Beruflich Dokumente
Kultur Dokumente
Kul. 4 Shock
Hochgeladen von
Friska FurnandariOriginalbeschreibung:
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Kul. 4 Shock
Hochgeladen von
Friska FurnandariCopyright:
Verfügbare Formate
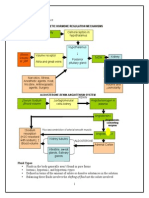
Diagnosis and Management
of Shock
dr. Rudi, Sp.An
SHK 1
Objectives
Identify the major types of shock and principles of
management
Review fluid resuscitation and use of vasopressor and
inotropic agents
Understand concepts of O
2
supply and demand
Discuss the differential diagnosis of oliguria
SHK 2
Shock
Always a symptom of primary cause
Inadequate blood flow to meet tissue oxygen
demand
May be associated with hypotension
Associated with signs of hypoperfusion: mental
status change, oliguria, acidosis
SHK 3
Shock Categories
Cardiogenic
Hypovolemic
Distributive
Obstructive
SHK 4
Cardiogenic Shock
Decreased contractility
Increased filling pressures, decreased LV
stroke work, decreased cardiac output
Increased systemic
vascular resistance compensatory
Hypovolemic Shock
Decreased cardiac output
Decreased filling pressures
Compensatory increase in
systemic vascular resistance
SHK 6
Distributive Shock
Normal or increased cardiac output
Low systemic vascular resistance
Low to normal filling pressures
Sepsis, anaphylaxis, neurogenic,
and acute adrenal insufficiency
SHK 7
Obstructive Shock
Decreased cardiac output
Increased systemic vascular
resistance
Variable filling pressures dependent
on etiology
Cardiac tamponade, tension
pneumothorax, massive pulmonary
embolus
Cardiogenic Shock Management
Treat arrhythmias
Diastolic dysfunction may require
increased filling pressures
Vasodilators if not hypotensive
Inotrope administration
Cardiogenic Shock Management
Vasopressor agent needed if
hypotension present to raise aortic
diastolic pressure
Consultation for mechanical assist
device
Preload and afterload reduction to
improve hypoxemia if blood pressure
adequate
Hypovolemic Shock
Management
Volume resuscitation crystalloid, colloid
Initial crystalloid choices
Lactated Ringers solution
Normal saline (high chloride may produce
hyperchloremic acidosis)
Match fluid given to fluid lost
Blood, crystalloid, colloid
SHK 11
Distributive Shock Therapy
Restore intravascular volume
Hypotension despite volume therapy
Inotropes and/or vasopressors
Vasopressors for MAP < 60 mm Hg
Adjunctive interventions dependent on
etiology
SHK 12
Obstructive Shock Treatment
Relieve obstruction
Pericardiocentesis
Tube thoracostomy
Treat pulmonary embolus
Temporary benefit from fluid or
inotrope administration
Fluid Therapy
Crystalloids
Lactated Ringers solution
Normal saline
Colloids
Hetastarch
Albumin
Gelatins
Packed red blood cells
Infuse to physiologic endpoints
SHK 14
Fluid Therapy
Correct hypotension first
Decrease heart rate
Correct hypoperfusion abnormalities
Monitor for deterioration of oxygenation
SHK 15
Inotropic / Vasopressor Agents
Dopamine
Low dose (2-3 g/kg/min) mild inotrope
plus renal effect
Intermediate dose (4-10 g/kg/min)
inotropic effect
High dose ( >10 g/kg/min) vasoconstriction
Chronotropic effect
SHK 16
Inotropic Agents
Dobutamine
5-20 g/kg/min
Inotropic and variable chronotropic effects
Decrease in systemic vascular resistance
SHK 17
Inotropic / Vasopressor Agents
Norepinephrine
0.05 g/kg/min and titrate to effect
Inotropic and vasopressor effects
Potent vasopressor at high doses
SHK 18
Inotropic / Vasopressor Agents
Epinephrine
Both and actions for inotropic and
vasopressor effects
0.1 g/kg/min and titrate
Increases myocardial O
2
consumption
SHK 19
Therapeutic Goals in Shock
Increase O
2
delivery
Optimize O
2
content of blood
Improve cardiac output and
blood pressure
Match systemic O
2
needs with O
2
delivery
Reverse/prevent organ hypoperfusion
Oliguria
Marker of hypoperfusion
Urine output in adults
<0.5 mL/kg/hr for >2 hrs
Etiologies
Prerenal
Renal
Postrenal
SHK 21
Evaluation of Oliguria
History and physical examination
Laboratory evaluation
Urine sodium
Urine osmolality or specific gravity
BUN, creatinine
SHK 22
Evaluation of Oliguria
Laboratory Test Prerenal ATN
Blood Urea Nitrogen/ >20 1020
Creatinine Ratio
Urine Specific Gravity >1.020 <1.010
Urine Osmolality (mOsm/L) >500 <350
Urinary Sodium (mEq/L) <20 >40
Fractional Excretion of Sodium (%) <1 >2
Therapy in Acute Renal Insufficiency
Correct underlying cause
Monitor urine output
Assure euvolemia
Diuretics not therapeutic
Low-dose dopamine may urine flow
Adjust dosages of other drugs
Monitor electrolytes, BUN, creatinine
Consider dialysis or hemofiltration
SHK 24
Pediatric Considerations
BP not good indication of hypoperfusion
Capillary refill, extremity temperature better
signs of poor systemic perfusion
Epinephrine preferable to norepinephrine due to more
chronotropic benefit
Fluid boluses of 20 mL/kg titrated to BP or total 60
mL/kg, before inotropes or vasopressors
SHK 25
Pediatric Considerations
Neonates consider congenital
obstructive left heart syndrome as cause of
obstructive shock
Oliguria
<2 yrs old, urine volume <2 mL/kg/hr
Older children, urine volume
<1 mL/kg/hr
SHK 26
Das könnte Ihnen auch gefallen
- Fluid & ElectrolyteDokument26 SeitenFluid & Electrolytesanjana bhatia100% (1)
- Cardiogenic ShockDokument20 SeitenCardiogenic Shockanimesh pandaNoch keine Bewertungen
- First Aid - CPR - AED Participant's ManualDokument196 SeitenFirst Aid - CPR - AED Participant's Manualadamiam100% (2)
- Vasoactive DrugsDokument61 SeitenVasoactive DrugsAde Gustina SiahaanNoch keine Bewertungen
- Sample Personal Statement For FellowshipDokument1 SeiteSample Personal Statement For FellowshipAbdul Basit Saeed100% (11)
- Antihypertensive DrugsDokument37 SeitenAntihypertensive Drugsleiann_jessicaNoch keine Bewertungen
- HypertensionDokument85 SeitenHypertensionmelkamu AssefaNoch keine Bewertungen
- Drugs Acting in CVSDokument63 SeitenDrugs Acting in CVSMeghan Norico Cristuta100% (1)
- Management of Shock: Role of Inotropic & Vasoactive DrugsDokument50 SeitenManagement of Shock: Role of Inotropic & Vasoactive DrugsbajaocNoch keine Bewertungen
- Vasoactive TherapyDokument26 SeitenVasoactive Therapylidya agustin100% (1)
- Remedial Part 2Dokument13 SeitenRemedial Part 2Prince Rener Velasco PeraNoch keine Bewertungen
- Shock: Erdiansyah Zulyadaini, MD, FIHA FK Universitas Muhammadiyah Purwokerto/ RSUD Dr. Soeselo Kabupaten TegalDokument47 SeitenShock: Erdiansyah Zulyadaini, MD, FIHA FK Universitas Muhammadiyah Purwokerto/ RSUD Dr. Soeselo Kabupaten TegalFarah AkhwanisNoch keine Bewertungen
- Drugs Affecting The Cardiovascular SystemDokument70 SeitenDrugs Affecting The Cardiovascular SystemRayne Bonifacio100% (2)
- Practice Questions - EDNDokument6 SeitenPractice Questions - EDNKaren BlancoNoch keine Bewertungen
- Letters Combined (11 Referral, 2 Discharge, 1 Transfer)Dokument49 SeitenLetters Combined (11 Referral, 2 Discharge, 1 Transfer)Faisal ImtiazNoch keine Bewertungen
- Fccs - ShockDokument27 SeitenFccs - ShockyuiflashNoch keine Bewertungen
- Drugs Acting On Cardiovascular SystemDokument81 SeitenDrugs Acting On Cardiovascular SystemevaNoch keine Bewertungen
- SupervisorsDokument1 SeiteSupervisorsBOOKREADER_NOW100% (2)
- Diagnosis & Management of Shock: SuriyadiDokument17 SeitenDiagnosis & Management of Shock: SuriyadiDeady NurdiantoNoch keine Bewertungen
- CARESCAPE Monitor B650: Clinical Reference ManualDokument210 SeitenCARESCAPE Monitor B650: Clinical Reference ManualJonathan ScottNoch keine Bewertungen
- Hypovolemic ShockDokument21 SeitenHypovolemic ShockOlga GoryachevaNoch keine Bewertungen
- Shock - Types Pathophysiology and Management: DR - Ravichandra Kumar Anaesthesia ResidentDokument64 SeitenShock - Types Pathophysiology and Management: DR - Ravichandra Kumar Anaesthesia ResidentHarika BandaruNoch keine Bewertungen
- Diagnosis and Management of ShockDokument31 SeitenDiagnosis and Management of ShockAmeliaNoch keine Bewertungen
- Diagnosis and Management of Shock: SHK 1 SHK 1Dokument27 SeitenDiagnosis and Management of Shock: SHK 1 SHK 1Agung NugrohoNoch keine Bewertungen
- Diagnosis Dan Manajemen SyokDokument22 SeitenDiagnosis Dan Manajemen SyokRatika Ayu PiliangNoch keine Bewertungen
- Kuliah Syok 2020 (DR Ahmad Yafiz Hasby SpAn)Dokument48 SeitenKuliah Syok 2020 (DR Ahmad Yafiz Hasby SpAn)RezaNoch keine Bewertungen
- Pemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220Dokument137 SeitenPemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220fahmi rosyadiNoch keine Bewertungen
- 1aAQ9K9el0XG34EBO27zATWpBZ9igCdV6 1Dokument23 Seiten1aAQ9K9el0XG34EBO27zATWpBZ9igCdV6 1Sonia khanNoch keine Bewertungen
- HypertensionDokument43 SeitenHypertensionAbin PNoch keine Bewertungen
- Haemorrhagic Shock, Resuscitation and HaemodynamicsDokument31 SeitenHaemorrhagic Shock, Resuscitation and HaemodynamicsNinaNoch keine Bewertungen
- Cardio Genic and Obstructive ShockDokument66 SeitenCardio Genic and Obstructive ShockdrkurniatiNoch keine Bewertungen
- Session 24 Heart FailureDokument15 SeitenSession 24 Heart Failuredreampurpose97Noch keine Bewertungen
- Approach To ShockDokument30 SeitenApproach To ShocktigistNoch keine Bewertungen
- Cardio Genic ShockDokument6 SeitenCardio Genic ShockDedy HartantoNoch keine Bewertungen
- Approach To Patient With HypertensionDokument64 SeitenApproach To Patient With HypertensionAndrassy Twinkle AlineaNoch keine Bewertungen
- Management of ShockDokument18 SeitenManagement of ShockObongsamuel IdiongNoch keine Bewertungen
- Penatalaksanaan SyokDokument59 SeitenPenatalaksanaan SyokArif NurfadhilahNoch keine Bewertungen
- Shock: Disampaikan Oleh: Dr. I G A G Utara Hartawan, Span MarsDokument88 SeitenShock: Disampaikan Oleh: Dr. I G A G Utara Hartawan, Span MarsNym Angga SantosaNoch keine Bewertungen
- Shock in Children Lecture NewDokument41 SeitenShock in Children Lecture NewDky HartonoNoch keine Bewertungen
- L15-Shock & Resuscitation LectureDokument49 SeitenL15-Shock & Resuscitation LectureYosra —Noch keine Bewertungen
- PBL 1Dokument111 SeitenPBL 1fahmi rosyadiNoch keine Bewertungen
- Shock: William Lawson, MD Division of Allergy, Pulmonary, and Critical Care MedicineDokument41 SeitenShock: William Lawson, MD Division of Allergy, Pulmonary, and Critical Care MedicinerohitNoch keine Bewertungen
- Shock Syndrome: DR Melkamu BDokument62 SeitenShock Syndrome: DR Melkamu BAsteway MesfinNoch keine Bewertungen
- NullDokument58 SeitenNullElteyb Nor eldaimNoch keine Bewertungen
- Terapi Cairan PediatriDokument74 SeitenTerapi Cairan PediatriAnonymous 0SYzMqje2100% (1)
- Arterial Blood Pressure RegulationDokument21 SeitenArterial Blood Pressure Regulationnaresh sharmaNoch keine Bewertungen
- Hypertension and Angina DrugsDokument158 SeitenHypertension and Angina DrugsMelissa SalayogNoch keine Bewertungen
- Vasoactive Drugs (PICUCOURSE)Dokument52 SeitenVasoactive Drugs (PICUCOURSE)surasuarezlopezNoch keine Bewertungen
- Shock in The Pediatric Patient: or Oxygen Don't Go Where The Blood Won't Flow!Dokument63 SeitenShock in The Pediatric Patient: or Oxygen Don't Go Where The Blood Won't Flow!Nishanth BabuNoch keine Bewertungen
- Manajemen ShockDokument47 SeitenManajemen ShockPutry RizqiaNoch keine Bewertungen
- Pharm CH 11 AntihypertensivesDokument42 SeitenPharm CH 11 AntihypertensivesDaniel AdamsNoch keine Bewertungen
- Cardiovascular Drugs 4Dokument31 SeitenCardiovascular Drugs 4ismailaiaibrahimNoch keine Bewertungen
- СердечнаяDokument70 SeitenСердечнаяDaniel FunkNoch keine Bewertungen
- Shock: in Multiple InjuryDokument32 SeitenShock: in Multiple InjuryNazirul HanifNoch keine Bewertungen
- Hypovolemic Shock Cardiogenic Shock Obstructive Shock: Prepared By: HO Tiviyah Mentor: DR Tiong Supervisor: DR Tham MinDokument29 SeitenHypovolemic Shock Cardiogenic Shock Obstructive Shock: Prepared By: HO Tiviyah Mentor: DR Tiong Supervisor: DR Tham MinTeik Wei TanNoch keine Bewertungen
- Lecture 6 Anti HypertensionDokument40 SeitenLecture 6 Anti HypertensionMNGS StudioNoch keine Bewertungen
- Vasoactive TherapyDokument26 SeitenVasoactive Therapylidya agustinNoch keine Bewertungen
- Pharmacology Semi FinalsDokument269 SeitenPharmacology Semi FinalsTrishaNoch keine Bewertungen
- Fluids and Electrolytes and Acid Base PhysiologyDokument64 SeitenFluids and Electrolytes and Acid Base PhysiologyJesserene Mangulad SorianoNoch keine Bewertungen
- Hypovolemic ShockDokument36 SeitenHypovolemic ShockRia CintyaNoch keine Bewertungen
- Pad HPNDokument137 SeitenPad HPNpmm21d229Noch keine Bewertungen
- Cardivascular DrugsDokument27 SeitenCardivascular DrugsYounas BhattiNoch keine Bewertungen
- Emergency Drugs: A Review: Jeselo O. Gorme, RNDokument71 SeitenEmergency Drugs: A Review: Jeselo O. Gorme, RNdodong skyroseNoch keine Bewertungen
- 10.15 Edrian Zulkarnain - ShockDokument42 Seiten10.15 Edrian Zulkarnain - ShockBintang UbamnataNoch keine Bewertungen
- Pulmonary Edema by DR Gireesh Kumar K PDokument16 SeitenPulmonary Edema by DR Gireesh Kumar K PAETCM Emergency medicineNoch keine Bewertungen
- Perspective Plan 2022-27Dokument57 SeitenPerspective Plan 2022-27So kharap kuchNoch keine Bewertungen
- ESTAVILLO, Karen G. (FEVER UTI, CONSTI)Dokument4 SeitenESTAVILLO, Karen G. (FEVER UTI, CONSTI)Karen EstavilloNoch keine Bewertungen
- Project CharterDokument9 SeitenProject CharterTatianaObregon100% (1)
- Telehealth Research and Evaluation Implications For Decision MakersDokument9 SeitenTelehealth Research and Evaluation Implications For Decision Makerscharlsandroid01Noch keine Bewertungen
- Rad 3 PDFDokument5 SeitenRad 3 PDFjovanaNoch keine Bewertungen
- Contraceptive Options For Women and Couples With HIV: Intrauterine Device (Iud or Iucd)Dokument23 SeitenContraceptive Options For Women and Couples With HIV: Intrauterine Device (Iud or Iucd)Sitha MahendrataNoch keine Bewertungen
- Damage Control Orthopaedics DR Bambang SpOT (Salinan Berkonflik Enggar Yusrina 2015-10-14)Dokument37 SeitenDamage Control Orthopaedics DR Bambang SpOT (Salinan Berkonflik Enggar Yusrina 2015-10-14)SemestaNoch keine Bewertungen
- Patient Safety and Quality Improvement 101Dokument81 SeitenPatient Safety and Quality Improvement 101Manasi PandaNoch keine Bewertungen
- 3 Speech and Language Therapy DDokument2 Seiten3 Speech and Language Therapy DBárbara FerreiraNoch keine Bewertungen
- Drug Study - AlleyahDokument10 SeitenDrug Study - AlleyahLorenzo, Alleyah Jaira D.Noch keine Bewertungen
- ENDOCRINE 1.3 Incidentallomas, Conn's SyndromeDokument5 SeitenENDOCRINE 1.3 Incidentallomas, Conn's SyndromeJem QuintoNoch keine Bewertungen
- Block 4 Lung PathDokument31 SeitenBlock 4 Lung PathShalini ShanmugalingamNoch keine Bewertungen
- CsaDokument10 SeitenCsaBEATRIZ CUBILLONoch keine Bewertungen
- Cefotaxime and Ceftriaxone PDFDokument7 SeitenCefotaxime and Ceftriaxone PDFDwi FitriyaniNoch keine Bewertungen
- A 25-Year-Old Man With New-Onset Seizures PDFDokument8 SeitenA 25-Year-Old Man With New-Onset Seizures PDFMr. LNoch keine Bewertungen
- KyphosisDokument3 SeitenKyphosismnatuelNoch keine Bewertungen
- Drug Regulations in India DR Surinder SinghDokument29 SeitenDrug Regulations in India DR Surinder SinghnutelladdictNoch keine Bewertungen
- Varicose Veins Diagnosis and TreatmentDokument7 SeitenVaricose Veins Diagnosis and Treatmenthossein kasiriNoch keine Bewertungen
- EU Digital COVID Certificate Certificat Digital European COVIDDokument2 SeitenEU Digital COVID Certificate Certificat Digital European COVIDDespre FotografieNoch keine Bewertungen
- Advancement in The Recently Development of Sublingual Tablet For Various Diseases A ReviewDokument7 SeitenAdvancement in The Recently Development of Sublingual Tablet For Various Diseases A ReviewEditor IJTSRDNoch keine Bewertungen
- Primary HyperparathyroidismDokument9 SeitenPrimary HyperparathyroidismJamesNoch keine Bewertungen
- Drug Regulatory Agency of Pakistan (DRAP)Dokument12 SeitenDrug Regulatory Agency of Pakistan (DRAP)Mrs YezdaniNoch keine Bewertungen
- Medicinecomplete Clark Drug and PoisonDokument25 SeitenMedicinecomplete Clark Drug and PoisonArménio SantosNoch keine Bewertungen