamsMark JosephNoch keine Bewertungen
- Psycho PharmaDokument8 SeitenPsycho PharmaMark JosephNoch keine Bewertungen
- Patho InflammationDokument1 SeitePatho InflammationMark JosephNoch keine Bewertungen
- Diabetes Mellitus - Pathophysiological ParadigmDokument4 SeitenDiabetes Mellitus - Pathophysiological ParadigmMark JosephNoch keine Bewertungen
- RH Bill 2011Dokument31 SeitenRH Bill 2011Mark JosephNoch keine Bewertungen
- Fundamentals of NursingDokument4 SeitenFundamentals of NursingMark JosephNoch keine Bewertungen
- Types of FeedingDokument21 SeitenTypes of FeedingMark JosephNoch keine Bewertungen
- KuljeetDokument5 SeitenKuljeetSatyam TejiNoch keine Bewertungen
- WakoDokument2 SeitenWakoJimmy HarperNoch keine Bewertungen
- Clinical Exam RequirementDokument7 SeitenClinical Exam Requirementyb5fdt8cp7Noch keine Bewertungen
- Gordon's 11 Functional Health PatternDokument4 SeitenGordon's 11 Functional Health PatternVhince Norben PiscoNoch keine Bewertungen
- Raport StimulatorDokument88 SeitenRaport StimulatorEghet SilviuNoch keine Bewertungen
- Mitral Valve ProlapseDokument7 SeitenMitral Valve ProlapsehracakNoch keine Bewertungen
- Chest Pain DiagnosisDokument6 SeitenChest Pain DiagnosisJefri SoniNoch keine Bewertungen
- Puskesmas Cipadung Patient List December 2020Dokument65 SeitenPuskesmas Cipadung Patient List December 2020Aprilia PuspitasariNoch keine Bewertungen
- ACCSAP 10 Qs & As ReviewDokument470 SeitenACCSAP 10 Qs & As ReviewAdeel Lakhiar100% (8)
- Presentation 1Dokument12 SeitenPresentation 1Rizka FarahinNoch keine Bewertungen
- Britain: Nasty, British and ShortDokument3 SeitenBritain: Nasty, British and ShortLuana BarretoNoch keine Bewertungen
- Obesity - Kusimbisa: "Vanhu Vakawanda Munyika Varikufa Nokuda Kwekudya .... Kutopfuura Kufa Nenzara... " - BenjaminDokument8 SeitenObesity - Kusimbisa: "Vanhu Vakawanda Munyika Varikufa Nokuda Kwekudya .... Kutopfuura Kufa Nenzara... " - BenjaminMthabisi Tawanda NembawareNoch keine Bewertungen
- Pacemaker ThesisDokument4 SeitenPacemaker Thesissandraarvesethsaltlakecity100% (2)
- Nursing Care of Children with Cardiovascular DisordersDokument11 SeitenNursing Care of Children with Cardiovascular DisordersJœnríčk AzueloNoch keine Bewertungen
- Cardiac Sequential AnalysisDokument34 SeitenCardiac Sequential AnalysisMochamad Rizky HendiperdanaNoch keine Bewertungen
- Jambore-Pkb (Lazuardi Dwipa, DR - SPPD, K-Ger)Dokument65 SeitenJambore-Pkb (Lazuardi Dwipa, DR - SPPD, K-Ger)UPT PKM UJUNGBERUNG INDAHNoch keine Bewertungen
- Articulo - Theory and Desicion MakingDokument5 SeitenArticulo - Theory and Desicion MakingJaNe RNNoch keine Bewertungen
- Acs Guideline PDFDokument56 SeitenAcs Guideline PDFPrimasari HijriyahNoch keine Bewertungen
- 1-1-3 English CoreDokument11 Seiten1-1-3 English CoreRavneet KaurNoch keine Bewertungen
- Paralele Lijekova: Generičko Ime Djelovanje Tvorničko ImeDokument3 SeitenParalele Lijekova: Generičko Ime Djelovanje Tvorničko ImeStella GašparušNoch keine Bewertungen
- Estenosis Carotidea en Paciente Con Cardiopatía IsquémicaDokument57 SeitenEstenosis Carotidea en Paciente Con Cardiopatía IsquémicaSOLACI - Sociedad Latinoamericana de Cardiología IntervencionistaNoch keine Bewertungen
- Cardiac Arrest Upon Induction of General AnesthesiaDokument7 SeitenCardiac Arrest Upon Induction of General AnesthesiaIlona HiariejNoch keine Bewertungen
- L1 - SyncopeDokument5 SeitenL1 - SyncopeMuthukumaranNoch keine Bewertungen
- Jurnal Artikel Feby Nurlia 1907110032Dokument8 SeitenJurnal Artikel Feby Nurlia 1907110032Feby NurLiaNoch keine Bewertungen
- Rigel Uni Sim Lite DatasheetDokument5 SeitenRigel Uni Sim Lite Datasheetmailalexmd.vrn.ruNoch keine Bewertungen
- Physiology Lecture - Dr. Dominguez: Slow FastDokument3 SeitenPhysiology Lecture - Dr. Dominguez: Slow FastJayricDepalobosNoch keine Bewertungen
- NU 636 WK 2 DP 2 - Treatment of HyperlipidemiaDokument3 SeitenNU 636 WK 2 DP 2 - Treatment of HyperlipidemiaShayNoch keine Bewertungen
- ECG Guide: Understanding Waves, Intervals & Electrical EventsDokument164 SeitenECG Guide: Understanding Waves, Intervals & Electrical EventsMohsan RafiqNoch keine Bewertungen
- Errata updates for paspap 2nd Edition and Lang by Dr HameedDokument11 SeitenErrata updates for paspap 2nd Edition and Lang by Dr HameedUsama1987Noch keine Bewertungen
- Cap 6 Heart and Cardiovascular SystemDokument19 SeitenCap 6 Heart and Cardiovascular Systemgorexz goreNoch keine Bewertungen