Beruflich Dokumente
Kultur Dokumente
Enteral Feeding of The High Risk Newborn
Hochgeladen von
Sri Soelistijawati0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
298 Ansichten56 SeitenEnteral feeding of the High Risk Newborn - Session 1 Competency Based Training Module for physicians. Module aims to provide facilitators with knowledge, skills and competencies to provide appropriate enteral nutritional support for high risk neonates. Goal is to achieve nutritional support by the enteral route in order to provide optimal growth and development.
Originalbeschreibung:
Originaltitel
Enteral Feeding of the High Risk Newborn
Copyright
© Attribution Non-Commercial (BY-NC)
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenEnteral feeding of the High Risk Newborn - Session 1 Competency Based Training Module for physicians. Module aims to provide facilitators with knowledge, skills and competencies to provide appropriate enteral nutritional support for high risk neonates. Goal is to achieve nutritional support by the enteral route in order to provide optimal growth and development.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
298 Ansichten56 SeitenEnteral Feeding of The High Risk Newborn
Hochgeladen von
Sri SoelistijawatiEnteral feeding of the High Risk Newborn - Session 1 Competency Based Training Module for physicians. Module aims to provide facilitators with knowledge, skills and competencies to provide appropriate enteral nutritional support for high risk neonates. Goal is to achieve nutritional support by the enteral route in order to provide optimal growth and development.
Copyright:
Attribution Non-Commercial (BY-NC)
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 56
Module: Enteral feeding of the High
Risk Newborn - Session 1
Competency Based Training Module for Physicians
Neonatal Health Care Modules
Enteral Feeding of the
High Risk Newborn
Jayashree Ramasethu, M.D.
Georgetown University Hospital
Washington, D.C.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Module Overview: Purpose
The purpose of this module is to provide
facilitators with a sound, competency based
training methodology which if implemented
as designed, will result in physicians
attaining the knowledge, skills and
competencies to provide appropriate enteral
nutritional support for high risk neonates.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Module Overview: Purpose
Physicians will learn to:
Identify newborn infants at risk for feeding difficulties
Determine the appropriate route and type of feeding,
including selection of milk and supplements.
Initiate enteral feeding in at - risk newborns at the
appropriate time, and advancement of feeds appropriately.
Identify and manage feeding intolerance
Identify and manage necrotizing enterocolitis.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Module Overview: Story
Providing adequate nutritional support by the enteral route
to neonates with problems is a challenge.
Feeding may be limited by immaturity, illness or both.
The initiation and advancement of feeds, the selection of
milk for feeding, and the route of feeding are to be
considered carefully in each case.
The final goal is to achieve nutritional support by the
enteral route in order to provide optimal growth and
development.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Learning objectives
+ Define feeding difficulties in sick or at- risk
neonates.
+Assess when to start enteral feeds, including
contraindications to feeding.
+Define trophic feeding, indications and strategy.
+Understand appropriate advancement of enteral
nutrition.
+Identify the nutritional and caloric contents of
various milks.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Learning objectives
eSelect the appropriate route of feeding
e oral
e tube feeding- gastric or transpyloric feeds,
continuous or bolus feeds
eUnderstand the goals of nutritive feeds, and
the monitoring of nutrition and growth.
eAssess and manage feeding intolerance.
eIdentify necrotizing enterocolitis
Module: Enteral feeding of the High
Risk Newborn - Session 1
The best feeding is
Breast feeding
Breast feeding
Breast feeding
For Term & Preterm
babies!
Module: Enteral feeding of the High
Risk Newborn - Session 1
High Risk Newborns may not be able to
breastfeed (or even tolerate enteral nutrition)
Prematurity
Perinatal asphyxia
Respiratory distress
Sepsis
Hemodynamic instability
Paralytic ileus
Intestinal obstruction
Craniofacial abnormalities
cleft lip
cleft palate
Module: Enteral feeding of the High
Risk Newborn - Session 1
Sick newborns may need intravenous nutrition
until they are stable enough to have enteral feeds
But intravenous nutrition :
is expensive
is more complicated
requires more laboratory testing and monitoring
has more complications
Module: Enteral feeding of the High
Risk Newborn - Session 1
Feeding
Trophic effect on intestinal mucosa
Starvation thinning of intestinal mucosa, villus
shortening, reduction of enzyme activity
Enteral feeding increased DNA synthesis,
increased intestinal mucosal mass
Maturation of intestinal muscular function
Endocrine and metabolic effects
Module: Enteral feeding of the High
Risk Newborn - Session 1
Enteral Nutrition in High Risk Newborns:
When to feed
How to feed
What to feed
Module: Enteral feeding of the High
Risk Newborn - Session 1
When to feed: as early as possible
Early Feeding
+ feeding intolerance
Full enteral nutrition established earlier!
+ days of parenteral nutrition
+ cholestasis
+ days in hospital
No increase in incidence of NEC
Module: Enteral feeding of the High
Risk Newborn - Session 1
Initiation of
enteral feeds
_Hemodynamically stable
_No ileus
_No significant acidosis
_No significant PDA
Module: Enteral feeding of the High
Risk Newborn - Session 1
How to feed:
based on gestational age and clinical condition
Oromotor skills - normal development
Gag reflex: 18 weeks gestation
Sucking reflex
non nutritive 30-32 weeks
uncoordinated 32-34 weeks
coordinated 35-36 weeks
Rooting reflex: 37 weeks
Module: Enteral feeding of the High
Risk Newborn - Session 1
How to feed:
Oral feeding: breast (or bottle)
at least 33 weeks gestation
no respiratory distress ( rate<60/min)
Tube feeding
less than 33 weeks gestation
neurological impairment (abnormal suck/
swallow)
respiratory distress (no hypoxia)
on a ventilator
Module: Enteral feeding of the High
Risk Newborn - Session 1
How to feed:
Tube feeding
Nasogastric or orogastric tube feeds
intermittent or continuous
Nasojejunal / transpyloric tube feeds
severe reflux
delayed gastric emptying
continuous feeds only
Module: Enteral feeding of the High
Risk Newborn - Session 1
Procedure: Placement of Orogastric or
Nasogastric tube
Use size 5 ( for babies less than 2 kg) or size 8 (for
babies more than 2 kg) feeding tube
Tube may be silastic ( best), polyurethane or PVC
Measure distance from nose or mouth to ear
opening, and then down to xiphisternum.
Pass tube down nose or mouth to pre- determined
distance + 1- 2 cms.
Check placement by injecting air into tube and
auscultating over stomach, or by aspirating
stomach contents. Tape into place.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Procedure: Placement of
transpyloric tube
Use only size 5 silastic tube
Polyurethane or PVC tubes harden with
time and can cause perforation of
duodenum.
Module: Enteral feeding of the High
Risk Newborn - Session 1
What to feed:
Choice of milk for initial feeds
Colostrum or Maternal milk
_isotonic
_low renal solute load
_immunologic advantages
_psychosocial advantages
Module: Enteral feeding of the High
Risk Newborn - Session 1
Advantages of human milk
decreases infections
decreases allergic disease
increases IQ?
decreases adult obesity/ HTN/DM
cost / availability
Module: Enteral feeding of the High
Risk Newborn - Session 1
Advantage of
human milk
in the NICU
easily digested
better tolerance
decreases infection rate
decreases hospitalization
better outcomes
For mother: psychosocial wellbeing
Module: Enteral feeding of the High
Risk Newborn - Session 1
Composition of human milk
Colostrum Preterm Mature Milk
Calories Kcal / dl 67 67 67
Protein g/dl 3.1 1.4 1.05
Lactose g/dl 4.1 6.6 7.2
Fat g/dl 2 -2.5 3.5- 4 3.5 - 4.5
Module: Enteral feeding of the High
Risk Newborn - Session 1
Is Human Milk alone adequate for the
growing preterm infant?
15 day old preterm infant
150 ml/ kg /day of mothers milk
= 90 -100 kcal / kg/day
= 2- 2.5 g/kg/day of protein
Module: Enteral feeding of the High
Risk Newborn - Session 1
Estimated caloric requirement of a
growing preterm infant (AAP 1985)
Kcal / kg / day
Resting metabolic rate 50
Cold stress 10
Activity 15
Synthesis / thermic effect of food 8
Fecal loss 12
Growth 25
Total 120
Aim: 120 Kcal/ kg/day, 3 to 3.8 g protein/ kg/day
Module: Enteral feeding of the High
Risk Newborn - Session 1
Rate of weight gain in fetus highest between 26 and 36 weeks
Aim:
Growth of the preterm infant should be similar to
intrauterine growth of a fetus at the same gestational age,
approximately 15g/kg/day.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Additives
Human milk fortifier : carbohydrate
protein, minerals,
vitamins
MCT oil: 1 cc = 7.7 Kcal
Canola oil: 1 cc = 8 kcal
Promod 1 tsp: 1 g whey protein
Polycose: glucose polymers
Module: Enteral feeding of the High
Risk Newborn - Session 1
Nutrient Distribution
Nutrient Caloric range Maximum calories
Protein 8-12 % 20%
Carbohydrate 40-55% 60%
Fat 35-50% 60%
Module: Enteral feeding of the High
Risk Newborn - Session 1
Nutrient Composition of Preterm Human Milk
with Human Milk Fortifier (from Berseth CL, Pediatrics 2004)
Nutrients Preterm Human
Milk (100 ml)
PHM + HMF
(100 ml + 4 packets)
Energy, kJ 277 336
Protein, g 1.6 2.7
Fat, g 3.5 4.5
Carbohydrate, g 7.3 7.5
Vitamin A, IU 48 998
Vitamin D, IU 8 158
Vitamin E, IU 0.4 5.0
Vitamin K, IU 2.0 6.4
Calcium, mg 25 115
Phosphorus, mg 14.5 64.5
Iron, mg 0.09 1.53
Zinc, mg 0.37 1.09
Module: Enteral feeding of the High
Risk Newborn - Session 1
Preterm Formula
Formula Kcal
/30 ml
Protein
gm/dl
Fat
gm/dl
CHO
gm/dl
Calcium
mg/dl
Phosphate
mg/dl
Human
milk
20 1.1 4.5 7.1 33 15
Enfamil
premature
20 2.0 3.4 7.4 112 56
Enfamil
premature
24 2.4 4.1 8.9 134 68
Module: Enteral feeding of the High
Risk Newborn - Session 1
Fortified human milk versus
preterm formula ( Schanler Pediatrics 1999)
Gest: 28 1 weeks Birth Wt: 1.07 0.17 kg
Infants fed fortified human milk
slower rate of weight gain ( 22 g vs 26 g/kg/d)
lower length increase ( 0.8 cms vs 1.0 cms)
decreased incidence of late onset sepsis
decreased incidence of NEC
discharged earlier ( 73 days vs 88 days)
Module: Enteral feeding of the High
Risk Newborn - Session 1
Specialized formulas
Short bowel syndrome,
malabsorption, etc
Alimentum: casein hydrolysate, free amino acids,
modified tapioca starch, sucrose, safflower and soy oil,
50% MCT
Pregestimil: casein hydrolysate, free amino acids,
modified corn starch, glucose, corn oil, 55% MCT
Neocate: free aminoacids, corn syrup solids and modified
corn starch, safflower, coconut and soy oils
Module: Enteral feeding of the High
Risk Newborn - Session 1
Feeding Protocols
Trophic feeds
Advancement of feeds
Monitoring for tolerance
Nutritional goals
Nutrition monitoring
Module: Enteral feeding of the High
Risk Newborn - Session 1
Trophic feeding
+ Start as soon as baby is stable 1-3 days
+ Human milk or formula 10 cc/ kg/day
+ Feed every 3 or 4 hours
+ Continue at same volume
+ Advance feeds when baby demonstrates
tolerance and is medically stable
( usually in 3 to 7 days)
Module: Enteral feeding of the High
Risk Newborn - Session 1
Advancement of feeds
Start at 10 ml / kg/day
Advance by 5 - 20 ml /kg /day
Time to full feeds
3 -5 days in baby > 2000g
10 -14 days in baby < 1250g
Module: Enteral feeding of the High
Risk Newborn - Session 1
Feeding Baby J
28 weeks gestation, 1200 g weight, RDS
Day 2: BP stable, RDS better, passed meconium, abdomen soft
Start feeds with MBM 1cc oro-gastric q6h
Day 3: CPAP, feeds to 2 cc every 3 hours
Day 4: nasal cannula oxygen, feeds to 4 cc every 3 h
Day 5: feeds to 6 cc every 3 hours (16 cc or 13 cc/kg increase)
Day 6,7,8: feeds by 2 cc every day to 12 cc every 3 hours
Day 9: 1 residual of 6 cc, then another of 8 cc, no abdominal distension
+ feeds to 10 cc q3h
Day 10: no residuals, advance feeds to 12 cc q3h..
Day 11, 12,13 : advance feeds to 15, 18 and 21 cc every 3 hours
Day 14: full feeds 24 cc every 3 hours
Module: Enteral feeding of the High
Risk Newborn - Session 1
Feeding Baby Girl J - wt 1.2 kg
24 cc MBM every 3 hours
= 160 cc / kg / day = 105 kcal/ kg/day
= 2.5 g / kg /day protein
Add HMF (human milk fortifier)
increase calories to 22 kcal /oz first
after 1-2 days increase calories to 24 kcal /oz
Goal: 120 kcal/ kg/day, 3 - 3.5 g/kg/day protein
Module: Enteral feeding of the High
Risk Newborn - Session 1
Vitamin supplementation in preterm
babies
Vitamin A 1500 IU/ kg/day
Vitamin D 400 IU/day
Vitamin E 6 -12 IU / kg/day
Vitamin K- IM at birth
Vitamin B complex
Vitamin C
Multivitamin drops 0.5- 1.0 ml/day
Module: Enteral feeding of the High
Risk Newborn - Session 1
Iron supplementation
2- 4 mg/ kg / day of dietary elemental iron
Preferably after 2 weeks of age
No later than 2 months of age
Module: Enteral feeding of the High
Risk Newborn - Session 1
Feeding Intolerance
Stop enteral feeds and reassess:
Bilious ( or greenish residuals)
Increased residuals ( > 25% of a feed, or
more than the hourly rate if fed
continuously), or vomiting
Acute increase in abdominal girth > 2 cms
Frankly bloody or very watery stool
Other signs of illness
Module: Enteral feeding of the High
Risk Newborn - Session 1
Feeding Intolerance- assessment
Does baby appear well?
Is the abdomen soft?
Has the nature of the stool changed?
Is this the first episode of intolerance or has
this problem been increasing?
Module: Enteral feeding of the High
Risk Newborn - Session 1
Feeding Intolerance- management
If baby appears well, and the abdomen is
soft, may consider re-feeding after a brief
(2 to 6 hour period of observation).
If unsure, may discontinue enteral feeds for
24 hours and restart at a smaller volume.
If abdomen is distended, or tense, or stools
are bloody, discontinue feeds and obtain
Xray of the abdomen to rule out NEC.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Necrotizing Enterocolitis (NEC)
Module: Enteral feeding of the High
Risk Newborn - Session 1
Necrotizing Enterocolitis (NEC)
Predisposing conditions:
Prematurity, perinatal asphyxia, formula feeding
Signs:
gastrointestinal: feeding intolerance, abdominal distension,
bloody stools
systemic: lethargy, temperature instability, apnea,
bradycardia, acidosis, DIC, hypotension
Radiological: intestinal dilatation, pneumatosis intestinalis,
ascites, perforation
Module: Enteral feeding of the High
Risk Newborn - Session 1
Necrotizing Enterocolitis (NEC)
Management:
Stop feeds, start IV fluids, place NG tube on
dependent drainage or low suction
Obtain blood culture, Complete blood
count, start antibiotics
Refer early to facility that can closely
monitor and manage these patients, and
perform surgery if necessary.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Other feeding issues
Suck- swallow incoordination
Oro- tactile defensiveness
Gastroesophageal reflux
Module: Enteral feeding of the High
Risk Newborn - Session 1
Gastroesophageal
Reflux
e19 % of preterm babies on
treatment for reflux
eAssociated with apnea?
eAssociated with airway problems- wheezing,
stridor and recurrent aspiration
eTreatment: small volume feeds, positioning,
thickening of feeds, H2 receptor blockers, proton
pump inhibitors
Module: Enteral feeding of the High
Risk Newborn - Session 1
Monitoring nutrition
in high risk neonates
Module: Enteral feeding of the High
Risk Newborn - Session 1
Monitoring Growth in the VLBW infant
Weight 15g/ day
Length 1 cm/ week
Head circumference 1 cm / week
Hematocrit/ retic count Every 1-2 weeks
Albumin/ electrolytes Every 2 weeks
Calcium/ phosphorus Every 2 weeks
Alkaline phosphatase Every 2 weeks
Module: Enteral feeding of the High
Risk Newborn - Session 1
Post -discharge
nutrition
Usual discharge weight
for preterm infants : 1800 - 2000 g
At discharge
smaller than term infants
low body stores
deficient bone mineralization
greater energy needs
Module: Enteral feeding of the High
Risk Newborn - Session 1
Post -discharge nutrition monitoring
Monitor weight, length, head circumference
Plot on growth charts adjusted for preterm infants
Increased caloric needs
add formula powder to maternal milk
special transition formula
Multivitamins
Iron
Module: Enteral feeding of the High
Risk Newborn - Session 1
Recommendations for post discharge
nutrition for preterm infants
( J Perinatol May 2005)
< 1800 g: 24 Cal / oz milk
Change to 22 Cal/ oz at > 1800 g when
growth parameters are 25th percentile and
infant is gaining 15 to 40 g/day
Change to 20 Cal/ oz at 4 to 6 months
corrected gestation if all growth parameters
are above 25th percentile
Module: Enteral feeding of the High
Risk Newborn - Session 1
Simple rule:
Regular breast milk or formula if
age > 3 months old
weight > 3 kgs
serum albumin > 3g/ dl
alkaline phosphatase < 300 IU/ ml
Module: Enteral feeding of the High
Risk Newborn - Session 1
Module: Enteral feeding of the High
Risk Newborn - Session 1
Case 1
Preterm baby girl E, born at 33 weeks gestation.
Birth weight 1800 g.
Apgar scores 1- 9, 5- 9
Baby appears alert and active, has no respiratory
distress.
When will you initiate feeds?
What feeds will you order?
How will you monitor adequacy of nutrition?
Module: Enteral feeding of the High
Risk Newborn - Session 1
Case 2.
Preterm baby boy born at 32 weeks
gestation. Birth weight 1500g.
Apgar scores 17, 5-8
Baby has mild RDS and is on CPAP.
Discuss nutritional support for this baby.
Module: Enteral feeding of the High
Risk Newborn - Session 1
Case 3
Preterm boy in case 2 is now 8 days old. He has
been receiving tube feeds of maternal breast milk
at 10 cc every 3 hours.
At 9 am today he had 6 cc undigested milk in the
stomach. You decided to give only 4 ml and
reassess. At 12 noon he had 10 ml of greenish
aspirate, and his abdominal circumference has
increased by 2 cms. What will you do?
Das könnte Ihnen auch gefallen
- Clinical Handbook of Insomnia (2017)Dokument292 SeitenClinical Handbook of Insomnia (2017)jcholguin.conciencia4100100% (8)
- Colchicine Drug Study For Gouty ArthritisDokument3 SeitenColchicine Drug Study For Gouty ArthritisLeslie PaguioNoch keine Bewertungen
- Forceps Delivery For Gravidocardiac PatientsDokument80 SeitenForceps Delivery For Gravidocardiac PatientsTots A. Macahilo-LayawonNoch keine Bewertungen
- Tuesday 14 January 2020: BiologyDokument24 SeitenTuesday 14 January 2020: Biologysham80% (5)
- Liver BiopsyDokument3 SeitenLiver BiopsyBiway RegalaNoch keine Bewertungen
- PREMATURITYDokument40 SeitenPREMATURITYBlykeBantuganNoch keine Bewertungen
- Clinical Approach To Respiratory Distress in NewbornDokument29 SeitenClinical Approach To Respiratory Distress in Newbornabhivnair100% (1)
- Hemolytic Disease of The NewbornDokument43 SeitenHemolytic Disease of The Newbornalibayaty1Noch keine Bewertungen
- Neonatal JaundiceDokument36 SeitenNeonatal JaundiceJenaffer Achamma JohnNoch keine Bewertungen
- Breech PresentationDokument85 SeitenBreech Presentationwidya vannesaNoch keine Bewertungen
- Assessment of Fetal Well-BeingDokument63 SeitenAssessment of Fetal Well-BeingArhum Siddiqi100% (1)
- Low Birth Weight Feeding: Neocon Nursing Workshop 2021 DR Jyothi Prabhakar Consultant KIMSDokument40 SeitenLow Birth Weight Feeding: Neocon Nursing Workshop 2021 DR Jyothi Prabhakar Consultant KIMSAswathy RCNoch keine Bewertungen
- Division of Perinatology Department of Child Health Medical School University of Sumatera UtaraDokument37 SeitenDivision of Perinatology Department of Child Health Medical School University of Sumatera UtaraJosephine IrenaNoch keine Bewertungen
- Lecture 11 Failure To Thrive (FTT)Dokument25 SeitenLecture 11 Failure To Thrive (FTT)jaish8904100% (2)
- Golden Hours Management of High Risk Newborns - 2019Dokument10 SeitenGolden Hours Management of High Risk Newborns - 2019Suryadi LimardiNoch keine Bewertungen
- 17 Normal PuerperiumDokument12 Seiten17 Normal PuerperiumAhmed TarigNoch keine Bewertungen
- Breast FeedingDokument3 SeitenBreast FeedingArla Donissa-Donique Castillon AlviorNoch keine Bewertungen
- PREMATURITYDokument27 SeitenPREMATURITYHamizi MD HanapiahNoch keine Bewertungen
- Neonatal ResuscitationDokument138 SeitenNeonatal ResuscitationAbcdeNoch keine Bewertungen
- Amniotic FluidDokument34 SeitenAmniotic Fluidannu panchalNoch keine Bewertungen
- Postpartum Hemorrhage (PPH)Dokument12 SeitenPostpartum Hemorrhage (PPH)Asteway MesfinNoch keine Bewertungen
- Harika Priyanka. K Asst. Professor AconDokument30 SeitenHarika Priyanka. K Asst. Professor AconArchana MoreyNoch keine Bewertungen
- Birth AsphyxiaDokument26 SeitenBirth Asphyxiawizborrlyzo006Noch keine Bewertungen
- Thromboembolic Disease in Pregnancy د.علية شعيبDokument50 SeitenThromboembolic Disease in Pregnancy د.علية شعيبMohammad Belbahaith0% (1)
- Neonatal Jaundice (Wong)Dokument54 SeitenNeonatal Jaundice (Wong)Siti Hajar100% (1)
- Newborn of A Diabetic Melitus MotherDokument22 SeitenNewborn of A Diabetic Melitus MotherDennis MiritiNoch keine Bewertungen
- Neonatal PneumoniaDokument16 SeitenNeonatal Pneumoniaelyuchan100% (1)
- Management of Paediatric Diabetic KetoacidosisDokument21 SeitenManagement of Paediatric Diabetic KetoacidosisAsad M AminNoch keine Bewertungen
- Hyperbiribunemia: Tjakrapawira, Agnes Yarte, DanaDokument23 SeitenHyperbiribunemia: Tjakrapawira, Agnes Yarte, DanaByrn Yarte100% (1)
- LBW, Care & FeedingDokument34 SeitenLBW, Care & FeedingManju KumariNoch keine Bewertungen
- Neonatal JaundiceDokument45 SeitenNeonatal JaundiceDrhassan HuseinNoch keine Bewertungen
- Essential Newborn CareDokument14 SeitenEssential Newborn CareJam Corros100% (1)
- 5 Asphyxia NeonetrumDokument27 Seiten5 Asphyxia NeonetrumRana VandanaNoch keine Bewertungen
- ITISMITA Biswal MSC, Nursing 2 YearDokument48 SeitenITISMITA Biswal MSC, Nursing 2 YearGandimareiNoch keine Bewertungen
- Infants Diabetic MothersDokument17 SeitenInfants Diabetic MothersJaya PrabhaNoch keine Bewertungen
- P PyrexiaDokument23 SeitenP PyrexiaRex BishopNoch keine Bewertungen
- Birth InjuriesDokument11 SeitenBirth Injuriesdapurna86Noch keine Bewertungen
- Presentation Aids and HivDokument27 SeitenPresentation Aids and HivLamnunnem HaokipNoch keine Bewertungen
- Newborn ResuscitationDokument7 SeitenNewborn ResuscitationYwagar YwagarNoch keine Bewertungen
- Neonatal Hypoglycemia (Infant of Diabetic Mother)Dokument15 SeitenNeonatal Hypoglycemia (Infant of Diabetic Mother)diana rossNoch keine Bewertungen
- Congenital AnomaliesDokument22 SeitenCongenital Anomaliesjessy100% (1)
- IUGRDokument33 SeitenIUGRPantas Saroha SiburianNoch keine Bewertungen
- Developed by D. Ann Currie, RN, MSNDokument40 SeitenDeveloped by D. Ann Currie, RN, MSNtri utamiNoch keine Bewertungen
- Jaundice-Neonatal 2016Dokument45 SeitenJaundice-Neonatal 2016Awatef AbushhiwaNoch keine Bewertungen
- Perinatal and Neonatal MortalityDokument40 SeitenPerinatal and Neonatal MortalityDuncan Jackson0% (1)
- Follow-upoftheNICUPatient Medscape FormatDokument65 SeitenFollow-upoftheNICUPatient Medscape FormatJohn ParudaNoch keine Bewertungen
- Threatened AbortionDokument1 SeiteThreatened AbortionKEn PilapilNoch keine Bewertungen
- Neonatal JaundiceDokument72 SeitenNeonatal JaundiceThya HakimNoch keine Bewertungen
- Maisel S 2012Dokument5 SeitenMaisel S 2012marsyaNoch keine Bewertungen
- Infant of A Diabetic MotherDokument17 SeitenInfant of A Diabetic MotherLovina Falendini AndriNoch keine Bewertungen
- Infant of Diabetic Mother: DR: Eman Khammas Al-SadiDokument60 SeitenInfant of Diabetic Mother: DR: Eman Khammas Al-SadiEman KhammasNoch keine Bewertungen
- Asphyxia NeonatorumDokument35 SeitenAsphyxia NeonatorumMuhammad RagilNoch keine Bewertungen
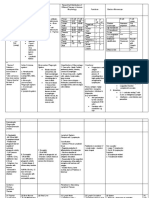
- Infection in NeonateDokument28 SeitenInfection in Neonateamel015Noch keine Bewertungen
- Lecture Notes On AphDokument41 SeitenLecture Notes On AphEyob MizanNoch keine Bewertungen
- Exercises To Facilitate Change of Baby's Position From Breech To CephalicDokument3 SeitenExercises To Facilitate Change of Baby's Position From Breech To CephalicaziskarnNoch keine Bewertungen
- Birth Injuries: Dr. Alsayed Alsharkawy Senior Pediatric Lecturer Widad University CollegeDokument35 SeitenBirth Injuries: Dr. Alsayed Alsharkawy Senior Pediatric Lecturer Widad University CollegeEllis NabilaNoch keine Bewertungen
- Fetal MalpositionDokument14 SeitenFetal MalpositionMiche DairoNoch keine Bewertungen
- Care of The Pregnant Woman With HIVDokument34 SeitenCare of The Pregnant Woman With HIVJenelle Melinda TullochNoch keine Bewertungen
- Amniotic Fluid & Its AbnormalitiesDokument29 SeitenAmniotic Fluid & Its AbnormalitiesSTAR Plus SerialsNoch keine Bewertungen
- Partograph DR OdofinDokument61 SeitenPartograph DR OdofinEkiran BabajideNoch keine Bewertungen
- Febrile Seizure Case FileDokument4 SeitenFebrile Seizure Case Filehttps://medical-phd.blogspot.comNoch keine Bewertungen
- Fanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsVon EverandFanconi Anemia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNoch keine Bewertungen
- The Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesVon EverandThe Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesNoch keine Bewertungen
- Fetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsVon EverandFetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsPeter RolfeNoch keine Bewertungen
- Endocrine PancreasDokument21 SeitenEndocrine Pancreaslacafey741Noch keine Bewertungen
- BGH Case SlipsDokument7 SeitenBGH Case SlipsLoungayvan BatuyogNoch keine Bewertungen
- Chandy C. John - Advances in The Diagnosis and Treatment of Pediatric Infectious Diseases - 2013Dokument212 SeitenChandy C. John - Advances in The Diagnosis and Treatment of Pediatric Infectious Diseases - 2013Alla AlkateebNoch keine Bewertungen
- Gambaran Penemuan Kasus Tuberkulosis Paru Oleh Petugas Puskesmas Di Kabupaten SukoharjoDokument8 SeitenGambaran Penemuan Kasus Tuberkulosis Paru Oleh Petugas Puskesmas Di Kabupaten SukoharjoBenti Eka WatiNoch keine Bewertungen
- Final Diabetes & Its Role in PeriodonticsDokument140 SeitenFinal Diabetes & Its Role in Periodonticsvinay jainNoch keine Bewertungen
- Desain Tanpa JudulDokument1 SeiteDesain Tanpa Judulsuci maharaNoch keine Bewertungen
- Prospect Port A Cath PDFDokument95 SeitenProspect Port A Cath PDFbogdan5ene5564Noch keine Bewertungen
- Seizure Disorders: Assessment and Diagnostic FindingsDokument3 SeitenSeizure Disorders: Assessment and Diagnostic FindingsBlessed GarcianoNoch keine Bewertungen
- بنك الأسئلةDokument775 Seitenبنك الأسئلةسماح صلاح100% (1)
- Medical Terms and Definitons Commonly Used in MCNDokument15 SeitenMedical Terms and Definitons Commonly Used in MCNjoemel gregoriNoch keine Bewertungen
- Contact Urticaria Syndrome: Occupational Aspects: Becky S. Li, Iris S. Ale, and Howard I. MaibachDokument34 SeitenContact Urticaria Syndrome: Occupational Aspects: Becky S. Li, Iris S. Ale, and Howard I. MaibachsaskiakonitaNoch keine Bewertungen
- Pharmacology Test 1Dokument39 SeitenPharmacology Test 1Niki BolinNoch keine Bewertungen
- Analisis Lama Waktu Pelayanan Laboratorium Di Rumah Sakit Umum Daerah Pasaman BaratDokument8 SeitenAnalisis Lama Waktu Pelayanan Laboratorium Di Rumah Sakit Umum Daerah Pasaman Baratdina filanNoch keine Bewertungen
- The European Guideline On Management of Major Bleeding and Coagulopathy Following Trauma Sixth Edition (2023) PDFDokument1 SeiteThe European Guideline On Management of Major Bleeding and Coagulopathy Following Trauma Sixth Edition (2023) PDFMatheus LiraNoch keine Bewertungen
- Ophthalmology: Cycloplegic Refraction in Children With Cyclopentolate Versus AtropineDokument6 SeitenOphthalmology: Cycloplegic Refraction in Children With Cyclopentolate Versus AtropineKiara NurmathiasNoch keine Bewertungen
- 2003 HemaDokument19 Seiten2003 Hemahavana1975Noch keine Bewertungen
- BernottiDokument44 SeitenBernottiAlexandra Alexandra100% (2)
- Exchange Blood Transfusion 2Dokument15 SeitenExchange Blood Transfusion 2Sarah100% (1)
- Women The Skilled Architect of The SocietyDokument4 SeitenWomen The Skilled Architect of The SocietyInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Vaccination Certificate 20435699572410Dokument1 SeiteVaccination Certificate 20435699572410MANOJ BHADANENoch keine Bewertungen
- Ontogeny and Phylogeny of Immune SystemDokument3 SeitenOntogeny and Phylogeny of Immune SystemPM Basiloy - AloNoch keine Bewertungen
- Polysomnography (PSG) : Patient Information Patient InformationDokument12 SeitenPolysomnography (PSG) : Patient Information Patient Informationhotland sitorusNoch keine Bewertungen
- 33rd IACDE National Conference 2018 - VijayawadaDokument5 Seiten33rd IACDE National Conference 2018 - VijayawadaHari PriyaNoch keine Bewertungen
- PWD Id GuideDokument3 SeitenPWD Id GuideErickson MasNoch keine Bewertungen
- Functional Gastrointestinal Disorders History Pathophysiology Clinical Features and Rome IVDokument20 SeitenFunctional Gastrointestinal Disorders History Pathophysiology Clinical Features and Rome IVwenyinriantoNoch keine Bewertungen
- SWAN Parkinson MRIDokument9 SeitenSWAN Parkinson MRIulfi yunitaNoch keine Bewertungen