Beruflich Dokumente
Kultur Dokumente
Gut Ry
Hochgeladen von
matrixtrinity0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
14 Ansichten98 SeitenUrine Controls fluid and electrolyte balance. 2. Controls acid-base balance 3. Excrete end products of body metabolism 4. Secrete renin and eryhtropoietin 5. Manufacture and activation of vitamin D URINE STUDIES 1. URINALYSIS - examination to assess the nature of the urine produced COLOR: pale to amber VOLUME: 30 ml / hour ODOR: aromatic then strong ammoniacal odor SPEC
Originalbeschreibung:
Originaltitel
GUT RY
Copyright
© © All Rights Reserved
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenUrine Controls fluid and electrolyte balance. 2. Controls acid-base balance 3. Excrete end products of body metabolism 4. Secrete renin and eryhtropoietin 5. Manufacture and activation of vitamin D URINE STUDIES 1. URINALYSIS - examination to assess the nature of the urine produced COLOR: pale to amber VOLUME: 30 ml / hour ODOR: aromatic then strong ammoniacal odor SPEC
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
14 Ansichten98 SeitenGut Ry
Hochgeladen von
matrixtrinityUrine Controls fluid and electrolyte balance. 2. Controls acid-base balance 3. Excrete end products of body metabolism 4. Secrete renin and eryhtropoietin 5. Manufacture and activation of vitamin D URINE STUDIES 1. URINALYSIS - examination to assess the nature of the urine produced COLOR: pale to amber VOLUME: 30 ml / hour ODOR: aromatic then strong ammoniacal odor SPEC
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 98
1. Controls fluid and electrolyte balance.
2. Controls of acid-base balance
3. Excrete end products of body metabolism
4. Secrete renin & eryhtropoietin
5. Manufacture & activation of vitamin D
URINE STUDIES
1. URINALYSIS
- examination to assess the nature of the urine produced.
a. Evaluates color, pH, and specific gravity
COLOR: pale to amber
VOLUME: 30 ml/hour
APPEARANCE: Clear
ODOR: aromatic then strong ammoniacal odor
SPECIFIC GRAVITY: 1.015-1.025 (24 hr urine collection)
1.003-1.030 (random specimen)
pH: 4.8-8.0
b. Determines the presence of glucose, protein, ketones and blood.
c. Analyzes sediment for cells
- presence of WBC, casts bacteria, crystals
URINE STUDIES
2. URINE CULTURE and SENSITIVITY
- diagnoses bacterial infections of the urinary tract.
3. RESIDUAL URINE
- amount of urine left in the bladder after voiding measured via
catheter (permanent or temporary) in bladder.
4. CREATININE CLEARANCE
- determines amount of creatinine (waste product of protein
breakdown) in the urine over 24 hours
- measures overall renal function; measures GFR
URINE COLLECTION METHODS
1. ROUTINE URINALYSIS
Wash perineal area if soiled.
Obtain first voided morning specimen.
Send to lab immediately.
- should be examined within 1 hour of voiding
URINE COLLECTION METHODS
2. CLEAN CATCH (MIDSTREAM) SPECIMEN for
URINE CULTURE
Cleanse perineal area.
FEMALE
Spread labia and cleanse meatus front to back using antiseptic
sponges.
MALE
Retract foreskin (if uncircumcised) and cleanse glans with antiseptic
sponges.
Have client initiate urine stream then stop.
Collect specimen in a sterile container.
Have client complete urination, but not in specimen container.
URINE COLLECTION METHODS
3. 24-hour URINE SPECIMEN
- preferred method for creatinine clearance test.
Have client void and discard specimen; note time.
Collect all subsequent urine specimens for 24 hours.
If specimen is accidentally discarded, the test must be
restarted.
Record exact start and finish of collection; include date and
time.
BLOOD STUDIES
BICARBONATE
- 22-26 mEq/L
BUN
- measures renal ability to excrete urea nitrogen
- Normal: 5-20 mg/dl
CALCIUM
- 9.0-10.5 mg/dl
SERUM CREATININE
- Specific tests for renal disorders
- Reflects ability of kidneys to excrete creatinine
- 0.7-1.5 mg/dl
PHOSPORUS
- 2.5-4.5 mg/dl
Sodium
- 136-145 mEq/L
INTRAVENOUS PYELOGRAM (IVP)
Fluoroscopic visualization of the urinary tract after injection with a
radiopaque dye.
NURSING CARE (PRE-TEST)
Assess for iodine sensitivity.
Obtain consent
Inform client he will lie on a table throughout procedure.
Administer cathartic or enema the night before.
Keep the client NPO for 8 hours pretest.
Inform client about possible throat irritations, flushing of face, warmth
or a salty taste that may be experienced during the test
NURSING CARE (POST-TEST)
Force fluids.
Assess venipincture site for bleeding
Monitor V/S for U/O
CYSTOSCOPY
Use of a lighted scope (cystoscope) to inspect the bladder.
- Inserted into the bladder via the urethra.
- May be used to remove tumors, stones, or other foreign material or
to implant radium, place catheters in ureters.
NURSING CARE (PRE-TEST)
Explain to client that the procedure will be done under general/local
anesthesia.
Obtain CONSENT
Confirm consent form is signed.
Administer sedatives 1 hour before test, as ordered.
General anesthesia: Keep client on NPO.
Local anesthesia: offer liquid breakfast.
CYSTOCOPY
NURSING CARE (POST-TEST)
Monitor V/S & I/O
-PINK TINGED/TEA COLORED URINE is expected
-BRIGHT RED URINE/PRESENCE OF LARGE CLOTS shld be
reported
Advise client that burning on urination is normal and will
subside.
Encourage DBE to relieve bladder spasms
Administer sitz baths for back & abdominal pain
Administer analgesics as Rx
Force fluids as prescribed
RENAL ANGIOGRAPHY
the injection of a radiopaque dye through a catheter for
examination of the renal artery supply
NURSING CARE ( PRE-TEST)
Obtain consent
Assess client for allergies to iodine, seafoods & radiopaque dyes
Inforn pt about possible burning sensation along the vessel
NPO postmidnight before the test
Instruct client to void immediately before the procedure
Shave injection sites as prescribed
Assess & mark the peripheral pulses
RENAL ANGIOGRAPHY
NURSING CARE ( POST TEST)
Assess V/S & peripheral pulses
Provide bedrest & use of sandbag @ the insertion site
for 4-8 hrs
NPO postmidnight before the test
Assess color & temp of the involved extremity
Force fluids unless C/I
Monitor urinary output
CLINICAL FINDINGS
Abdominal or flank pain/tenderness
Frequency and urgency of urination
Pain on voiding
Nocturia
Fever
DIAGNOSTIC TESTS
Urine culture and sensitivity
- presence of E. coli (80%)
NURSING CARE
Force fluids (3L/day)
Warm sitz bath for comfort.
Assess urine for odor, hematuria, & sediment.
Use strict aseptic technique in FBC
Administer medications as ordered.
Client teaching
GENERAL INFORMATION
Presence of stones anywhere in the urinary tract.
Frequent compositions of stones:
- calcium (phosphate), uric acid and cystine (rare) stones
Most often occurs in men age 20-55 years; more common in the
summer
PREDISPOSING FACTORS
Diet: large amount of calcium, oxalate
Increased uric acid levels
Sedentary lifestyles, immobility
Family history of gout or calculi
Hyperparathyroidism
CLINICAL FINDINGS
Abdominal pain or flank pain
Renal colic
- severe pain in the kidney area radiating down the flank to the
pubic area
Hematuria, frequency, urgency, nausea
History of prior associated health problems
- gout, parathyroidism, immobility, dehydration, UTI
Diaphoresis
Pallor
Grimacing
Vomiting
Pyuria if infection is present
MEDICAL MANAGEMENT
1. SURGERY
A. PERCUTANEOUS NEPHROSTOMY
- Tube is inserted through skin and underlying tissues into
renal pelvis to remove calculi.
B. PERCUTANEOUS NEPHROLITHOTOMY
- Delivers U/S waves thorough a probe placed on the calculus
2. PERCUTANEOUS ULTRASONIC LITHOTRIPSY (PUL)
- Nephroscope is inserted through skin into kidney.
- Ultrasonic waves disintegrate stones that are then removed
by suction and irrigation.
MEDICAL MANAGEMENT
3. EXTRACORPOREAL SHOCK-WAVE LITHOTRIPSY
(ESWL)
- Client is placed in water and exposed to shock waves
that disintegrate stones so that they can be
passed with urine.
- This procedure is non-invasive.
NURSING CARE
Strain all urine through gauze to detect stones and crush all
clots.
Force fluids (3000 4000 ml/day).
Encourage ambulation to prevent stasis.
Relieve pain by administration of analgesics as ordered and
application of moist heat to flank area.
Monitor I & O.
Provide modified diet, depending upon stone consistency.
DIET MODIFIED/STONE
CALCIUM STONES
Low calcium diet ( 400 mg daily)
Achieved by eliminating milk/dairy products
Provide acid-ash diet to acidify urine
- Cranberry or prune juice
- Meat
- Eggs
- Poultry
- Fish
- Grapes
- Whole grains
- Take vitamin A & C, Folic acid supplements and Riboflavin
DIET MODIFIED/STONE
OXALATE STONES
Avoid excess intake of foods/fluids high in oxalate
- Tea
- Chocolate
- Rhubarb
- Spinach
Maintain alkaline-ash diet to alkalinize urine
- Milk
- Vegetables
- Fruits except prunes, cranberries and plums
DIET MODIFIED/STONE
URIC ACID STONES
Uric acid is a metabolic product of purines
Reduce foods high in purine
- Liver, brains, kidneys, venison, shellfish, meat soups, gravies,
legumes and whole grains
Maintain alkaline urine
- Alkaline-ash diet
DIET MODIFIED/STONE
CYSTINE STONES (rare)
Low methionine
- Methionine is the essential amino acid from which the non-
essential amino acid cystine is formed
Limit protein foods
- Meat, milk, eggs, cheese
Maintain alkaline-ash diet
NURSING CARE
Administer Allopurinol (Zyloprim) as ordered.
- to decrease uric acid production
- force fluids when giving Allopurinol
Encourage daily weight-bearing exercise
Provide client teaching and discharge planning concerning:
- Prevention of urinary stasis by EOF esp. in hot weather and
during illness, mobility, voiding whenever the urge is felt and
at least twice during the night.
- Adherence to prescribed diet.
- Need for routine U/A (at least every 3-4 months)
- Need to recognize and report S/Sx of recurrence
- hematuria, flank pain
NURSING CARE
Provide care ff a nephrolithotomy or PUL
- Change dressings frequently during the first
24 hours after a nephrolithotomy.
- Maintain patency of ureteral catheter as well
as urethral catheter to prevent
hydronephrosis.
- Encourage use of incentive spirometry and
coughing and deep breathing to prevent
atelectasis.
Inflammation of the renal pelvis & parenchyma, commonly caused
by bacterial invasion
Acute Infection
- usually ascends from the lower urinary tract or following an
invasive procedure of the urinary tract
- can progress to bacteremia or chronic pyelonephritis
ASSESSMENT
Fever & Chills
N/V
CVA tenderness, flank pain on the affected side
Headache, muscular pain, dysuria
Frequency & urgency
Chronic Infection
- Major cause is ureterovesical reflux
- Result of recurrent infections is eventual parenchymal
deterioration and possible renal failure
ASSESSMENT
Client usually unaware of the disease
May have bladder irritability
Chronic fatigue
Slight dull ache over the kidneys
Eventually develops hypertension, atrophy of the kidneys
Azotemia
NURSING CARE
Monitor I & O
EOF
Encourage adequate rest
Administer antibiotics, analgesics as ordered.
Support client and significant others and explain
the possibility of dialysis, transplant options if
significant renal deterioration.
Provide client teaching and discharge planning:
- Medication regimen
- Diey: high calorie, low protein
PRERENAL CAUSES INTRARENAL
CAUSES
POSTRENAL CAUSES
Calculi
BPH
Tumors
Strictures
Blood clots
Trauma
Anatomic malformation
Hypotension
Acute tubular necrosis (ATN)
Diabetes mellitus
Cardiogenic shock
Acute vasoconstriction Malignant hypertension
Hemorrhage Acute glomerulonephritis
Tumors Burns
Septicemia
Blood transfusion reactions
CHF
Nephrotoxins
CLINICAL FINDINGS
OLIGURIC PHASE
Hypernatremia
Hyperkalemia
Hyperphosphatemia
Hypocalcemia
Hypermagnesemia
Metabolic acidosis
DIURETIC PHASE
Hyponatremia
Hypokalemia
Hypovolemia
CONVALESCENT PHASE
Normal Urine Volume
Increase in LOC
BUN stable and normal
May develop CRF
NURSING CARE
Monitor fluid and electrolyte balance.
Monitor alteration in fluid volume.
Promote optimal nutritional status
Prevent complications from impaired mobility
Prevent fever and infection
Support client/S.O. & reduce/relieve anxiety
CLINICAL FINDINGS
STAGE 1
Diminished Renal
Reserve
STAGE 2
Renal Insufficiency
STAGE 3
End Stage
CLINICAL FINDINGS
Nausea and vomiting Uremic frost
Decreased urinary output Dyspnea
Hypotension (early) Azotemia
Hypertension (later) Lethargy
Convulsions Memory impairment
Pericardial friction rub CHF
NURSING CARE:
Prevent neurologic complications.
Promote optimal GI function.
Monitor/prevent alteration in F/E.
Promote maintenance of skin integrity.
Monitor for bleeding complications, and prevent
injury.
NURSING CARE
Assess for hyperphosphatemia
- Paresthesias
- Muscle cramps
- Seizures
- Abnormal reflexes
Administer Aluminum hydroxide gels as ordered
- Amphogel, AlternaGEL
Promote/maintain maximal cardiovascular function.
Provide care for client receiving dialysis.
DIFFUSION
OSMOSIS
ULTRAFILTRATION
TYPES
Hemodialysis Peritoneal dialysis
1) CAPD
2) APD
a) CCPD
b) IPD
c) NPD
GENERAL INFORMATION
Shunting of blood from the clients vascular system through an artificial
dialyzing system and return of dialyzed blood to the clients circulation.
Dialysis coil acts as the semi-permeable membrane.
Dialysate is a specially prepared solution.
Shunting of blood from the clients vascular system through an artificial
dialyzing system and return of dialyzed blood to the clients circulation.
Dialysis coil acts as the semi-permeable membrane.
Dialysate is a specially prepared solution.
NURSING CARE:
(BEFORE and DURING HEMODIALYSIS)
Have client void.
Chart clients weight.
Assess vital signs before and every 30 mins. during procedure.
Withhold antihypertensives, sedatives, and vasodilators.
- to prevent hypotensive episode (unless ordered otherwise).
Ensure bed rest with frequent position changes for comfort.
Inform client that headache and nausea may occur.
Monitor closely for signs of bleeding since blood has been
heparinized for procedure.
NURSING CARE:(POST- DIALYSIS)
Chart clients weight.
Assess for complications.
A. HYPOVOLEMIC SHOCK
- may occur as a result of rapid removal or ultrafiltration
of fluid from the intravascular compartment.
B. DIALYSIS DISEQUILIBRIUM SYNDROME
- Urea is removed more rapidly from the blood than from
the brain.
- Assess for nausea, vomiting, elevated BP, disorientation, leg
cramps, and peripheral paresthesias.
GENERAL INFORMATION
Introduction of a specially prepared dialysate solution
into the abdominal cavity, where the peritoneum acts as
a semi-permeable membrane between the dialysate and
blood into the abdominal vessels.
NURSING CARE
Chart clients weight.
Assess V/S before, q15 min during first exchange, &qH
thereafter.
Assemble specially prepared dialysate solution with added
medications.
Have client void.
Warm dialysate solution to body temperature.
Assist physician with trocar insertion.
Inflow: Allow dialysate to flow unrestricted into peritoneal
cavity.
- 10-20 minutes
Dwell: Allow fluid to remain in peritoneal cavity for prescibe
period
- 30-45 minutes
Drain: Unclamp outflow tube and allow to flow by gravity.
NURSING CARE
Observe characteristics of dialysate outflow.
a. CLEAR PALE YELLOW
- normal
b. CLOUDY
- infection, peritonitis
c. BROWNISH
- bowel perforation
d. BLOODY
- common during first few exchanges
- ABNORMAL: if continuous
MIO and maintain records.
Assess for complications.
NURSING CARE
A. PERITONITIS
B. RESPIRATORY DIFFICULTY
C. PROTEIN LOSS
- Most serum proteins pass through the peritoneal membrane
and are lost in the dialysate fluid.
- Monitor serum protein levels closely.
GENERAL INFORMATION
A continuous type of peritoneal dialysis at home by the
client or significant others.
Dialysate is delivered from flexible plastic containers
through a permanent peritoneal catheter.
Following infusion of the dialysate into the peritoneal
cavity, the bag is folded and tucked away during the
dwell period.
NURSING CARE
Provide client teaching and discharge planning
concerning:
- Need to assess the permanent peritoneal catheter
for complications:
a. Dialysate leak
b. Exit site infection
c. Bacterial/Fungal contamination
d. Obstruction
Adherence to high-protein (if indicated), well-balanced
diet.
Importance of periodic blood chemistries.
Daily weights.
GENERAL INFORMATION
Transplantation of a kidney from a donor to recipient to
prolong the life of person with renal failure.
SOURCES OF DONOR SELECTION
Living relative with compatible serum and tissue studies,
free from systemic infection and emotionally stable.
Cadavers with good serum and tissue crossmatching, free
from renal disease, neoplasms and sepsis, absence of
ischemia/trauma.
NURSING CARE: PRE-OP
Provide routine pre-op care.
Discuss the possibility of post-op dialysis/immunosuppressive
drug therapy with client and significant others.
NRSG CARE: POST-OP
Provide routine post-op care.
Monitor fluid and electrolyte balance carefully.
- Monitor I & O hourly and adjust IV fluid administration
accordingly.
- Anticipate possible massive diuresis.
Encourage frequent and early ambulation.
Monitor V/S esp. temperature and report significant changes.
Provide mouth care and Nystatin (Mycostatin) mouthwashes for
Candidiasis.
Administer immunosuppressive agents as ordered.
NURSING CARE: POST-OP
Assess for signs of rejection.
Note for:
- Decreased urine output
- Fever/pain over transplant site
- Edema
- Sudden weight gain
- Increasing BP
- Generalized malaise
- Rise in serum creatinine
- Decrease in creatinine clearance
NURSING CARE: POST-OP
Provide client teaching and discharge planning concerning:
- Medication regimen
- S/Sx of tissue rejection and the need to
report it immediately to the physician
- Dietary restrictions
- Restricted Na and calories
- Increased CHON
- Daily weights
- Daily measurements of I & O
- Resumption of activity and avoidance of contact sports in
which the transplanted kidney may be injured
Renal tumor
Massive trauma
Removal for a donor
Polycystic kidneys
NURSING CARE: PRE-OP
Provide routine pre-op care.
Ensure adequate fluid intake.
Assess electrolyte values and correct any imbalances
before surgery.
Avoid nephrotoxic agents in any diagnostic tests.
Advise client to expect flank pain after surgery if
retroperitoneal approach (flank incision) is used.
Explain that the client will have chest tube if thoracic
approach is used.
NURSING CARE:POST-OP
Provide routine post-op care.
Assess urine output every hour.
Observe urinary drainage on dressing and estimate
amount.
Weigh daily.
Maintain adequate functioning of chest drainage, ensure
adequate oxygenation and prevent pulmonary
complications.
Administer analgesics as ordered.
Encourage early ambulation.
NURSING CARE: POST-OP
Teach client to splint incision while turning, coughing, and
deep breathing.
Teach client teaching and discharge planning concerning:
- Prevention of urinary stasis
- Maintenance of acidic urine
- Avoidance of activities that might cause trauma to
remaining kidney
- contact sports, horse back riding
- No lifting of heavy objects for at least 6 months
- Need to report unexplained weight gain, decreased
urine output, flank pain on unoperative side, hematuria
NURSING CARE: POST-OP
Teach client teaching and discharge planning concerning:
- Need to notify physician if cold or other infection
present for more than 3 days
- Medication regimen and avoidance of OTC drugs that
may be nephrotoxic (except with physician approval)
GENERAL INFORMATION
Most common problem of the male reproductive system
- occurs in 50% of men over age 50
- 75% of men over age 75
ETIOLOGY
Unknown
- may be related to hormonal mechanism
CLINICAL FINDINGS
Nocturia
Frequency
Decreased force and amount of urinary stream
Hesitancy
- difficulty in starting voiding
Hematuria
Enlargement of prostate gland upon palpation by digital rectal
exam
DIAGNOSTIC TESTS
Urinalysis
- alkalinity increased
- specific gravity normal or increased
BUN and creatinine elevated
- if long standing BPH
Prostate-specific antigen (PSA) elevated
- Normal: <4 ng/ml
Cystoscopy
- reveals enlargement of gland and obstruction of urine flow
NURSING CARE
Administer antibiotics as ordered.
Provide client teaching concerning medications
- Terazocin (Hytrin)
- relaxes bladder spincter and makes it easier to urinate
- may cause hypotension and dizziness
- Finasteride (Proscar)
- shrinks enlarged prostate
Force fluids.
Provide care for the catheterized client.
Provide care for the client with prostatic surgery.
GENERAL INFORMATION
Indicated for benign prostatic hypertrophy and prostatic
cancer
TYPES
1.TRANSURETHRAL RESECTION
2.SUPRAPUBIC PROSTATECTOMY
3.RETROPUBIC PROSTATECTOMY
4. RADICAL PERINEAL PROSTATECTOMY
NURSING CARE: PRE-OP
Provide routine pre-op care.
Information about the procedure & the expected post-op care,
including catheter drainage, irrigation, and monitoring of
hematuria is discussed.
Reinforce what surgeon has told client/significant others
regarding effects of surgery on sexual function.
Bowel prep
Force fluids, administer antibiotics, acid-ash diet to eradicate
UTI.
NURSING CARE: POST-OP
Provide routine post-op care.
Maintain patency of urethral catheter placed after surgery
Prevent Infection
Relieve pain
Reduce anxiety
Health education and health maintenance
PREDISPOSING FACTORS
Poor hygiene
Irritation from bubble baths
Urinary reflux
CLINICAL FINDINGS
Low-grade fever
Abdominal pain
Enuresis
Pain/burning on urination
Frequency
Hematuria
NURSING CARE
Administer antibiotics as ordered.
- prevention of kidney infection/glomerulonephritis.
- obtain cultures before starting antibiotics
Provide warm sitz baths to alleviate painful voiding.
Force fluids.
Encourage measures to acidify urine.
Provide client teaching and discharge planning
GENERAL INFORMATION
Autoimmune process leading to structural alteration of
glomerular membrane that results in increased permeability
to plasma proteins, particularly albumin.
Course of the disease consists of exacerbations and
remissions over a period of months to years.
Commonly affects preschoolers.
- boys more often than girls
Prognosis is good unless edema does not respond to
steroids.
Plasma CHON enter the renal tubule
Excreted in urine
PROTEINURIA
Oncotic pressure
Plasma volume
HYPOVOLEMIA
Release of RENIN & ANGIOTENSIN
Secretion of aldosterone
Reabsorption of H2O & Na in distal
tubule
BP
Release of ADH
Reabsorption
of H2O
General shift
of plasma into
interstitial
spaces
MASSIVE EDEMA
CLINICAL FINDINGS
Proteinuria, hypoproteinemia, hyperlipidemia
Dependent body edema
- puffiness around eyes in morning
- ascites
- scrotal edema
- ankle edema
Anorexia, vomiting, diarrhea, malnutrition
Pallor, lethargy
Hepatomegaly
MEDICAL MANAGEMENT
Drug therapy
- Corticosteroids
- to resolve edema
- Antibiotics
- for bacterial infections
- Thiazide diuretics
- edematous stage
Bedrest
Diet modification
- High CHON
- Low Na
NURSING CARE
Provide bed rest.
- Conserve energy.
- Find activities for quiet play.
Provide high CHON, low sodium diet during edema phase
only.
Maintain skin integrity.
- Dont use Band-Aids.
- Avoid IM injections
- medication is not absorbed in edematous tissue.
Obtain morning urine for CHON studies.
Provide scrotal support.
MIO, V/S and WOD
Administer steroids to suppress autoimmune response as
ordered.
Protect from known sources of infection.
GENERAL INFORMATION
Immune complex disease resulting from an antigen-
antibody reaction.
Secondary to a beta-hemolytic streptococcal infection
occurring elsewhere in the body.
Occurs more frequently in boys, usually between ages 6-7
years
Usually resolves in about 14 days
Self-limiting
CLINICAL FINDINGS
History of a precipitating streptoccal infection,
usually URTI or impetigo
Edema, anorexia, lethargy
Hematuria or dark-colored urine
Fever
Hypertension
DIAGNOSTIC FINDINGS
U/A
- reveals RBCs, WBCs, CHON, cellular casts
Urine specific gravity increased
BUN and serum creatinine increased
ESR elevated
Hgb and Hct decreased
NURSING CARE
MIO, BP, urine and WOD.
provide diversional therapy.
Provide client teaching and planning concerning:
- Medication administration
- Prevention of infection
- Signs of renal complications
- Importance of long-term follow-up
CLINICAL FINDINGS
Repeated UTIs
Failure to thrive
Abdominal pain, fever
Fluctuating mass in region of kidney
MEDICAL MANAGEMENT
Surgery to correct or remove obstruction
NURSING CARE
monitor V/S frequently
monitor for F/E imbalances including
dehydration after the obstruction is relieved.
monitor diuresis w/c could lead to fluid
depletion
WOD
monitor urine fro specific gravity, albumin &
glucose
administer fluid replacement as prescribed.
NURSING CARE
Post-op care
Monitor drains.
- may have one from bladder and one from each
ureter (ureteral stents)
Check output from all drains and record carefully.
- expect bloody urine initially
Observe drainage from abdominal dressing and note
color, amount and frequency.
Administer medication for bladder spasms as ordered.
Das könnte Ihnen auch gefallen
- Critical ThinkingDokument6 SeitenCritical ThinkingmatrixtrinityNoch keine Bewertungen
- antepartumTEST1 MOSBYDokument14 SeitenantepartumTEST1 MOSBYmatrixtrinity50% (2)
- Intelligence in PsychologyDokument29 SeitenIntelligence in PsychologymatrixtrinityNoch keine Bewertungen
- Distinguishing Features of Anthropology - Characteristics 1-5 6.78 What Are The3 Unique Approaches of AnthropologyDokument2 SeitenDistinguishing Features of Anthropology - Characteristics 1-5 6.78 What Are The3 Unique Approaches of AnthropologymatrixtrinityNoch keine Bewertungen
- Stress and Illness: Castillo, Justine GDokument19 SeitenStress and Illness: Castillo, Justine GmatrixtrinityNoch keine Bewertungen
- Intestinal Obstruction5Dokument4 SeitenIntestinal Obstruction5matrixtrinityNoch keine Bewertungen
- Socio - GENDER, ETHNICITY AND RACEDokument22 SeitenSocio - GENDER, ETHNICITY AND RACEmatrixtrinity100% (1)
- Group Number: Case Title: Year and Section: Group Members: 1. 5. 2. 6. 3. 7. 4. 8Dokument1 SeiteGroup Number: Case Title: Year and Section: Group Members: 1. 5. 2. 6. 3. 7. 4. 8matrixtrinityNoch keine Bewertungen
- Antepartumtest2 LippincottDokument7 SeitenAntepartumtest2 Lippincottmatrixtrinity100% (1)
- What Is Intestinal ObstructionDokument5 SeitenWhat Is Intestinal ObstructionmatrixtrinityNoch keine Bewertungen
- Cardiovascular Therapeutic ManagementDokument15 SeitenCardiovascular Therapeutic ManagementmatrixtrinityNoch keine Bewertungen
- Cerebrovascular Accidents: Rochee P. Benito, RNDokument23 SeitenCerebrovascular Accidents: Rochee P. Benito, RNmatrixtrinityNoch keine Bewertungen
- Intestinal Obstruction Wit Pic2Dokument2 SeitenIntestinal Obstruction Wit Pic2matrixtrinityNoch keine Bewertungen
- Cardio DiseasesDokument17 SeitenCardio DiseasesmatrixtrinityNoch keine Bewertungen
- Cardiovascular Physio Logic ProcessDokument35 SeitenCardiovascular Physio Logic ProcessmatrixtrinityNoch keine Bewertungen
- Blood ComponentDokument33 SeitenBlood Componentmatrixtrinity100% (1)
- Circulatory System: Rochi Paraon Benito, RN Infection Control NurseDokument15 SeitenCirculatory System: Rochi Paraon Benito, RN Infection Control NursematrixtrinityNoch keine Bewertungen
- Burns and Environmental EmergenciesDokument33 SeitenBurns and Environmental EmergenciesmatrixtrinityNoch keine Bewertungen
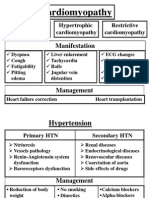
- Cardiomyopathy 02Dokument2 SeitenCardiomyopathy 02matrixtrinityNoch keine Bewertungen
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Nephrology: Edward F. Foote, Pharm.D., FCCP, BCPSDokument32 SeitenNephrology: Edward F. Foote, Pharm.D., FCCP, BCPSandirio7486Noch keine Bewertungen
- An Approach To Drug Induced Delirium in The Elderly BMJDokument7 SeitenAn Approach To Drug Induced Delirium in The Elderly BMJLeonela Ramirez Almanza y Lina Maria Ossa HerreraNoch keine Bewertungen
- Guidelines-Anticoagulation: Heparin & Warfarin: Sydney South West Area Health ServiceDokument27 SeitenGuidelines-Anticoagulation: Heparin & Warfarin: Sydney South West Area Health ServiceDiana MihaiNoch keine Bewertungen
- Pharmacist Workup of Drug Therapy in Pharmaceutical Care: Problem Oriented Pharmacist RecordDokument20 SeitenPharmacist Workup of Drug Therapy in Pharmaceutical Care: Problem Oriented Pharmacist RecordNurwahidah Moh WahiNoch keine Bewertungen
- Drug Dosing in CRRT FinalDokument42 SeitenDrug Dosing in CRRT FinalVrushali MahajanNoch keine Bewertungen
- S 016 LBLDokument23 SeitenS 016 LBLMuhammadAmdadulHoqueNoch keine Bewertungen
- Renal Function TestsDokument7 SeitenRenal Function Testsiyuth dytiartiNoch keine Bewertungen
- Renal Function Tests: Dr. Arisha Sohail Dep. of Biochemistry DimcDokument28 SeitenRenal Function Tests: Dr. Arisha Sohail Dep. of Biochemistry DimcArisha SohailNoch keine Bewertungen
- Protein Debate: Performance MenuDokument33 SeitenProtein Debate: Performance MenuJonasongNoch keine Bewertungen
- Chronic Kidney Disease Case PresentationDokument14 SeitenChronic Kidney Disease Case Presentationnnaesor_109150% (2)
- Article: Matthew K. Abramowitz, Michal L. Melamed, Carolyn Bauer, Amanda C. Raff, and Thomas H. HostetterDokument7 SeitenArticle: Matthew K. Abramowitz, Michal L. Melamed, Carolyn Bauer, Amanda C. Raff, and Thomas H. Hostetterdianaerlita97Noch keine Bewertungen
- CT & MRI Pathology: A Pocket AtlasDokument570 SeitenCT & MRI Pathology: A Pocket AtlasIvraym Barsoum100% (7)
- كتاب اسئلة جميلDokument401 Seitenكتاب اسئلة جميلMohammadSAL-Rawashdeh100% (1)
- Fluids Electrolytes PDFDokument27 SeitenFluids Electrolytes PDFAnonymous rDD9I2Noch keine Bewertungen
- Pathophysiology of DMDokument5 SeitenPathophysiology of DMRgn Mckl100% (3)
- Acute Nephrology For The Critical Care Physician PDFDokument280 SeitenAcute Nephrology For The Critical Care Physician PDFMahtosurup GodavarthyNoch keine Bewertungen
- Nephrology TestDokument112 SeitenNephrology TestRapid Medicine50% (2)
- 007160393X Shargel TOCDokument18 Seiten007160393X Shargel TOCRaju NiraulaNoch keine Bewertungen
- MCQDokument21 SeitenMCQNazaqat FarooqNoch keine Bewertungen
- AKI & Indikasi CRRTDokument25 SeitenAKI & Indikasi CRRTMaya Sari BaharumNoch keine Bewertungen
- 313 - Disorders of Renal and Urinary SystemsDokument8 Seiten313 - Disorders of Renal and Urinary SystemsChrissy Mendoza100% (2)
- Drug Therapy Considerations Across The LifespanDokument43 SeitenDrug Therapy Considerations Across The LifespanhealingnurseNoch keine Bewertungen
- Urea Nitrogen AnalyzerDokument16 SeitenUrea Nitrogen AnalyzerSkywalker_92Noch keine Bewertungen
- Betelehem JimaDokument56 SeitenBetelehem JimaMustafa KhandgawiNoch keine Bewertungen
- Chronic Kidney DiseaseDokument13 SeitenChronic Kidney DiseaseJobelle AcenaNoch keine Bewertungen
- Tanaman 2Dokument10 SeitenTanaman 2Mohamad YasinNoch keine Bewertungen
- Andre Surgery Notes (Ed 3, 2013) W Washington+ChinYeeDokument155 SeitenAndre Surgery Notes (Ed 3, 2013) W Washington+ChinYeeDaniel Lim100% (3)
- Pedia NotesDokument8 SeitenPedia NotesQurrataini IbanezNoch keine Bewertungen
- Reviewer Board ExamDokument10 SeitenReviewer Board ExamKristen Villacarlos83% (6)
- GFRDokument4 SeitenGFRUok RitchieNoch keine Bewertungen