Beruflich Dokumente
Kultur Dokumente
Antikoagulasi Pada Hemodialisis
Hochgeladen von
AndriKusuma0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
143 Ansichten24 SeitenDokumen tersebut membahas berbagai metode antikoagulasi yang digunakan pada hemodialisis, termasuk unfractionated heparin, low molecular weight heparin, regional heparin/protamine, dan citrate. Metode-metode tersebut dimaksudkan untuk mencegah pembekuan darah pada sirkuit ekstrakorporal sambil meminimalkan risiko perdarahan.
Originalbeschreibung:
Originaltitel
Antikoagulasi pada Hemodialisis.ppt
Copyright
© © All Rights Reserved
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenDokumen tersebut membahas berbagai metode antikoagulasi yang digunakan pada hemodialisis, termasuk unfractionated heparin, low molecular weight heparin, regional heparin/protamine, dan citrate. Metode-metode tersebut dimaksudkan untuk mencegah pembekuan darah pada sirkuit ekstrakorporal sambil meminimalkan risiko perdarahan.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
143 Ansichten24 SeitenAntikoagulasi Pada Hemodialisis
Hochgeladen von
AndriKusumaDokumen tersebut membahas berbagai metode antikoagulasi yang digunakan pada hemodialisis, termasuk unfractionated heparin, low molecular weight heparin, regional heparin/protamine, dan citrate. Metode-metode tersebut dimaksudkan untuk mencegah pembekuan darah pada sirkuit ekstrakorporal sambil meminimalkan risiko perdarahan.
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 24
Dipergunakan pada Hemodialisis sejak 1960-an
Tujuan yang diharapkan adalah memberikan
dosis seoptimal mungkin untuk mencegah
terjadinya pembekuan pada extracorporeal
sirkuit dan meminimalisir resiko komplikasi
perdarahan
Faktor pencetus pembekuan extracorporeal sirkuit :
a. Low blood flow
b. High hematokrit
c. High ultrafiltration rate
d. Dyalisis access recirculation
e. Intradialytic blood and blood product transfusion
f. Intradialytic lipid infusion
g. Use of drip chambers (air exposure,foam formation,turbulence)
Penilaian koagulasi selama Dialisis
Visual inspeksi, tanda-tandanya :
1. Extremely dark blood
2. Shadows or black streaks in the dialyzer
3. Foaming with subsequent clot formation in drip chambers and venous
trap
4. Presence of clots at the arterial side header
Tekanan extracorporeal sirkuit
Tampilan Dialiser setelah dialisis
Pengukuran volume residual dialiser
Koagulasi pada pasien dialisis
Dapat terjadi 5-10% selama 3-4 jam sesi dialisis
Resiko kehilangan darah hingga 100-150ml
Mengurangi luas permukaan membran dialiser volume
dialiser
Mengurangi adekuasi hd
Penggunaan jenis membran juga akan meningkatkan aktivasi
koagulasi mis. Cellulose (cuprophane)
Pertimbangan penggunaan antikoagulasi berbeda-beda
AS ------- Unfractioned heparin
European Union ----------- low molecular weight heparin
Unfractionated Heparin
Inaktivasi faktor-faktor pembekuan terutama faktor Xa
Membentuk komplek heparin-trombin-antitrombin
aktifitas antitrombin (heparin dgn 18 sakarida)
Half life : 30 menit - 2 jam
Dapat diberikan rutin pada pasien yang tidak mempunyai
resiko perdarahan
Ada 2 cara :
a. Bolus 2000 IU (3-5 mnt) drip 1000 IU/jam
b. Bolus 3000-4000 IU ; diulang jika perlu 1000-2000 IU
Unfractionated Heparin
Dihentikan 30-60 mnt sebelum akhir dialisis
Target ACT 200-250 detik (angka normal 90-140 detik)
Efek samping : gatal, alergi, osteoporosis, hiperlipidemia (
aktivitas lipoprotein lipase hipertrigliserida),
trombositopenia dan perdarahan
Heparin Induce Trombositopenia (HIT)
HIT 1 non imun , dapat kembali normal
HIT 2 antibodi terhadap heparin-platelet faktor 4 kompleks ,
tidak dapat kembali normal
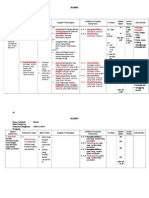
ANTIKOAGULAN
1. Antikoagulan rutin
a. Kontinyu
b. Bolus berulang
2. Heparinisasi minimal
(resiko perdarahan sedang)
3. Dialisis bebas heparin
(resiko perdarahan besar)
ANTIKOAGULAN
Resiko perdarahan sedang
o perkarditis
o riwayat perdarahan kurang
dari 48 jam
o setelah pemasangan
tunneled catheter kurang dari
24 jam
o pembedahan minor kurang
dari 72 jam
o pembedahan mata dan
pembedahan besar dalam 3-7
hari
Resiko perdarahan tinggi
o bleeding diathesis
o penyakit dengan
gangguan faktor
pembekuan
o perdarahan aktif
o pembedahan mata dan
pembedahan besar
kurang dari 72 jam
o perdarahan intrakranial
kurang dari 7 hari
Heparinisasi Minimal
Heparin diberikan bolus 500 unit setiap 30 menit, untuk
mencapai target ACT 150-200 detik
Dapat juga dengan teknik bolus heparin 5-10 unit/kg,
dilanjutkan tanpa heparin atau infus sangat pelan 250-500
unit/jam. Jika nilai ACT menurun atau terlihat pembekuan
darah, maka bolus heparin 500 unit dapat diberikan diantara
infus kontinyu
Dialisis Bebas Heparin
Bilas sirkuit dialisis dengan NaCL 0,9% yang telah dicampur
heparin 3000-5000 unit
Bilas dan keluarkan cairan tersebut diatas (jangan dimasukkan ke
dalam tubuh pasien)
Gunakan secepat mungkin aliran darah (Qb 250 ml/mnt)
Bilas sirkulasi dialisis tiap 15-30 menit dengan NaCl 0,9% sebanyak
25-200 ml untuk mencegah pembekuan di jalur arteri
Naikkan laju ultrafiltrasi untuk mengeluarkan NaCl ekstra
Perhatikan dialiser dan awasi tekanan vena dengan hati-hati untuk
mendeteksi tanda-tanda awal pembekuan darah
Hindari pemberian tranfusi darah
Naikkan UF goal
Dialisis Bebas Heparin
HD selama 2-3 jam
Penggunaan membran polysulfone (lowest
trombogenicity)
Low Molecular Weight Heparin(LMWH)
Depolymerised fractions of heparin obtained by chemical or enzymatic
treatment of UFH
Anionic glycosaminoglycans
2 - 9 kDa but mostly around 5kDa ie 15 saccharide units
less coagulation inhibitory
LMWH binds with antithrombin III to inhibit factor Xa, but mostly (50-70%) does
not have the second binding sequence needed to inhibit thrombin due to
smaller size/length
Affinity to Xa vs Thrombin is 2.5-3 to 1
Only cleared by renal/dialysis mechanisms
Can be monitored by Anti-Factor Xa activity in plasma
Administered into venous limb as cleared by hi-flux membrans
Low Molecular Weight Heparin(LMWH)
Convenience of single administration
less dialysis membrane associated clotting, fibrin deposition
and cellular debris
Less non specific binding
Less binding to platelets- less platelet dysfunction
Less binding to endothelium- fewer interactions between von
Willebrand factor, platelets and endothelium
Minor beneficial changes in lipid profile LDL/VLDL//HDL Heparin
Lower K - heparin induces inhibition of mineralocorticoid metabolism
reduced adrenal aldosterone secretion. Less aldosterone inhibition
with LMWH
Cost disadvantage
Low Molecular Weight Heparin(LMWH)
Because of high bioavailability and predictable effect monitoring
may not be required.
Anti-Xa Testing may be used for
monitoring of effect during/end dialysis
ensure no accumulation at beginning of next dialysis - to
adjust dose in subsequent dialyses
Low Molecular Weight Heparin(LMWH)
The findings of a meta-analysis showed that LMW heparin and
unfractionated heparin were similarly safe and effective in
preventing extracorporeal circuit thrombosis
11 studies included
No significant differences in terms of bleeding or thrombosis
Safety and efficacy of low molecular weight heparins forhemodialysis in patients
with end-stage renal failure: a metaanalysis of randomized trials. Lim W; Cook
DJ; Crowther MA J Am Soc Nephrol 2004 Dec;15(12):3192-206.
Regional
Heparin / Protamine
Infuse Heparin into arterial line (coming out of patient)
Infuse Protamine into venous return line
Technically difficult, no significant advantage over low dose
heparin
Protamine has shorter half life than heparin, also R.E. system
frees heparin from protamine-heparin complex therefore
increased risk of bleeding 2-4 hrs post dialysis
1 mg protamine neutralises 90-115 USP U heparin
Not in HITS!!
No longer a recommended technique
Regional
Heparin / Protamine
Regional
CITRATE
Infusion of iso-osmotic trisodium citrate or hypertonic
trisodium citrate into arterial side of circuit - binds ionised
calcium and inhibits clotting cascade
Citrate-calcium complex partly removed by dialyser
Needs or is Enhanced by calcium (and Mg) free dialysate
Infuse 5% CaCl into venous return at 0.5ml/min
May need low-bicarb Dialysate to avoid alkalosis if daily dialysis
Frequent measures of plasma calcium eg 2hrly
Regional
CITRATE
PROBLEMS
Too complex to be a routine method-maybe in bleeding pt
Requires two infusion pumps and two infusion solns
Risk of life threatening Low or High Calcium
Hypernatraemia a risk if using hypertonic NaCitrate - use low Na
dialysate
Metabolic alkalosis - from metabolism of citrate
ADVANTAGES
Bleeding complications reduced compared to low dose heparin
Improves biocompatibility - reduced granulocyte activation
Reduced deposition of blood components on dialysis membrane
compared to UFH or LMWH
Simplified protocols being developed
Das könnte Ihnen auch gefallen
- Kasus Antikoagulan Pada Pasien HDDokument16 SeitenKasus Antikoagulan Pada Pasien HDmesi purnama100% (1)
- Antikoagulan Pada HD EditDokument15 SeitenAntikoagulan Pada HD EditRaja LaknatNoch keine Bewertungen
- OPTIMASI GIZI DIALISISDokument25 SeitenOPTIMASI GIZI DIALISISWisnu Surya PamungkasNoch keine Bewertungen
- Resep HD AkutDokument31 SeitenResep HD AkutBukuPilihanNoch keine Bewertungen
- CAPDDokument22 SeitenCAPDlindaNoch keine Bewertungen
- HD Prescr 2Dokument52 SeitenHD Prescr 2Gerrard Ella100% (2)
- Askep CapdDokument22 SeitenAskep CapdAndre PoeyNoch keine Bewertungen
- Perawatan Komplikasi Pada Pasien Continuous Ambulatory Peritoneal Dialisis Ipdi JabarDokument59 SeitenPerawatan Komplikasi Pada Pasien Continuous Ambulatory Peritoneal Dialisis Ipdi JabarBuCil RidixNoch keine Bewertungen
- Perawatan Peritoneal Kateter Dan Exit Site Dalam PD - PPT - YuningsihDokument13 SeitenPerawatan Peritoneal Kateter Dan Exit Site Dalam PD - PPT - YuningsihDefan Dapat Titik TerangNoch keine Bewertungen
- Sop TerminasiDokument3 SeitenSop TerminasiHannyNoch keine Bewertungen
- Checklist Perawatan Hemocath HDDokument2 SeitenChecklist Perawatan Hemocath HDFance Ronaldo100% (1)
- HD DialisisDokument3 SeitenHD DialisissantiNoch keine Bewertungen
- Penatalaksanaan Ultrafiltrasi Terpisah1Dokument10 SeitenPenatalaksanaan Ultrafiltrasi Terpisah1rukmaNoch keine Bewertungen
- Stenosis AV Shunt Pada Pasien HemodialisaDokument1 SeiteStenosis AV Shunt Pada Pasien HemodialisaMuhamad LutfiNoch keine Bewertungen
- Terapi Pengganti GinjalDokument6 SeitenTerapi Pengganti GinjalYusuf Ali Quddusi100% (2)
- Tips Merawat Akses CiminoDokument4 SeitenTips Merawat Akses CiminoNissa SusantiNoch keine Bewertungen
- 07-Edukasi Pasien CAPDDokument33 Seiten07-Edukasi Pasien CAPDFanny soronganNoch keine Bewertungen
- Komplikasi CAPDDokument57 SeitenKomplikasi CAPDagazi hendryNoch keine Bewertungen
- Metode SleddDokument62 SeitenMetode SleddSalam SalmaNoch keine Bewertungen
- HEMODIALISADokument20 SeitenHEMODIALISAchacha1203Noch keine Bewertungen
- DOKUMENDokument2 SeitenDOKUMENRSPM100% (1)
- Anemia Pada Gagal GinjalDokument22 SeitenAnemia Pada Gagal GinjalvputrikartikaNoch keine Bewertungen
- DIALYZER REUSE (MNHU PODIN JAN 2021) (Edited)Dokument33 SeitenDIALYZER REUSE (MNHU PODIN JAN 2021) (Edited)wanda100% (1)
- Pendokumentasian Di Unit HDDokument24 SeitenPendokumentasian Di Unit HDKhairul YulianNoch keine Bewertungen
- Presentase Mengakhiri HDDokument17 SeitenPresentase Mengakhiri HDhemodialisa rsifNoch keine Bewertungen
- RSUP Sanglah CDL tunellingDokument1 SeiteRSUP Sanglah CDL tunellingYoseph BugaNoch keine Bewertungen
- Persiapan HDDokument12 SeitenPersiapan HDDEDE PURINoch keine Bewertungen
- Pap 3.6 Spo Penatalaksanaan Kegawatan Selama HemodialisaDokument3 SeitenPap 3.6 Spo Penatalaksanaan Kegawatan Selama HemodialisamitaoktavNoch keine Bewertungen
- HEMODIALISIS PELAYANANDokument11 SeitenHEMODIALISIS PELAYANANwawan100% (1)
- Pengambilan Sampel Pemeriksaan Adekuasi Dialisis CapdDokument3 SeitenPengambilan Sampel Pemeriksaan Adekuasi Dialisis CapdHygiena Kumala SuciNoch keine Bewertungen
- DIALISER REUSEDokument7 SeitenDIALISER REUSEfaustinaNoch keine Bewertungen
- Tata Laksana Pasien HemodialisisDokument39 SeitenTata Laksana Pasien HemodialisisAndri RaisNoch keine Bewertungen
- Clinical Pathway CKDDokument6 SeitenClinical Pathway CKDHaerul gumilarNoch keine Bewertungen
- Laporan Kasus SledDokument8 SeitenLaporan Kasus SledNana HdarpaNoch keine Bewertungen
- MEDICAL KNOWLEDGE ON CAPD AND CKD MANAGEMENTDokument112 SeitenMEDICAL KNOWLEDGE ON CAPD AND CKD MANAGEMENTDina AryaniNoch keine Bewertungen
- Spo Sled DGN Mesin BelcoDokument2 SeitenSpo Sled DGN Mesin BelcoCerilNoch keine Bewertungen
- PreeklamsiaDokument35 SeitenPreeklamsiawina nafullaniNoch keine Bewertungen
- Rencana Asuhan KeperawatanDokument4 SeitenRencana Asuhan Keperawatanangga agustiniNoch keine Bewertungen
- PENANGANAN PASIEN HEMODIALISIS DENGAN COVID 19Dokument43 SeitenPENANGANAN PASIEN HEMODIALISIS DENGAN COVID 19Putri Anena AyuNoch keine Bewertungen
- SEMINAR IPDI KORWIL 6Dokument8 SeitenSEMINAR IPDI KORWIL 6agusmerirojaNoch keine Bewertungen
- Dializer PDFDokument41 SeitenDializer PDFaris budionoNoch keine Bewertungen
- Pedoman Unit HDDokument16 SeitenPedoman Unit HDruthmindosiahaanNoch keine Bewertungen
- SOP PDDokument4 SeitenSOP PDelsaNoch keine Bewertungen
- Terapi Pengganti Ginjal BerkesinambunganDokument9 SeitenTerapi Pengganti Ginjal Berkesinambunganhartanto_budi6222Noch keine Bewertungen
- CAPD pasien anemia obat eritropuitinDokument2 SeitenCAPD pasien anemia obat eritropuitinIrwan WicaksonoNoch keine Bewertungen
- CRRT AKIDokument51 SeitenCRRT AKImartinNoch keine Bewertungen
- REFERAT HemodialisaDokument24 SeitenREFERAT HemodialisaYuli AnaNoch keine Bewertungen
- Pedoman Penatalaksanaan Dialisis OkDokument32 SeitenPedoman Penatalaksanaan Dialisis OkUsman A Dy100% (1)
- Basic CAPD Fisiologi - HSDDokument70 SeitenBasic CAPD Fisiologi - HSDzaroziNoch keine Bewertungen
- PPK HEMODIALISA Lebih 2xDokument9 SeitenPPK HEMODIALISA Lebih 2xRanti HumaeraNoch keine Bewertungen
- A To Z About HemodialisaDokument45 SeitenA To Z About Hemodialisanurul ainNoch keine Bewertungen
- Komplikasi IntradilaisisDokument46 SeitenKomplikasi IntradilaisisBuCil Ridix100% (1)
- Sap HD2Dokument10 SeitenSap HD2Ipcln CikarangNoch keine Bewertungen
- Penanganan Emboli UdaraDokument2 SeitenPenanganan Emboli Udarama riantoNoch keine Bewertungen
- HEMODIALISADokument39 SeitenHEMODIALISAhemodialisa rsudbatusangkar100% (1)
- Adekuasi HemodialisisDokument9 SeitenAdekuasi HemodialisisRahmahani AisyahNoch keine Bewertungen
- Komplikasi Non Infeksi CAPD IPDI Okt2020Dokument46 SeitenKomplikasi Non Infeksi CAPD IPDI Okt2020ronyheryadiNoch keine Bewertungen
- HEMODIALISISDokument23 SeitenHEMODIALISISsarsihNoch keine Bewertungen
- Heparinisasi PPT Teti HDDokument24 SeitenHeparinisasi PPT Teti HDAchmad DainuriNoch keine Bewertungen
- Hemodialisis dan AnticoagulanDokument24 SeitenHemodialisis dan AnticoagulanFITRINoch keine Bewertungen
- 2a. Form Analisis SKL MapelDokument16 Seiten2a. Form Analisis SKL MapelAndriKusumaNoch keine Bewertungen
- 1d. Form Analisis SI-SK-KDDokument19 Seiten1d. Form Analisis SI-SK-KDAndriKusumaNoch keine Bewertungen
- 2c. Form Analisis SKL SatdikDokument3 Seiten2c. Form Analisis SKL SatdikAndriKusumaNoch keine Bewertungen
- 2a. Form Analisis SKL MapelDokument16 Seiten2a. Form Analisis SKL MapelAndriKusumaNoch keine Bewertungen
- Form. Analisis Standar PengelolaanDokument6 SeitenForm. Analisis Standar PengelolaanAndriKusumaNoch keine Bewertungen
- Contoh Instr. Validasi KTSPDokument7 SeitenContoh Instr. Validasi KTSPro3zaqNoch keine Bewertungen
- 2a. Form Analisis SKL MapelDokument16 Seiten2a. Form Analisis SKL MapelAndriKusumaNoch keine Bewertungen
- Form SilabusDokument4 SeitenForm SilabusAndriKusumaNoch keine Bewertungen
- 2b. Form. Analisis Kelp. MapelDokument3 Seiten2b. Form. Analisis Kelp. MapelAndriKusumaNoch keine Bewertungen
- Analisis Kondisi Lingk. EksternalDokument1 SeiteAnalisis Kondisi Lingk. EksternalAndriKusumaNoch keine Bewertungen
- AKSES VASKULARDokument43 SeitenAKSES VASKULARAndriKusuma100% (4)
- Antikoagulasi Pada HemodialisisDokument24 SeitenAntikoagulasi Pada HemodialisisAndriKusumaNoch keine Bewertungen
- 1d. Form Analisis SI-SK-KDDokument19 Seiten1d. Form Analisis SI-SK-KDAndriKusumaNoch keine Bewertungen
- 11.00-12.00 Membran DializerDokument44 Seiten11.00-12.00 Membran DializerAndriKusumaNoch keine Bewertungen
- Askep CKDDokument9 SeitenAskep CKDAndriKusumaNoch keine Bewertungen
- Contoh Instr. Validasi KTSPDokument7 SeitenContoh Instr. Validasi KTSPro3zaqNoch keine Bewertungen
- Kerangka Penyusunan KTSPDokument30 SeitenKerangka Penyusunan KTSPAndriKusumaNoch keine Bewertungen
- 11.00-12.00 Membran DializerDokument44 Seiten11.00-12.00 Membran DializerAndriKusumaNoch keine Bewertungen
- ASkep Ggk-UkaDokument7 SeitenASkep Ggk-UkaAndriKusumaNoch keine Bewertungen
- Contoh Instr. Validasi KTSPDokument7 SeitenContoh Instr. Validasi KTSPro3zaqNoch keine Bewertungen
- Kebutuhan Ruang HDDokument2 SeitenKebutuhan Ruang HDAndriKusumaNoch keine Bewertungen
- Kerangka Penyusunan KTSPDokument30 SeitenKerangka Penyusunan KTSPAndriKusumaNoch keine Bewertungen
- Prota Promes SMT 2 Xi Ipa NewDokument7 SeitenProta Promes SMT 2 Xi Ipa NewAndriKusumaNoch keine Bewertungen