Beruflich Dokumente
Kultur Dokumente
Pharma CO Vigilance
Hochgeladen von
Sravani ReddyCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Pharma CO Vigilance
Hochgeladen von
Sravani ReddyCopyright:
Verfügbare Formate
CONTENTS
INTRODUCTION
AIM AND OBJECTIVES
GOALS OF PHARMACOVIGILANCE
FUNCTIONS OF PHARMACOVIGILANCE AT VARIOUS LEVELS
ADVERSE DRUG REACTIONS
PHARMACOVIGILANCE IN DRUG REGULATION
PHARMACOVIGILANCE METHODS IN ADR DETECTION
ROLES OF HEALTH PROFESSIONALS
PARTNERS OF PHARMACOVIGILANCE
PREVENTING OF ADRs
MONITORING OF ADRs
CONCLUSION
REFERENCES
WHAT IS PHARMACOVIGILANCE?
Pharmakon (Greek) : Medicinal substances
Vigilia (Latin) : To keep watch
DEFINITION :
The science and activities relating to the detection,
assessment, understanding and prevention of adverse
effects or any drug related problems
All the medicines with the ability to produce the
desired therapeutic effect also have the potential
cause the unwanted adverse effects. The important to
monitor both known and unknown side effects of
medicines in order to determine any new information
related to their safety profile.
AIM :
To identify new information about hazards as associated
with medicines.
OBJECTIVES :
Improve patient care and safety.
Improve public health and safety.
Encourage safe, rational and appropriate use of drugs.
Promote advertising, education and clinical training in
pharmacovigilance.
GOALS OF PHARMACOVIGILANCE
Monitors the quality of drugs.
Identify the health risks involved in
administration of certain drugs.
Prevent harm to patients.
Research and efficacy of the drugs.
NATIONAL PHARMACOVIGILANCE CENTRE
NATIONAL PHARMACOVIGILANCE PROGRAMME
PERIPHERAL PHARMACOVIGILANCE CENTRES
REGIONAL PHARMACOVIGILANCE CENTRE
ZONAL PHARMACOVIGILANCE CENTRE
HOW PHARMACOVIGILANCE WORK?
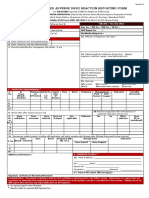
ADR SUSPICION ADR REPORTING
SHARING OF ADR ANALYSIS
FINDINGS
ANALYSIS
RESPONSE
DATA
ADVERSE DRUG REACTIONS
TYPES OF ADRs
Type A effects(augmented) : common ,dose dependent and
predictable
Type B effects (bizzare) : rare, dose independent and
unpredictable
Type C effects (chronic) : after long term therapy no time
relationship
Type D effects (delayed) :may be prevented years after
Type E effects : absence of drug after withdrawn
(end of treatment)
FACTORS AFFECTING SUSCEPTABILITY TO ADRs
1.Age 4.Ethnicity
2.Gender 5.pharmacogenetics
3.co-mobidities & concomitant 6.porphyrias
medicines used
Drug combinations Irrationality
1.Gramnegativeantibacterials+anti
staphylococcal antibiotics
E.g: ampicillin+ cloxacillin
2.Antibacterials+antiamoebi c agents
E.g:ciprofloxacin+metronidazole/ofloxacin+
ornidazole
3.NSAIDS combinations
E.g:nimeslide+diclofenac
4.Antiemetics + Antacids
E.g:dompertidon+ranitidine
5.Antacids+antianxiety drugs
E.g:diazepam+antacids
Results increase resistanse of bacteria,
greater side effects, increase duration of
therapy & cost of treatment.
Ameobiasis and bacterial diarrhoea are
usually foond together in patient.one of
the drugs is wasted.
Risk of nephrotoxicity I increased
Peptic ulcer is not always associated
with emesis. increase cost of treatment.
Antacids reduce the absorption of anti-
anxiety drugs.
DRUGS BANNED IN INDIA
Amidopyrine
Fixed dose combinations of atropine in analgesics and
antipyrine
Fixed dose combinations of strychnine and caffeine in
tonics
Tetracycline liquid oral preparations
Fived dose combinations of penicillins with
sulphonamides
Fixed dose combinations of vitamins with analgesics.
Penicillins skin/eye ointment.
DRUGS PROHIBITED FOR IMPORT
Drugs formulation
Effective data Notification
1.cosmetics licensed as
toothpaste/tooth powder
containing tobacco
2.Parenteral preparations fixed
dose combinations of
streptomycin with penicillin
3.Fixed dose combination of
phenobarbitone with anti-
asthmatic drugs
4.Fenformin
5.Rofecoxib
With immediate
effect
Jan. 1, 1998
Jan. 1, 2002
Oct. 1 , 2003
Dec. 13, 2004
GSR 444(E)
GSR 93(E)
GSR 170(E)
GSR 780(E)
GSR 810(E)
PHARMACOVIGILENCE IN DRUG
REGULATION
CLINICAL TRIAL REGULATION
1.collection of ADR
2.monitoring clinical data
3.reporting of clinical data
POST MARKETING SAFETY MONITORING
PHARMACOVIGILANCE METHODS IN
ADR DETECTION
SPONTANEOUS REPORTING
It is the core data generating system, relying on health
care professionals to identify and report any adverse
events to their NPC, health authority or drug manufacturer
1.Signal detection 2.causality assessment
YELLOW CARD SCHEME
This scheme is operated MHRA ,they submit report on
ADRs using yellow card or on-line form
PUBLISHED CASE REPORTS
The first suspicions of unpredictable reactions may often
be seen in a case report from a practioner e.g: cases of
thalidomide and practolol
COHORT STUDIES
1. These studies monitor large group of patients taking a
particular drug over a period of time
2. These studies can indicate the relative risks associated with
the adverse event in people exposed to drug being studied
CASE-CONTROL STUDIES
1. These studies are an effective method of confirming
whether are not a drug causes given reaction once a
suspicions has been raised.
2.By comparing the prevalence of drug taking between the
groups, it may be possible to identify whether significantly
more people who experienced the event also took a
particular drug.
WHO SHOULD REPORT SAFETY DATA
Physicians
Pharmacists
Pharmaceuticals companies qualified persons-
(pharmacovigilance/regulatory managers).
Investigational products (clinical trails).
Post-approval reporting individual case safety
report(ICSR), periodic safety update reports(PSUR).
In many countries patients are encouraged to report
side effects.
WHAT TO REPORT?
It is important to report serious unexpected ADRs.
Most cases of unexpected ADRs are associated with
medicines newly introduced in the market.
Al suspected adverse reactions.
Every single problem related to the use of a drug.
ADRs associated with the radiology contrast media,
vaccines, diagnostics, drugs in traditionalmedicines,
herbal remedies, cosmetics, medical devices and
equipment.
SYSTEM OF SAFETY DATABASES
Health
professional
Patients
Pharmaceutical
companies
National
Regulatory
Authority
Clinical
Trails
International
Safety databases
Pre-approval
Post-approval
ROLES OF HEALTH PROFESSIONALS
Ensuring medicines are used safely is fundamental to the
role of all health professionals who prescribe, supply,
administer, monitor or advise on their use.
They should take of all relevant patent factors, which may
predispose to an ADR as co-morbidities, concomitant drugs,
renal &liver function and genetic predisposition.
An important role all health professionals is the
documentation identified ADRs.
Identifying and assessing ADRs in clinical practice.
Pharmacists in particular , because of their role in
dispensing prescriptions, may also be involved in educating
and supportying others in preventing ADRs.
PATNERS IN PHARMACOVIGILANCE
The WHO quality assurance and safety: medicines
team
The uppsala monitoring centre (UMC)
Hospitals and academia
Health professionals
Patients
Other partners
PREVENTING OF ADRs
ADRs can be prevented by checking previous ADR history.
Minimizing the use of drugs known to carry high risk of
ADRs.
Tailoring drug selection to individuals based on the factors
which predispose them to ADRs.
Increasing regular review of medicines.
Improved sharing of information about patients between
health care providers.
Increasing availability of guidance on drug selection.
Increase rational prescribing, which may have an effect on
incidence on ADRs.
MONITORING THERAPY
Monitoring the effects of drugs either by direct
measurement of concentration or by measurement of
physiological markers is another potential mechanism to
reduce risk o ADRs.
Advice on monitoring should be clear, provide an evidence-
based frequency of monitoring and acceptable values.
An examination of adequacy of manufacturers advice on
monitoring for haematological ADRs found useful to
prescribers.
CONCLUSION
Pharmacovigilance is used for preventing patients from
being effected unnecessarily.
Work of WHO is the area of safety monitoring of medicines
is necessary if we are to achieve the mission of EDM.
Medicines should be available, affordable safe and properly
used.
Think less about drug safety and more about patient safety.
Think more about impact and consequences of decisions
and non-decisions.
REFERENCES
Clinical pharmacy and therapeutics, Roger walker
and cate whittlesea ; fifth edition.
The importance of WHO 2002.
Who technical report no:498(1972).
Pharmacovigilance pragmatic appraoches, 2001,
Geneva.
Administratio regulatory.
WHO global ICSR database system: basic facts.
Drug information journal 2008.
ICH E2B standard E2B
Data elements for transition of individual case safety reports
ICH E2B standard.
Pharmacovigilance mann RD, Andrews EB, eds.john wiey
& sons ltd, chichester,2002.
Organization ICH.
Organization of Steering committee.
History of involvement in drug safety monitoring by WHO
Sara gambrill,2011 ,chnas pharmacovigilance system: the
hunger for safety insights, clinical leader ,Dec 7,2011
accessed march 28 2014.
Das könnte Ihnen auch gefallen
- Clinical Pharmacy Complete Notes-CompressedDokument355 SeitenClinical Pharmacy Complete Notes-CompressedM. Huzaifa Nasir100% (1)
- Australian Medicines Handbook Pty LTDDokument5 SeitenAustralian Medicines Handbook Pty LTDDia Sb67% (3)
- Medication Error 2017Dokument51 SeitenMedication Error 2017Christina100% (1)
- Pharmacovigilance: The Science of Monitoring Drug SafetyDokument29 SeitenPharmacovigilance: The Science of Monitoring Drug SafetyMaurizio Sessa100% (1)
- ADMEDokument10 SeitenADMEdhavalNoch keine Bewertungen
- Adverse Drug ReactionsDokument54 SeitenAdverse Drug ReactionsAprilVivienCu100% (2)
- Pharmacology Question Bank-1Dokument18 SeitenPharmacology Question Bank-1Abd El-Rahman SalahNoch keine Bewertungen
- Brief Notes On PharmacovigilanceDokument78 SeitenBrief Notes On Pharmacovigilancejay100% (1)
- Equivalencia AntipsicóticosDokument4 SeitenEquivalencia AntipsicóticosLuis Felipe Varela Espinoza100% (1)
- Interview Questions-PVDokument9 SeitenInterview Questions-PVtausif100% (1)
- Ondansetron (Zofran)Dokument1 SeiteOndansetron (Zofran)Cassie100% (1)
- Clinical Trial PhasesDokument11 SeitenClinical Trial Phasesheyyo ggNoch keine Bewertungen
- Electrophoresis DocumentationDokument17 SeitenElectrophoresis DocumentationSravani ReddyNoch keine Bewertungen
- Electrophoresis DocumentationDokument17 SeitenElectrophoresis DocumentationSravani ReddyNoch keine Bewertungen
- Pharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyVon EverandPharmacoepidemiology and Pharmacovigilance: Synergistic Tools to Better Investigate Drug SafetyBewertung: 4.5 von 5 Sternen4.5/5 (3)
- By BhartiDokument17 SeitenBy BhartikundagolNoch keine Bewertungen
- Post-Marketing Drug SurveillanceDokument123 SeitenPost-Marketing Drug SurveillanceRachma DyraNoch keine Bewertungen
- PharmacovigilanceDokument43 SeitenPharmacovigilanceTanoy SahaNoch keine Bewertungen
- PHARMACOVIGILANCEDokument15 SeitenPHARMACOVIGILANCEmanveer84100% (3)
- SMB5401Dokument288 SeitenSMB5401funnymemesworld2023Noch keine Bewertungen
- ADR Reporting, Medication Error Reporting SystemDokument100 SeitenADR Reporting, Medication Error Reporting Systemfarmasi_hm100% (1)
- Systematic Approach in Reporting and Monitoring of Adverse Drug ReactionDokument7 SeitenSystematic Approach in Reporting and Monitoring of Adverse Drug ReactionInternational Journal of Innovative Science and Research TechnologyNoch keine Bewertungen
- Monitoring Efek Samping Obat (MESO)Dokument25 SeitenMonitoring Efek Samping Obat (MESO)Nienies NurikaNoch keine Bewertungen
- Practice School - Bhavya PDFDokument25 SeitenPractice School - Bhavya PDFBhavyaNoch keine Bewertungen
- PharmacovigilanceDokument45 SeitenPharmacovigilancepavani valluriNoch keine Bewertungen
- Adverse Drug Reactions ExplainedDokument71 SeitenAdverse Drug Reactions ExplainedVaibhav ThoratNoch keine Bewertungen
- PharmacovilgilanceDokument60 SeitenPharmacovilgilanceMohanad Al-BayatiNoch keine Bewertungen
- Pharmacovigilance in India: An OverviewDokument42 SeitenPharmacovigilance in India: An OverviewAlkaNoch keine Bewertungen
- Detection and Monitoring of ADRsDokument24 SeitenDetection and Monitoring of ADRsDewiNoch keine Bewertungen
- Irrational Use of DrugDokument9 SeitenIrrational Use of Drugsreedam100% (2)
- Medication Error PDFDokument61 SeitenMedication Error PDFChelsea Ritz MendozaNoch keine Bewertungen
- Pharmacovigilance Presentation on Meaning, Aims, Need and ReportingDokument13 SeitenPharmacovigilance Presentation on Meaning, Aims, Need and ReportingShilpi KhattriNoch keine Bewertungen
- Pharmacovigilance V01Dokument33 SeitenPharmacovigilance V01Karveer AghadeNoch keine Bewertungen
- PharmacoviilanceDokument93 SeitenPharmacoviilancekirti.unadkat70.nuNoch keine Bewertungen
- Guidance On Adverse Drug ReactionsDokument7 SeitenGuidance On Adverse Drug ReactionsAnonymous hF5zAdvwCCNoch keine Bewertungen
- Herbal Drug - Drug InteractionDokument22 SeitenHerbal Drug - Drug Interactionmunni sundaraneedi07Noch keine Bewertungen
- ADRs, Reporting and Causality AssessmentDokument37 SeitenADRs, Reporting and Causality AssessmentRaymond ManjengwaNoch keine Bewertungen
- For Partial Fulfilment of The Requirement For TheDokument45 SeitenFor Partial Fulfilment of The Requirement For ThesalmanNoch keine Bewertungen
- Introduction To Pharmacovigilance UNIT - 1Dokument58 SeitenIntroduction To Pharmacovigilance UNIT - 1meghana vasNoch keine Bewertungen
- Pharmacovigilance: FROMDokument46 SeitenPharmacovigilance: FROMmeyhal17Noch keine Bewertungen
- Manufacturing Pharmacy ADR DetectionDokument29 SeitenManufacturing Pharmacy ADR Detectionheyyo ggNoch keine Bewertungen
- Ad Hoc Data Sources for Pharmacoepidemiological StudiesDokument11 SeitenAd Hoc Data Sources for Pharmacoepidemiological StudiesVINAY KUMARNoch keine Bewertungen
- Basic Pharmacovigilance Interview Questions For FRESHERSDokument8 SeitenBasic Pharmacovigilance Interview Questions For FRESHERSPrakash MishraNoch keine Bewertungen
- Adverse Drug Reaction-Causality Assessment: International Journal of Research in Pharmacy and ChemistryDokument7 SeitenAdverse Drug Reaction-Causality Assessment: International Journal of Research in Pharmacy and ChemistryLalo MaldonadoNoch keine Bewertungen
- Adverse Drug Reaction ADR Monitoring and PharmacovDokument8 SeitenAdverse Drug Reaction ADR Monitoring and PharmacovDipankar NathNoch keine Bewertungen
- Ad Hoc Data Sources for Pharmacoepidemiology StudiesDokument12 SeitenAd Hoc Data Sources for Pharmacoepidemiology StudiesRaju BaiNoch keine Bewertungen
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceVon EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceBewertung: 3 von 5 Sternen3/5 (1)
- Final Patient Safety Alert Medication ErrorsDokument2 SeitenFinal Patient Safety Alert Medication ErrorsAbeer AljNoch keine Bewertungen
- PVCR AssessmentDokument19 SeitenPVCR AssessmentNikitha SreeNoch keine Bewertungen
- Pharmacotherapeutics-CH-1-Pharmacotherapeutics-NotesDokument9 SeitenPharmacotherapeutics-CH-1-Pharmacotherapeutics-Notesmaharachandana18Noch keine Bewertungen
- Advarse Drug ReactionDokument9 SeitenAdvarse Drug ReactionAyanNoch keine Bewertungen
- Adversedrugreactionmonitoringandreporting Pertemuan 14-15Dokument33 SeitenAdversedrugreactionmonitoringandreporting Pertemuan 14-15Ani RahayuNoch keine Bewertungen
- Medication Safety: Improving Public HealthDokument6 SeitenMedication Safety: Improving Public HealthViee Nie SfarmNoch keine Bewertungen
- Importance of Pharmacovigilance For Pharmaceutical IndustryDokument24 SeitenImportance of Pharmacovigilance For Pharmaceutical IndustryPiratesNoch keine Bewertungen
- Pharmacovigilance Ensuring The Safe Use of MedicinesDokument18 SeitenPharmacovigilance Ensuring The Safe Use of MedicinespopadrianionutzNoch keine Bewertungen
- Updated Synopsis 18-10-22Dokument18 SeitenUpdated Synopsis 18-10-22Nikhil KamdiNoch keine Bewertungen
- Introduction To PharmacovigillanceDokument93 SeitenIntroduction To PharmacovigillanceRanjan Kumar MajhiNoch keine Bewertungen
- Dr. Jarir at Thobari, PHD - Basic Pharmacovigilance PDFDokument35 SeitenDr. Jarir at Thobari, PHD - Basic Pharmacovigilance PDFFerina AngeliaNoch keine Bewertungen
- Imp of PVDokument5 SeitenImp of PVrr48843Noch keine Bewertungen
- Introduction to PharmacovigillanceDokument93 SeitenIntroduction to Pharmacovigillancefunnymemesworld2023Noch keine Bewertungen
- Adverse Drug ReactionDokument3 SeitenAdverse Drug ReactionTin SagmonNoch keine Bewertungen
- Knowledge, Attitude and Practice Regarding Adverse Drug Reaction Monitoring & Reporting Amongst Physicians in A Tertiary Care Teaching Hospital, Ahmedabad Indian Journal of Applied ResearchDokument4 SeitenKnowledge, Attitude and Practice Regarding Adverse Drug Reaction Monitoring & Reporting Amongst Physicians in A Tertiary Care Teaching Hospital, Ahmedabad Indian Journal of Applied ResearchChandresh DumatarNoch keine Bewertungen
- NPMCN Update Course 2011 PharmacovigilanceDokument66 SeitenNPMCN Update Course 2011 PharmacovigilanceIsmail RajiNoch keine Bewertungen
- Pharmacovigilance Safety Drug Clinical TrialsDokument58 SeitenPharmacovigilance Safety Drug Clinical TrialsSshan ChaturvediNoch keine Bewertungen
- Analysis of The Strength and Weakness of The Different Methods For Detection of Adverse Drug ReactionsDokument11 SeitenAnalysis of The Strength and Weakness of The Different Methods For Detection of Adverse Drug ReactionsRohitNoch keine Bewertungen
- Improving Medicines Management Guide Prevents HarmDokument49 SeitenImproving Medicines Management Guide Prevents HarmSulfia ArifahNoch keine Bewertungen
- Berlin Declaration On Pharmacovigilance January 2005Dokument28 SeitenBerlin Declaration On Pharmacovigilance January 2005Juan Pablo LópezNoch keine Bewertungen
- A Prospective Study On Antibiotics-Associated Spontaneous Adverse Drug Reaction Monitoring and Reporting in A Tertiary Care HospitalDokument8 SeitenA Prospective Study On Antibiotics-Associated Spontaneous Adverse Drug Reaction Monitoring and Reporting in A Tertiary Care HospitalNurul Hikmah12Noch keine Bewertungen
- Artificial IntelligenceDokument7 SeitenArtificial IntelligenceSravani ReddyNoch keine Bewertungen
- Barcode GeneratorDokument3 SeitenBarcode GeneratorSravani ReddyNoch keine Bewertungen
- Barcode GeneratorDokument3 SeitenBarcode GeneratorSravani ReddyNoch keine Bewertungen
- Guide to Drug Therapy in Patients with Enteral Feeding TubesDokument13 SeitenGuide to Drug Therapy in Patients with Enteral Feeding TubesCecep Dicki HeriyandiNoch keine Bewertungen
- Generic Drugs Assessment and Approval Process in India: Dr. H. G. KoshiaDokument41 SeitenGeneric Drugs Assessment and Approval Process in India: Dr. H. G. KoshiaPrasoon MishraNoch keine Bewertungen
- Kategori Obat VenDokument40 SeitenKategori Obat Venmulla ali qoriNoch keine Bewertungen
- Medication Worksheets: Condition Medication Type Use Nutrition Interactions/Guidelines ExamplesDokument8 SeitenMedication Worksheets: Condition Medication Type Use Nutrition Interactions/Guidelines ExamplesLupuleac ClaudiaNoch keine Bewertungen
- Ethics in Pharmaceutical Industry: Presented byDokument16 SeitenEthics in Pharmaceutical Industry: Presented bysiddheshsonawaneNoch keine Bewertungen
- Medication AdministrationDokument134 SeitenMedication Administrationaryanmohamad210Noch keine Bewertungen
- DDS Lec - 1-3 TransesDokument9 SeitenDDS Lec - 1-3 TransesROSIE ROSALNoch keine Bewertungen
- Evidence Based Validation of Traditional Medicines 2021Dokument1.135 SeitenEvidence Based Validation of Traditional Medicines 2021shubham panditNoch keine Bewertungen
- Pharmacokinetics and Dynamics DefinitionsDokument3 SeitenPharmacokinetics and Dynamics Definitionsو عجلت اليك ربي لترضيNoch keine Bewertungen
- Asynchronous ActivityDokument2 SeitenAsynchronous ActivityNathaniel PulidoNoch keine Bewertungen
- Dose Adjustment in Patients With Liver DiseaseDokument17 SeitenDose Adjustment in Patients With Liver DiseaseNurul Fitrializa ElfNoch keine Bewertungen
- Một số nghiên cứu phác đồ diệt HpDokument20 SeitenMột số nghiên cứu phác đồ diệt HpPhạm Ngọc VănNoch keine Bewertungen
- 120 1 312 1 10 20170109Dokument4 Seiten120 1 312 1 10 20170109Riza TamaNoch keine Bewertungen
- Evolution of Diclofenac Products Using Pharmaceutical Technology PDFDokument19 SeitenEvolution of Diclofenac Products Using Pharmaceutical Technology PDFGhada Abd ElfattahNoch keine Bewertungen
- Natural Products ChemistryDokument12 SeitenNatural Products ChemistryJyotiNoch keine Bewertungen
- Acid Peptic Disease (APD)Dokument73 SeitenAcid Peptic Disease (APD)Uma MounaNoch keine Bewertungen
- International Journal of Research in Pharmacy and ScienceDokument10 SeitenInternational Journal of Research in Pharmacy and ScienceAat Prayoga MuhtarNoch keine Bewertungen
- Ketorolac Tromethamine Tablet PDFDokument5 SeitenKetorolac Tromethamine Tablet PDFrabd samNoch keine Bewertungen
- Multiple-Dosage Regimen (MDR) : Name: Md. Jabedul Alam Sarkar Id: 11715017 Department of Pharmacy, Comilla UniversityDokument14 SeitenMultiple-Dosage Regimen (MDR) : Name: Md. Jabedul Alam Sarkar Id: 11715017 Department of Pharmacy, Comilla Universityjabed sarkarNoch keine Bewertungen
- PatternDokument35 SeitenPatternHJNoch keine Bewertungen
- ADRnewReporting Form 1.4Dokument2 SeitenADRnewReporting Form 1.4Sourabh kundara0% (1)
- DRUG-STUDY (Celecoxib)Dokument3 SeitenDRUG-STUDY (Celecoxib)NicholeGarcesCisnerosNoch keine Bewertungen
- Cc2lab TDM Part1Dokument3 SeitenCc2lab TDM Part1Krisiah Anne HernandezNoch keine Bewertungen
- QtynotifDokument7 SeitenQtynotifrakawidNoch keine Bewertungen