Beruflich Dokumente
Kultur Dokumente
Gangguan Katatonik Organik
Hochgeladen von
Ferji Rhenald Arditya0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
61 Ansichten41 Seitenaa
Originaltitel
gangguan katatonik organik
Copyright
© © All Rights Reserved
Verfügbare Formate
PPTX, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenaa
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPTX, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
61 Ansichten41 SeitenGangguan Katatonik Organik
Hochgeladen von
Ferji Rhenald Ardityaaa
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPTX, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 41
SUPERVISOR
dr. Sabar P. Siregar, Sp.KJ
MORNING REPORT
Monday 2
nd
JuneMay 2014
PATIENT IDENTITY
Name :
Mrs. SN
Sex :
female
Age :
33 years old
Address :
Kebumen
Occupation :
Labor
Marital State :
Married
General education : primary school
RELATIVES IDENTITY
Name : Mr. S
Sex : Male
Age : 58 years old
Relation : father
REASON PATIENT WAS BROUGHT TO
EMERGENCY ROOM
Patient was angry without any reason and
damaging anythings.
STRESSOR
Unclear
PRESENT HISTORY
Angry without reason,
gelisah, keluyuran
Hospitalize in RSJ
2010
she didnt go to work
she couldnt utilize his leisure time
she didnt socialize with neighbor
She poor grooming
she was hospitalized
I : for 1 months in 2010
II : for 1 months in 2012
III : for 1 months in 2013
IV : for 1 months in 2014
DAY OF ADMISSION
02 June 2014
Brought to
hospital by his
father
she cant do his daily activity.
she couldnt socialize with friends
she cant go to work
Poor grooming
Patient brought with the
complaints of:
Angry without reason
unable to sleep
Attact his husband
talking to himself
PSYCHIATRIC HISTORY
No psychiatric history
General
medical history
Head injury (-)
Hypertension (-)
Convulsion (-)
Asthma (-)
Allergy (-)
Drugs and alcohol
abuse history and
smoking history
Drugs consumption (-)
Alcohol consumption (-)
Cigarette Smoking (-)
EARLY CHILDHOOD PHASE (0-3 YEARS OLD)
Psychomotoric
- There were no valid data on patients growth and development such as:
first time lifting the head (3-6 months)
rolling over (3-6 months)
Sitting (6-9 months)
Crawling (6-9 months)
Standing (6-9 months)
walking-running (9-12 months)
holding objects in her hand(3-6 months)
putting everything in her mouth(3-6 months)
Psychosocial
- There were no valid data on which age patient
started smiling when seeing another face (3-6 months)
startled by noises(3-6 months)
when the patient first laugh or squirm when asked to play, nor
playing claps with others (6-9 months)
Communication
- There were no valid data on when patient started bubbling. (6-9 months)
Emotion
- There were no valid data of patients reaction when playing, frightened
by strangers, when starting to show jealousy or competitiveness
towards other and toilet training.
Cognitive
- There were no valid data on which age the patient can follow objects,
recognizing his mother, recognize his family members.
- There were no valid data on when the patient first copied sounds that
were heard, or understanding simple orders.
INTERMEDIATE CHILDHOOD (3-11 YEARS OLD)
Psychomotor
No valid data on when patients first time playing hide and seek or if
patient ever involved in any kind of sports.
Psychosocial
No valid data regarding patient psychosocial.
Communication
No valid data regarding patient ability to make friends at school and
how many friends patient have during his school period
Emotional
No valid data on patients emotional.
Cognitive
No valid data on patients cognitive.
LATE CHILDHOOD & TEENAGE PHASE
Sexual development signs & activity
No data on when patient first experience of menarcher
Psychomotor
No data if patient had any favourite hobbies or games, if patient involved in
any kind of sports.
Psychosocial
No valid data regarding patient psychosocial.
Emotional
No valid data on patients emotional.
Communication
No valid data regarding patient ability to make friends at school and how
many friends patient have during his high school period
ADULTHOOD
Educational History
finished primary school, he
is average student in the
class
Occupational history
In 2008, the patient worked in a
factory, then he was dismissed due
to bankruptcy
2013-now, the patient worked in a
factory
Marital Status
they married in 2005
in 2008, he divorced his wife.
They have 1 child
Criminal History
No Criminal history.
Social Activity
Before he was sick, he was
friendly and had many
friends
Current Situation
He lives with his parents
and his brother
ERIKSONS STAGES OF PSYCHOSOCIAL
DEVELOPMENT
Stage Basic Conflict Important Events
Infancy
(birth to 18 months)
Trust vs mistrust Feeding
Early childhood
(2-3 years)
Autonomy vs shame and doubt Toilet training
Preschool
(3-5 years)
Initiative vs guilt Exploration
School age
(6-11 years)
Industry vs inferiority School
Adolescence
(12-18 years)
Identity vs role confusion Social relationships
Young Adulthood
(19-40 years)
Intimacy vs isolation Relationship
Middle adulthood
(40-65 years)
Generativity vs stagnation Work and parenthood
Maturity
(65- death)
Ego integrity vs despair Reflection on life
FAMILY HISTORY
Patient is the 4
th
child of 6 siblings
There is no psychiatry history in
the family
Genogram
MALE FEMALE Patient
PSYCHOSEXUAL HISTORY
.
Patient realizes that she is a female, and interest to a
male. Her attitude is appropriate as a female
Socio-economic history
Economic scale : low
Validity
Alloanamnesis: valid
Autoanamnesis: valid
Progression of Disorder
Symptom
Role Function
2008
2009 2010
2011
27/05/2014 2013 2012
Appearance
A male, appropriate to his age, completely clothed
State of Consciousness
Cloudy
Speech
Quantity : Decreased
Quality : Decreased
MENTAL STATE
27
TH
MAY 2014
BEHAVIOUR
Hypoactive
Hyperactive
Echopraxia
Catatonia
Active negativism
Cataplexy
Streotypy
Mannerism
Automatism
Bizarre
Command automatism
Mutism
Acathysia
Tic
Somnabulism
Psychomotor agitation
Compulsive
Ataxia
Mimicry
Aggresive
Impulsive
Abulia
ATTITUDE
Non-cooperative
Indiferrent
Apathy
Tension
Dependent
Passive
Infantile
Distrust
Labile
Rigid
Passive negativism
Stereotypy
Catalepsy
Cerea flexibility
Excited
Emotion
Mood
Dysphoric
Euthymic
Elevated
Euphoria
Expansive
Irritable
Agitation
Cant be assesed
Affect
Inappropriate
Restrictive
Blunted
Flat
Labile
Disturbance of Perception
Hallucination
Auditory (-)
Visual (-)
Olfactory (-)
Gustatory (-)
Tactile (-)
Somatic (-)
Illusion
Auditory (-)
Visual (-)
Olfactory (-)
Gustatory (-)
Tactile (-)
Somatic (-)
Depersonalization (-) Derealization (-)
Thought Progression
Quantity
Logorrhea
Blocking
Remming
Mutism
Talk active
Quality
Irrelevant answer
Incoherence
Flight of idea
Poverty of speech
Confabulation
Loosening of association
Neologisme
Circumtansiality
Tangential
Verbigration
Perseveration
Sound association
Word salad
Echolalia
Content of Thought
Idea of Reference
Idea of Guilt
Preoccupation
Obsession
Phobia
Delusion of Persecution
Delusion of Reference
Delusion of Envious
Delusion of Hipochondry
Delusion of magic-mystic
Delusion of grandiose
Delusion of Control
Delusion of Influence
Delusion of Passivity
Delusion of Perception
Thought of Echo
Thought of Insertion &
withdrawal
Thought of Broadcasting
Form of Thought
Non Realistic
Dereistic
Autism
Cannot be evaluated
Sensorium and Cognition
Level of education : primary school
General knowledge : Cant be accessed
Orientation of time : Cant be accessed
Orientations of place : Cant be accessed
Orientations of people : Good
Orientations of situation : Cant be accessed
Working/short/long memory : Cant be accessed
Writing and reading skills : Cant be accessed
Visuospatial : Cant be accessed
Abstract thinking : Cant be accessed
Ability to self care : Cant be accessed
Impulse control when
examined
Self control: enough
Patient response to
examiners question:
bad
Insight
Impaired insight
Intellectual Insight
True Insight
Physical State
Consciousnes : compos mentis
Vital sign :
Blood pressure : 163/78 mmHg
Pulse rate : 92 x/mnt
Temperature : 36.5 C
RR : 20 x/mnt
Head : normocephali, mouth deviation (-)
Eyes : anemic conjungtiva (-), icteric sclera (-), pupil isocore
Neck : normal, no rigidity, no palpable lymph nodes
Thorax:
Cor : S 1,2 regular
Lung : vesicular sound, wheezing -/-, ronchi-/-
Abdomen : Pain (-) , normal peristaltic, tympany sound
Extremity : Warm acral, capp refill <2, motoric strength
Symptoms Mental Status
Impairment
-Behaviour : Hypoactive, catatonia
- Attitude : non-cooperative,
catalepsi
- Affect : Blunted
-Thought Progression : Remming
-Form of Thought : autism
1. -Seizure
2. -unable to
sleep
3. -talking to
himself
4. -angry
without any
reason
5. -disturbing
other people
He cant do his daily
activity.
he couldnt socialize
with friends
He cant go to work
Poor grooming
Decrease appetite
Male 31 years old, appropiate to his age, completely clothed
Differential Diagnosis
F06.1 Katatonik Organic Disorder
F20.4 Skizophrenia Catatonic
Multiaxial Diagnosis
Axis I : F06.1 Catatonik Organic Disorder
Axis II : Z03.2 No Diagnose
Axis III : Hypertension grade II, Seizure
Axis IV : unclear
Axis V : GAF admission 40-31
PROBLEM RELATED TO THE PATIENT
1. Problem about patients life
in 2008, Patients were laid off by the company because to
bankrupt. Patients had been divorced by his wife. he never
met with the child and his wife.
2. Problem about patients biological state
In Schizophrenic patient, there is abnormal balancing of the
neurotransmitter (increasing of dopamine) which has the
contribution for the positive symptoms : have hallucination
and delusion. We need pharmacotherapy to rebalance the
neurotransmitter.
PLANNING MANAGEMENT
Inpatient (hospitalization)
To reduce 50% the symptoms :
1. Seizure
2. unable to sleep
3. talking to himself
4. angry without any reason
5. disturbing other people
6. Poor grooming
7. Decrease appetite
8. hipertension
Response Remission Recovery
RESPONSE PHASE
Target therapy : 50% decrease of symptoms
Emergency department
Inj Diazepam 5 mg IV (sedation)
Inj Lodomer Inj. 1 amp. IM
Maintanance
Clozapine Tab 2x5mg (anti-psykotic)
Captopril Tab 2x12,5 mg (anti hypertension)
Inj. Diazepam 5mg I.V (anti convulsion) *if symptoms occur seizure
PLAN :
EEG
CT-Scan
Re-assess patient
REMISSION PHASE
Target therapy :
100% remission of symptom
Inpatient management
1. Continue the pharmacotherapy: maintenance Haloperidol
2x5mg & captopril Tab 2x12,5 mg,
2. Improving the patient quality of life :
Teach patient about his social & environment
(interact with his family, socialize with his neighbor or friends,
find a hobby to do on his spare time)
Outpatient management
1. Pharmacotherapy
2. Psychosocial therapy
RECOVERY PHASE
Target therapy : 100% remission of symptom within 1 year.
- Continue the medication, control to
psychiatric
- Rehabilitation : help patient to find a
hobby, help patient to interact normally with
her family, his friends and neighbor
- Family education such as tell his family
about patient condition and how much
familly support affect the success of
therapy
Das könnte Ihnen auch gefallen
- Psychiatry PDFDokument53 SeitenPsychiatry PDFArushiNoch keine Bewertungen
- Case History, MSE and Rating Scales - in Psychological AssessmentDokument29 SeitenCase History, MSE and Rating Scales - in Psychological Assessmentsu84Noch keine Bewertungen
- PsychiatryDokument92 SeitenPsychiatrykimNoch keine Bewertungen
- Mental Status ExaminationDokument17 SeitenMental Status ExaminationDharek IleshNoch keine Bewertungen
- 2015 Resident ManualDokument850 Seiten2015 Resident ManualPeter AgabaNoch keine Bewertungen
- UW Notes - 13 - PsychiatryDokument21 SeitenUW Notes - 13 - PsychiatryDor BenayounNoch keine Bewertungen
- Schizophrenia and Biblical Counseling Notes Doc-DrDokument4 SeitenSchizophrenia and Biblical Counseling Notes Doc-DrJulio Cezar de Pinho Jr.Noch keine Bewertungen
- MP 2015 - Term PaperDokument356 SeitenMP 2015 - Term PaperMelvyn Zhang100% (2)
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDokument41 SeitenMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJAyunita PermataNoch keine Bewertungen
- MCQ I II Psych 2 PDFDokument19 SeitenMCQ I II Psych 2 PDFSpacetoon DaysNoch keine Bewertungen
- Psychiatry CourseDokument29 SeitenPsychiatry CourseOmar AbdillahiNoch keine Bewertungen
- 3th Year Residency 2Dokument17 Seiten3th Year Residency 2Spacetoon DaysNoch keine Bewertungen
- Case Study 2Dokument29 SeitenCase Study 2falguni mondalNoch keine Bewertungen
- Coagulation Disorders:: Primary HemostasisDokument58 SeitenCoagulation Disorders:: Primary HemostasisFerji Rhenald Arditya100% (1)
- A Hippocratic Odyssey: Lessons From a Doctor Couple on Life, In Medicine, Challenges and DoctorprneurshipVon EverandA Hippocratic Odyssey: Lessons From a Doctor Couple on Life, In Medicine, Challenges and DoctorprneurshipBewertung: 5 von 5 Sternen5/5 (1)
- Morning Report Details Patient's Organic Manic DisorderDokument40 SeitenMorning Report Details Patient's Organic Manic DisorderWilutami Rahardiyaning TyasNoch keine Bewertungen
- June 2021 MCQ Psychiatry at DAMSDokument61 SeitenJune 2021 MCQ Psychiatry at DAMSAli HusseinNoch keine Bewertungen
- 1000 Plus Psychiatry MCQ Book DranilkakunjeDokument141 Seiten1000 Plus Psychiatry MCQ Book DranilkakunjeChatura UdharaNoch keine Bewertungen
- Psychiatry ExamDokument4 SeitenPsychiatry Examapi-3703352Noch keine Bewertungen
- Psychiatry: Questions&AnswersDokument92 SeitenPsychiatry: Questions&AnswersCielNoch keine Bewertungen
- Psychiatric Case Clerking for Medical StudentsVon EverandPsychiatric Case Clerking for Medical StudentsNoch keine Bewertungen
- SchizophreniaDokument46 SeitenSchizophreniaEmilyne Joy Mendoza CabayaNoch keine Bewertungen
- Dams Psychiatry Pyq Fmge SolvedDokument81 SeitenDams Psychiatry Pyq Fmge SolvedmeetsinhhermaNoch keine Bewertungen
- Morpot 21 SeptDokument41 SeitenMorpot 21 SeptTasia DeastutiNoch keine Bewertungen
- Lecture Notes On PsychiatryDokument38 SeitenLecture Notes On PsychiatrysrossgellNoch keine Bewertungen
- MCQ in Psychiatry Board II Aug 06 PDFDokument5 SeitenMCQ in Psychiatry Board II Aug 06 PDFSpacetoon DaysNoch keine Bewertungen
- TrOn ReferencesDokument11 SeitenTrOn ReferencesAnonymous CbnCgjNoch keine Bewertungen
- Sunday, 24 November 2013 Supervisor: DR Sabar P Siregar SP - KJDokument37 SeitenSunday, 24 November 2013 Supervisor: DR Sabar P Siregar SP - KJMutiara SazkiaNoch keine Bewertungen
- Morning Report 17 SeptemberDokument42 SeitenMorning Report 17 SeptemberkadibhaNoch keine Bewertungen
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDokument47 SeitenMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJVike Poraddwita YuliantiNoch keine Bewertungen
- Sample Psychiatry Questions & Critiques: Question #1Dokument18 SeitenSample Psychiatry Questions & Critiques: Question #1Vik SharNoch keine Bewertungen
- Geriatric Psychiatry LectureDokument113 SeitenGeriatric Psychiatry LectureabrihamNoch keine Bewertungen
- Preoperative Anesthesia and PremedicationDokument10 SeitenPreoperative Anesthesia and PremedicationFlorida Siregar0% (1)
- Daily Self-Discipline: Increase Self-Discipline, Stop Fear & Stress, Hack Your Mind & Influence PeopleVon EverandDaily Self-Discipline: Increase Self-Discipline, Stop Fear & Stress, Hack Your Mind & Influence PeopleNoch keine Bewertungen
- EOP Group D January 2018 RecapDokument7 SeitenEOP Group D January 2018 RecapNadhirah ZulkifliNoch keine Bewertungen
- Morning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDokument40 SeitenMorning Report: Supervisor Dr. Sabar P. Siregar, SP - KJDani Fahma Qur'aniNoch keine Bewertungen
- Use of Psychotropics in PregnancyDokument24 SeitenUse of Psychotropics in Pregnancymanahil waqasNoch keine Bewertungen
- Rapid Antigen Testing Centers Approved by GoAPDokument2 SeitenRapid Antigen Testing Centers Approved by GoAPRambabu Moravineni100% (1)
- Nuero-Psychiatry: Multiple Choice Questions: (Mcqs Model Paper 2007)Dokument25 SeitenNuero-Psychiatry: Multiple Choice Questions: (Mcqs Model Paper 2007)usamaNoch keine Bewertungen
- Black SabbathDokument111 SeitenBlack Sabbathbedah umum fk unpad100% (14)
- Seminar On Organization of Camps and Clinics in Community SettingsDokument18 SeitenSeminar On Organization of Camps and Clinics in Community SettingsRethina Bai C100% (2)
- Mumbai PPN List of HospitalsDokument47 SeitenMumbai PPN List of HospitalsPriyanka PatelNoch keine Bewertungen
- Psychiatry MCQs 2Dokument11 SeitenPsychiatry MCQs 2Majed Alami100% (1)
- Psychiatry Diagnosis PDFDokument4 SeitenPsychiatry Diagnosis PDFEpstein HouseNoch keine Bewertungen
- Terms in The Field of PsychiatryDokument18 SeitenTerms in The Field of PsychiatryOchie YecyecanNoch keine Bewertungen
- Why Psychiatry? Some Thoughts For Medical Students.Dokument3 SeitenWhy Psychiatry? Some Thoughts For Medical Students.Davin TanNoch keine Bewertungen
- Second and Third Year Psychiatry Residency QuizDokument5 SeitenSecond and Third Year Psychiatry Residency QuizSpacetoon Days100% (1)
- Psychiatry Final - Summer 2020!Dokument83 SeitenPsychiatry Final - Summer 2020!Manushi Henadeera100% (1)
- First vs Second Generation Antipsychotics: CATIE & CUtLASS TrialsDokument3 SeitenFirst vs Second Generation Antipsychotics: CATIE & CUtLASS TrialsvinodksahuNoch keine Bewertungen
- 05.psychiatry Fixed by E.G E.KDokument54 Seiten05.psychiatry Fixed by E.G E.KMoataz Trabeh100% (1)
- Gillman's AD Algorithm - PsychotropicalDokument50 SeitenGillman's AD Algorithm - Psychotropicaldo leeNoch keine Bewertungen
- How To Pass The Mrcpsych Examination: DR Bruce OwenDokument34 SeitenHow To Pass The Mrcpsych Examination: DR Bruce OwendanielNoch keine Bewertungen
- Archives of Indian Psychiatry OctoberDokument63 SeitenArchives of Indian Psychiatry OctoberGanpat Vankar100% (1)
- Dr. Ziad Arandi (History - Examination) PDFDokument19 SeitenDr. Ziad Arandi (History - Examination) PDFFiras AnayaNoch keine Bewertungen
- Methadone Clinic Psychiatry CaseDokument11 SeitenMethadone Clinic Psychiatry CaseshafernNoch keine Bewertungen
- Brain Imaging in PsychiatryDokument7 SeitenBrain Imaging in PsychiatryRoci ArceNoch keine Bewertungen
- Higher Education Module ProgramDokument2 SeitenHigher Education Module ProgramWen Jie LauNoch keine Bewertungen
- CWU Psy 3Dokument8 SeitenCWU Psy 3Codillia CheongNoch keine Bewertungen
- Neuroanatomy For The Psychiatrist: Textbook of PsychiatryDokument37 SeitenNeuroanatomy For The Psychiatrist: Textbook of Psychiatrykrysdana22Noch keine Bewertungen
- Introduction to Psychiatry and Behavioural SciencesDokument40 SeitenIntroduction to Psychiatry and Behavioural SciencesSambili TonnyNoch keine Bewertungen
- Notes On PsychiatryDokument10 SeitenNotes On PsychiatryMark VillenaNoch keine Bewertungen
- Psychiatry MilestonesDokument36 SeitenPsychiatry MilestonesrjfeeleyNoch keine Bewertungen
- My Basal GangliaDokument18 SeitenMy Basal GangliaPriya GKNoch keine Bewertungen
- Process of Rehabilitation in PsychiatryDokument29 SeitenProcess of Rehabilitation in PsychiatryRahul Kumar DiwakarNoch keine Bewertungen
- SGPC SSG General Psychiatry DC2299.PDF 48458388Dokument31 SeitenSGPC SSG General Psychiatry DC2299.PDF 48458388AKNTAI002Noch keine Bewertungen
- MRCPsych Log Book (Updated)Dokument30 SeitenMRCPsych Log Book (Updated)Afrah YasinNoch keine Bewertungen
- AOBNP General Certification Exam GuideDokument3 SeitenAOBNP General Certification Exam GuidebunteekNoch keine Bewertungen
- MCMLVNCXMVNXCVCXDokument1 SeiteMCMLVNCXMVNXCVCXFerji Rhenald ArdityaNoch keine Bewertungen
- Hysterectomy, Salphingooverectomy, Adhesiolysis Prof IOM - Docx Ferji MeriDokument4 SeitenHysterectomy, Salphingooverectomy, Adhesiolysis Prof IOM - Docx Ferji MeriFerji Rhenald ArdityaNoch keine Bewertungen
- Ferji LutsDokument24 SeitenFerji LutsFerji Rhenald ArdityaNoch keine Bewertungen
- JEANETDokument7 SeitenJEANETRijma NugrahaNoch keine Bewertungen
- Journal Reading - ECTDokument45 SeitenJournal Reading - ECTFerji Rhenald ArdityaNoch keine Bewertungen
- SEO-Optimized Title for Morning Report DocumentDokument41 SeitenSEO-Optimized Title for Morning Report DocumentFerji Rhenald ArdityaNoch keine Bewertungen
- CCDokument1 SeiteCCFerji Rhenald ArdityaNoch keine Bewertungen
- Thesis Protocol NewDokument11 SeitenThesis Protocol NewChemudupati BharaniNoch keine Bewertungen
- DR Shubranshuprofile PDFDokument4 SeitenDR Shubranshuprofile PDFBablu JiNoch keine Bewertungen
- Hospital Discharge GuideDokument11 SeitenHospital Discharge GuideBetarie Anum AlmiraNoch keine Bewertungen
- Florence Nightingale 1221228702236164 8Dokument5 SeitenFlorence Nightingale 1221228702236164 8Vee Estrada0% (1)
- House Brokerage ReceiptDokument2 SeitenHouse Brokerage Receiptdev dutt dev duttNoch keine Bewertungen
- 2015-06-11 Calvert County TimesDokument24 Seiten2015-06-11 Calvert County TimesSouthern Maryland OnlineNoch keine Bewertungen
- Correction Traumatic LPDokument2 SeitenCorrection Traumatic LPFitrisia 'pipit' AmelinNoch keine Bewertungen
- Elite - The Dark Wheel NovellaDokument43 SeitenElite - The Dark Wheel NovellameNoch keine Bewertungen
- KUMC International Observership Program GuidelinesDokument12 SeitenKUMC International Observership Program Guidelinesসোমনাথ মহাপাত্রNoch keine Bewertungen
- Assessor Non Compliance ObservationDokument9 SeitenAssessor Non Compliance ObservationSwati BajpaiNoch keine Bewertungen
- Brachial Plexus Injuries in Adults PrefaceDokument2 SeitenBrachial Plexus Injuries in Adults PrefaceSatrio Bangun NegoroNoch keine Bewertungen
- HBulletinDokument115 SeitenHBulletinShafiq_R0% (1)
- Villar PRC Cases (DONE)Dokument5 SeitenVillar PRC Cases (DONE)Meijie Vino ManiegoNoch keine Bewertungen
- Traction MethodsDokument11 SeitenTraction MethodsalcaponeNoch keine Bewertungen
- Knowledge, Attitudes and Practices of Nurses Regarding To Post-Operative Pain Management at Hospitals of Arsi Zone, Southeast Ethiopia, 2018Dokument6 SeitenKnowledge, Attitudes and Practices of Nurses Regarding To Post-Operative Pain Management at Hospitals of Arsi Zone, Southeast Ethiopia, 2018kebedeNoch keine Bewertungen
- Rachelle Manuel PobleteDokument4 SeitenRachelle Manuel PobleteRachelle MondidoNoch keine Bewertungen
- CCS Exam Content OutlineDokument2 SeitenCCS Exam Content OutlineSundarajan ManiNoch keine Bewertungen
- Nandakishore cv031821Dokument3 SeitenNandakishore cv031821Nandakishore RajkumarNoch keine Bewertungen
- Introduction of Cancer Center in KMUHDokument36 SeitenIntroduction of Cancer Center in KMUHSantoNoch keine Bewertungen
- Institutionalized ChildrenDokument2 SeitenInstitutionalized ChildrenMuhammad Khan KhosoNoch keine Bewertungen
- Best PracticesDokument21 SeitenBest Practicesjordyn1990Noch keine Bewertungen
- History of The Burroughs Wellcome Fund 1955-2005Dokument100 SeitenHistory of The Burroughs Wellcome Fund 1955-2005Russ Campbell100% (1)
- Implementing Hospital Autonomy in Jordan: An Economic Cost Analysis of Al Karak HospitalDokument98 SeitenImplementing Hospital Autonomy in Jordan: An Economic Cost Analysis of Al Karak HospitalEng-Mohammed Abu NuktaNoch keine Bewertungen
- IRCS Cancer Hospital - Different Health Checkup Packages at Reasonable RatesDokument2 SeitenIRCS Cancer Hospital - Different Health Checkup Packages at Reasonable RatessureshNoch keine Bewertungen
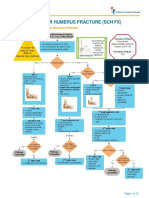
- Fracture Supracondylar HumerusDokument12 SeitenFracture Supracondylar HumeruskemsNoch keine Bewertungen