Beruflich Dokumente
Kultur Dokumente
Lapjag Bangsal IPD 22 OKTOBER DHF
Hochgeladen von
Leony Nerry SabatiniCopyright
Verfügbare Formate
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenCopyright:
Verfügbare Formate
Lapjag Bangsal IPD 22 OKTOBER DHF
Hochgeladen von
Leony Nerry SabatiniCopyright:
Verfügbare Formate
GP ON DU T Y : DR .
T I K A
R E S I DE NT ON DU T Y : DR . E VI R OS S A
CO- A S S ON DU T Y :
L E ONY NE R R Y S . T A MB U NAN
R A DE N A NNI S A CI T R A P E R MADI
DUTY REPORT WARD UNIT
22
ND
OCTOBER , 2014
PATIENTS RECAP
3
rd
floor
Nasopharingeal Carcinoma
4
th
floor
POST SYNCOPE
IBD
Anemia, with susp. Pneumonia
SIDA
6
th
floor
DHF
PATIENTS IDENTITY
Name : Mr. J
DOB : 17 Feb 1989
Age : 25 y.o
Gender : Male
Occupation : Unemployed
Address : Manggarai Jakbar
Medical Record no. : 225164
Date of admission : 22
nd
October , 2014 at 01.00
WIB
ANAMNESIS
Chief Complain:
Fever since 4 days before admission
History of present illness:
Patient came with fever since 4 days before admission.
FEVER
all day
Relieved by paracetamol on day 2 but not to the baseline
temperature
No fever prior to admission (day 4)
Associated with diarrhea, 7 times a day on the 4
th
day > the
stool is watery, no blood, no mucus, no pus, no waste, not oily
nor smelly with yellow brownish color.
Nausea and Vomiting (+), 3 times a day, food containing vomit
Autoanamnesa at 01.00 WIB on 22
nd
October 2014
Patient denied
any bleeding from gum, nose, bloody stool or urine
Headache
Pain in the back of the eyes
Rash
Abdominal pain
Muscle ache
This is the first time patient experiences these
complaints.
History of past illness:
Denies any history of hypertension, DM, heart problems, stroke,
asthma, hepatitis, and allergies.
Family History:
No known family member or relatives have the same
complaints
History of Socio-habits:
Smoking 1 pack/day since 3yr before admission
No history of drinking alcohol
No one in the relatives or family or collegue have the same
complaints
History of medications:
Paracetamol 3 x 500 mg for 3 days
PHYSICIAL EXAMINATION
GENERAL EXAMINATION
General condition :
Consciousness : compos mentis
Blood pressure : 120/80 mmHg
HR : 88x/min, regular, full
RR : 18x/min, thoracoabdomino, kussmaul (-)
Body temperature : 34 C
Body Weight : 96 kg
Body Height : 170 cm
IMT : 33,2 (obese)
PHYSICIAL EXAMINATION
PHYSICAL EXAMINATION
Head: normocephal
Hair: normal distribution, black color
Face: symmetrical, deformity (-)
Eye: pale conjunctiva -/-, icteric conjunctiva -/-, -
ENT: normotia, normosepta, rhinorrhea (-), otorrhea (-), blood(-),
hyperemic pharynx (-), calm T1-T1
Mouth: mucous is normal
Neck: Lymphadenopathy (-)
Skin: warm, pale (-)
PHYSICIAL EXAMINATION
PHYSICAL EXAMINATION
Thorax
Pulmonary Examination
Inspection : normochest, symmetrical chest movement on static
and dynamic. ICS retraction (-), no rash
Palpation : symmetrical chest expansion and tactile fremitus, (-)
mass, (-) tenderness
Percussion : sonor at both lung field
Auscultation : bronchovesicular +/+, rhonchi -/-, wheezing -/-
PHYSICIAL EXAMINATION
PHYSICAL EXAMINATION
Thorax
Cardiac Examination
Inspection : invisible ictus cordis
Palpation : impalpable ictus cordis
Percussion
Right heart border : Right parasternal line
Left heart border : Left midclavicular line
Heart waist : ICS III left parasternal line
Auscultation : S1/S2 regular, gallop (-), murmur (-)
PHYSICIAL EXAMINATION
PHYSICAL EXAMINATION
Abdominal examination
Inspection : not distended, mass(-)
Auscultation : normal bowel sound ; 8x/min
Palpation : tenderness and rebound tenderness alll over
regio (-),hepatomegaly and splenomegaly (-)
Percussion : timpani
Special examination : shifting dullness (-), fluid wave (-)
Rumple Leed : +
Extremities: warm skin, pale (-) CRT <2 sec , rash (-)
RUMPLE LEED
RUMPLE LEED
WORK UP
Jenis Pemeriksaan Saat Ini Nilai Rujukan
HEMATOLOGY
Hemoglobin 20.5* 13-18 mg/dL
Hematocrit 58* 40-52%
Leukocyte 5700 4800 10800 /uL
Trombocyte 80.000* 150000 400000 /uL
Jenis Pemeriksaan Nilai Saat Ini Nilai Rujukan
IMMUNOSEROLOGY
Salmonella Thypii O 1/80 negative
Salmonella Para
Thypii AO
negative negative
Salmonella Para
Thypii BO
negative
negative
Salmonella Para
Thypii CO
negative
negative
l
Salmonella Thypii H 1/80 negative
Salmonella Para
Thyoii AH
negative
negative
Salmonella Para
Thypii BH
negative
negative
Salmonella Para
Thypii CH
1/160 negative
RESUME
Male, 25 y.o, came with fever since 4 days
before admission, with no rash, any
bleeding from gum, nose, bloody stool or
urine, headache , retroorbital pain, rash,
abdominal pain, myalgia, shortness of
breath. On physical examination, vital signs
are normal, percussion on both lung fields
are sonor, there is no sign of peural
efussioin nor asictes and the positive
rumple leed test. On the work up lab,
patient has hemoconcentration and
trombocytopenia.
LIST OF PROBLEMS
1. Acute Fever
2. Nausea and vomiting
3. Diarrhea
4. Obese
5. Hemoconcentration
6. Thrombocytopenia
DIAGNOSIS
Working diagnosis
Dengue Hemorrhagic Fever gr I
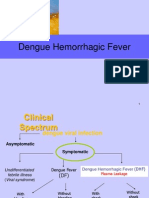
DENGUE HEMORRHAGIC FEVER
Complete 4 of the following criteria :
Fever or history of fever lasting 27 days, occasionally biphasic
A haemorrhagic tendency shown by at least one of the
following: a positive tourniquet test*; petechiae, ecchymoses
or purpura; bleeding from the mucosa, gastro-intestinal tract,
injection sites or other locations; haematemesis or melaena
Thrombocytopenia [(100,000 cells/mm3 (1006109/L)]{
Evidence of plasma leakage due to increased vascular
permeability shown by: an increase in the haematocrit >20%
above average for age, sex and population; a decrease in
the haematocrit after intervention >20% of baseline; signs of
plasma leakage such as pleural effusion, ascites or
hypoproteinaemia
PLANNING
DIAGNOSTIC PLAN MANAGEMENT PLAN
CBC Non Pharmacology :
- Bed rest
- Soft Dietary
- Urine catheter placement
Serology Test (IgM, IgG) Pharmacology :
- Fluid Therapy RL
NS-1 Antigen - Ondancentron 3 x 4 mg IV
SGOT/SGPT - Paracetamol 3 x 500 mg PO
Radiology > X-ray Thorax AP,
Lateral Decubitus
FLUID REPLACEMENT
LOADING DOSE
5-7 ml/kg/hr 1-2 hr
500 cc in 1-2hr
3-5 ml/kg/hr in 2-4 hr
300 cc in 2-4hr
2-3 ml/kg/hr or less according to
clinical response
200 cc/hr
Monitor VS (4 hourly
urine output(4-6hrly)
Hct(before & after fluid
replacement then 6-12hrly)
BG
MAINTANANCE
1500 + 20 (BB-20)
1500 + 20 (96-20)
3020 ml/24 hr
PROGNOSIS
Quo ad Vitam: bonam
Quo ad functionam: bonam
Quo ad sanactionam: bonam
REFERENCES
DENGUE
EPIDEMIOLOGY
Most important arthropod-borne viral diseases in
terms of human morbidity and mortality.
Important public health problem.
Tropical & subtropical regions around the world
urban and semi urban areas
VIROLOGY
Dengue virus
mosquito-borne flavivirus.
Transmitted by
Aedes aegypti
Aedes albopictus.
DEN-1, 2, 3 and 4.
VIROLOGY
Each episode of infection
a life-long protective immunity to the homologous serotype
partial & transient protection against subsequent infection
by the other three serotypes.
Secondary infection is a DHF major risk factor
VIROLOGY
Other important contributing factors for DHF are
viral virulence
host genetic background
T-cell activation
viral load
auto-antibodies
SPECTRUM OF INFECTION
The incubation period is 4-7 days (range 3-14)
Asymptomatic a spectrum of illness
Undifferentiated mild febrile illness severe disease
(plasma leakage (-/+_) & organ impairment
Systemic & dynamic disease with
Clinical
Haematological
Serological
profiles changing from day to day.
PATHOPHYSIOLOGY
Increased vascular permeability is the primary
pathophysiological abnormality in DHF/ DSS.
Increased vascular permeability leads to plasma
leakage and results in hypovolaemia/ shock.
PATHOPHYSIOLOGY
The pathogenetic mechanism for the increased
vascular permeability (?)
Destructive vascular lesions (-)
post-mortem (microscopically),
perivascular oedema
loss of integrity of endothelial junctions
endothelial dysfunction
AbN immune response
production of cytokines or chemokines,
activation of T-lymphocytes
disturbances of haemostatic system
C3a, C5a, TNF-, IL-2, 6 & 10, IFN-, histamine
TOURNIQUET TEST
In DHF grade 1 (+) tourniquet test serves as the
only indicator of haemorrhagic tendency.
Sensitivity 0% to 57% (phase of illness)
5-21% false positive
How to perform tourniquet test
Inflate the blood pressure cuff on the upper arm to
a point midway between the systolic and diastolic
pressures for 5 minutes.
A positive test is when 20 or more petechiae per
2.5 cm (1 inch) square are observed.
The 1997 WHO classification of dengue virus infection.
DF
Probable
An acute febrile illness with two or more of the
following manifestations: headache, retro-orbital
pain, myalgia, arthralgia, rash, haemorrhagic
manifestations and leucopenia
And
Supportive serology (a reciprocal
haemagglutination-inhibition antibody titre >1280, a
comparable IgG enzyme-linked immunosorbent
assay (ELISA, see chapter 455) titre or a positive IgM
antibody test on a late acute or convalescent-phase
serum specimen)
Or
Occurrence at the same location and time as other
DF cases
Confirmed
A case confirmed by one of the following laboratory
criteria:
Isolation of the dengue virus from serum/autopsy samples
At least a four-fold change in reciprocal IgG/IgM titres to one
or more dengue virus antigens in paired samples
Demonstration of dengue virus antigen in autopsy tissue, serum
or cerebrospinal fluid samples by immunohistochemistry,
immunofluorescence or ELISA
Detection of dengue virus genomic sequences in autopsy
tissue serum or cerebrospinal fluid samples by polymerase
chain reaction (PCR)
Reportable
Any probable or confirmed case should be reported
DHF
For a diagnosis of DHF, a case must meet all four of the
following criteria:
Fever or history of fever lasting 27 days, occasionally
biphasic
A haemorrhagic tendency shown by at least one of the
following: a positive tourniquet test*; petechiae,
ecchymoses or purpura; bleeding from the mucosa,
gastro-intestinal tract, injection sites or other locations;
haematemesis or melaena
Thrombocytopenia [(100,000 cells/mm3 (1006109/L)]{
Evidence of plasma leakage due to increased vascular
permeability shown by: an increase in the haematocrit
>20% above average for age, sex and population; a
decrease in the haematocrit after intervention >20% of
baseline; signs of plasma leakage such as pleural
effusion, ascites or hypoproteinaemia
DSS
For a case of DSS, all four criteria for DHF must be
met, in addition to evidence of circulatory failure
manifested by:
Rapid and weak pulse
And
Narrow pulse pressure (,20 mmHg or 2.7 kPa)
or manifested by
Hypotension for age
And
Cold, clammy skin and restlessness
World Health Organization. Dengue
Guidelines for Diagnosis, Treatment,
Prevention and Control
New Edition 2009. WHO: Geneva; 2009
The following manifestations are important in
dengue infection but are often under- recognised
or misdiagnosed
Acute abdomen :
Hepatitis and liver failure :
Neurological manifestation :
Haemophagocytic syndrome
DISEASE MONITORING LABORATORY
TESTS
Full Blood Count (FBC)
1. White cell count (WCC) :
2. Haematocrit (HCT) :
3. Thrombocytopaenia :
Liver Function Test
DIAGNOSTIC TESTS
DENGUE SEROLOGY TESTS
Haemagglutination Inhibition Test
Dengue IgM test
Indirect IgG ELISA test
Cross-react with:
other flavivirus Japanese Encephalitis
non-flavivirus malaria, leptospirosis, toxoplasmosis, syphilis
connective tissue diseases rheumatoid arthritis
VIRUS ISOLATION
POLYMERASE CHAIN REACTION (PCR)
NON-STRUCTURAL PROTEIN-1 (NS1 Antigen)
Clinical and Laboratory Criteria for Patients Who Can be Treated at
Home
The following should be taken into consideration
before discharging a patient.
Afebrile for 48 hours
Improved general condition
Improved appetite
Stable haematocrit
Rising platelet count
No dyspnoea or respiratory distress from pleural effusion
or ascites
Resolved bleeding episodes
Resolution/recovery of organ dysfunction
THANK YOU
Das könnte Ihnen auch gefallen
- Case Report Typhoid Fever (A01.0)Dokument32 SeitenCase Report Typhoid Fever (A01.0)Alvin PratamaNoch keine Bewertungen
- Sample Case Presentation - Occult BacteremiaDokument51 SeitenSample Case Presentation - Occult BacteremiaPrecious Gutierrez BagazinNoch keine Bewertungen
- Case Report Typhoid Fever (A01.0)Dokument32 SeitenCase Report Typhoid Fever (A01.0)Alvin PratamaNoch keine Bewertungen
- LAPKAS-Elsa Nur Rahma Diahnissa-2016730030-1Dokument34 SeitenLAPKAS-Elsa Nur Rahma Diahnissa-2016730030-1Raka WibisonoNoch keine Bewertungen
- TYPHOID FEVER Morport InternaDokument17 SeitenTYPHOID FEVER Morport InternapoonpatchaNoch keine Bewertungen
- DUTY REPORT Igd Ecy AbeDokument21 SeitenDUTY REPORT Igd Ecy AbeAsiah AbdillahNoch keine Bewertungen
- Pleurak EffusionDokument16 SeitenPleurak EffusionElfriska SihombingNoch keine Bewertungen
- Acute Rheumatic FeverDokument37 SeitenAcute Rheumatic FeverQadriyah Ramadhani100% (1)
- Duty Report Er 23 07 2015Dokument25 SeitenDuty Report Er 23 07 2015Auditya WidyasariNoch keine Bewertungen
- Hema Case 2Dokument55 SeitenHema Case 2jlcocm-2022-00028Noch keine Bewertungen
- CKDDokument48 SeitenCKDJuniorNoch keine Bewertungen
- Duty Report On Ward 24-06-15Dokument25 SeitenDuty Report On Ward 24-06-15Annisa Rizki Ratih PratiwiNoch keine Bewertungen
- CMD DBDDokument11 SeitenCMD DBDAnnisa Aulia AnandaNoch keine Bewertungen
- IM Case ReportDokument5 SeitenIM Case ReportGurungSurajNoch keine Bewertungen
- DengueDokument38 SeitenDengueadetiquezNoch keine Bewertungen
- Lascano, Joanne Alyssa - RheumatologyDokument13 SeitenLascano, Joanne Alyssa - RheumatologyJoanne Alyssa Hernandez LascanoNoch keine Bewertungen
- Community Acquired PneumoniaDokument56 SeitenCommunity Acquired Pneumoniashiean06Noch keine Bewertungen
- Ward Duty Report 12-2-14 (English)Dokument25 SeitenWard Duty Report 12-2-14 (English)gilnifNoch keine Bewertungen
- LAPJAG DR RidwanDokument13 SeitenLAPJAG DR RidwanElsy Pramitha SariNoch keine Bewertungen
- Infectious Disease ReviewDokument12 SeitenInfectious Disease ReviewjyothiNoch keine Bewertungen
- DF Case ReportDokument26 SeitenDF Case ReportMuhamad IrsyadNoch keine Bewertungen
- Duty Report 01 MARCH, 2015: GP On Duty: Dr. Ruben Coass On Duty: Aris ZikrilDokument24 SeitenDuty Report 01 MARCH, 2015: GP On Duty: Dr. Ruben Coass On Duty: Aris ZikrilKarina Pratiwi SoetomoNoch keine Bewertungen
- Lapsus Cardio v3Dokument31 SeitenLapsus Cardio v3Nurfitrianti ArfahNoch keine Bewertungen
- Dengue Case Management Card 125085 12x6 Zcard DengueDokument2 SeitenDengue Case Management Card 125085 12x6 Zcard DenguejmbobitNoch keine Bewertungen
- Morning Report Friday, Aug 11 2018Dokument51 SeitenMorning Report Friday, Aug 11 2018Efan StiawanNoch keine Bewertungen
- Dengue: West Visayas State University-Medical Center Department of PediatricsDokument89 SeitenDengue: West Visayas State University-Medical Center Department of PediatricsVanessa YunqueNoch keine Bewertungen
- DENGUE Janice LouieDokument38 SeitenDENGUE Janice LouieclikgoNoch keine Bewertungen
- Copy-A CASE OF ALTERED SENSORIUM - ALOKDokument37 SeitenCopy-A CASE OF ALTERED SENSORIUM - ALOKAlok MohanNoch keine Bewertungen
- Dengue Hemorrhagic FeverDokument27 SeitenDengue Hemorrhagic FeverTristiana DewiNoch keine Bewertungen
- Pericardial EffusionDokument35 SeitenPericardial EffusionRizky Amalia WakanoNoch keine Bewertungen
- Acute Nephrotic SyndromeDokument10 SeitenAcute Nephrotic SyndromeEvi SilviaNoch keine Bewertungen
- Dengu Syndrome & Its Managment - Prof. Kaka1Dokument39 SeitenDengu Syndrome & Its Managment - Prof. Kaka1Aditi SahaNoch keine Bewertungen
- Reumato and EndocrineDokument106 SeitenReumato and Endocrinehasanatiya41Noch keine Bewertungen
- Fever of Unknown Origin (FUO)Dokument55 SeitenFever of Unknown Origin (FUO)mohamed hanyNoch keine Bewertungen
- Intraoperatively Inadequate BlockMORBIDITY ProtocolDokument9 SeitenIntraoperatively Inadequate BlockMORBIDITY Protocoldocv526Noch keine Bewertungen
- Yuniarti, CHF, Krisis Tiroid, CAP Duty HannaDokument17 SeitenYuniarti, CHF, Krisis Tiroid, CAP Duty HannaHanna GustinNoch keine Bewertungen
- Grand ReportsDokument60 SeitenGrand ReportsfilchibuffNoch keine Bewertungen
- Case ConfrenceDokument48 SeitenCase ConfrenceantogantengbangetzNoch keine Bewertungen
- Group 2 - Case Child With Severe Measles Pneumonia - DDokument20 SeitenGroup 2 - Case Child With Severe Measles Pneumonia - Dazzahra zahidaNoch keine Bewertungen
- Case Conference Monday Night Shift, March 16 2019Dokument42 SeitenCase Conference Monday Night Shift, March 16 2019delfiaNoch keine Bewertungen
- Differential Diagnosispage of ValidationDokument38 SeitenDifferential Diagnosispage of ValidationiinmsNoch keine Bewertungen
- Polymyalgia RheumaticaDokument23 SeitenPolymyalgia RheumaticaGabriella TungadiNoch keine Bewertungen
- Duty Report: Wednesday, June 14 2017Dokument29 SeitenDuty Report: Wednesday, June 14 2017Qonita Aizati QomaruddinNoch keine Bewertungen
- Care of Clients With Problems in OxygenationDokument282 SeitenCare of Clients With Problems in OxygenationAYTONA, JAMAICA F.Noch keine Bewertungen
- Duty - MahyunarDokument13 SeitenDuty - Mahyunarelsy pramithaNoch keine Bewertungen
- Clinical Diagnosis of Dengue Infection in Primary Care: Agung NugrohoDokument26 SeitenClinical Diagnosis of Dengue Infection in Primary Care: Agung NugrohotaniarafraNoch keine Bewertungen
- Accident and Emergency Posting Case Write UpDokument8 SeitenAccident and Emergency Posting Case Write UpAmbhi Gana0% (1)
- Dengue: Clinical Manifestations and Laboratory Diagnosis DR Malobika BhattacharyaDokument31 SeitenDengue: Clinical Manifestations and Laboratory Diagnosis DR Malobika BhattacharyaSundeep KaushikNoch keine Bewertungen
- Case Presentation BronchiectasisDokument61 SeitenCase Presentation BronchiectasisUzair Muhd100% (6)
- Duty Report 27 AUGUST 2014: GP On Duty: Dr. Ananita Resident On Duty: Dr. Ardhestiro Co-Ass On Duty: Alvin & TedyDokument22 SeitenDuty Report 27 AUGUST 2014: GP On Duty: Dr. Ananita Resident On Duty: Dr. Ardhestiro Co-Ass On Duty: Alvin & TedyAlvin BernardNoch keine Bewertungen
- Case Presentation and Discussion On Dengue: Bedside Rounds OutputDokument5 SeitenCase Presentation and Discussion On Dengue: Bedside Rounds OutputCalingalan Hussin CaluangNoch keine Bewertungen
- Case Conference Thursday Night Shift, September 4 2018Dokument47 SeitenCase Conference Thursday Night Shift, September 4 2018Aisya FikritamaNoch keine Bewertungen
- (29 August, 2016) Department of General Medicine PIMS IslamabadDokument43 Seiten(29 August, 2016) Department of General Medicine PIMS IslamabadwaseemNoch keine Bewertungen
- Duty Report: Co-Assistant On Duty: Fadhila Ayu Safirina Succi Islami PutriDokument29 SeitenDuty Report: Co-Assistant On Duty: Fadhila Ayu Safirina Succi Islami PutriDhila SafirinaNoch keine Bewertungen
- Myelodisplastic SyndromeDokument29 SeitenMyelodisplastic SyndromeTiara RahmawatiNoch keine Bewertungen
- Lupus Case PresentationDokument48 SeitenLupus Case PresentationRoscelie KhoNoch keine Bewertungen
- Nyeri DadaDokument27 SeitenNyeri DadaAji Setia UtamaNoch keine Bewertungen
- Case On Odematous 80Dokument46 SeitenCase On Odematous 80Ginger SodarNoch keine Bewertungen
- Anatomy Physiology Visual System April 2013Dokument54 SeitenAnatomy Physiology Visual System April 2013Leony Nerry SabatiniNoch keine Bewertungen
- Guidelines TBC TerbaruDokument160 SeitenGuidelines TBC TerbaruSutoto MoeljadiNoch keine Bewertungen
- Guidelines AHF ES 2005Dokument33 SeitenGuidelines AHF ES 2005Leony Nerry SabatiniNoch keine Bewertungen
- Lecture Tropmed 2013 DHF NataDokument40 SeitenLecture Tropmed 2013 DHF NataLeony Nerry SabatiniNoch keine Bewertungen
- PETA Vegan Baking SubstitutionsDokument1 SeitePETA Vegan Baking SubstitutionsJane KimNoch keine Bewertungen
- Ann Oncol 2012 Chan Vii83 5Dokument3 SeitenAnn Oncol 2012 Chan Vii83 5Fibrianti SeputriNoch keine Bewertungen
- Chemical Carcinogenesis and Nasopharyngeal Carcinoma: Faqing Tang, Xiaowei Tang, Daofa Tian and Ya CaoDokument23 SeitenChemical Carcinogenesis and Nasopharyngeal Carcinoma: Faqing Tang, Xiaowei Tang, Daofa Tian and Ya CaoLeony Nerry SabatiniNoch keine Bewertungen
- Etiologi KNFDokument4 SeitenEtiologi KNFLeony Nerry SabatiniNoch keine Bewertungen
- JOURNAL OM Preventive and Management - OpenaccessDokument10 SeitenJOURNAL OM Preventive and Management - OpenaccessLeony Nerry SabatiniNoch keine Bewertungen
- Cerebrovascular Abnormality LNKDokument19 SeitenCerebrovascular Abnormality LNKLeony Nerry SabatiniNoch keine Bewertungen
- Ec/irbDokument28 SeitenEc/irbRachana ShettyNoch keine Bewertungen
- Dagmawi Alemu D.p.proposalDokument13 SeitenDagmawi Alemu D.p.proposalYe Geter Lig NegnNoch keine Bewertungen
- Makalah Bahasa InggrisDokument7 SeitenMakalah Bahasa InggrisRima Novianti100% (1)
- Facial PalsyDokument7 SeitenFacial PalsyPedro FonsecaNoch keine Bewertungen
- Case Study On AnaemiaDokument16 SeitenCase Study On AnaemiaLavie Gangwar100% (1)
- CholesteatomaDokument29 SeitenCholesteatomawhitelotusoo7Noch keine Bewertungen
- Case Study Part 2 Patient With Uti (Bag-O)Dokument48 SeitenCase Study Part 2 Patient With Uti (Bag-O)Eaht Quirong0% (1)
- Anti-Cancer Drugs : DR Dale Srinivas University of GuyanaDokument79 SeitenAnti-Cancer Drugs : DR Dale Srinivas University of Guyanamasterpiece101Noch keine Bewertungen
- 62 Lecture Menstrual Cycle Abnormalities, Infertility, MenopauseDokument69 Seiten62 Lecture Menstrual Cycle Abnormalities, Infertility, MenopauseTarek TarekNoch keine Bewertungen
- Zoheir Aissaoui Rals03 10016 1Dokument5 SeitenZoheir Aissaoui Rals03 10016 1babelfirdaousNoch keine Bewertungen
- Case Presentation IM DDHDokument12 SeitenCase Presentation IM DDHAishwarya BharathNoch keine Bewertungen
- Sample Subspecialty Census FormatDokument3 SeitenSample Subspecialty Census FormatMon FabileNoch keine Bewertungen
- Physical Assessment of Preeclamptic PatientDokument3 SeitenPhysical Assessment of Preeclamptic PatientAndreiNoch keine Bewertungen
- PDF&Rendition 1Dokument6 SeitenPDF&Rendition 1Budong BernalNoch keine Bewertungen
- Calcarea PhosphoricaDokument12 SeitenCalcarea PhosphoricaAnaSkopje100% (1)
- A Case Study On Diabetes MellitusDokument26 SeitenA Case Study On Diabetes MellitusLida100% (3)
- Assessment: Facial ShavingDokument2 SeitenAssessment: Facial ShavingA CNoch keine Bewertungen
- Cholangitis and Cholecystitis (DR - Dr. Hery Djagat Purnomo, SpPD-KGEH)Dokument47 SeitenCholangitis and Cholecystitis (DR - Dr. Hery Djagat Purnomo, SpPD-KGEH)Aditya SahidNoch keine Bewertungen
- Assissting FNAB in The Liver Liver Biopsy Checklist FinalDokument10 SeitenAssissting FNAB in The Liver Liver Biopsy Checklist FinalCamille T. SanchezNoch keine Bewertungen
- Rehabilitation After Plate Fixation of Upper and Lower Extremity FracturesDokument6 SeitenRehabilitation After Plate Fixation of Upper and Lower Extremity FractureswirasenaNoch keine Bewertungen
- Urinary InfectionDokument33 SeitenUrinary InfectionNithish SNoch keine Bewertungen
- Chapter 15 - Dental CariesDokument23 SeitenChapter 15 - Dental CariesShoyo HinataNoch keine Bewertungen
- 2.1 Market Analysis of Non-Needle Injector in IndonesiaDokument5 Seiten2.1 Market Analysis of Non-Needle Injector in IndonesiaPROFESSOR HUDANoch keine Bewertungen
- Final Announcement REV 5 200523Dokument24 SeitenFinal Announcement REV 5 200523AgilSugiaNoch keine Bewertungen
- WHO Surgical Safety Checklist: Before Induction On AnesthesiaDokument1 SeiteWHO Surgical Safety Checklist: Before Induction On AnesthesiaDienizs LabiniNoch keine Bewertungen
- Tumor Pituitari: Pembimbing: Ervita Yuda, DR., SPPD, M.Kes Davin Takaryanto, DRDokument34 SeitenTumor Pituitari: Pembimbing: Ervita Yuda, DR., SPPD, M.Kes Davin Takaryanto, DRDavin TakaryantoNoch keine Bewertungen
- Pituitary Disorders (Final Draft)Dokument17 SeitenPituitary Disorders (Final Draft)Kiprono Keitany TimothyNoch keine Bewertungen
- Informed Consent Form For Research StudyDokument11 SeitenInformed Consent Form For Research Studyrn.kathavateNoch keine Bewertungen
- General Surgery v1.0Dokument59 SeitenGeneral Surgery v1.0SamiaNazNoch keine Bewertungen
- Autoimmune Abnormalities of Postpartum Thyroid DiseasesDokument8 SeitenAutoimmune Abnormalities of Postpartum Thyroid DiseasesIpan MahendriyansaNoch keine Bewertungen