Beruflich Dokumente
Kultur Dokumente
Cancer Larync
Hochgeladen von
Saya MenangCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Cancer Larync
Hochgeladen von
Saya MenangCopyright:
Verfügbare Formate
Cancer Larynx
Contents
1. Definition
2. Epidemiology
3. Etiology
4. Anatomical sites of larynx
5. Tumor, node, metastasis (TNM) system and Histologic
grading
6. Laryngeal carcinoma based on anatomical sites
supraglottic, glottic and subglottic cancer
7. Laryngeal carcinoma based on histologic classification
8. Diagnosis
9. Principle of Treatment
Definition
Laryngeal carcinoma is cancer of the larynx,
including the vocal cords (glottis), supraglottis,
and subglottis.(Ferri's Clinical Advisor 2014)
Epidemiology
Laryngeal carcinoma is the most common
malignancy among head and neck
There are 12,000 new cases per year in the
U.S.
Male predominance, M:F (10:1)
4
th
to 7
th
decade, peak incidence at sixth
decade
Ferri's Clinical Advisor 2014
Aetiology
Smoking
Alcohol
Previous radiation
Genetic
Occupational exposure
Gastroesophageal reflux disease (GERD)
Human papillomavirus
Cummings Otolaryngology Head & Neck Surgery , Fifth Edition
Larynx is divided into 3 regions:
1. Supraglottis
2. Glottis
3. Subglottis
This division reflects the embryologic structure of
the larynx and the anatomic barriers to spread of
cancer.
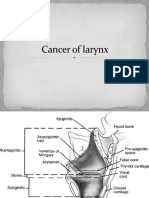
Anatomical Sites of Larynx
Classification of sites and various sub-
sites under each site in larynx
Site Sub-sites
Supraglottis Suprahyoid epiglottis
Infrahyoid epiglottis
Aryepiglottic folds
Arytenoids
Ventricular bands/ false cords
Glottis True vocal cord including anterior
and posterior commissure
Subglottis Subglottic up to the lower border
of cricoid cartilage
AJCC (American Joint Committee on Cancer) Classification 1997
Anatomic regions and structures of the
larynx.
horizontal plane 1 cm below the apex of the ventricle, or 0.5 cm below the free edge of the true vocal cords. Head and
neck surgeons typically refer to the former definition and radiation oncologists refer to the latter. The subglottis extends
down to the inferior margin of the cricoid cartilage and the beginning of the trachea.
FIGURE 31-1!
Anatomic regions and structures of the larynx.
The appearance of the larynx as seen in the indirect mirror examination is shown in Fig. 31-2 . The cartilaginous
framework of the larynx is important in diagnostic radiology and in evaluating simulation and port films. The relationship of
the various cartilages to surface anatomy is shown in Fig. 31-3 . The thyroid, cricoid, and the majority of the arytenoid
cartilages are composed of hyaline cartilage, which begins to ossify at approximately 20 years of age. The epiglottis, the
corniculate and cuneiform cartilages, and the apex and vocal process of the arytenoids are made up of elastic cartilage,
which does not ossify and therefore is not radiopaque.
FIGURE 31-2!
Structures of the larynx as seen by indirect mirror examination.
Leibel and Phillips Textbook of Radiation
Oncology , Third Edition
cancer outlined earlier. The TNM staging system further subdivides the supraglottis and glottis of the larynx
into multiple subsites, used to define the T stage ( Table 107-1 ).
6
Figure 107-1.
Classification of laryngeal lesions by the anatomic site involved.
(Adapted from Ogura JH, Biller HF. Partial and total laryngectomy and radical neck dissection. In:
Maloney WH, ed. Otolaryngology. Vol 4. New York: Harper & Row; 1971.)
Table 107-1
Anatomic Sites and Subsites of the Larynx
Site Subsite
Supraglottis
Suprahyoid epiglottis
Infrahyoid epiglottis
Aryepiglottic folds, right and left (laryngeal surfaces)
Arytenoids, right and left
Ventricular bands, right and left
Glottis
True vocal cords, right and left (including the anterior and posterior
commissures)
Subglottis No separate subsites defined
From Greene F, Page D, Fleming I, et al. AJCC Cancer Staging Manual. 6th ed. New York: Springer; 2002.
The supraglottis is composed of the suprahyoid and infrahyoid epiglottis (both the lingual and the laryngeal
surfaces), aryepiglottic folds (laryngeal surfaces only), arytenoids, and ventricular bands (false vocal cords).
The boundary between the suprahyoid and infrahyoid epiglottis is a horizontal plane passing through the hyoid
Cummings Otolaryngology Head & Neck
Surgery , Fifth Edition
FIGURE 31-3!
A, Anterior view of surface anatomy with cartilages shown. B, Lateral view of surface anatomy with cartilages
shown.
The anterior limits of the larynx consist of the lingual surface of the suprahyoid epiglottis, the thyrohyoid membrane, the
anterior commissure, and the anterior wall of the subglottic region, which is composed of the thyroid cartilage, the
cricothyroid membrane, and the anterior arch of the cricoid cartilage (see Fig. 31-3 B). To avoid underdosing the anterior
portion of the larynx when using megavoltage radiation to treat larynx cancer, it is important to remember that the anterior
commissure usually lies within 1 cm of the skin surface and that bolus may be required to deliver adequate dose to this
area. The posterior and lateral limits include the aryepiglottic folds, the arytenoids, the interarytenoid space, and the
posterior surface of the subglottic space formed by the mucous membrane covering the cricoid cartilage. Superiorly, the
epiglottis demarcates the boundary with the pharynx, which is usually at the lower border of the C3 vertebra. The inferior
extent of the larynx is at the lower margin of the cricoid, which is typically at the level of the C6 vertebra ( Fig. 31-4 ). The
anatomy of the larynx can also be appreciated on computed tomography (CT) scans. The key structures are seen in Fig.
31-5 .
FIGURE 31-4!
Structures of the larynx as seen from behind.
FIGURE 31-5!
Structures of the larynx as seen on computed tomography scans at the level of true vocal cords (A) and
subglottis (B).
Pathologic Conditions
Squamous cell carcinomas account for at least 95% of all malignant neoplasms of the larynx. Carcinomas arising from the
true vocal cords are usually well differentiated or moderately well differentiated, whereas carcinomas of the supraglottis
and subglottis are less differentiated. Carcinoma in situ (CIS) occurs in the vocal cords but is rare in the supraglottis. CIS
is a pathologic entity representing carcinomatous changes confined to the thickened epithelium without breaching the
lamina propria. As in other malignancies, invasion through the basement membrane distinguishes invasive carcinoma
from CIS. When carcinogens promote DNA damage, they lead to a multistep progression of hyperplasia, dysplasia, in situ
carcinoma, and invasive malignant lesions. Thus, it is common to see abnormal specimens that contains areas of
dysplasia, CIS, and invasive carcinoma.
Verrucous carcinoma is an uncommon but distinct variety of squamous cell carcinoma. It accounts for less than 5% of all
larynx cancers. It is a bulky, exophytic, papillomatous, low-grade squamous cell carcinoma. Typically it has a heavily
keratinized surface and a blunt, well-demarcated, invasive, deep margin, often with a broad base. Other rare tumors of the
larynx include malignant minor salivary gland tumors, small cell carcinoma (SCC), lymphoma, plasmacytoma,
chemodectoma, carcinoid, pseudosarcoma, soft-tissue sarcoma, chondrosarcoma, malignant melanoma, and metastatic
disease. The management of these tumors is dictated primarily by their histology rather than the location.
Structures of the larynx as seen from behind.
Leibel and Phillips Textbook of Radiation
Oncology , Third Edition
TNM system
T: tumor and its extent
N: indicates regional lymph node enlargement
and its size
M: distant metastasis
Histologic Grading
(WHO 1987- Modified Broders Classification)
Grade 1 : Well differentiated
- Excessive keratin pearl formation
Grade 2: Moderately differentiated
- Moderate keratin formation
Grade 3: Poorly differentiated
- Keratin formation is only detected by
cytokeratin immunohistochemical reaction or
electron miscroscopy
Supraglottic Cancer
Extent:
The common sites: Epiglottis, false cord followed
by aryepiglottic fold
Spread:
For supraglottic cancer: Locally spread or invade the
adjoining areas like vallecula, base of tongue and
pyriform form
Nodal metastasis:
Occur early. Upper and middle jugular nodes are
often involved. Bilateral metastasis can be seen in
epiglottic cancer
Symptoms:
Always silent
Throat pain, dysphagia, referred pain to ear,
painful neck swelling
Hoarseness of voice late symptom
Weight loss, airway obstruction, halitosis
late features
Supraglottic Cancer
Glottic Cancer
Extent:
The most common site for laryngeal carcinoma, especially
free edge and upper surface of vocal cord in its anterior
middle third
Spread: Locally may spread to
Anteriorly: Anterior commissure
Posteriorly: Vocal process and arytenoid region
Superiorly: Ventricle and false cord
Inferiorly: Subglottic region
Early stage: Vocal cord is mobile
Late stage: Fixation of cord spread to thyroarytenoid mucscle
bad prognosis
Nodal metastasis: Not common
Glottic Cancer
Symptoms:
Hoarseness of voice early sign
Stridor
Laryngeal obstruction
Subglottic Cancer
Extent: From the glottic area to lower border of cricoid
cartilage
Rare
Spread:
Spread around anterior wall to the opposite side
Spread downward to the trachea
Upward spread to vocal cord is late symptoms no early
hoarseness of voice
Invade cricothyroid membrane, thyroid gland
Nodal metastasis:
Prelaryngeal nodes
Pretracheal nodes
Paratracheal nodes
Lower jugular nodes
Subglottic Cancer
Symptoms:
Stridor and laryngeal obstruction
Hoarseness of voice
Histologic Classification
Epithelial cancers:
Squamous cell carcinoma
Basaloid squmous carcinoma
Verrucous carcinoma
Adenocarcinoma
Pseudosarcoma
Anaplastic cancer
Transitional cell carcinoma
Neuroendocrine tumors, including small cell and
carcinoid
Sarcoma: Metastatic malignancies
Squamous cell carcinoma
More than 95% of laryngeal tumours are
squamous cell carcinoma
Common site: Glottic region true vocal cord
Squamous Cell Carcinoma
Four subtypes:
1. Glottic carcinoma
2. Supraglottic carcinoma
3. Subglottic carcinoma
4. Transglottic carcinoma: cross the ventricle from the
supraglottic area to involve the true and false vocal folds
or involve the glottis and extend subglottically more than
10mm or both
Glottic carcinomas (50%-60%)
Supraglottic carcinomas (30%-40%)
Subglottic carcinomas are uncommon (5% or less).
Diagnosis
1. History
2. Indirect laryngoscopy
3. Neck examination
4. Radiology
5. CT Scan
6. Direct laryngoscopy
7. Microlaryngoscopy
Persistent or gradually increasing hoarseness
of voice for 3 weeks
1.History
2. Indirect laryngoscopy
Appearance of lesion
Vocal cord mobility
Extent of disease
3. Examination of the Neck
Extralaryngeal spread of disease
Nodal metastasis
4. Radiology
X-ray Chest
Soft tissue lateral view neck
5. CT scan
Extent of tumour
Invasion
Destruction of cartilage
Lymph node involvement
6. Direct laryngoscopy
Hidden area of larynx
Extent of the disease
7. Microlaryngoscopy
Small lesion of vocal lesion
For accurate biopsy specimens
Treatment
Depends upon the site of lesion, extent of lesion,
presence or absence of nodal and distant
metastases.
Radiotherapy
Surgery
Conservative
Total laryngectomy
Combined therapy
1. Radiotherapy
Early lesions which neither impair cord
mobility nor invade cartilage or cervical nodes
Not suitable for lesion with fixed cords,
subglottic extension, cartilage invasion, and
nodal metastasis
2. Surgery
a. Conservative surgery
i. Preserve the voice
ii. Avoid a permanent tracheal opening
iii. Includes:
Excision of vocal cord after splitting the larynx
(cordectomy via laryngofissure)
Excision of vocal cord and anterior commissure
(partial frontolateral laryngectomy)
Excision of the epiglottis
2. Surgery
b. Total laryngectomy
Indications:
i. T3 lesion with cord fixation
ii. All T4 lesion
iii. Invasion of thyroid and cricoid cartilage
iv. Bilateral arytenoid cartilage involvement
v. Posterior commissure lesion
vi. Failure after conservative surgery or radiotherapy
vii. Transglottic cancer
Contraindication: Patient with distant metastasis
3. Combined Therapy
Surgery may be combined with pre-operative
or post-operative radiotherapy
To reduce the recurrence
References (Draft)
Ferri's Clinical Advisor 2014, Fred F. Ferri, 643-643.e1
Diseases of ear, nose and throat, P.L Dhingra, 3
rd
edition
Cummings Otolaryngology Head & Neck Surgery , Fifth Edition, Paul W.
Flint, Bruce H. Haughey, Valerie J. Lund, John K. Niparko, Mark A.
Richardson, K. Thomas Robbins, and J. Regan Thomas CHAPTER 107, 1482-
1511
Leibel and Phillips Textbook of Radiation Oncology , Third Edition,
Richard T. Hoppe, Theodore Locke Phillips, and Mack Roach, Chapter 31,
642-665
Atlas of Head and Neck Pathology , Second Edition, Bruce M. Wenig
Chapter 13, 439-532
Das könnte Ihnen auch gefallen
- Nasopharyngeal Carcinoma: From Etiology to Clinical PracticeVon EverandNasopharyngeal Carcinoma: From Etiology to Clinical PracticeAnne W.M. LeeNoch keine Bewertungen
- Tumours of HypopharynxDokument32 SeitenTumours of HypopharynxDurrikamil khattakNoch keine Bewertungen
- Lecture 1 Carcinoma LarynxDokument5 SeitenLecture 1 Carcinoma Larynxpa3roorNoch keine Bewertungen
- Maxillary Sinus CarcinomaDokument4 SeitenMaxillary Sinus CarcinomaSuresh MettaNoch keine Bewertungen
- Ototoxicity LatestDokument37 SeitenOtotoxicity LatestSucdi CabdiNoch keine Bewertungen
- Foreign Bodies in The NoseDokument37 SeitenForeign Bodies in The NosenedvedcoxNoch keine Bewertungen
- Laryngeal Cancer: Dr. Tan'Im Arief, SPTHT-KLDokument58 SeitenLaryngeal Cancer: Dr. Tan'Im Arief, SPTHT-KLRani Dwi HapsariNoch keine Bewertungen
- Anatomy of Nose andDokument29 SeitenAnatomy of Nose andMuhammad Waqar UlfatNoch keine Bewertungen
- Foreign Bodies of The Ear and NoseDokument6 SeitenForeign Bodies of The Ear and NoseLeez KhanNoch keine Bewertungen
- Non Allergic RhinitisDokument42 SeitenNon Allergic RhinitisKadek Seruni KusumanegaraNoch keine Bewertungen
- Tonsillitis BK (LR)Dokument57 SeitenTonsillitis BK (LR)Tiffany NurzamanNoch keine Bewertungen
- New Vertin CME Slides FinalDokument98 SeitenNew Vertin CME Slides FinalGaurav KatariaNoch keine Bewertungen
- Tumors of External EarDokument10 SeitenTumors of External Earsavin1996100% (2)
- Cortical Mastoid SurgeryDokument22 SeitenCortical Mastoid Surgerymanu100% (1)
- Ears, Nose and Throat Diseases: Prepared By: Hannelli BelingonDokument103 SeitenEars, Nose and Throat Diseases: Prepared By: Hannelli BelingonPatricia Kamille I. PawidNoch keine Bewertungen
- Deviated Nasal Septum: Ahmednagar Homoeopathic Medical College & Hospital AhmednagarDokument13 SeitenDeviated Nasal Septum: Ahmednagar Homoeopathic Medical College & Hospital AhmednagarSuhas IngaleNoch keine Bewertungen
- Benign Malignant LarynxDokument28 SeitenBenign Malignant LarynxfaizNoch keine Bewertungen
- Acute Suppurative Otitis MediaDokument41 SeitenAcute Suppurative Otitis Mediarani suwadjiNoch keine Bewertungen
- Functional Endoscopic Sinus Surgery - Overview, Preparation, TechniqueDokument10 SeitenFunctional Endoscopic Sinus Surgery - Overview, Preparation, TechniqueHendra SusantoNoch keine Bewertungen
- Pharyngeal Tumours2Dokument46 SeitenPharyngeal Tumours2miramirajalalNoch keine Bewertungen
- Tracheostomy: Dr. Amar KumarDokument18 SeitenTracheostomy: Dr. Amar KumarSudhanshu ShekharNoch keine Bewertungen
- Perichondritis PinnaDokument2 SeitenPerichondritis PinnaAnish RajNoch keine Bewertungen
- Laryngeal CancerDokument41 SeitenLaryngeal CancerNidya PutriNoch keine Bewertungen
- Congenital AnomaliesDokument39 SeitenCongenital Anomaliesiqiqiqiqiq100% (1)
- MastoiditisDokument5 SeitenMastoiditisJessica Fredelina0% (1)
- E.N.T Guide For Medical Students: Neck Examination: Dr. Giovanni Henry ENT Resident 2016Dokument79 SeitenE.N.T Guide For Medical Students: Neck Examination: Dr. Giovanni Henry ENT Resident 2016John M. HemsworthNoch keine Bewertungen
- Laryngeal Cancer Powerpoint FinalllllDokument30 SeitenLaryngeal Cancer Powerpoint Finalllllapi-396575125Noch keine Bewertungen
- AdenoidsDokument6 SeitenAdenoidsIfeanyichukwu OgbonnayaNoch keine Bewertungen
- Presentation1 Cervical BiopsyDokument14 SeitenPresentation1 Cervical BiopsyChanta MaharjanNoch keine Bewertungen
- Esophageal CancerDokument25 SeitenEsophageal CancerK poojithaNoch keine Bewertungen
- Antral WashDokument19 SeitenAntral WashRavi Bhushan SinghNoch keine Bewertungen
- Surgical Treatment of Postintubation Tracheal StenosisDokument40 SeitenSurgical Treatment of Postintubation Tracheal StenosisJessieca LiusenNoch keine Bewertungen
- Thyroglossal CystsDokument4 SeitenThyroglossal CystsCondurache Ilie-AndreiNoch keine Bewertungen
- Temp Bone Trauma Slides 051012Dokument55 SeitenTemp Bone Trauma Slides 051012RaihanFarhanaNoch keine Bewertungen
- Myringotomy & MyringoplastyDokument35 SeitenMyringotomy & MyringoplastypriyaNoch keine Bewertungen
- Epidemiology of Oral Cancer PDFDokument6 SeitenEpidemiology of Oral Cancer PDFمحمد عبدالهادي إسماعيلNoch keine Bewertungen
- Chronic Otitis MediaDokument4 SeitenChronic Otitis MediaOvyanda Eka MItraNoch keine Bewertungen
- LabyrinthitisDokument8 SeitenLabyrinthitisVIDYANoch keine Bewertungen
- ENT Emergency PresentationDokument135 SeitenENT Emergency PresentationshahiruddinNoch keine Bewertungen
- Choriocarcinoma 11Dokument23 SeitenChoriocarcinoma 11Fakhir HasanNoch keine Bewertungen
- RTS1-K13-Anatomy of LungsDokument22 SeitenRTS1-K13-Anatomy of LungsYohanna SinuhajiNoch keine Bewertungen
- Basic Sinus AnatomyDokument71 SeitenBasic Sinus AnatomyTalal AlanzyNoch keine Bewertungen
- Congenital Lobar EmphysemaDokument25 SeitenCongenital Lobar Emphysemasheme1711Noch keine Bewertungen
- Diseases of Pharynx and Larynx 150406135136 Conversion Gate01Dokument68 SeitenDiseases of Pharynx and Larynx 150406135136 Conversion Gate01dr. EndahNoch keine Bewertungen
- Pediatric Liver TransplantationDokument30 SeitenPediatric Liver TransplantationMadhu Sinha100% (1)
- Recurrent Respiratory Papillomatosis: FaringDokument49 SeitenRecurrent Respiratory Papillomatosis: FaringIchsanJuliansyahNoch keine Bewertungen
- Chronic Suppurative Otitis Media A Model Case Sheet by DrtbaluDokument2 SeitenChronic Suppurative Otitis Media A Model Case Sheet by DrtbaluMaria Arifuddin0% (1)
- Cancer of LarynxDokument46 SeitenCancer of LarynxVIDYANoch keine Bewertungen
- Barium Swallow: DR Akash Bhosale Jr1Dokument66 SeitenBarium Swallow: DR Akash Bhosale Jr1Aakash BhosaleNoch keine Bewertungen
- Esophageal Atresia and Tracheoesophageal FistulaDokument21 SeitenEsophageal Atresia and Tracheoesophageal FistulaIslam AmerNoch keine Bewertungen
- Bone Marrrow TransplantationDokument28 SeitenBone Marrrow TransplantationvinoliNoch keine Bewertungen
- Carcinoma of NasopharynxDokument15 SeitenCarcinoma of NasopharynxAmeliana KamaludinNoch keine Bewertungen
- A Topic Presentation ON: Emerging Communicable DiseasesDokument52 SeitenA Topic Presentation ON: Emerging Communicable DiseasesGiri SivaNoch keine Bewertungen
- Ent Instruments With DetailsDokument15 SeitenEnt Instruments With Detailsmahi_20Noch keine Bewertungen
- Otitis Media With EffusionDokument3 SeitenOtitis Media With EffusionAnish RajNoch keine Bewertungen
- Ca LarynxDokument36 SeitenCa LarynxTito PNoch keine Bewertungen
- Pediatric InstrumentsDokument30 SeitenPediatric InstrumentsSanjit PandeyNoch keine Bewertungen
- Laryngeal CancerDokument19 SeitenLaryngeal Cancerduong thi myNoch keine Bewertungen
- Prevalence of Teenage Pregnancy Among Pregnant Mothers Presenting at Hoima Regional Referral Hospital During The Covid-19 Pandemic (2020 To 2021)Dokument8 SeitenPrevalence of Teenage Pregnancy Among Pregnant Mothers Presenting at Hoima Regional Referral Hospital During The Covid-19 Pandemic (2020 To 2021)KIU PUBLICATION AND EXTENSIONNoch keine Bewertungen
- Non Surgical Treatment Modalities of SCCHN: Presentation by Post Gradute StudentDokument113 SeitenNon Surgical Treatment Modalities of SCCHN: Presentation by Post Gradute StudentZubair VajaNoch keine Bewertungen
- Contraindications of Eswl B Pass Bleeding Diathesis Pregnancy Aneursym Sepsis Stone More Than 2MmDokument1 SeiteContraindications of Eswl B Pass Bleeding Diathesis Pregnancy Aneursym Sepsis Stone More Than 2MmSaya MenangNoch keine Bewertungen
- Basketball Students Attendance List 2017 Dates Class 9/1 16/1 23/1 6/2 13/2 20/2 27/2 6/3 13/3 27/3 3/4 10/4 17/4 24/4Dokument2 SeitenBasketball Students Attendance List 2017 Dates Class 9/1 16/1 23/1 6/2 13/2 20/2 27/2 6/3 13/3 27/3 3/4 10/4 17/4 24/4Saya MenangNoch keine Bewertungen
- Physics PEKA Scoring Check ListDokument2 SeitenPhysics PEKA Scoring Check ListSaya MenangNoch keine Bewertungen
- Physics PEKA Scoring Check ListDokument2 SeitenPhysics PEKA Scoring Check ListSaya MenangNoch keine Bewertungen
- Vitamin of Seizure Vascular Idiopathic Autoimmune Metabollic Infection NeoplasmDokument1 SeiteVitamin of Seizure Vascular Idiopathic Autoimmune Metabollic Infection NeoplasmSaya MenangNoch keine Bewertungen
- Presentation 1Dokument1 SeitePresentation 1Saya MenangNoch keine Bewertungen
- Esa Waterpark D Weekday, Mon - Tue / Thu - Fri (Adult) : Ticket To Desa WaterparkDokument1 SeiteEsa Waterpark D Weekday, Mon - Tue / Thu - Fri (Adult) : Ticket To Desa WaterparkSaya MenangNoch keine Bewertungen
- Rates of Reaction TestDokument10 SeitenRates of Reaction TestSaya MenangNoch keine Bewertungen
- Cerebellar ExaminationDokument1 SeiteCerebellar ExaminationSaya MenangNoch keine Bewertungen
- Physics p2 Trial SPM 2007 (Kedah)Dokument14 SeitenPhysics p2 Trial SPM 2007 (Kedah)Saya MenangNoch keine Bewertungen
- Bacterialcornealulcer 140129095140 Phpapp02Dokument48 SeitenBacterialcornealulcer 140129095140 Phpapp02Saya MenangNoch keine Bewertungen
- IAU Case Write UpDokument4 SeitenIAU Case Write UpSaya MenangNoch keine Bewertungen
- Sample Referral LetterDokument2 SeitenSample Referral LetterSaya Menang100% (1)
- Trial Terengganu Biologi SPM 2014 K2 SkemaDokument12 SeitenTrial Terengganu Biologi SPM 2014 K2 SkemaCikgu Faizal100% (1)
- 01 - 012 Obstructive Sleep ApneaDokument2 Seiten01 - 012 Obstructive Sleep ApneaSaya MenangNoch keine Bewertungen
- Case Report in Psychiatry051.03Dokument4 SeitenCase Report in Psychiatry051.03Saya MenangNoch keine Bewertungen
- Factors Affecting Rate of Reaction CatalystDokument1 SeiteFactors Affecting Rate of Reaction CatalystSaya MenangNoch keine Bewertungen
- Chemistry Chapter 5 Form 5Dokument1 SeiteChemistry Chapter 5 Form 5Saya MenangNoch keine Bewertungen
- Chemistry Chapter 5 Form 5Dokument1 SeiteChemistry Chapter 5 Form 5Saya MenangNoch keine Bewertungen
- Trial Terengganu SPM 2013 PHYSICS Ques - Scheme All PaperDokument0 SeitenTrial Terengganu SPM 2013 PHYSICS Ques - Scheme All PaperCikgu Faizal67% (3)
- Sleep Apnea - Could It Be Robbing You of Rest?Dokument4 SeitenSleep Apnea - Could It Be Robbing You of Rest?Saya MenangNoch keine Bewertungen
- Su20140331031237x52 609594142 1403057431Dokument14 SeitenSu20140331031237x52 609594142 1403057431Saya MenangNoch keine Bewertungen
- ENT Short Cases Records & OSCE Questions: 1 EditionDokument15 SeitenENT Short Cases Records & OSCE Questions: 1 EditionSaya MenangNoch keine Bewertungen
- ADD MATHS Progressions FORM 5Dokument6 SeitenADD MATHS Progressions FORM 5Cik NursharwaniNoch keine Bewertungen
- Trachy 121106090823 Phpapp02Dokument46 SeitenTrachy 121106090823 Phpapp02Saya MenangNoch keine Bewertungen
- Casewriteup Ent 110911092915 Phpapp01Dokument8 SeitenCasewriteup Ent 110911092915 Phpapp01Saya MenangNoch keine Bewertungen
- Comprehensive Key For ENT Cases: CSOM Never Painful Except inDokument21 SeitenComprehensive Key For ENT Cases: CSOM Never Painful Except inSaya Menang100% (1)
- Ent Instruments 100503041754 Phpapp02Dokument59 SeitenEnt Instruments 100503041754 Phpapp02Krittin NaravejsakulNoch keine Bewertungen
- Larynx (Anatomy, Laryngomalacia, Laryngeal Web)Dokument12 SeitenLarynx (Anatomy, Laryngomalacia, Laryngeal Web)Saya MenangNoch keine Bewertungen
- Unit 4: Modern Biotechnological Processes: Guidelines For Choosing Host-Vector SystemsDokument3 SeitenUnit 4: Modern Biotechnological Processes: Guidelines For Choosing Host-Vector SystemsSudarsan CrazyNoch keine Bewertungen
- Na'aman, Josiah & The Kingdom of JudahDokument32 SeitenNa'aman, Josiah & The Kingdom of JudahKeith HurtNoch keine Bewertungen
- 3 - QMT425-T3 Linear Programming (29-74)Dokument46 Seiten3 - QMT425-T3 Linear Programming (29-74)Ashraf RadzaliNoch keine Bewertungen
- Types of Communicative StrategyDokument46 SeitenTypes of Communicative StrategyMyra Bolinas100% (1)
- Krautkrämer Ultrasonic Transducers: For Flaw Detection and SizingDokument48 SeitenKrautkrämer Ultrasonic Transducers: For Flaw Detection and SizingBahadır Tekin100% (1)
- 19 March 2018 CcmaDokument4 Seiten19 March 2018 Ccmabronnaf80Noch keine Bewertungen
- XM 301 StudDokument594 SeitenXM 301 StudNarendar ReddyNoch keine Bewertungen
- HeartCry Magazine Summer 2022 WebsiteDokument29 SeitenHeartCry Magazine Summer 2022 WebsiteefraNoch keine Bewertungen
- Tugas Pak Hendro PoemDokument24 SeitenTugas Pak Hendro PoemLaila LalaNoch keine Bewertungen
- Utah GFL Interview Answers TableDokument5 SeitenUtah GFL Interview Answers TableKarsten WalkerNoch keine Bewertungen
- System Design PrimerDokument60 SeitenSystem Design PrimerPendyala SrinivasNoch keine Bewertungen
- Question Bank of Financial Management - 2markDokument16 SeitenQuestion Bank of Financial Management - 2marklakkuMSNoch keine Bewertungen
- School Work - The Marriage CrisisDokument2 SeitenSchool Work - The Marriage CrisisTreesy NgoNoch keine Bewertungen
- Chapter 9Dokument35 SeitenChapter 9Cameron LeishmanNoch keine Bewertungen
- Clinical Standards For Heart Disease 2010Dokument59 SeitenClinical Standards For Heart Disease 2010Novita Dwi MardiningtyasNoch keine Bewertungen
- TaTa TeA Ad AnaLysiSDokument3 SeitenTaTa TeA Ad AnaLysiSAmiya RautNoch keine Bewertungen
- Relative Plate Motion:: Question # Difference Between Relative Plate Motion and Absolute Plate Motion and ApparentDokument9 SeitenRelative Plate Motion:: Question # Difference Between Relative Plate Motion and Absolute Plate Motion and ApparentGet TipsNoch keine Bewertungen
- Chapter-1-Operations and Management: There Are Four Main Reasons Why We Study OM 1)Dokument3 SeitenChapter-1-Operations and Management: There Are Four Main Reasons Why We Study OM 1)Karthik SaiNoch keine Bewertungen
- Legal Insights Issue 4 2018Dokument24 SeitenLegal Insights Issue 4 2018Weicong TanNoch keine Bewertungen
- The Importance of MoneyDokument9 SeitenThe Importance of MoneyLinda FeiNoch keine Bewertungen
- Chapter 1 To 3. Methods of ResearchDokument18 SeitenChapter 1 To 3. Methods of ResearchMaryAnnLasquiteNoch keine Bewertungen
- TNR Evaluation RD 2Dokument7 SeitenTNR Evaluation RD 2api-302840901Noch keine Bewertungen
- Spouses Benatiro V CuyosDokument1 SeiteSpouses Benatiro V CuyosAleli BucuNoch keine Bewertungen
- 128 Bit Carry Select AdderDokument53 Seiten128 Bit Carry Select AddergrtabhilkwNoch keine Bewertungen
- A Journey To SomnathDokument8 SeitenA Journey To SomnathUrmi RavalNoch keine Bewertungen
- The Myth of HITLER's POPE - Hubert - LunsDokument13 SeitenThe Myth of HITLER's POPE - Hubert - LunsHubert LunsNoch keine Bewertungen
- Evaluation Sheet For RankingDokument6 SeitenEvaluation Sheet For RankingSonny MatiasNoch keine Bewertungen
- Mediated Read Aloud Lesson PlanDokument4 SeitenMediated Read Aloud Lesson PlanMandy KapellNoch keine Bewertungen
- 1.CH 211 IntraductionDokument13 Seiten1.CH 211 IntraductionCarlos BuchwaNoch keine Bewertungen
- The Campanile (Vol 90, Ed 2), Published Oct 22, 2007Dokument24 SeitenThe Campanile (Vol 90, Ed 2), Published Oct 22, 2007The CampanileNoch keine Bewertungen