Beruflich Dokumente
Kultur Dokumente
Cardiac Diseases in Pregnancy
Hochgeladen von
Honey May Rollan VicenteCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Cardiac Diseases in Pregnancy
Hochgeladen von
Honey May Rollan VicenteCopyright:
Verfügbare Formate
Cardiovascular Disease In
Pregnancy
It is a relatively common in women of child bearing
age, complicate about 1% of pregnancies
Maternal mortality related to heart disease has
decreased remarkably over the past 50 years (from 5.6
to 0.3/100 000 live birth)
Heart disease are still the second most common non
obstetrical cause of maternal mortality.
Cardiac Diseases
Rheumatic heart disease
Congenital heart disease
Hypertensive heart disease
Coronary
Thyroid
Syphilitic
Kyphoscoliotic cardiac disease
Idiopathic cardiomyopathy
Corpulmonale
Constrictive pericarditis
Heart block
Isolated myocarditis
Physiological Consideration with Heart
Disease In Pregnancy
The most important changes in cardiac function occurs in
the first 8 weeks of pregnancy with maximum changes at
28 weeks
Vascular resistance
Blood pressure
Heart rate Stroke volume COP
Blood volume 30% - 50%
Maternal weight and basal metabolic rate also affect COP
cont
Later in pregnancy COP is higher when women is in the
lateral recumbent position than when she is in the supine
During labor COP increase moderately in the first stage
of labor and appreciably greater in the second stage
COP also increase in the immediate post partum period
cont
Heart:
The heart is displaced upward and to the left with lateral
rotation on its long axis
Resting pulse increase by about 10 bpm
There is some changes in the cardiac sounds include:
An exaggerated splitting of the first heart sound with
increase loudness of both components, no definite
changes in the aortic and pulmonary elements of the
second sound, and aloud easily heard third sound
conti.
Systolic murmur is heard in 90 % of cases
Soft diastolic murmur transiently in 20 %
Continuous murmur arising from the breast vasculature
in10 % of cases
Diagnosis of Heart Disease
Some clinical indicators of heart disease during
Pregnancy
Symptoms:
Progressive dyspnea or orthopnea
Nocturnal cough
Hemoptysis
Syncope
Chest pain
Clinical findings
Cyanosis
Clubbing of fingers
persistent neck vein distension
Systolic murmur grade 3/6 or greater
Diastolic murmur
Cardiomegaly
Persistent arrhythmia
Persistent split-second sound
Criteria for pulmonary hypertension
Diagnostic studies
Electrocardiography
An average 15 degree left axis deviation in the
ECG , and mild ST changes may be seen in the
inferior leads, Atrial and ventricular premature
contractions are relatively frequent
Chest x ray:
Heart silhouette normally is larger in pregnancy,
however gross cardiomegaly can be excluded
Echocardiography:
Normal changes include : Tricuspid regurgitation ,
Significantly increase left atrial size and left
ventricular outflow cross sectional area.
Clinical clssification
The New York Heart Associations Functional
Classification [ NYHA] First published in 1928
Class 1 : Uncompromised , no limitation of physical
activity
Class 2 : Slightly compromised , slight limitation of
physical activity
Class 3 : Markedly compromised , marked limitation
of physical activity
Class 4 : Severely compromised , inability to perform
any physical activity without discomfort
Preconceptional counseling
Maternal mortality generally varies directly with
functional classification at pregnancy onset;
However this relationship may change as pregnancy
progresses
Patient with pulmonary hypertension, primary or
secondary are in danger of undergoing decompensation
during pregnancy
cont
Life threatening cardiac abnormalities can be reversed
by corrective surgery and subsequent pregnancy is
less dangerous
In other cases fetal consideration predominate, for
example the teratogenic effect of warfarin
Risks for Maternal Mortality Caused by Various Heart
Disease
Cardiac Disorder Mortality %
Group 1 Minimal Risk
Atrial septal defect 0 -1 %
Ventricular septal defect
Patent ductus arteriosus
Pulmonic or tricuspid disease
Fallot tetralogy,corrected
Bioprosthetic valve
Mitral stenosis,NYHA classes 1&2
Group 2 Moderate Risk 5 -15 %
2A :
Mitral stenosis , NYHA classes 3 & 4
Aortic stenosis
Aortic coarctation without valvar involvement
Fallot tetralogy , uncorrected
Previous myocardial infarction
Marfan syndrome , normal aorta
2B :
Mitral stenosis with atrial fibrillation
Artificial valve
Group 3 Major Risk 25 -50 %
Pulmonary hypertension
Aortic coarctation with valvar involvement
Marfan syndrome with aortic involvement
NYHA = New York Heart Association.
From the American College of Obstetrics and Gynecologists
(1992a ) , with permission .
Management
In assuring an optimal outcome , management should
be a team approach involving ;obstetrician, cardiologist
and anesthesiologist
Risk to patient of : Heart failure, subacute bacterial
endocarditis, and thromboembolic disease will be
identified and minimized
Management
Four concepts that affect management are emphasized
by the American College of Obs /Gyn :-
1) the 50% increase in blood volume and COP by the
early 3
rd
trimester
2) further fluctuation in volume and COP in the
peripartum period
3) a decline in systemic vascular resistance, reaching
a nadir in the 2
nd
trimester, and then rising to 20%
below normal by late pregnancy
4) hyprcoagulability of special importance in women
requiring anticoagulation in the non pregnant state
Management of Class 1 & 2
General measures:
_ avoid contact with persons who have respiratory
infection
_ pneumococcal and influenza vaccines are recommended
( patient with valvar heart disease)
_ cigarette smoking is prohibited
_ diet , avoidance of strenuous activity and avoidance of
anemia
management cont..
signs of heart failure:
persistent basilar rales
nocturnal cough
a sudden diminution in ability to carry
out usual duties
increasing dyspnea on exertion
attacks of smothering with cough
hemoptysis, progressive edema and
tachycardia
Management cont..
Labor and Delivery :
* vaginal delivery is preferred unless there is obstetrical
indication
* relief of pain with intravenous analgesics ,
continuous epidural analgesia is recommended for
most situation , but its contraindicated in patient with:
[ Intracardiac shunt , pulmonary hypertension , Aortic stenosis ] ,
to avoid the risk of maternal hypotension
* fluid balance and antibiotic prophylactic
* semi recumbent position with lateral tilt
* intensive medical management for any signs of
impending ventricular failure
[ pulse > 100 , RR > 24 , dyspnea ]
* expedite vaginal delivery
* close monitoring for the 3
rd
stage of labor
puerperium
* avoid complication of pph, anemia, infection
and thromboembolism
* delay the procedure of tubal sterilization until
it is obvious that the mother is a febrile, not
anemic and can ambulate without evidence
of distress
* option of contraceptive advise
Management of class 3&4
whether pregnancy should be undertaken
consider pregnancy interruption
prolonged hospitalization or bed rest
vaginal delivery is preferred
caesarian section delivery should be with the availability
of experience anesthetic support in a facility with
experience with complicated cardiac disease
Most common lesions:
_Rheumatic heart disease
Incidence of rheumatic fever is decreasing in developed
countries , It still remain the chief cause of serious mitral
valve disease in women,(3/4
th
of cases of mitral stenosis)
_Congenital Heart Disease:
many congenital heart lesions appear to be inherited as
polygenic characteristic , 10% of women with congenital
heart disease would give birth to similarly affected infants ,
50 % were concordant for the same anomaly
Peripartum cardiomyopathy :
this is a diagnosis of exclusion , it describe women
with peripartum heart failure with no apparent etiology,
symptoms of cardiac decompensation appear during
the last weeks of pregnancy or 1 to 6 months postpartum
obstetrical complications such as : preeclampsia, anemia
from blood loss , and infection either contribute or
precipitate heart failure
Prognosis :
favorable outcome for the mother with heart
disease depends upon the :
_ functional cardiac capacity
_ other complications that further increase cardiac load
_ quality of medical care provided
_ psychological and socioeconomical factors
Das könnte Ihnen auch gefallen
- Medical Terminology Practice SheetsDokument7 SeitenMedical Terminology Practice Sheetsmarcus colgrove100% (1)
- The Human Brain: Anatomy, Functions, and InjuryDokument42 SeitenThe Human Brain: Anatomy, Functions, and InjuryHoney May Rollan Vicente100% (1)
- The Brain Is Composed of The,, andDokument23 SeitenThe Brain Is Composed of The,, andMohd NizamNoch keine Bewertungen
- Classification of FracturesDokument26 SeitenClassification of FracturesHoney May Rollan VicenteNoch keine Bewertungen
- 3rd Stage ComplicationsDokument84 Seiten3rd Stage ComplicationsDream100% (1)
- InfertilityDokument24 SeitenInfertilitySimran JosanNoch keine Bewertungen
- Nicu ReportDokument66 SeitenNicu ReportEr Shah Rukh QadriNoch keine Bewertungen
- Heart Disease in PregnancyDokument20 SeitenHeart Disease in PregnancyAnironOrionNoch keine Bewertungen
- Heart Disease in PregnancyDokument14 SeitenHeart Disease in PregnancyManisha ThakurNoch keine Bewertungen
- AbortionDokument35 SeitenAbortionHoney May Rollan VicenteNoch keine Bewertungen
- Obstetric Emergencies and Anesthetic Management: Co-Ordinator: DR - Navab Singh (M.D.) Speaker: Dr. UdayDokument35 SeitenObstetric Emergencies and Anesthetic Management: Co-Ordinator: DR - Navab Singh (M.D.) Speaker: Dr. UdayKutumela MolebogengNoch keine Bewertungen
- Postnatal Assessment Tool M.SC NSGDokument12 SeitenPostnatal Assessment Tool M.SC NSGM. jehovah Nissie YeshalomeNoch keine Bewertungen
- Cervical IncompetenceDokument28 SeitenCervical IncompetenceHoney May Rollan Vicente100% (1)
- AMNIOCENTESISDokument9 SeitenAMNIOCENTESISSANCHAYEETA100% (1)
- List of Hospitals in Ahmedabad DistrictDokument190 SeitenList of Hospitals in Ahmedabad DistrictTushar Y. JaniNoch keine Bewertungen
- Lesson Plan on Postpartum Hemorrhage NursingDokument4 SeitenLesson Plan on Postpartum Hemorrhage Nursingpreet kaur100% (1)
- Apollo Hospital Case StudyDokument55 SeitenApollo Hospital Case StudyVaani Sharma100% (2)
- MENOPAUSE SEMINAR OBG MSC Nursing 1st YearDokument11 SeitenMENOPAUSE SEMINAR OBG MSC Nursing 1st YearVishwanath VisNoch keine Bewertungen
- My ThesisDokument46 SeitenMy ThesisManish SharmaNoch keine Bewertungen
- SEMINAR ON TUMOUR COMPLICATING PREGNANCYDokument22 SeitenSEMINAR ON TUMOUR COMPLICATING PREGNANCYMonika shankarNoch keine Bewertungen
- Neonatal Hematologic ConditionsDokument2 SeitenNeonatal Hematologic ConditionsDelphy Varghese100% (1)
- Seminar On Obstetrical EmergencieDokument21 SeitenSeminar On Obstetrical EmergencieJyothi RameshNoch keine Bewertungen
- Last Minute RevisionDokument108 SeitenLast Minute RevisionRahul All83% (6)
- HIV SeminarDokument20 SeitenHIV SeminarRoselineTiggaNoch keine Bewertungen
- Ectopic Pregnancy: Causes, Symptoms and Treatment Options Under 40 CharactersDokument45 SeitenEctopic Pregnancy: Causes, Symptoms and Treatment Options Under 40 CharactersHoney May Rollan VicenteNoch keine Bewertungen
- MATERNAL MORBIDITY, MORTALITY AND FERTILITY RATESDokument18 SeitenMATERNAL MORBIDITY, MORTALITY AND FERTILITY RATESmadhu.BNoch keine Bewertungen
- Records Maintained at Choithram College of NursingDokument3 SeitenRecords Maintained at Choithram College of Nursingkiran mahalNoch keine Bewertungen
- Lesson Plan On ResuscitationDokument17 SeitenLesson Plan On ResuscitationFarheen khanNoch keine Bewertungen
- Identification Data: A. Past Medical HistoryDokument12 SeitenIdentification Data: A. Past Medical HistoryPrernaSharmaNoch keine Bewertungen
- Care of Low Birth WeightDokument21 SeitenCare of Low Birth WeightPrernaSharmaNoch keine Bewertungen
- Peptic Duodenal Ulcer History, Causes, Symptoms and TreatmentDokument106 SeitenPeptic Duodenal Ulcer History, Causes, Symptoms and TreatmentCanan YilmazNoch keine Bewertungen
- LESSON PLAN ON Hyper Emesis GravidarumDokument12 SeitenLESSON PLAN ON Hyper Emesis GravidarumMadhavi ModaNoch keine Bewertungen
- PIHDokument30 SeitenPIHPatcharavit PloynumponNoch keine Bewertungen
- Phototherapy On The Postnatal WardDokument5 SeitenPhototherapy On The Postnatal WardYwagar Ywagar100% (1)
- Introduction To Pediatric NursingDokument36 SeitenIntroduction To Pediatric Nursingcharan poonia100% (1)
- Teaching Methods and Evaluation in Family PlanningDokument9 SeitenTeaching Methods and Evaluation in Family PlanningDeepika PatidarNoch keine Bewertungen
- OB CH20 NotesDokument16 SeitenOB CH20 NotesVeronica EscalanteNoch keine Bewertungen
- Antenatal CareDokument82 SeitenAntenatal Caremdasad18Noch keine Bewertungen
- 001hypertensive Disorders in Pregnancy PDFDokument23 Seiten001hypertensive Disorders in Pregnancy PDFRosechelle Bas SamsonNoch keine Bewertungen
- Causes and Management of APHDokument42 SeitenCauses and Management of APHReena TyagiNoch keine Bewertungen
- Procedures ObgDokument12 SeitenProcedures Obgraghuram reddyNoch keine Bewertungen
- Postmature Infants 1Dokument13 SeitenPostmature Infants 1LyssaMarieKathryneEge100% (1)
- Disease Condition:: Hyperemsis Gravidarum: DefinitionDokument4 SeitenDisease Condition:: Hyperemsis Gravidarum: DefinitionPriyanka JohnNoch keine Bewertungen
- Question Bank PBBSC 1 Year Nursing SUBJECT: Child Health NursingDokument23 SeitenQuestion Bank PBBSC 1 Year Nursing SUBJECT: Child Health NursingYashoda SatputeNoch keine Bewertungen
- NCP2 - Active PhaseDokument14 SeitenNCP2 - Active PhasepriyankaNoch keine Bewertungen
- Causes and Treatment of Postpartum HemorrhageDokument29 SeitenCauses and Treatment of Postpartum Hemorrhagemedical chroniclesNoch keine Bewertungen
- Abnormalities of PuerperiumDokument70 SeitenAbnormalities of PuerperiumYasmin SharmaNoch keine Bewertungen
- Case Study On RDSDokument43 SeitenCase Study On RDSNeha Patel100% (1)
- Immediate Newborn Care (Autosaved)Dokument183 SeitenImmediate Newborn Care (Autosaved)mftaganasNoch keine Bewertungen
- Breast Problems After DeviveryDokument19 SeitenBreast Problems After DeviverySanthosh.S.UNoch keine Bewertungen
- MANAGEMENT OF HYDRAMNIOS AND OLIGOHYDRAMNIOSDokument12 SeitenMANAGEMENT OF HYDRAMNIOS AND OLIGOHYDRAMNIOSEaster Soma HageNoch keine Bewertungen
- Budgeting ConceptsDokument19 SeitenBudgeting ConceptsJitendra NagvekarNoch keine Bewertungen
- Diagnosis of PregnancyDokument16 SeitenDiagnosis of PregnancySùjâl PätídàrNoch keine Bewertungen
- Pregnancy Thyroid Disease 508Dokument12 SeitenPregnancy Thyroid Disease 508Ankush RanaNoch keine Bewertungen
- Govt. College of Nursing, Siddhpur Subject: Obstetrics Nursing Topic: High Risk PregnancyDokument36 SeitenGovt. College of Nursing, Siddhpur Subject: Obstetrics Nursing Topic: High Risk PregnancyJOSHI MITALINoch keine Bewertungen
- Nephro Case StudyDokument26 SeitenNephro Case Studyanimesh pandaNoch keine Bewertungen
- Antepartum Haemorrhage: Women's & Children's ServicesDokument4 SeitenAntepartum Haemorrhage: Women's & Children's ServicesYwagar YwagarNoch keine Bewertungen
- Extremely Low Birth Weight (ELBW) InfantDokument48 SeitenExtremely Low Birth Weight (ELBW) InfanthannanyusofNoch keine Bewertungen
- Birth AsphyxiaDokument26 SeitenBirth Asphyxiawizborrlyzo006Noch keine Bewertungen
- Lesson PlanDokument8 SeitenLesson PlanUpendra Nayka50% (2)
- Birth Injuries Nursing TeachingDokument24 SeitenBirth Injuries Nursing Teachingsaleha sultanaNoch keine Bewertungen
- Essential Obstetrical and Gynecological Skills (Iii Semester)Dokument5 SeitenEssential Obstetrical and Gynecological Skills (Iii Semester)RajaNoch keine Bewertungen
- Hyperbilirubinemia Teaching PlanDokument2 SeitenHyperbilirubinemia Teaching Planapi-25291041167% (3)
- Nursing EmpowermentDokument1 SeiteNursing Empowermentsudhakar pNoch keine Bewertungen
- What Is Pneumothorax?Dokument3 SeitenWhat Is Pneumothorax?Santhosh.S.U100% (1)
- Clinical Teaching 4PEUPERAL SEPSISDokument5 SeitenClinical Teaching 4PEUPERAL SEPSISAjit M Prasad PrasadNoch keine Bewertungen
- Nursing Audit MethodsDokument7 SeitenNursing Audit MethodsSam ParkNoch keine Bewertungen
- ITISMITA Biswal MSC, Nursing 2 YearDokument48 SeitenITISMITA Biswal MSC, Nursing 2 YearGandimareiNoch keine Bewertungen
- Charateristics of NewbornDokument3 SeitenCharateristics of NewbornRagupathyRamanjuluNoch keine Bewertungen
- Nursing Council extends staffing rulesDokument5 SeitenNursing Council extends staffing rulessrinivasanaNoch keine Bewertungen
- The Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesVon EverandThe Ideal Neutropenic Diet Cookbook; The Super Diet Guide To Replenish Overall Health For A Vibrant Lifestyle With Nourishing RecipesNoch keine Bewertungen
- SchizophreniaDokument25 SeitenSchizophreniaHoney May Rollan VicenteNoch keine Bewertungen
- Proper Patient Positioning Techniques in the ORDokument33 SeitenProper Patient Positioning Techniques in the ORshenric16Noch keine Bewertungen
- Head Injurires PresentationDokument93 SeitenHead Injurires PresentationHoney May Rollan VicenteNoch keine Bewertungen
- Brain Structure and FunctionDokument47 SeitenBrain Structure and FunctionRegel MarieNoch keine Bewertungen
- Work Related AsthmaDokument13 SeitenWork Related AsthmaHoney May Rollan VicenteNoch keine Bewertungen
- Gestational Trophoblastic Disease: Di WenDokument40 SeitenGestational Trophoblastic Disease: Di WenarshadmraziNoch keine Bewertungen
- DR AiaiDokument42 SeitenDR AiaiNava AinanieNoch keine Bewertungen
- Hearing Tests LectureDokument12 SeitenHearing Tests LectureHoney May Rollan VicenteNoch keine Bewertungen
- HIV and Pregnancy: Prevention of Mother-to-Child TransmissionDokument23 SeitenHIV and Pregnancy: Prevention of Mother-to-Child TransmissionHoney May Rollan VicenteNoch keine Bewertungen
- Work Related AsthmaDokument13 SeitenWork Related AsthmaHoney May Rollan VicenteNoch keine Bewertungen
- Communicable Disease ReportDokument23 SeitenCommunicable Disease ReportHoney May Rollan VicenteNoch keine Bewertungen
- Family Planning LetureDokument37 SeitenFamily Planning LetureHoney May Rollan VicenteNoch keine Bewertungen
- Urinary SystemDokument30 SeitenUrinary SystemHoney May Rollan VicenteNoch keine Bewertungen
- UrinaryDokument89 SeitenUrinaryHoney May Rollan VicenteNoch keine Bewertungen
- UrinaryDokument89 SeitenUrinaryHoney May Rollan VicenteNoch keine Bewertungen
- Diagnostic Tests For HIVDokument27 SeitenDiagnostic Tests For HIVJoshua SmithNoch keine Bewertungen
- Blood GroupDokument31 SeitenBlood GroupHoney May Rollan VicenteNoch keine Bewertungen
- Abruptio Placentae: Jeannet E. Canda, RN Nddu College of NursingDokument9 SeitenAbruptio Placentae: Jeannet E. Canda, RN Nddu College of NursingHoney May Rollan VicenteNoch keine Bewertungen
- Gestational Trophoblastic DiseaseDokument43 SeitenGestational Trophoblastic DiseaseHoney May Rollan VicenteNoch keine Bewertungen
- Placenta Previa: Jeannet E. Canda, RN Nddu College of NursingDokument15 SeitenPlacenta Previa: Jeannet E. Canda, RN Nddu College of NursingHoney May Rollan VicenteNoch keine Bewertungen
- BRAIN PresentationDokument17 SeitenBRAIN PresentationHoney May Rollan VicenteNoch keine Bewertungen
- Gestational Trophoblastic DiseaseDokument65 SeitenGestational Trophoblastic DiseaseHoney May Rollan VicenteNoch keine Bewertungen
- BRAIN PresentationDokument17 SeitenBRAIN PresentationHoney May Rollan VicenteNoch keine Bewertungen
- Indian Wound Care Market Overview Morulaa HealthTechDokument1 SeiteIndian Wound Care Market Overview Morulaa HealthTechSakshi KhuranaNoch keine Bewertungen
- Inguinal HerniaDokument27 SeitenInguinal HerniaNeneng WulandariNoch keine Bewertungen
- CRIB Score Predicts NICU MortalityDokument10 SeitenCRIB Score Predicts NICU MortalityFiaz medicoNoch keine Bewertungen
- Nama Putri Ramadani Kelas Xi Ipa 1: I Expression of PainDokument10 SeitenNama Putri Ramadani Kelas Xi Ipa 1: I Expression of PainJohn YoungNoch keine Bewertungen
- DAFO 4 SoftyDokument1 SeiteDAFO 4 SoftyaliaskarNoch keine Bewertungen
- Wvsu MC Org ChartDokument1 SeiteWvsu MC Org ChartquesterNoch keine Bewertungen
- رسائل القصر العينيDokument47 Seitenرسائل القصر العينيTaher ElBarbaryNoch keine Bewertungen
- Burkitt's LymphomaDokument22 SeitenBurkitt's LymphomaClementNoch keine Bewertungen
- Apex LocatorsDokument6 SeitenApex LocatorsbanupriyamdsNoch keine Bewertungen
- Anorectal ClinicalDokument17 SeitenAnorectal ClinicalEster Sibarani100% (1)
- Gastric Carcinoid After Long-Term Use of A Proton Pump InhibitorDokument6 SeitenGastric Carcinoid After Long-Term Use of A Proton Pump InhibitorBpmStfbNoch keine Bewertungen
- Respiration in Amphibians and ReptilesDokument10 SeitenRespiration in Amphibians and ReptilesNahrowiNoch keine Bewertungen
- SAUD VSD KonklinDokument91 SeitenSAUD VSD KonklinDedy Tesna AmijayaNoch keine Bewertungen
- Cep2020 Chapter03c HealthDokument10 SeitenCep2020 Chapter03c HealthLyan TejedoNoch keine Bewertungen
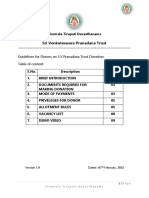
- Sri Venkateswara Pranadana Trust: Guidelines For Donors On S.V.Pranadana Trust Donation: Table of ContentDokument9 SeitenSri Venkateswara Pranadana Trust: Guidelines For Donors On S.V.Pranadana Trust Donation: Table of ContentBhavaraju Chandra Sekhar SharmaNoch keine Bewertungen
- Nicole Ryan ThesisDokument7 SeitenNicole Ryan ThesisEnglishPaperHelpSaintPaul100% (1)
- Practical Nursing Clinical 14/15 SyllabusDokument110 SeitenPractical Nursing Clinical 14/15 Syllabusjedisay1Noch keine Bewertungen
- Cardiac Imaging Sept 2016tDokument254 SeitenCardiac Imaging Sept 2016tColeen Joyce NeyraNoch keine Bewertungen
- Best IVF Doctors in Delhi With High Success RatesDokument11 SeitenBest IVF Doctors in Delhi With High Success RatesPrabha SharmaNoch keine Bewertungen
- Blindness in Indonesia: Farida SirlanDokument41 SeitenBlindness in Indonesia: Farida SirlannonawitaNoch keine Bewertungen
- Campus Map Building List PDFDokument1 SeiteCampus Map Building List PDFRicky Quizzagan MaguigadNoch keine Bewertungen
- 01-Sdh DH Iphs Guidelines-2022Dokument244 Seiten01-Sdh DH Iphs Guidelines-2022பிரேம் குமார் ராஜாமணிNoch keine Bewertungen
- Ancient Egyptian MedicineDokument8 SeitenAncient Egyptian Medicineapi-276953527Noch keine Bewertungen
- Emily J. Mathios: EducationDokument2 SeitenEmily J. Mathios: Educationapi-427066976Noch keine Bewertungen
- HemiplegiaDokument5 SeitenHemiplegiaRyan TOgzNoch keine Bewertungen