Beruflich Dokumente
Kultur Dokumente
$EBM Prof Darwin 1. Introduction - Prof Sudigdo
Hochgeladen von
Junaida RahmiOriginalbeschreibung:
Originaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
$EBM Prof Darwin 1. Introduction - Prof Sudigdo
Hochgeladen von
Junaida RahmiCopyright:
Verfügbare Formate
jk
klk
Evidence-Based Medicine
(Bringing research evidence into practice)
Evidence-based Medicine
Opinion-based medicine
Experience-based medicine
Power-based medicine
Hope-based medicine
Logic-based medicine
Erratic-based medicine
Obat berbasis Opini
Obat berbasis pengalaman
Obat berbasis-Power
Kedokteran berbasis Harapan
Obat berbasis logika
Obat menentu berbasis
Medicine-based evidence
Pragmatic research
Outcome research
Evidence-based Medicine
Related with morbidity, mortality, & quality of life
Morbidity
Mortality
QoL
Patient
Satisfaction
Health
Status
Value
=
Quality
Cost
Diagnosis
Patient with complaint
History
Physical
Simple test
Specific test
Yes or no answer
Predictive value is the most important
The spectrum of the presentations must resemble
that in practice
Treatment
Patient with certain diagnosis
Does drug X more effective than Y?
Focus on the outcome, rather than its
explanation (biomolecular markers)
Yes or no outcome most useful
Prognosis
Usually in cohort studies
To inform the patient about the fate of the
patient
Absolute risk is more important than relative
risk
Absolute: Your risk of having second stroke in 1 year is 30%
Relative: Your risk of having second stroke in 1 year is 2 times
than in non-smokers (RR = 2)
EBM
Started in early 90s by clinical epidemiologists
1992 : only few articles on EBM
2000 : >1000 articles
Indonesia : started in 1997
Workshops : Yogya (2000)
IKA FKUI (2000, 2001, etc)
Group discussion on EBM / mailing list:
<ebm-f2000@yahoogroups.com>
EBM & Clinical Epidemiology
Fletcher & Fletcher: CE = The application of
epidemiologic principles in problems
encountered in clinical medicine
Sackett et al: CE = The basic science for clinical
medicine
Much resistance by experts
EBM: In principle no one disagree
All major medical journals have adopted EBM
Centers for EBM all over the world
Previous Practice
6 yrs medical
education
40-50 yrs
medical practice
Problems with patients:
Dx, Rx, Px
Consultants, colleagues
Textbooks
Handbooks
Lecture notes
Clinical guidelines
CME, seminars, etc
Journals
Usu. see only Results section,
or even worse, Abstract section
Previous Practice
Trust me
In my experience .
Logically
Textbook, handbook, capita selecta
The results.
Opinion-based medicine
Steroid inj. in prematures to prevent RDS
Routine episiotomy
Routine circumcision
Antibitotics for flu-like syndrome
Use of immunomodulators
Skin test before antibiotic injection
Routine chest X-ray for pre-op preparation
CT scan after minor head trauma
etc
What is
Evidence-based Medicine?
The conscientious, explicit, and judicious use of
current best evidence in making decisions about
the care of individual patients
Pemanfaatan bukti mutakhir yang sahih dalam
tata laksana pasien
Integration of (1) physicians competence
(2) valid evidence from studies
(3) patients preference
Pros : New paradigm in medicine
Extraordinary innovations,
only 2nd to Human Genome Project
Cons : New version of an old song
Fair : Nothing wrong with EBM, but:
Be careful in searching evidence
Meta-analyses, clinical trials, and all study
results should be critically appraised
Keyword for EBM:
Methodological skill to judge the validity of study
reports (Re. Andersen B: Methodo-logical errors in
medical research, 1989)
Years after graduation
Relative
% of
remaining
knowledge
2 4 6 8 10 12
$
100%
THE SLIPPERY SLOPE
WHY EBM?
1. Information overload
2. Keeping current with literature
3. Our clinical performance deteriorates with time
(the slippery slope)
4. Traditional CME does not improve clinical
performance
5. EBM encourages self directed learning process
which should overcome the above shortages
Our textbooks are
out-of-date
Fail to recommend Rx up to ten years after
its been shown to be efficacious.
Continue to recommend therapy up to ten
years after its been shown to be useless.
The Inevitable Consequence
On average, the clinically-important
knowledge of physicians deteriorates
rapidly after we complete our training.
Steps in EBM practice
1. Formulate clinical problems in answerable questions
2. Search the best evidence: use internet or other on-
line database for current evidence
3. Critically appraise the evidence for
Validity (was the study valid?)
Importance (were the results clinically
important?)
Applicability (could we apply to our patient?)
4. Apply the evidence to patient
5. Evaluate our performance
VIA
Main Area
Diagnosis
(Determination of disease or problem)
Treatment
(Intervention necessary to help the patient)
Prognosis
(Prediction of the outcome of the disease)
A 2-year old boy diagnosed presented with 6-
day high fever, conjunctival injection without
secretion, skin rash> blood test shows
leukocytosis, high ESR, CRP +++. He was
suspected to have Kawasaki disease. The
pediatrician is aware of the use of
immunoglobulin to prevent coronary
involvement, but uncertain about the dosage.
Medical students:
(Background question)
What is Kawasaki disease?
What is the etiology?
How it is diagnosed?
What is the treatment of choice?
Complications?
House Officers
(Foreground Question)
In a child with KD, would immuno -
globulin treatment, compared with no
immunoglobulin, reduce the chance to
develop coronary complication?
Foreground
questions
Background
questions
Experience with condition
Other Examples
In women with history of eclampsia, would
administration of low-dose aspirin during pregnancy
prevent eclampsia? (Prevention)
In young women with solitary thyroid nodule, can
USG, compared with biopsy, differentiate between
benign from malignant? (Diagnosis)
In women systemic lupus erythematosus, is history
of congestive heart failure, compared with no heart
failure, worsen the prognosis? (Prognosis)
1
Four elements of good clinical question: P I
C O
The Patient or Problem
The Intervention / Index
Comparative intervention (if relevant)
The Outcome
Four elements of a well constructed clinical
question: PICO
P I C O
The main
intervention
considered
The
alternative
to compare
with the
intervention
Outcome
expected
from this
intervention?
Description
of patient
or problem
B e b r i e f a n d s p e c i f i c
Relevance: Type of Evidence
POE: Patient-oriented evidence
mortality, morbidity, quality of life
DOE: Disease-oriented evidence
pathophysiology, pharmacology,
etiology
POEM
Patient-Oriented
Evidence
Morbity, Mortality
E
Comparing DOES and POEMs
Example
DOE
POEM
Comment
Antiarrhythmic
Therapy
Prostate
screening
PSA screening
detects prostate
Ca. early
? whether PSA
screening
mortality
Antihypertens.
Therapy
Drug A PVC
On ECG
Drug X BP
Drug X
mortality
Drug A >
mortality
DOE & POEM
contradicts
POEM agrees
With DOE
3
Appraising the evidence:
VIA
VIA
Validity: In Methods section:
design, sample, sample size, eligibility criteria
(inclusion, exclusion), sampling method,
randomization method, intervention,
measurements, methods of analysis, etc
Importance: In Results section
characteristics of subjects, drop out, analysis,
p value, confidence intervals, etc
Applicability: In Discussion section + our patients
characteristics, local setting
Example:
Critical appraisal for therapy
Were the subjects randomized?
Were all subjects received similar treatment?
Were all relevant outcomes considered?
Were all subjects randomized included in the
analysis?
Calculate CER, EER, RRR, ARR, and NNT
Were study subjects similar to our patients in
terms of prognostic factors?
Hierarchy of evidence
Weight of
Scientific
Scrutiny
Meta-analysis of RCT
Large RCT
Small RCT
Non-Randomized trials
Observational studies
Case series / reports
Anecdotes, expert, consensus
Level 1
Level 2
Level 3
Level 4
A
B
C
Rec
Implementation of EBM practice:
How to get started
1. Teaching EBM in medical schools / PPDS
Easier than to change the already existing attitude
Most important
May be included in formal curricula or integrated in
existing activities: ward rounds, on calls, case
presentations, group discussions, journal clubs, etc
2. Workshop for teaching staff
3. Workshop for practitioners, incl. nurses
Resistance to EBM teaching & learning
Rudimentary skill in critical appraisal /
methodological skill
Limited resources, esp. time factor
Lack of high quality evidence
Skepticism toward evidence-based practice
Happy with current practice
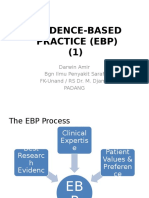
Patients
values
Physicians
competence
Valid
evidence
Formulate
In answerable
question
Search the
evidence
Critically
Appraise
The evidence
Apply
The evidence
Patient
With problem
Criticism to EBM
EBM makes expensive medical care
EBM cannot be implemented in developing
countries
EBM is costly and time consuming
EBM ignore pathophysiology & reasoning
EBM ignore experience and clinical judgment
EB-guidelines etc interfere with professional
autonomy
Criticism to EBM
EBM makes expensive medical care
Cf:
Routine antibiotics for ARTI & diarrhea
Liberal indication for C-section
Unnecessary sophisticated procedures /
exams
Unnecessary / harmful treatment:
steroid for recurrent cough
Criticism to EBM
EBM cannot be implemented in developing countries
By definition EBM is implemented if it is
implementable (patients preference and local
condition) for the benefit of the patients and
the community
Criticism to EBM
EBM is costly and time consuming
EBM does requires facilities at the cost of
quality medical care!
Cost benefit ratio should be assessed in
individual and community levels
Criticism to EBM
EBM ignores pathophysiology & reasoning
EBM encourages clinical reasoning in the light
of valid and important evidence
Pathophysiology and reasoning should be
seen as hypothesis and should end-up in
empirical evidence
Criticism to EBM
EBM ignore experience and clinical judgment
Personal experience and clinical judgment are
by no means can be eliminated
EBM encourage detailed and systematic
documentation of experience and judgment
Subjective experience should be, whenever
possible, translated into more objective
measures
Criticism to EBM
EB-guidelines interfere with professional autonomy
Professional conduct (competence, altruism,
openness, collegiality, ethics) is encouraged in EBM
Every physician should develop their own practice
attitude based on his/her profess-ionalism, valid
evidence, and patients values
Development of clinical guidelines and other
standards of care should be seen as a guide and
implemented according to clinical setting
Advantages of EBM
Encourages reading habit
Improves methodological skill (and willingness
to do research?!)
Encourages rational & up to date management
of patients
Reduces intuition & judgment in clinical
practice, but not eliminates them
Consistent with ethical and medico-legal aspects
of patient management
End Result
Self directed, life-long learning attitude
for high quality patient care
Conclusion
EBM is nothing more than a
framework of systematic use of
current valid study results
relevant to our patient
Das könnte Ihnen auch gefallen
- The Pearls of Communication, History Taking, and Physical Examination: The Road to Passing Clinical ExaminationsVon EverandThe Pearls of Communication, History Taking, and Physical Examination: The Road to Passing Clinical ExaminationsBewertung: 5 von 5 Sternen5/5 (1)
- Evidence Based MedicineDokument52 SeitenEvidence Based MedicineAmie Tahir Rajagukguk100% (1)
- RHU Blue Book 6 - 070852 1Dokument14 SeitenRHU Blue Book 6 - 070852 1Jm Jm100% (1)
- Hydroponics - Introduction To HydroponicsDokument91 SeitenHydroponics - Introduction To HydroponicscorradiniaNoch keine Bewertungen
- Research & Statistics: Evidence Based PracticeDokument34 SeitenResearch & Statistics: Evidence Based Practicevruttika parmar100% (1)
- How To Form An Answerable Pico QuestionDokument32 SeitenHow To Form An Answerable Pico QuestionkxviperNoch keine Bewertungen
- How To Form Answerable QuestionsDokument32 SeitenHow To Form Answerable Questionsapi-150223943Noch keine Bewertungen
- Neuromuscular Blocking DrugsDokument23 SeitenNeuromuscular Blocking DrugsRA TranceNoch keine Bewertungen
- Astm D790-03Dokument11 SeitenAstm D790-03breynnero100% (2)
- Emergency and Disaster NursingDokument13 SeitenEmergency and Disaster Nursingkarenkaren09Noch keine Bewertungen
- Materia Medica For Students - Part-1 - by Ritu KinraDokument253 SeitenMateria Medica For Students - Part-1 - by Ritu KinraAshish Pandey100% (1)
- Well-Built Clinical Question (PICO)Dokument32 SeitenWell-Built Clinical Question (PICO)noniNoch keine Bewertungen
- 01 Introduction To Clinical MedicineDokument30 Seiten01 Introduction To Clinical MedicineYared TJNoch keine Bewertungen
- ENT Scholar Volume 1Dokument93 SeitenENT Scholar Volume 1Dr. T. BalasubramanianNoch keine Bewertungen
- Prioritization of ProblemsDokument8 SeitenPrioritization of ProblemsFirenze Fil100% (3)
- Scaling and Root Planing Presentation - DR - Naaz GillDokument37 SeitenScaling and Root Planing Presentation - DR - Naaz GillNaazGill100% (1)
- NP4 Nursing Board Exam NotesDokument9 SeitenNP4 Nursing Board Exam NotesNewb TobikkoNoch keine Bewertungen
- EVIDENCE-BASED MEDICINE GUIDEDokument34 SeitenEVIDENCE-BASED MEDICINE GUIDEMuhamad Ghifari Azhar100% (1)
- EBNPDokument62 SeitenEBNPShailja Sharma100% (1)
- Introduction - Prof SudigdoDokument49 SeitenIntroduction - Prof Sudigdoyulia fatma nstNoch keine Bewertungen
- EBM Prof Darwin 1. Introduction - Prof SudigdoDokument49 SeitenEBM Prof Darwin 1. Introduction - Prof SudigdoMelda Amalia Sikumbang100% (1)
- Materi Kuliah - Introduction To EBMDokument40 SeitenMateri Kuliah - Introduction To EBMRosi IndahNoch keine Bewertungen
- 6-7. Introduction To Evidence-Based MedicineDokument35 Seiten6-7. Introduction To Evidence-Based MedicinekrisnadewirahadiNoch keine Bewertungen
- Evidence Based MedicineDokument55 SeitenEvidence Based MedicineHelen SusantoNoch keine Bewertungen
- Evidence-Based Practice Resources For HINARI Users: (Module 7.2)Dokument120 SeitenEvidence-Based Practice Resources For HINARI Users: (Module 7.2)thelordhaniNoch keine Bewertungen
- Evidence-Based Practice Resources For HINARI Users: (Module 7.2)Dokument120 SeitenEvidence-Based Practice Resources For HINARI Users: (Module 7.2)thelordhaniNoch keine Bewertungen
- Introduction To Evidence-Based MedicineDokument33 SeitenIntroduction To Evidence-Based MedicineIreine RoosdyNoch keine Bewertungen
- 503 - Using and Teaching Evidence Based Medicine in Child PsychiatryDokument32 Seiten503 - Using and Teaching Evidence Based Medicine in Child PsychiatryAlvaro HuidobroNoch keine Bewertungen
- Pico+Kuliah+Modul+Ebm+2010 EditDokument39 SeitenPico+Kuliah+Modul+Ebm+2010 EditcystanarisaNoch keine Bewertungen
- EBM CYCLE AND PICO QUESTIONDokument40 SeitenEBM CYCLE AND PICO QUESTIONmuthia saniNoch keine Bewertungen
- Evidence Based Medicine: by Dr. Balgis Msc. CM FMDokument125 SeitenEvidence Based Medicine: by Dr. Balgis Msc. CM FMPartone MoviemakerNoch keine Bewertungen
- Evidence Based Medicine: Didik Setiawan, PHD., AptDokument42 SeitenEvidence Based Medicine: Didik Setiawan, PHD., Aptmeiliadiana48Noch keine Bewertungen
- Introduction to Evidence-Based MedicineDokument18 SeitenIntroduction to Evidence-Based MedicineLastry WardaniNoch keine Bewertungen
- Cita Sympo Workshop EBM FKUA PICO HighlightDokument54 SeitenCita Sympo Workshop EBM FKUA PICO HighlightSultan Rahmat SeptianNoch keine Bewertungen
- Critical Appraisal: An Introduction to Evidence-Based PracticeDokument59 SeitenCritical Appraisal: An Introduction to Evidence-Based Practicebabah79Noch keine Bewertungen
- EBM Guide to Evidence Based MedicineDokument34 SeitenEBM Guide to Evidence Based MedicineHiya KontetNoch keine Bewertungen
- Introduction To Evidence-Based Case Report (EBCR)Dokument48 SeitenIntroduction To Evidence-Based Case Report (EBCR)Mohammad Taufik PwNoch keine Bewertungen
- Clinical ReasoningDokument60 SeitenClinical ReasoningFrances DeiNoch keine Bewertungen
- PICO - Indah S. Widyahening PDFDokument39 SeitenPICO - Indah S. Widyahening PDFJordan FadhillaNoch keine Bewertungen
- محاضرة رقم 3 البرهانDokument38 Seitenمحاضرة رقم 3 البرهانareejjooryNoch keine Bewertungen
- Ebm C2Dokument53 SeitenEbm C2Anonymous UHnQSkxLBDNoch keine Bewertungen
- EBP Process: Ask Clinical Questions & Search EvidenceDokument24 SeitenEBP Process: Ask Clinical Questions & Search EvidenceMelda Amalia SikumbangNoch keine Bewertungen
- EBP Presentation Session 5 - 4th March 2021Dokument52 SeitenEBP Presentation Session 5 - 4th March 2021Vuluwa GeorgeNoch keine Bewertungen
- Good PICO QuestionDokument122 SeitenGood PICO QuestionFerdy Lainsamputty100% (1)
- Introduction To Evidence-Based MedicineDokument16 SeitenIntroduction To Evidence-Based MedicineGunung MahameruNoch keine Bewertungen
- Evidence-Based Therapy For Emergency Cases in The Era of Controversial TherapyDokument36 SeitenEvidence-Based Therapy For Emergency Cases in The Era of Controversial TherapyMasda Kamarullah RibasNoch keine Bewertungen
- EBP: Formulating Clinical QuestionsDokument44 SeitenEBP: Formulating Clinical QuestionsDiah agung100% (1)
- Fome EbmDokument40 SeitenFome EbmTry Mutiara100% (1)
- Ebm Therapeutics Lecture For MsucomDokument51 SeitenEbm Therapeutics Lecture For MsucomKenneth NuñezNoch keine Bewertungen
- Evidence Based Medicine (EBM)Dokument41 SeitenEvidence Based Medicine (EBM)adelllblNoch keine Bewertungen
- Evidence Based Medicine (EBM) : Tim FomeDokument31 SeitenEvidence Based Medicine (EBM) : Tim Fomenurul ramadhiniNoch keine Bewertungen
- Ebm Dalam Pendidikan Profesi 2009Dokument45 SeitenEbm Dalam Pendidikan Profesi 2009dian_c87Noch keine Bewertungen
- BIOSTAT MIDTERM: EVALUATING CLINICAL TRIALSDokument14 SeitenBIOSTAT MIDTERM: EVALUATING CLINICAL TRIALSRoh BilalNoch keine Bewertungen
- Evidence-Based Medicine MamanDokument79 SeitenEvidence-Based Medicine MamanAlma WijayaNoch keine Bewertungen
- Introduction To Evidence-Based MedicineDokument16 SeitenIntroduction To Evidence-Based MedicineSheilla ElfiraNoch keine Bewertungen
- Developing Clinical Questions: Clinton Pong, MD Randi Sokol, MD, MPHDokument34 SeitenDeveloping Clinical Questions: Clinton Pong, MD Randi Sokol, MD, MPHRani AndikaNoch keine Bewertungen
- EBCRDokument19 SeitenEBCRdoddydrNoch keine Bewertungen
- Prev MedDokument51 SeitenPrev MedJam JamaNoch keine Bewertungen
- Drug Development: Basic: Phase I-III: Overview of Clinical TrialsDokument71 SeitenDrug Development: Basic: Phase I-III: Overview of Clinical TrialsKomal KhanNoch keine Bewertungen
- Evidence Based-How To Ask An Answerable QuestionsDokument66 SeitenEvidence Based-How To Ask An Answerable QuestionsQiqin DechrifentoNoch keine Bewertungen
- Evidence Based Medicine For General Practitioner: Agus WidiyatmokoDokument61 SeitenEvidence Based Medicine For General Practitioner: Agus WidiyatmokodewisuryandariNoch keine Bewertungen
- Evidence Based Practice First PartDokument31 SeitenEvidence Based Practice First PartRon OpulenciaNoch keine Bewertungen
- Introduction To Evidence Based Medicine: Pediatric Clerkship LsuhscDokument19 SeitenIntroduction To Evidence Based Medicine: Pediatric Clerkship LsuhscAdhika WijayantiNoch keine Bewertungen
- EBM IntroductionDokument49 SeitenEBM IntroductionFanny AgustiaWandanyNoch keine Bewertungen
- Use of EBM in Developing CPGDokument50 SeitenUse of EBM in Developing CPGHilma Nadhifa100% (1)
- DOC-20240331-WA0012.Dokument4 SeitenDOC-20240331-WA0012.Sreeja ReddyNoch keine Bewertungen
- Evidence Based Practice: Ilham, Ners, M. KepDokument17 SeitenEvidence Based Practice: Ilham, Ners, M. KepBaiq ItaNoch keine Bewertungen
- Bahan Kuliah 2011 EBM - PendahuluanDokument34 SeitenBahan Kuliah 2011 EBM - PendahuluanararapiaNoch keine Bewertungen
- 1 s2.0 S0165032714008222 PDFDokument7 Seiten1 s2.0 S0165032714008222 PDFJunaida RahmiNoch keine Bewertungen
- 1 s2.0 S0376871615014295 PDFDokument1 Seite1 s2.0 S0376871615014295 PDFJunaida RahmiNoch keine Bewertungen
- 1 s2.0 S0165032714008222 PDFDokument7 Seiten1 s2.0 S0165032714008222 PDFJunaida RahmiNoch keine Bewertungen
- 1 s2.0 S1028455915002983 PDFDokument5 Seiten1 s2.0 S1028455915002983 PDFJunaida RahmiNoch keine Bewertungen
- 2 Kuliah Sense OrganDokument20 Seiten2 Kuliah Sense OrganJunaida RahmiNoch keine Bewertungen
- 1 s2.0 S0924977X15302224 PDFDokument2 Seiten1 s2.0 S0924977X15302224 PDFJunaida RahmiNoch keine Bewertungen
- 1 PDFDokument3 Seiten1 PDFJunaida RahmiNoch keine Bewertungen
- Kuliah OiDokument61 SeitenKuliah OiNovasuryatiNoch keine Bewertungen
- 1 s2.0 S0165032714008222 PDFDokument7 Seiten1 s2.0 S0165032714008222 PDFJunaida RahmiNoch keine Bewertungen
- 4 Kuliah Ecg 2Dokument70 Seiten4 Kuliah Ecg 2Junaida Rahmi100% (1)
- KP 2.1.6.4&8 Infertilitas Dan Kontrasepsi PriaDokument57 SeitenKP 2.1.6.4&8 Infertilitas Dan Kontrasepsi PriaMuhammad Ari AnugrahNoch keine Bewertungen
- 4 Kuliah Ecg 2Dokument70 Seiten4 Kuliah Ecg 2Junaida Rahmi100% (1)
- Helminth PictureDokument11 SeitenHelminth PictureJunaida RahmiNoch keine Bewertungen
- Helminth PictureDokument11 SeitenHelminth PictureJunaida RahmiNoch keine Bewertungen
- Virus DnaDokument24 SeitenVirus DnaJunaida RahmiNoch keine Bewertungen
- Epidemiology Risk and Causation ReportDokument24 SeitenEpidemiology Risk and Causation ReportJunaida RahmiNoch keine Bewertungen
- EBM Prof Darwin 4. Prognosis EBM - DR KuntjoroDokument29 SeitenEBM Prof Darwin 4. Prognosis EBM - DR KuntjoroJunaida RahmiNoch keine Bewertungen
- Latihan Fisher Exact TestDokument4 SeitenLatihan Fisher Exact TestJunaida RahmiNoch keine Bewertungen
- Tugas Irma SerianaDokument6 SeitenTugas Irma SerianaJunaida RahmiNoch keine Bewertungen
- EBM Prof Darwin 4. Prognosis EBM - DR KuntjoroDokument29 SeitenEBM Prof Darwin 4. Prognosis EBM - DR KuntjoroJunaida RahmiNoch keine Bewertungen
- Epidemiology Risk and Causation ReportDokument24 SeitenEpidemiology Risk and Causation ReportJunaida RahmiNoch keine Bewertungen
- Jawaban Analisis VariansDokument6 SeitenJawaban Analisis VariansJunaida RahmiNoch keine Bewertungen
- MiconazoleDokument3 SeitenMiconazoleapi-3797941Noch keine Bewertungen
- Boards Garden Ph-2Dokument32 SeitenBoards Garden Ph-2Vijay KumarNoch keine Bewertungen
- Formulation of Mosquito Repellent Lotion by Using Oregano (, Neem Tree and Lemongrass Extracted OilDokument9 SeitenFormulation of Mosquito Repellent Lotion by Using Oregano (, Neem Tree and Lemongrass Extracted OilSimi- Simi0% (1)
- Emergency drugs study guideDokument75 SeitenEmergency drugs study guideQuinonez Anna MarieNoch keine Bewertungen
- DylasisDokument3 SeitenDylasisyuvi087Noch keine Bewertungen
- Aonla: Aonla (Emblica Officinalis) or Indian Gooseberry Is Indigenous To Indian Sub-Continent. India Ranks First inDokument21 SeitenAonla: Aonla (Emblica Officinalis) or Indian Gooseberry Is Indigenous To Indian Sub-Continent. India Ranks First inphani kumarNoch keine Bewertungen
- EAU Pocket Guideline 2021Dokument525 SeitenEAU Pocket Guideline 2021Maria Angelica Rodriguez100% (1)
- Nervous System WorksheetDokument3 SeitenNervous System WorksheetaNoch keine Bewertungen
- 1 Septicemia, & SepsisDokument14 Seiten1 Septicemia, & SepsisfgrNoch keine Bewertungen
- Chapter 22: Young Adult Edelman: Health Promotion Throughout The Life Span, 8th EditionDokument10 SeitenChapter 22: Young Adult Edelman: Health Promotion Throughout The Life Span, 8th Editionmarvado10100% (1)
- Tests for Liver Function: Serum BilirubinDokument4 SeitenTests for Liver Function: Serum BilirubinHiba EmadNoch keine Bewertungen
- University of Cambridge Local Examinations Syndicate Biomedical Admissions TestDokument20 SeitenUniversity of Cambridge Local Examinations Syndicate Biomedical Admissions TestNeil SahooNoch keine Bewertungen
- Gluten Free Marketing Program - OUTLINEDokument8 SeitenGluten Free Marketing Program - OUTLINEslipperinoNoch keine Bewertungen
- Medical Physics - RespiratoryDokument9 SeitenMedical Physics - RespiratoryAhmad wastiNoch keine Bewertungen
- Oral Myiasis PublicationDokument6 SeitenOral Myiasis PublicationAnkita GoklaniNoch keine Bewertungen
- The Positive Effects of Tourism With Horse Riding On Human Health - C. Yıldırım, H. Çalışkan, M. T. Koçkar, A. E. Ün, M. Ünlüoğlu, 2018Dokument15 SeitenThe Positive Effects of Tourism With Horse Riding On Human Health - C. Yıldırım, H. Çalışkan, M. T. Koçkar, A. E. Ün, M. Ünlüoğlu, 2018M. Tekin KOÇKARNoch keine Bewertungen
- FOCAL DYSTONIA-A NEUROLOGICAL CONDITION-TREATED WITH CAUSTICUM - Karl Robinson MDDokument2 SeitenFOCAL DYSTONIA-A NEUROLOGICAL CONDITION-TREATED WITH CAUSTICUM - Karl Robinson MDFaker FockerNoch keine Bewertungen
- Diabetes & Metabolic Syndrome: Clinical Research & ReviewsDokument5 SeitenDiabetes & Metabolic Syndrome: Clinical Research & ReviewsPetra Diansari ZegaNoch keine Bewertungen
- TG - Health 10 - Q2Dokument76 SeitenTG - Health 10 - Q2Pitski Zulueta VIINoch keine Bewertungen
- Full HD English Editorials 2-1-2022Dokument25 SeitenFull HD English Editorials 2-1-2022uihuyhyubuhbNoch keine Bewertungen
- Diabetes Mellitus (D9)Dokument92 SeitenDiabetes Mellitus (D9)Alishba MushtaqNoch keine Bewertungen