Beruflich Dokumente
Kultur Dokumente
Morport 10 Juni 2014
Hochgeladen von
lettasamudraOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Morport 10 Juni 2014
Hochgeladen von
lettasamudraCopyright:
Verfügbare Formate
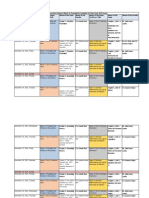
MORNING
REPORT
Department of Internal Medicine
Christian University of Indonesia
June, 10
th
2014
TEAM 2
Findings Assesment Therapy Planning
Vomiting , Fever , Loss of appetite, painful swallowing,
cough without phlegm
PHYSICAL EXAMINATION
Appearance : being sick, GCS E4V5M6
BP : 130/70mmHg
HR : 96x/min
RR : 20x/min, T : 37.3C
Eye hyperemic conjunctiva (-/-), Icteric sclera -/-
THT : normal
Mouth : normal
Neck : lymph nodes not enlarge, JVP : 5-2 cmH2O
Thorax
Ins : chest movement symmetric
Pal : vocal fremitus sound symmetric
Per : symmetric sonor sound
Aus : basic sound of breath vesicular, wheezing (-/-), ronchi
(-/-)
Heart sound I & II regular, murmur (-), gallop (-)
Abdominal
Ins : looks flat
Aus : bowel sound (+), 4x/min
Per : percution pain, timpani sound
Pal : tenderness epigastrium and defence muscular
Extremities
warm acral, CRT < 2 s, edema
LABORATORIUM
Hemoglobin : 15,9 g/dl
Haematocrit : 41,1 %
Leucocyte: 17,6 ribu/ul
Thrombocyte : 200.000 /ul
Dyspepsia
Gastritis akut
-Prohospitalized
-Diet : soft, not to stimulate
-IVFD : III RL / 24 hours
-Mm/
Ceftriaxone drip 2 x
200 mg
Paracetamol 3 x 50 mg
Omeperazole 2 x 20mg
Ondansetron 1 amp
Laboratorium (Blood
H2TL)/day
Mr. Fernando, 24 years old
-
- -
-
Tuesday , June 10
th
2014, 07.15 PM
Subjective Data
Name : Mr. Fernando
TC : Tuesdsay , June 10
th
2014
CC : Vomiting
Anamnesis
Main symptom : Vomiting
Additional symptom : Fever, loss of appetite, painful
swallowing, cough without phlegm
Patient came to UKI hospital with vomiting about 1
day ago before entering the hospital. Vomiting containing
liquid and food. Patient also get fever and he felt his
appetite diminished because he felt painful when
swallowing. Patient also complained cough without phlegm.
Bowel and bladder normal.
Past Medical History and Treatment
Gastritis (occur when he get stress)
Family History
Denied
Social History
Smoking (-), Alcohol (-)
Objective Data
Appearance : Being sick
GCS E4M6V5
BP : 130/70 mmHg
RR: 20x/minute
T : 37.3C
HR : 96x/minute
Eyes: Pale conjunctiva (-/-), sclera icteric (-/-)
Ears, nose and mouth: Normal
Lymph nodes: Not enlarged
JVP : Not distended
Thorax
Ins: Chest wall movement symmetric
Pal: Vocal fremitus sound symmetric
Per: Symmetric sonor sound
Aus: Basic sound of breath vesicular, wheezing (-/-), ronchi (-/-)
Heart sound I & II regular, murmur (-), gallop (-)
Abdomen
Ins: Looks flat
Aus: Bowel sound (+) 4x/minute
Per: Timpani, percussion tenderness in all abdomens regio (-)
Pal: Abdominal tenderness in epigastrium regio (+), liver and
spleen enlargement (-)
Extremities
Warm
Capillary refill time <2 seconds
Edema (-)
Clinical Laboratory
Hemoglobin : 15,9 g/dl
Haematocrit : 41,1 %
Leucocyte: 17,6 ribu/ul
Thrombocyte : 200.000 /ul
Assessment
Dyspepsia
Gastritis akut
Therapy
Prohospitalized
Diet : soft, not to stimulate
IVFD : III RL / 24 hours
Mm/
Ceftriaxone drip 2 x 200 mg
Paracetamol 3 x 50 mg
Omeperazole 2 x 20mg
Ondansetron 1 amp
Planning
Check laboratorium (Blood H2TL)/day
Thank
You
Department of Internal
Medicine
Christian University of
Indonesia
Das könnte Ihnen auch gefallen
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (399)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (73)
- Journey To The ARI-ARhAyas AL-Uma-UN Core of The Krystar Seed Atom FileDokument14 SeitenJourney To The ARI-ARhAyas AL-Uma-UN Core of The Krystar Seed Atom FileSungwon Kang100% (2)
- Lambika YogaDokument2 SeitenLambika Yogavsyamkumar100% (3)
- Case Study No. 11 - Hydroelectric Power Plant in The PhilippinesDokument26 SeitenCase Study No. 11 - Hydroelectric Power Plant in The PhilippinespicefeatiNoch keine Bewertungen
- Epidemiological Cutoff Values For Antifungal Susceptibility TestingDokument36 SeitenEpidemiological Cutoff Values For Antifungal Susceptibility Testingdadrrui100% (1)
- Openstack Deployment Ops Guide PDFDokument197 SeitenOpenstack Deployment Ops Guide PDFBinank PatelNoch keine Bewertungen
- Zombie Exodus Safe Haven GuideDokument148 SeitenZombie Exodus Safe Haven GuidejigglepopperNoch keine Bewertungen
- 7 Rinitis AtropikanDokument26 Seiten7 Rinitis AtropikanlettasamudraNoch keine Bewertungen
- 7 Rinitis AtropikanDokument26 Seiten7 Rinitis AtropikanlettasamudraNoch keine Bewertungen
- 7 Rinitis AtropikanDokument26 Seiten7 Rinitis AtropikanlettasamudraNoch keine Bewertungen
- 7 Rinitis AtropikanDokument26 Seiten7 Rinitis AtropikanlettasamudraNoch keine Bewertungen
- Shift of Heart and Trachea To Left: Tension PneumothoraxDokument44 SeitenShift of Heart and Trachea To Left: Tension PneumothoraxlettasamudraNoch keine Bewertungen
- SK5 GaluhDokument17 SeitenSK5 GaluhlettasamudraNoch keine Bewertungen
- Kuliah Ards DesDokument23 SeitenKuliah Ards DesOena SheQueen AL MusallyNoch keine Bewertungen
- Dr. Karuniawan - Bone Tumor, 2012 November (English)Dokument36 SeitenDr. Karuniawan - Bone Tumor, 2012 November (English)lettasamudraNoch keine Bewertungen
- Penatalaksanaan Osteosarkoma: Nirwana Sihol Marito Simanjuntak 1061050175Dokument10 SeitenPenatalaksanaan Osteosarkoma: Nirwana Sihol Marito Simanjuntak 1061050175lettasamudraNoch keine Bewertungen
- Penatalaksanaan Osteosarkoma: Nirwana Sihol Marito Simanjuntak 1061050175Dokument10 SeitenPenatalaksanaan Osteosarkoma: Nirwana Sihol Marito Simanjuntak 1061050175lettasamudraNoch keine Bewertungen
- Types of Primary and Secondary Bone CancersDokument14 SeitenTypes of Primary and Secondary Bone CancerslettasamudraNoch keine Bewertungen
- KJG DmamDokument12 SeitenKJG DmamBernard LeonardoNoch keine Bewertungen
- "Morning Report": Christian University of IndonesiaDokument12 Seiten"Morning Report": Christian University of IndonesialettasamudraNoch keine Bewertungen
- Penatalaksanaan Osteosarkoma: Nirwana Sihol Marito Simanjuntak 1061050175Dokument10 SeitenPenatalaksanaan Osteosarkoma: Nirwana Sihol Marito Simanjuntak 1061050175lettasamudraNoch keine Bewertungen
- PRINT-Morport, 14 Juni 2014Dokument2 SeitenPRINT-Morport, 14 Juni 2014lettasamudraNoch keine Bewertungen
- Morning Report 10 Juni 2014Dokument12 SeitenMorning Report 10 Juni 2014lettasamudraNoch keine Bewertungen
- 1 Imobilisasi N KomplikasiDokument24 Seiten1 Imobilisasi N KomplikasilettasamudraNoch keine Bewertungen
- Types of Primary and Secondary Bone CancersDokument14 SeitenTypes of Primary and Secondary Bone CancerslettasamudraNoch keine Bewertungen
- Gastropati Nsaid Blok 2 6Dokument32 SeitenGastropati Nsaid Blok 2 6Petrik Aqrasvawinata FsNoch keine Bewertungen
- Etoposide JurnalDokument6 SeitenEtoposide JurnalShalie VhiantyNoch keine Bewertungen
- Lesson Plan Garbage Gym GameDokument3 SeitenLesson Plan Garbage Gym Gameapi-272479731Noch keine Bewertungen
- Chapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsDokument10 SeitenChapter 1-The Indian Contract Act, 1872, Unit 1-Nature of ContractsALANKRIT TRIPATHINoch keine Bewertungen
- Radial Drill Catalog-110620Dokument14 SeitenRadial Drill Catalog-110620Anto SiminNoch keine Bewertungen
- Geomatics Lab 6 (GPS)Dokument24 SeitenGeomatics Lab 6 (GPS)nana100% (1)
- Newly Constructed Masculinity' in Mahesh Dattani's Dance Like A ManDokument4 SeitenNewly Constructed Masculinity' in Mahesh Dattani's Dance Like A ManIJELS Research JournalNoch keine Bewertungen
- Estimating PSCC for Electrical InstallationsDokument2 SeitenEstimating PSCC for Electrical InstallationsgmuitaNoch keine Bewertungen
- Tiger Tales: From Colonial MalayaDokument16 SeitenTiger Tales: From Colonial MalayamatarsNoch keine Bewertungen
- A. Rationale: Paulin Tomasuow, Cross Cultural Understanding, (Jakarta: Karunika, 1986), First Edition, p.1Dokument12 SeitenA. Rationale: Paulin Tomasuow, Cross Cultural Understanding, (Jakarta: Karunika, 1986), First Edition, p.1Nur HaeniNoch keine Bewertungen
- Advisory Circular: Aircraft Maintenance Engineer Licence - Examination Subject 2 Aircraft Engineering KnowledgeDokument44 SeitenAdvisory Circular: Aircraft Maintenance Engineer Licence - Examination Subject 2 Aircraft Engineering KnowledgejashkahhNoch keine Bewertungen
- Lecturer No 1 - Transformer BasicDokument1 SeiteLecturer No 1 - Transformer Basiclvb123Noch keine Bewertungen
- Liquid Air Energy Storage Systems A - 2021 - Renewable and Sustainable EnergyDokument12 SeitenLiquid Air Energy Storage Systems A - 2021 - Renewable and Sustainable EnergyJosePPMolinaNoch keine Bewertungen
- School newspaper report teaches Present PerfectDokument2 SeitenSchool newspaper report teaches Present PerfectMiro MiroNoch keine Bewertungen
- 74VHCU04Dokument6 Seiten74VHCU04Alexandre S. CorrêaNoch keine Bewertungen
- Rigor Mortis and Lividity in Estimating Time of DeathDokument2 SeitenRigor Mortis and Lividity in Estimating Time of DeathfunnyrokstarNoch keine Bewertungen
- JNTUA Mechanical Engineering (R09) Syllabus BookDokument147 SeitenJNTUA Mechanical Engineering (R09) Syllabus Bookslv_prasaad0% (1)
- Important instructions on judicial procedure from Narada SmritiDokument6 SeitenImportant instructions on judicial procedure from Narada SmritirohitNoch keine Bewertungen
- DX DiagDokument42 SeitenDX DiagVinvin PatrimonioNoch keine Bewertungen
- MIL (Second Quarter)Dokument13 SeitenMIL (Second Quarter)Menma ChanNoch keine Bewertungen
- Hireena Essay AnsDokument2 SeitenHireena Essay AnsTasniiem ChandraaNoch keine Bewertungen
- CVR College of Engineering: UGC Autonomous InstitutionDokument2 SeitenCVR College of Engineering: UGC Autonomous Institutionshankar1577Noch keine Bewertungen
- System Bus in Computer Architecture: Goran Wnis Hama AliDokument34 SeitenSystem Bus in Computer Architecture: Goran Wnis Hama AliGoran WnisNoch keine Bewertungen
- Comandos HuaweiDokument3 SeitenComandos Huaweicgottoli0% (1)
- Silyzer 300 - Next Generation PEM ElectrolysisDokument2 SeitenSilyzer 300 - Next Generation PEM ElectrolysisSaul Villalba100% (1)