Beruflich Dokumente
Kultur Dokumente
NCM 103-Cardio Anatomy & Physio
Hochgeladen von
louradelOriginaltitel
Copyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
NCM 103-Cardio Anatomy & Physio
Hochgeladen von
louradelCopyright:
Verfügbare Formate
The
Cardiovascular
System
Ms. Louradel Ulbata-Alfonso,MAN, RN
Heart
A hollow muscular organ
Located in thorax between 2
lungs
4 chambers
2 atria (atrium) & 2 ventricles
4 valves
2 separate pumps (R & L
sides)
Right side receives blood from
the body and sends it to the
lungs (pulmonary)
Left side receives blood from
lungs and sends it to the body
(systemic)
PMI midclavicular line @ 5
th
IC space
Position of Heart
3 LAYERS:
1. ENDOCARDIUM
2. MYOCARDIUM
3. EPICARDIUM
Layers of the Heart
Pericardium
Myocardium
Fibrous pericardium
Serous pericardium (parietal layer)
Pericardial space
Serous pericardium (visceral layer - Epicardium)
Endocardium
The heart lies between
the lungs in a region
called the
mediastinum.
heart is wrapped by
some membranes that
also hold the heart in
its position relative to
the diaphragm and
lungs.
The Pericardium
The pericardium is the set of membranes around the
heart. It is actually composed of three layers of
membranes.
visceral pericardium - the innermost
parietal pericardium - the middle,
fibrous pericardium - the outer one is the extra one,
and is tough.
Pericardial Cavity- tiny space between the
visceral pericardium and the parietal
pericardium
15-50 ml
Pericardial Effusion VS Cardiac
Tamponade
Layers of the Heart
Pericardium
Myocardium
Fibrous pericardium
Serous pericardium (parietal layer)
Pericardial space
Serous pericardium (visceral layer - Epicardium)
Endocardium
CORONARY ARTERIES
L & R coronary arteries supply arterial
blood to the heart
Originate from the aorta above the aortic
valve leaflets
Perfused during diastole
HR Blood flow myocardial
ischemia
Heart has high metabolic requirements
(extract 70-80% of the oxygen delivered)
LEFT CORONARY ARTERIES
3 BRANCHES
1. Left main coronary artery
2. Left anterior descending artery
anterior wall of the heart
3. Circumflex artery circles around to the
lateral left wall of the heart
CORONARY ARTERIES
RIGHT CORONARY ARTERY
Right coronary artery
- inferior wall of the heart
Posterior descending artery
- posterior wall of the heart
- Drains into the coronary sinus
CORONARY ARTERIES
Coronary Arteries
Atherosclerosis is an accumulation
of fat on the inner walls of arteries.
When coronary arteries become
partially blocked.angina
When coronary arteries become
significantly blocked.myocardial
infarction
Chambers of the Heart
Valves of the Heart
4 valves
One way flow
Leaky valve = heart murmur
2 atrioventricular valves
Left AV valve- bicuspid or mitral
Right AV valve- tricuspid
2 semilunar valves
Pulmonic semilunar valve
Aortic semilunar valve
Valves of the Heart
Tricuspid Valve
Mitral Valve
Pulmonic
Valve
Aortic Valve
Atrioventricular Valves
1. Right AV valve
Between right atrium and right ventricle
Also called the tricuspid valve because it has three cusps.
Cusps close when right ventricle contracts.preventing blood
from going back up into the right atrium
2. Left AV valve
Between the left atrium and the left ventricle
Also called the bicuspid valve because it only has two cusps
Also called the mitral valve
Cusps close when left ventricle contracts.preventing blood
from back up into the left atrium
Semilunar Valves
1. Pulmonary semilunar valve
When right ventricle contracts, blood is forced
through this valve to enter pulmonary trunk
2. Aortic semilunar valve
When left ventricle contracts, blood is forced
through this valve to enter the aorta
Papillary muscles located on the sides of the
ventricular walls and and connected to the valve
leaflets by thin fibrous bands called CHORDAE
TENDINAE
CHORDAE TENDINAE
2 Pumps
Blood flow in the Heart
CARDIAC
ELECTROPHYSIOLOGY
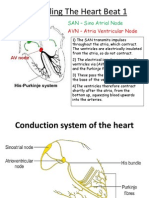
Cardiac Conduction System
The cardiac conduction system generates
and transmits impulses that stimulate
contraction of the myocardium.
Under normal circumstances, the conduction
system first stimulate the contraction of the
atria and then the ventricles.
CONDUCTION SYSTEM
SA NODE- main regulator of HR
- transmit impulse to the surrounding atrial
muscle.
AV NODE- transmit impulses to the
surrounding ventricular muscle.
BUNDLE OF HIS- continuation of AV Node
and has a left and right bundles and fuse
with purkinje fibers.
PURKINJE FIBERS- terminal branches of the
conduction system and are responsible for
carrying the wave of depolarization to both
ventricular walls.
10/17/2014
10/17/2014
2 TYPES OF SPECIALIZED ELECTRICAL
CELLS IN THE HEART
1. NODAL CELLS
2. PURKINJE CELLS
These provide synchronization
ELECTRICAL CELLS
Nodal Cells SA and AV nodes
Purkinje Cells Purkinje Fibers
3 Physiologic Properties of the Electrical Cells
Excitability. The ability of the heart to depolarize in response to a
stimulus. Once stimulated, the whole heart muscle contracts. It is
influenced by hormones, electrolytes, nutrition, oxygen supply,
medications, infection, and nerve characteristics.
- The ability to RESPOND
Automaticity/Rhythmicity. The ability of cardiac cells to initiate an
impulse spontaneously and repetitively, without external
neurohormonal control.
Conductivity. The ability of the heart muscle fibers to
propagate/ transmit electrical impulses along and across
cell membranes.
CONDUCTION SYSTEM OF
THE HEART
SA NODE (Primary pacemaker)
AV NODE
Bundle of his
R bundle L bundle
branch branch
PURKINJE FIBERS
VENTRICULAR CONTRACTIONS
Conduction System of the Heart
CARDIAC
ELECTROPHYSIOLOGY
CARDIAC
ELECTROPHYSIOLOGY
CARDIAC ACTION POTENTIAL
IONS
1. Sodium
2. Potassium
3. Calcium
3 PHASES
1. Resting membrane state
2. Depolarization
3. Repolarization
REFRACTORY PERIODS
Myocardial cells must COMPLETELY
repolarize (rest) before they can
depolarize/ stimulated again
2 PHASES:
1. Effective/ Absolute refractory period
2. Relative refractory period
ABSOLUTE REFRACTORY
Cell is COMPLETELY UNRESPONSIVE
to any electrical impulse
It is INCAPABLE of initiating early
depolarization
RELATIVE REFRACTORY
If an electrical stimulus is stronger than
normal, the cell may depolarize early or
prematurely
Early depolarization of atrium or ventricle
premature contractions
DYSRHYTHMIAS
CARDIAC HEMODYNAMICS
Principle that fluids flow from a region of
higher pressure to a region of lower
pressure
Cardiac Cycle- refers to the events
of one complete heart beat. The length of the
cardiac cycle is usually about 0.8 sec.
Systole (contraction of the muscle)- there
is ventricular pumping, the chambers of
the heart become smaller as the blood is
ejected. Occurs secondary to
depolarization of cells
Diastole (relaxation of the muscle)- there
is ventricular filling, the heart chambers fill
with blood in preparation for subsequent
ejection.
Cardiac Output
Volume of blood ejected per minute
Each ventricle ejects approximately 70mL of
blood/ beat
Averages between 4-8L/min
CO = Stroke volume X heart rate
=70 ml X 60 beats/min
=4,200 ml/min
Changes in SV and HR affects cardiac output
Controls of the heart
1. AUTONOMIC NS
- sympathetic and parasym
2. CNS and baroreceptors and
chemoreceptors
Baroreceptors
- aortic arch and R & L internal carotid
arteries
- sensitive to changes in BP
Chemoreceptors
- sensitive to CO2 level
Subdivisions of ANS
Parasympathetic acetylcholine produces
inhibitory response
Sympathetic catecholamines stimulate
Increase heart rate Beta 1 receptors
Dilate smooth muscles Beta 2 receptors
Vasoconstrict vessels Alpha receptors
Stroke Volume Is Determined
By Three Factors
Preload
Afterload
Contractility
Preload
Degree of stretch of myocardial fibers
Determined by the volume of blood in left
ventricle (LV) at end of diastole
Increased blood volume increased
preload- increased cardiac output (CO)
Decreased blood volume decreased
preload decreased cardiac output (CO)
Frank- Starling Law-the critical factor controlling
stroke volume is how much the cardiac muscle cells
are stretched just before the contract. The more they
are stretched, the stronger the contraction will be. The
important factor stretching the heart muscles is the
venous return.
Factors Which Increase
Preload
IV fluids
Blood
Vasoconstriction
Factors Which Decrease
Preload
Diuretics
Dehydration
Hemorrhage
Vasodilation
Resistance or pressure the ventricles must
overcome to pump blood out
Left ventricle (LV) affected by systemic
vascular resistance (SVR)
Right ventricle (RV) affected by pulmonary
vascular resistance (PVR)
Related to arterial pressure or diameter of
arteries
As pressure increases, resistance
increases, afterload increases
As pressure decreases, resistance
decreases, afterload decreases
Contractility
Force generated by the myocardium when it
contracts inotropic property
END
Das könnte Ihnen auch gefallen
- Heart Blood HistoDokument53 SeitenHeart Blood HistoAnonymous 52lBinNoch keine Bewertungen
- Cadiac Cycle, Heart Sound, ECG, HypertensionDokument110 SeitenCadiac Cycle, Heart Sound, ECG, HypertensionNilesh100% (1)
- EKG Interpretation Basics Guide: Electrocardiogram Heart Rate Determination, Arrhythmia, Cardiac Dysrhythmia, Heart Block Causes, Symptoms, Identification and Medical Treatment Nursing HandbookVon EverandEKG Interpretation Basics Guide: Electrocardiogram Heart Rate Determination, Arrhythmia, Cardiac Dysrhythmia, Heart Block Causes, Symptoms, Identification and Medical Treatment Nursing HandbookNoch keine Bewertungen
- Chapter 15 - Cardiovascular SystemDokument89 SeitenChapter 15 - Cardiovascular SystemOliver Namyalo100% (1)
- Bio Rev CardsDokument21 SeitenBio Rev CardsTamannaBhatiaNoch keine Bewertungen
- Heart Valves and Blood FlowDokument8 SeitenHeart Valves and Blood FlowKyle MañiboNoch keine Bewertungen
- 3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumDokument3 Seiten3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumAebee Alcaraz100% (1)
- How Bloodis Propelled Throughthe Hum An Ci Rcula To Ry Sy StemDokument5 SeitenHow Bloodis Propelled Throughthe Hum An Ci Rcula To Ry Sy Stemridwan100% (1)
- 8 - DR. Khaled - Cardiac SurgeryDokument26 Seiten8 - DR. Khaled - Cardiac SurgeryMuhand.Noch keine Bewertungen
- The Cardiac Cycle: Chapter 19Dokument62 SeitenThe Cardiac Cycle: Chapter 19BishwambherNoch keine Bewertungen
- Tavi 150923155743 Lva1 App6892Dokument157 SeitenTavi 150923155743 Lva1 App6892Zhivka KostadinovaNoch keine Bewertungen
- Ekg Panum or OsceDokument69 SeitenEkg Panum or OsceGladish RindraNoch keine Bewertungen
- 1 s2.0 S1109966616302226 Main PDFDokument6 Seiten1 s2.0 S1109966616302226 Main PDFdenisseNoch keine Bewertungen
- NAGA COLLEGE FOUNDATION ANATOMY & PHYSIOLOGY LABORATORYDokument4 SeitenNAGA COLLEGE FOUNDATION ANATOMY & PHYSIOLOGY LABORATORYPado100% (1)
- Hemodynamics: DR Axelle Saverettiar Mbbs Physiology Department SSR Medical CollegeDokument31 SeitenHemodynamics: DR Axelle Saverettiar Mbbs Physiology Department SSR Medical CollegeÑäd ÉèmNoch keine Bewertungen
- CH 11 Heart NotesDokument2 SeitenCH 11 Heart Notesummnicole0% (1)
- Properties of Cardiac Muscle and Conducting SystemsDokument38 SeitenProperties of Cardiac Muscle and Conducting Systemsnirilib100% (4)
- Hemodynamic Monitoring Guide (39Dokument49 SeitenHemodynamic Monitoring Guide (39Pratami Rieuwpassa IINoch keine Bewertungen
- Electrical Axis: Fast & Easy Ecgs - A Self-Paced Learning ProgramDokument29 SeitenElectrical Axis: Fast & Easy Ecgs - A Self-Paced Learning ProgramMihaela PrisacaruNoch keine Bewertungen
- Physiology notes on cardiac muscle and the heart's conductive systemDokument37 SeitenPhysiology notes on cardiac muscle and the heart's conductive systemDany SamuelNoch keine Bewertungen
- ELECTROCARDIOGRAM by Aldrin Jayson AlmadenDokument23 SeitenELECTROCARDIOGRAM by Aldrin Jayson AlmadenItsMe AJNoch keine Bewertungen
- Basics & Timing-PmDokument120 SeitenBasics & Timing-PmWiwik Puji Lestari100% (1)
- Cardiac CycleDokument29 SeitenCardiac CycleRussell Suter100% (1)
- Cardiac Output and Hemodynamic MeasurementDokument29 SeitenCardiac Output and Hemodynamic Measurementdeepa100% (1)
- Physiology of The Cardiovascular System-CVSDokument56 SeitenPhysiology of The Cardiovascular System-CVSAmanuel MaruNoch keine Bewertungen
- Pacemaker Cells Generate HeartbeatsDokument16 SeitenPacemaker Cells Generate Heartbeatswaqas_xsNoch keine Bewertungen
- Lecture 6 Cardiovascular: Vascular System - The HemodynamicsDokument70 SeitenLecture 6 Cardiovascular: Vascular System - The HemodynamicsAndreea ŞtefănescuNoch keine Bewertungen
- Ecg Treadmill and Holter TestDokument77 SeitenEcg Treadmill and Holter TestRiteka Singh100% (1)
- Cardiac Pacing: Terms You Will Become Familiar With in This Section of TheDokument21 SeitenCardiac Pacing: Terms You Will Become Familiar With in This Section of TheClt Miskeen100% (1)
- Action PotentialsDokument3 SeitenAction Potentialsleng cuetoNoch keine Bewertungen
- Cardiac NotesDokument25 SeitenCardiac Noteslovelyc95Noch keine Bewertungen
- Ecg 111029102429 Phpapp01Dokument103 SeitenEcg 111029102429 Phpapp01Vickry WahidjiNoch keine Bewertungen
- Cardiovascular Pathology 1:: Blood VesselsDokument48 SeitenCardiovascular Pathology 1:: Blood VesselsRaiver CadenNoch keine Bewertungen
- OutputDokument12 SeitenOutputzenishzalamNoch keine Bewertungen
- Blood Vessel (Student)Dokument148 SeitenBlood Vessel (Student)Jerkin Razhed PostanesNoch keine Bewertungen
- Cardiac CatherizationDokument52 SeitenCardiac CatherizationJovan Varona NealaNoch keine Bewertungen
- Lesson 12 HeartDokument9 SeitenLesson 12 HeartEly FructuosoNoch keine Bewertungen
- Blood Flow: Right AtriumDokument2 SeitenBlood Flow: Right AtriumDaffodelle AnneNoch keine Bewertungen
- Cardiac Cycle: Mechanical Event and Their Electrical and Clinical CorrelationDokument28 SeitenCardiac Cycle: Mechanical Event and Their Electrical and Clinical Correlationhawas muhammed100% (1)
- QOch 11 Studyguide QODokument16 SeitenQOch 11 Studyguide QOHenry HoNoch keine Bewertungen
- Basics of Pacing CombinedDokument54 SeitenBasics of Pacing CombinedMichael Susanto100% (1)
- The History of Perfusion PumpsDokument28 SeitenThe History of Perfusion PumpsMiguel Angel CastroNoch keine Bewertungen
- Focal Atrial Tachycardia I: Clinical Features, DiagnosisDokument10 SeitenFocal Atrial Tachycardia I: Clinical Features, Diagnosisapi-26166949Noch keine Bewertungen
- Unit 1 Basics of Echocardiography and Cardiac DopplerDokument29 SeitenUnit 1 Basics of Echocardiography and Cardiac DopplerJack TomarNoch keine Bewertungen
- Anatomy and Physiology II Course OutcomesDokument50 SeitenAnatomy and Physiology II Course OutcomesShirley LourdesNoch keine Bewertungen
- Coronary Circulation: Dr. Syma RizwanDokument34 SeitenCoronary Circulation: Dr. Syma RizwanAttiqaQureshiNoch keine Bewertungen
- ECG Learning ModulesDokument150 SeitenECG Learning ModulesdodiNoch keine Bewertungen
- Anatomi Fisiology Sist - KV@DR - ZainiDokument46 SeitenAnatomi Fisiology Sist - KV@DR - ZainiDikdik Iskandar DwiyantoNoch keine Bewertungen
- Cardiovascular Physiology:: Circuitry, Hemodynamics, ElectrophysiologyDokument27 SeitenCardiovascular Physiology:: Circuitry, Hemodynamics, Electrophysiologyrsmoney3Noch keine Bewertungen
- Cardiovascular Nursing: Study Online atDokument7 SeitenCardiovascular Nursing: Study Online atLilly DayeNoch keine Bewertungen
- ... 4 Finals Cardiovascular PhysiologyDokument8 Seiten... 4 Finals Cardiovascular PhysiologyELIZABETH GRACE AMADORNoch keine Bewertungen
- ECG Fast and Easy chp12 PDFDokument40 SeitenECG Fast and Easy chp12 PDFkikyfauziaNoch keine Bewertungen
- JVP Guide: Assessing Jugular Venous Pulse Waves and PressureDokument53 SeitenJVP Guide: Assessing Jugular Venous Pulse Waves and PressureJoshua JayakaranNoch keine Bewertungen
- Basic ECG Interpretation GuideDokument61 SeitenBasic ECG Interpretation GuideHayat Hamzah DawiNoch keine Bewertungen
- AP Chapter 16BDokument35 SeitenAP Chapter 16BJay Patel100% (1)
- ANPH-M2-CU8. The HeartDokument20 SeitenANPH-M2-CU8. The HeartMary Grace MapulaNoch keine Bewertungen
- Cardiovascular Blood VesselsDokument12 SeitenCardiovascular Blood VesselswatuwaitingforNoch keine Bewertungen
- Heart SoundDokument15 SeitenHeart SoundLilian EdeniNoch keine Bewertungen
- Agents Used To Treat Hyperuricemia and GoutDokument19 SeitenAgents Used To Treat Hyperuricemia and GoutlouradelNoch keine Bewertungen
- EP - Lab NGR 6-15-2011Dokument51 SeitenEP - Lab NGR 6-15-2011louradelNoch keine Bewertungen
- Sample Teaching Strategies and Classroom Techniques That Address The Core CompetenciesDokument2 SeitenSample Teaching Strategies and Classroom Techniques That Address The Core CompetencieslouradelNoch keine Bewertungen
- Endocrine SystemDokument28 SeitenEndocrine SystemKarren Joy BuzonNoch keine Bewertungen
- Bsn-Essay Rubrics PDFDokument4 SeitenBsn-Essay Rubrics PDFlouradelNoch keine Bewertungen
- Cardiac TamponadeDokument3 SeitenCardiac TamponadeJenny Turado ArbitrarioNoch keine Bewertungen
- MedicalDokument51 SeitenMedicalravisikascNoch keine Bewertungen
- Cardiovascular AssessmentDokument108 SeitenCardiovascular AssessmentRaquel M. MendozaNoch keine Bewertungen
- Front PageDokument2 SeitenFront PagelouradelNoch keine Bewertungen
- 7.27.09 Burkhart TamponadeDokument26 Seiten7.27.09 Burkhart TamponadelouradelNoch keine Bewertungen
- Assessment and Management of Patients With Endocrine DisordersDokument78 SeitenAssessment and Management of Patients With Endocrine Disordershenny1620100% (1)
- Theories of LeadershipDokument161 SeitenTheories of Leadershiplouradel100% (6)
- Good PRSS 3Dokument64 SeitenGood PRSS 3louradelNoch keine Bewertungen
- Meningoccal DiseaseDokument25 SeitenMeningoccal DiseaselouradelNoch keine Bewertungen
- Good PRSDokument80 SeitenGood PRSlouradelNoch keine Bewertungen
- Responses To Altered Oxygenation, Cardiac and Tissue - Anatomy To AssessmentDokument254 SeitenResponses To Altered Oxygenation, Cardiac and Tissue - Anatomy To Assessmentlouradel100% (1)
- MentoringDokument45 SeitenMentoringlouradelNoch keine Bewertungen
- Certificate of Attendance: Pambansang Samahan NG Mga Nars NG PilipinasDokument1 SeiteCertificate of Attendance: Pambansang Samahan NG Mga Nars NG PilipinaslouradelNoch keine Bewertungen
- 2013 T L Symposium Rubrics Presentation PPT 12267Dokument31 Seiten2013 T L Symposium Rubrics Presentation PPT 12267louradelNoch keine Bewertungen
- Tacloban City: Remedios T. Romualdez Medical Foundation College of NursingDokument1 SeiteTacloban City: Remedios T. Romualdez Medical Foundation College of NursinglouradelNoch keine Bewertungen
- Testimonial Program: Cong. Ferdinand Martin G. Romualdez and TheDokument3 SeitenTestimonial Program: Cong. Ferdinand Martin G. Romualdez and ThelouradelNoch keine Bewertungen
- Rubric SDokument3 SeitenRubric SDiana Laura LeiNoch keine Bewertungen
- NCM 105 SyllabusDokument8 SeitenNCM 105 SyllabuslouradelNoch keine Bewertungen
- Psychiatric Case StudyDokument32 SeitenPsychiatric Case Studyrachael85% (33)
- NCM 103 Syllabus NeptunitesDokument28 SeitenNCM 103 Syllabus NeptuniteslouradelNoch keine Bewertungen
- NCM 105 Syllabus RevisedDokument8 SeitenNCM 105 Syllabus RevisedlouradelNoch keine Bewertungen
- Immunodeficiency Disease: Prepared By: 1 Susana P. Arellano, RN, MAN, MSNDokument282 SeitenImmunodeficiency Disease: Prepared By: 1 Susana P. Arellano, RN, MAN, MSNlouradelNoch keine Bewertungen
- Rubric - Nursing Clinical NURS 316Dokument5 SeitenRubric - Nursing Clinical NURS 316louradelNoch keine Bewertungen
- Accurate Relevant And/or Mostly Accurate Inaccurate And/or Irrelevant, But Inaccurate And/or IrrelevantDokument1 SeiteAccurate Relevant And/or Mostly Accurate Inaccurate And/or Irrelevant, But Inaccurate And/or IrrelevantlouradelNoch keine Bewertungen
- Crisis & Anxiety DisordersDokument164 SeitenCrisis & Anxiety DisorderslouradelNoch keine Bewertungen
- Autopsy of Heart External ExaminationDokument20 SeitenAutopsy of Heart External ExaminationchinnnababuNoch keine Bewertungen
- Verb classes and types in English and UkrainianDokument16 SeitenVerb classes and types in English and UkrainianАнастасия ДобровольскаяNoch keine Bewertungen
- Movers Vocabulary Worksheet PDFDokument5 SeitenMovers Vocabulary Worksheet PDFSteve Haag100% (1)
- SCOUTINGDokument45 SeitenSCOUTINGmohitgadde89% (9)
- Inactivation of Viruses: June 2011Dokument13 SeitenInactivation of Viruses: June 2011Iqbal Muhammad Yaa-BegitulahNoch keine Bewertungen
- Madam PuddifootsDokument9 SeitenMadam Puddifootserica milaNoch keine Bewertungen
- Bbo Round One Final 2009Dokument30 SeitenBbo Round One Final 2009martynapet100% (2)
- Ut1fl"': (Artleulatory Phonetics)Dokument18 SeitenUt1fl"': (Artleulatory Phonetics)visvabharatiNoch keine Bewertungen
- JMC 2001 Ans HWrittenDokument11 SeitenJMC 2001 Ans HWrittenaditya.padi4Noch keine Bewertungen
- Baptist Health System Will Build New Hospital in BoerneDokument12 SeitenBaptist Health System Will Build New Hospital in BoerneBrittany LudwigNoch keine Bewertungen
- English Exercise Book 3 Eso A: Ies Canónigo ManchónDokument36 SeitenEnglish Exercise Book 3 Eso A: Ies Canónigo ManchónrobertoquinteiroNoch keine Bewertungen
- Read The Silent Alpha Chapter 37Dokument1 SeiteRead The Silent Alpha Chapter 37mykaorimiyazonoNoch keine Bewertungen
- Proposed Ordinance Creating An Anti Stray Dogs Task ForceDokument3 SeitenProposed Ordinance Creating An Anti Stray Dogs Task ForceKit BagaipoNoch keine Bewertungen
- Elephant Report & Recount TextDokument4 SeitenElephant Report & Recount TextAq N DiaNoch keine Bewertungen
- Hannah ReevesDokument2 SeitenHannah Reevesapi-242939734Noch keine Bewertungen
- Science Process Skills: Observe Classify Measure Infer Predict Credits Extensions About The AuthorDokument21 SeitenScience Process Skills: Observe Classify Measure Infer Predict Credits Extensions About The AuthorSharmaine TuazonNoch keine Bewertungen
- Identifying Venomous and Nonvenomous Snakes in TexasDokument10 SeitenIdentifying Venomous and Nonvenomous Snakes in TexasAttila KissNoch keine Bewertungen
- Readers For Teens Summer at The Zoo Sample PDFDokument8 SeitenReaders For Teens Summer at The Zoo Sample PDFPanambí Morales100% (3)
- KIB Common Myth ConceptionsDokument4 SeitenKIB Common Myth Conceptionscila111Noch keine Bewertungen
- Talking Turkey Final ReportDokument29 SeitenTalking Turkey Final ReportDavid CarrNoch keine Bewertungen
- Ivan Petrovic PavlovDokument3 SeitenIvan Petrovic PavlovNazreen Ayein Shukor100% (1)
- Respiratory SystemDokument36 SeitenRespiratory Systemسارة عبد الكاظم مكطوفNoch keine Bewertungen
- Neutrophil Function From Mechanism To DiseaseDokument33 SeitenNeutrophil Function From Mechanism To DiseaseMajoo HernándezNoch keine Bewertungen
- Phil-IRI New Passages LVL2 EnglishDokument4 SeitenPhil-IRI New Passages LVL2 EnglishAzul SabaytonNoch keine Bewertungen
- 1 Sex DeterminationDokument30 Seiten1 Sex DeterminationNeru Singh100% (1)
- The Mischievous Sparky Learns the Value of True FriendshipDokument15 SeitenThe Mischievous Sparky Learns the Value of True Friendshipankit chakrabortyNoch keine Bewertungen
- Present Simple Tense and To Be Verb Practice ExercisesDokument2 SeitenPresent Simple Tense and To Be Verb Practice ExercisesPontevedro English CentreNoch keine Bewertungen
- The Jungle Book - The Cobra 39 S Egg Watts Michael 2013Dokument36 SeitenThe Jungle Book - The Cobra 39 S Egg Watts Michael 2013mamermNoch keine Bewertungen
- English Turkish Grammar Functional and Transformational BookDokument407 SeitenEnglish Turkish Grammar Functional and Transformational BookYuksel Goknel100% (1)
- Jump To Navigationjump To Search: Kermode BearDokument4 SeitenJump To Navigationjump To Search: Kermode Bearswahyudi9Noch keine Bewertungen