Beruflich Dokumente
Kultur Dokumente
CH 29
Hochgeladen von
Jann Zaniel Allayne RiOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
CH 29
Hochgeladen von
Jann Zaniel Allayne RiCopyright:
Verfügbare Formate
Chapter 29: Renal Regulation of K, Ca, P, and Mg; Integration of Renal Mechanisms for Control of Blood Volume and
ECF Volume
Guyton and Hall, Textbook of Medical Physiology, 12th edition
Regulation of ECF Potassium Concentration and Excretion Regulation of Internal K Distribution a. Insulin stimulates K uptake into cells b. Aldosterone increases K uptake into cells c. Beta-adrenergic stimulation increases cellular uptake d. Acid-base abnormalities changes distribution e. Cell lysis causes increased extracellular K concentration f. Strenuous exercise causes hyperkalemia by releasing K from skeletal muscles g. Increased ECF osmolarity causes redistribution of K from cells to the ECF
Fig. 29.1 Normal potassium intake, distribution of potassium in the body fluids, and potassium output from the body
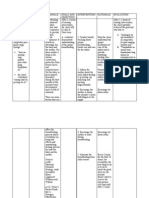
Table. 29.1 Factors that can alter potassium distribution between the intracellular and extracellular fluids Factors That Shift K into Cells and Decrease Extracellular K Concentration Factors That Shift K out of Cells and Increase Cellular K Concentration
Insulin Aldosterone Beta-adrenergic stimulation Alkalosis
Insulin deficiency (diabetes) Aldosterone deficiency (Addisons) Beta-adrenergic blockade Acidosis Cell lysis Strenuous exercise
Increased ECF osmolarity
Overview of Renal Potassium Excretion
Renal Potassium Excretion- determined by the sum of three processes
a. The rate of K filtration (GFR X plasma K conc. b. The rate of K reabsorption by the tubules c. The rate of K secretion by the tubules
Overview of Renal Potassium Excretion
Fig. 29.2
Overview of Renal Potassium Excretion (cont.) K Secretion by Principal Cells of Late Distal and Cortical Collecting Tubules
Fig. 29.3
Summary of Factors That Regulate Potassium Increased ECF Potassium Concentration Stimulates Potassium Secretion
Fig. 29.4
Summary of Factors That Regulate Potassium Aldosterone Stimulates Potassium Secretion Increased Extracellular Potassium Ion Concentration Stimulates Aldosterone Secretion
Fig. 29.5
Fig. 29.6 Basic feedback mechanism for control of ECF potassium concentration by aldosterone
Fig. 29.7 Primary mechanisms by which high potassium intake raises potassium excretion
Summary of Potassium Regulation (cont.) Blockade of Aldosterone Feedback System Impairs Control of Potassium Concentration
Fig. 29.8
Summary of Potassium Regulation (cont.) Increased Distal Tubular Flow Rate Stimulates Potassium Secretion
Fig. 29.9
Fig. 29.10 Effect of high sodium intake on renal excretion of potassium
Control of Renal Calcium Excretion and Extracellular Calcium Ion Concentration
50% of plasma calcium is in ionized form Intake must be balanced with net loss 99% of the bodys calcium is stored in bone Bone, therefore, is the primary reservoir of calcium PTH is one of the most important regulators of calcium release
Control of Renal Calcium Excretion and Extracellular Calcium Ion Concentration
PTH regulates through 3 main effects a. Stimulating bone resorption b. Stimulate activation of vitamin D which increases intestinal reabsorption of calcium
c. Directly increasing renal tubular calcium reabsorption
Control of Renal Calcium Excretion and Extracellular Calcium Ion Concentration
Fig. 29.11 Compensatory responses to decreased plasma ionized calcium concentration mediated by parathyroid hormone (PTH) and vitamin D
Control of Calcium Excretion By the Kidneys
Proximal Tubular Calcium Reabsorption a. Most occurs through the paracellular pathway dissolved in water
b. 20% occurs through a transcellular pathway
Control of Calcium Excretion By the Kidneys
Fig. 29.12 Mechanisms of calcium reabsorption by paracellular and transcellular pathways in the proximal tubular cells
Control of Calcium Excretion By the Kidneys
Loop of Henle and Distal Tubule Calcium Reabsorption
a. Restricted to the thick ascending limb of the Loop
b. Almost entirely by active transport in the distal tubule
Control of Calcium Excretion By the Kidneys Factors That Regulate Tubular Calcium Reabsorption
Table. 29.2 Factors that alter renal calcium excretion
Decreased Ca Excretion
Increased Parathyroid hormone Decreased ECF volume Decreased blood pressure Increased plasma phosphate Metabolic acidosis Vitamin D3
Increased Ca Excretion
Decreased Parathyroid hormone Increased ECF volume Increased blood pressure Decreased plasma phosphate Metabolic alkalosis
Regulation of Renal Phosphate Excretion Proximal tubule normally reabsorbs 75-80% of the filtered phosphate Distal tubule reabsorbs approx. 10% 10% excreted through the urine When plasma PTH is increased, phosphate reabsorption is decreased and excretion is increased
Regulation of Renal Magnesium More than 50% of the bodys Mg is stored in bones Primary reabsorption site is the loop of Henle Following lead to increased Mg excretion: a. Increased ECF Mg concentration b. ECF expansion c. Increased ECF Ca concentration
Regulation of Sodium Sodium Intake and Excretion are Matched Under Steady-State Conditions Sodium Excretion is Controlled by Altering GFR or Tubular Na reabsorption rate
Regulation of Sodium Importance of Pressure Natriuresis and Pressure Diuresis in Maintaining Body Na and Fluid Balance
Fig. 29.13 Acute and chronic effects of arterial pressure on sodium output by the kidneys (pressure natriuresis)
Regulation of Sodium Pressure Natriuresis and Diuresiskey components of feedback mechanism for regulating body fluid volumes and arterial pressure
Fig. 29.14
Fig. 29.15 Approximate effect of changes in daily fluid intake on blood volume
Precision of Blood Volume and ECF Volume Regulation
Blood volume remains almost exactly constant despite extreme changes in daily fluid intake (Fig. 29.14); the reason is a. A slight change in blood volume causes a marked change in cardiac output b. A slight change in CO causes a large change in blood pressure c. A slight change in BP causes a large change in urine output
Distribution of ECF
Fig. 29.16 Approximate relation between ECF and blood volume
Distribution of ECF Principal Factors That Can Cause Accumulation of Fluid in Interstitial Spaces a. Increased capillary hydorstatic pressure
b. Decreased plasma colloid osmotic pressure
c. Increased permeability of the capillaries
d. Obstruction of lymphatic vessels
Nervous and Hormonal Factors Increase the Effectiveness of Renal-Body Fluid Feedback Control SNS Control of Renal Excretion: arterial baroreceptor and low-pressure stretch receptor reflexes Role of Angiotensin II in Controlling Renal Excretion a. When Na intake is elevated above normal, renin secretion is decreased, causing decreased angiotensin II formation b. When Na intake is reduced below normal, increased angiotensin II causes Na and water retention
Importance of Changes in Angiotensin II in Altering Pressure Natriuresis
Fig. 29.17 Effects of excessive angiotensin II formation and blocking angiotensin II formation on the renal pressure natriuresis curve
Angiotensin II (cont.)
Excessive Angiotensin IIdoes not usually cause large increases in ECF volume Increased Arterial Pressure Counterbalances Angiotensin II Mediated Sodium Retention
Role of Aldosterone in Renal Excretion
Aldosterone Increases Sodium Reabsorption Reduction in Sodium Intake- increased angiotensin II stimulate aldosterone secretion Increase in Sodium Intake- suppression of aldosterone decreases tubular reabsorption, allowing increased Na excretion
Role of Aldosterone (cont.)
During Chronic Oversecretion of Aldosterone, the Kidneys Escape From Na Retention as Arterial Pressure Rises a. Caused by tumors of the adrenal gland b. Caused by Addisons disease
Nervous and Hormonal Factors (cont.)
Role of ADH in Controlling Renal Water Excretion a. Excess ADH secretion usually causes only small increases in ECF volume but large decreases in sodium concentration Role of Atrial Natriuretic Peptide a. Causes a small increase in GFR and decreases in Na reabsorption
Integrated Responses to Changes in Na Intake
High Sodium Intake a. Activation of low pressure receptor reflexes b. Suppression of angiotensin II formation c. Stimulation of natriuretic systems d. Small increases in arterial pressure
Conditions That Cause Large Increases in Blood and ECF Volumes
Increased Blood Volume and ECF Volume Caused By Heart Diseases Increased Blood Volume Caused By Increased Capacity of Circulation
Conditions That Cause Large Increases ECF Volume But With Normal Blood Volume Nephrotic Syndrome- loss of plasma proteins in urine and sodium retention by the kidneys Liver Cirrhosis- decreased synthesis of plasma proteins by the liver and sodium retention by the kidneys
Das könnte Ihnen auch gefallen
- Acid-Base and Electrolyte Handbook for Veterinary TechniciansVon EverandAcid-Base and Electrolyte Handbook for Veterinary TechniciansAngela Randels-ThorpNoch keine Bewertungen
- 4 ElectrolyteDokument30 Seiten4 ElectrolytePesan IslamNoch keine Bewertungen
- Equine Fluid TherapyVon EverandEquine Fluid TherapyC. Langdon FieldingNoch keine Bewertungen
- Endocrine 3Dokument115 SeitenEndocrine 3Dessalegn LemmaNoch keine Bewertungen
- Potassium Homeostasis and Causes of Hypo/HyperkalemiaDokument47 SeitenPotassium Homeostasis and Causes of Hypo/HyperkalemiaMayuresh ChaudhariNoch keine Bewertungen
- Adrenal Gland by Dr. Rajnee IInd PartDokument30 SeitenAdrenal Gland by Dr. Rajnee IInd Part9460106212Noch keine Bewertungen
- Renal Regulation of Extracellular Fluid Potassium ConcentrationDokument32 SeitenRenal Regulation of Extracellular Fluid Potassium ConcentrationDaniel AdamsNoch keine Bewertungen
- Causes and Evaluation of Hyperkalemia in Adults - UpToDate PDFDokument42 SeitenCauses and Evaluation of Hyperkalemia in Adults - UpToDate PDFRoberto PenedoNoch keine Bewertungen
- Regulation of Water & Electrolytes Balance: By: Husnil KadriDokument41 SeitenRegulation of Water & Electrolytes Balance: By: Husnil KadrimarsyaNoch keine Bewertungen
- Metabolic AlkalosisDokument54 SeitenMetabolic AlkalosispriyankagalhotraNoch keine Bewertungen
- Potassium BalanceDokument13 SeitenPotassium BalancePhysiology by Dr Raghuveer100% (1)
- Disorders of Calcium, Inorganic Phosphate and Magnesium Metabolism 1Dokument62 SeitenDisorders of Calcium, Inorganic Phosphate and Magnesium Metabolism 1IiiNoch keine Bewertungen
- Renal Failure Overview PPP 3Dokument31 SeitenRenal Failure Overview PPP 3Mudassar SattarNoch keine Bewertungen
- Pathogenesis, Diagnosis and Management of Hyperkalemia: Educational ReviewDokument8 SeitenPathogenesis, Diagnosis and Management of Hyperkalemia: Educational ReviewAlvaro FloresNoch keine Bewertungen
- Regulation of calcium, Parathyroid hormone, Vitamin D & CalcitoninDokument29 SeitenRegulation of calcium, Parathyroid hormone, Vitamin D & CalcitoninJessica StewartNoch keine Bewertungen
- POTASSIUM HOMEOSTASIS كيمياء سريريةDokument4 SeitenPOTASSIUM HOMEOSTASIS كيمياء سريريةMustafa Salah MahdiNoch keine Bewertungen
- Hypokalemia Case StudyDokument10 SeitenHypokalemia Case StudyJib SinsuatNoch keine Bewertungen
- SodiumDokument48 SeitenSodiumSanchita SahaNoch keine Bewertungen
- Basic Metabolic PanelDokument11 SeitenBasic Metabolic PanelLaurenNoch keine Bewertungen
- Dangerous Rhythms Tachycardia: Potassium Electrolyte HypokalemiaDokument7 SeitenDangerous Rhythms Tachycardia: Potassium Electrolyte HypokalemiagorodoeNoch keine Bewertungen
- Metabolic AlkalosisDokument15 SeitenMetabolic AlkalosisMenna ElesawyNoch keine Bewertungen
- Electrolyte&Fluid Balance Simple DR - Dicky, SPPDDokument38 SeitenElectrolyte&Fluid Balance Simple DR - Dicky, SPPDGhadiz Fhydhya FadhillaNoch keine Bewertungen
- Hyperkalemia: Samir El AnsaryDokument43 SeitenHyperkalemia: Samir El AnsaryStrept PneumoniaNoch keine Bewertungen
- CH 28Dokument22 SeitenCH 28Jann Zaniel Allayne RiNoch keine Bewertungen
- Electrolytes and Arterial Blood Gases: James H. Harrison, JR., M.D., Ph.D. Center For Oncology and Pathology InformaticsDokument30 SeitenElectrolytes and Arterial Blood Gases: James H. Harrison, JR., M.D., Ph.D. Center For Oncology and Pathology InformaticsPierre FlorendoNoch keine Bewertungen
- HyperkalemiaDokument86 SeitenHyperkalemiaSuresh KumarNoch keine Bewertungen
- Physiology 1 Fluid ElectrolyteDokument38 SeitenPhysiology 1 Fluid ElectrolyteHaziq KamardinNoch keine Bewertungen
- Chapter30 PhysioDokument19 SeitenChapter30 Physioناديه صاحبNoch keine Bewertungen
- Acute Renal Failure: Dr. Bobi Ahmad S, S.KPDokument62 SeitenAcute Renal Failure: Dr. Bobi Ahmad S, S.KPdr.Bobi Ahmad Sahid, S.KepNoch keine Bewertungen
- Pathogenesis, Diagnosis and Management of Hyperkalemia PDFDokument9 SeitenPathogenesis, Diagnosis and Management of Hyperkalemia PDFJbarrianNoch keine Bewertungen
- Distribution of This Potassium Between The Extracellular and Intracellular FluidDokument9 SeitenDistribution of This Potassium Between The Extracellular and Intracellular FluidLovelle LopezNoch keine Bewertungen
- Hypokalemia Induced Renal DysfunctionDokument6 SeitenHypokalemia Induced Renal DysfunctionTessa AcostaNoch keine Bewertungen
- Regulation of Sodium, Chloride and Water BalanceDokument41 SeitenRegulation of Sodium, Chloride and Water BalanceReentsha EllyNoch keine Bewertungen
- Hypo Kale MiaDokument34 SeitenHypo Kale MiaSyafniYuliaSistriNoch keine Bewertungen
- HYPOKALEMIADokument41 SeitenHYPOKALEMIAsamudraandiNoch keine Bewertungen
- Renal Funcetion Part 3Dokument3 SeitenRenal Funcetion Part 3Dr-Dalya ShakirNoch keine Bewertungen
- Electrolyte Disorders: Understanding Sodium and Potassium HomeostasisDokument14 SeitenElectrolyte Disorders: Understanding Sodium and Potassium HomeostasisBayu Budi SukocoNoch keine Bewertungen
- Lanjujutan Jawaban CADokument2 SeitenLanjujutan Jawaban CAAciNoch keine Bewertungen
- Body Fluids: M. Alif Prizarky 04011381419173 GammaDokument7 SeitenBody Fluids: M. Alif Prizarky 04011381419173 GammaAlviss RmidNoch keine Bewertungen
- Seminar RDokument93 SeitenSeminar Rmubarak abdulkadirNoch keine Bewertungen
- c15 Diuretic AgentsDokument13 Seitenc15 Diuretic AgentsmohammadNoch keine Bewertungen
- Pharmacology of Renal System Components of Renal System: Kidneys Ureters Urinary Bladder UrethraDokument30 SeitenPharmacology of Renal System Components of Renal System: Kidneys Ureters Urinary Bladder UrethraMirza HassanNoch keine Bewertungen
- RenalDokument8 SeitenRenalLoislane RullNoch keine Bewertungen
- Acid-base and hydromineral balance regulationDokument55 SeitenAcid-base and hydromineral balance regulationVio MincuNoch keine Bewertungen
- Describe Potassium Homeostasis in The Body and Its Functional ImportanceDokument2 SeitenDescribe Potassium Homeostasis in The Body and Its Functional ImportanceDhruvalNoch keine Bewertungen
- Gangguan Dan Keseimbangan Cairan Dan ElektrolitDokument37 SeitenGangguan Dan Keseimbangan Cairan Dan ElektrolitFyana PutriNoch keine Bewertungen
- Support of Renal Function: A Guide to Acute Renal Failure, Anatomy, Physiology and RegulationDokument86 SeitenSupport of Renal Function: A Guide to Acute Renal Failure, Anatomy, Physiology and RegulationRo-Anne LozadaNoch keine Bewertungen
- Approach To PT With HypokalemiaDokument14 SeitenApproach To PT With HypokalemiaTauhidul IslamNoch keine Bewertungen
- HiperkalemiaDokument41 SeitenHiperkalemiaJansonNoch keine Bewertungen
- Acid-Base Disorders NotesDokument10 SeitenAcid-Base Disorders NotesLovely100% (1)
- A Share WATER & ELECTROLYTE BALANCEDokument14 SeitenA Share WATER & ELECTROLYTE BALANCENaaz creates creativeNoch keine Bewertungen
- Disorders of Fluid and Electrolyte BalanceDokument71 SeitenDisorders of Fluid and Electrolyte BalanceIiiNoch keine Bewertungen
- Chapter 2 Electrolytes and Body Fluid AnalysiDokument103 SeitenChapter 2 Electrolytes and Body Fluid AnalysiSanyii MamuyeNoch keine Bewertungen
- Keseimbangan Cairan: Jurusan Analis Kesehatan Politeknik Kesehatan YogyakartaDokument75 SeitenKeseimbangan Cairan: Jurusan Analis Kesehatan Politeknik Kesehatan YogyakartaAndri HaryonoNoch keine Bewertungen
- Causes and Evaluation of Hyperkalemia in AdultsDokument25 SeitenCauses and Evaluation of Hyperkalemia in AdultsAnonymous iAoPnb2sNoch keine Bewertungen
- Metabolic AcidosisDokument1 SeiteMetabolic AcidosisLee June LyngNoch keine Bewertungen
- Cronic Kidney Disease (CKD) by RensiDokument50 SeitenCronic Kidney Disease (CKD) by RensiihdinzNoch keine Bewertungen
- Diuretics and Dialysis: DR Arpana HazarikaDokument104 SeitenDiuretics and Dialysis: DR Arpana HazarikaArpana HazarikaNoch keine Bewertungen
- Hyperkalemia: Samir El AnsaryDokument45 SeitenHyperkalemia: Samir El Ansarymariatul fithriasariNoch keine Bewertungen
- Electrolytes BalanceDokument13 SeitenElectrolytes BalanceMuhammad YounisNoch keine Bewertungen
- OPD census report for Feb 2018 with leading casesDokument1 SeiteOPD census report for Feb 2018 with leading casesJann Zaniel Allayne RiNoch keine Bewertungen
- Ankle SprainDokument55 SeitenAnkle SprainJann Zaniel Allayne RiNoch keine Bewertungen
- CH 28Dokument22 SeitenCH 28Jann Zaniel Allayne RiNoch keine Bewertungen
- CH 27Dokument40 SeitenCH 27Jann Zaniel Allayne RiNoch keine Bewertungen
- Report in Inborn Errors of Urea SynthesisDokument29 SeitenReport in Inborn Errors of Urea SynthesisJann Zaniel Allayne RiNoch keine Bewertungen
- Guyton and Hall Textbook Chapter 25: Body Fluid Compartments and Fluid BalanceDokument19 SeitenGuyton and Hall Textbook Chapter 25: Body Fluid Compartments and Fluid BalanceJann Zaniel Allayne RiNoch keine Bewertungen
- CH 30Dokument26 SeitenCH 30Jann Zaniel Allayne RiNoch keine Bewertungen
- CH 26Dokument40 SeitenCH 26Jann Zaniel Allayne RiNoch keine Bewertungen
- ChromatographyDokument3 SeitenChromatographyJann Zaniel Allayne RiNoch keine Bewertungen
- Congestive Heart FailureDokument2 SeitenCongestive Heart FailureJann Zaniel Allayne RiNoch keine Bewertungen
- Nerves and Muscles Both Initiate Their Activity Based On DepolarisationDokument1 SeiteNerves and Muscles Both Initiate Their Activity Based On DepolarisationJann Zaniel Allayne RiNoch keine Bewertungen
- Nerves and Muscles Both Initiate Their Activity Based On DepolarisationDokument1 SeiteNerves and Muscles Both Initiate Their Activity Based On DepolarisationJann Zaniel Allayne RiNoch keine Bewertungen
- DyosaakoDokument4 SeitenDyosaakoJann Zaniel Allayne RiNoch keine Bewertungen
- Cefazolin for Skin and Moderate Bacterial InfectionsDokument5 SeitenCefazolin for Skin and Moderate Bacterial InfectionsJann Zaniel Allayne RiNoch keine Bewertungen
- 1) How Does The Body Respond To Stressful ChallengesDokument57 Seiten1) How Does The Body Respond To Stressful ChallengesRitika SahniNoch keine Bewertungen
- AVIATION Flight Physiology: - Kirk Michael WebsterDokument56 SeitenAVIATION Flight Physiology: - Kirk Michael WebsterabriowaisNoch keine Bewertungen
- MastatisDokument15 SeitenMastatisJoven LorillaNoch keine Bewertungen
- 4th Term - G8 Daily Test (Biology) - MSDokument17 Seiten4th Term - G8 Daily Test (Biology) - MSMatthew EdbertNoch keine Bewertungen
- Sectiuni Si Radiografii - An I, Sem 2Dokument16 SeitenSectiuni Si Radiografii - An I, Sem 2Mihaela456Noch keine Bewertungen
- CH 01Dokument12 SeitenCH 01TahmidNoch keine Bewertungen
- Lactation Nation by Sarah Bird For Texas MonthlyDokument2 SeitenLactation Nation by Sarah Bird For Texas MonthlySarah BirdNoch keine Bewertungen
- Cardiovascular Notes - All in One FileDokument299 SeitenCardiovascular Notes - All in One FileHasan DiabNoch keine Bewertungen
- Chapter 13. Skin-"The Jack of All Trades": Exercise 1Dokument5 SeitenChapter 13. Skin-"The Jack of All Trades": Exercise 1Aditya SinhaNoch keine Bewertungen
- 4 Hodges and Tucker. Moving Differently in Pain. 2011Dokument9 Seiten4 Hodges and Tucker. Moving Differently in Pain. 2011ningaxshopNoch keine Bewertungen
- Nephrology - Internal Medicine, Dr. A. MowafyDokument64 SeitenNephrology - Internal Medicine, Dr. A. Mowafyrazan moneerNoch keine Bewertungen
- Immunology and Serology Lecture # 2: Overview of ImmunityDokument14 SeitenImmunology and Serology Lecture # 2: Overview of ImmunityBryan Michael BalunesNoch keine Bewertungen
- Santosh DevDokument45 SeitenSantosh Devdevdsantosh100% (1)
- Apraxia PDFDokument13 SeitenApraxia PDFAndré CantanhedeNoch keine Bewertungen
- Physiology of the Menstrual CycleDokument6 SeitenPhysiology of the Menstrual CyclegmindalanoNoch keine Bewertungen
- Multiple Organ Dysfunction SyndromeDokument4 SeitenMultiple Organ Dysfunction SyndromeJenny SisonNoch keine Bewertungen
- Benign Breast Conditions Malignant Breast Conditions: A: Breast Tissue. Connective Tissue, Fat TissueDokument1 SeiteBenign Breast Conditions Malignant Breast Conditions: A: Breast Tissue. Connective Tissue, Fat TissuedevilstNoch keine Bewertungen
- Adrenal Function, Adrenal Hyperfunction and HypofunctionDokument98 SeitenAdrenal Function, Adrenal Hyperfunction and HypofunctionAntony WaithakaNoch keine Bewertungen
- Digestive System GuideDokument25 SeitenDigestive System GuideprabuNoch keine Bewertungen
- TLE Grade-10-3rd-Quarter-Dll-PrDokument51 SeitenTLE Grade-10-3rd-Quarter-Dll-PrMartie AvancenaNoch keine Bewertungen
- Fisiologi Pengaturan Tekanan Darah SILBERNAGL 2Dokument6 SeitenFisiologi Pengaturan Tekanan Darah SILBERNAGL 221701101016 - Juliana Ayu NugrahaNoch keine Bewertungen
- Neurophysiology Systems of the Brain and Spinal CordDokument50 SeitenNeurophysiology Systems of the Brain and Spinal CordHomeground entertainmentNoch keine Bewertungen
- Sci 5 PPT q2 WK 1 Day 1-5 (Autosaved)Dokument93 SeitenSci 5 PPT q2 WK 1 Day 1-5 (Autosaved)renato.minaNoch keine Bewertungen
- Parts of The Human HeartDokument4 SeitenParts of The Human HeartKearly Joy VictorioNoch keine Bewertungen
- Abrevieri EchoDokument3 SeitenAbrevieri EchoAndreea MihaelaNoch keine Bewertungen
- Human Physiology Final ProjectDokument37 SeitenHuman Physiology Final ProjectAyesha MasoodNoch keine Bewertungen
- Anatomy & PhysiologyDokument12 SeitenAnatomy & PhysiologyTyrNoch keine Bewertungen
- Ineffective Breast FeedingDokument5 SeitenIneffective Breast Feedingcamilleandaj070575% (12)
- R E G U L A T I O N S: JohannesburgDokument24 SeitenR E G U L A T I O N S: JohannesburgdchunNoch keine Bewertungen
- Met Caz ClinicDokument57 SeitenMet Caz ClinicIndrecan AndreiNoch keine Bewertungen