Beruflich Dokumente
Kultur Dokumente
Hemostasis
Hochgeladen von
Qurrataini Ibanez0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
39 Ansichten40 SeitenBy Prof Sameh Shamaa
Medical Oncology and Internal medicine
Mansoura Faculty Of Medicine
Copyright
© © All Rights Reserved
Verfügbare Formate
PPT, PDF, TXT oder online auf Scribd lesen
Dieses Dokument teilen
Dokument teilen oder einbetten
Stufen Sie dieses Dokument als nützlich ein?
Sind diese Inhalte unangemessen?
Dieses Dokument meldenBy Prof Sameh Shamaa
Medical Oncology and Internal medicine
Mansoura Faculty Of Medicine
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
0 Bewertungen0% fanden dieses Dokument nützlich (0 Abstimmungen)
39 Ansichten40 SeitenHemostasis
Hochgeladen von
Qurrataini IbanezBy Prof Sameh Shamaa
Medical Oncology and Internal medicine
Mansoura Faculty Of Medicine
Copyright:
© All Rights Reserved
Verfügbare Formate
Als PPT, PDF, TXT herunterladen oder online auf Scribd lesen
Sie sind auf Seite 1von 40
HEMOSTASIS
By Prof\ Sameh Shamaa
Prof Of medical Oncology and
Internal medicine
Mansoura Faculty Of Medicine
HEMOSTASIS
HEMOSTASIS
Def:- stoppage of bleeding from the blood
vessels
Mechanisms
(I) v.c of blood vessels
(II) platelet plug formation
(III) Blood coagulation (fibrinogen fibrin)
(IV) Clot retraction
(V) fibrinolysis to dissolve the clot
HEMOSTASIS
PRIMARY HEMOSTASIS
includes the processes that result in the
formation of the platelet plug.
Necessary factors-:
-The blood vessels : the vessel walls esp. the
subendothelial layer.
- The platelets
- 2 plasma glycoproteins:
- fibrinogen
-Willebrand factor ,which
also presents inside the platelets
Mechanisms:
1-v.c of the bl. vessel.
2- Platelets adhesion to subendothelial layer, ( Willebrand
factor is necessary for this stage)
adhesion of platelets- 3- platelets secretion:
their activation and secretion of ADP,adrenaline,
noradrenaline > aggregation & activation of other
platelets.
4- Aggregation of platelets.
5- Formation of capillary plug.
HEMOSTASIS
Exploration of the 1ry homeostasis
1) Important points in the history
of any bleeding patients :
HEMOSTASIS
- Family history
- Duration (recent onset or since childhood)
- Duration of the bleeding episode.
- Circumstance of bleeding
(spontaneous, after trauma, or surgery)
HEMOSTASIS
Type and character of bleeding:
-
- Purpuric spots
(capillary or platelets defect not characteristic of
hemophilia)
- Hematoma, hemarthrosis or large ecchymoses at
the site of trauma :
suggests hemophilia (coagulation defect)
- Sudden severe bleeding from multiple sites after
prolonged surgery or during obstetric procedures
suggests acquired fibrinogen defect
HEMOSTASIS
2) Investigations :
HEMOSTASIS
1) Capillary resistance test of Hess
2) Platelets count
3) Bleeding time
time needed for the platelet plug formation
If . N. ------ Normal 1ry homeostasis .
------ platelet or vascular defect.
HEMOSTASIS
Capillary resistance test of
Hess:
sphygmomanometer cuff above the cubital
fossa and raise the pressure to 100 mm Hg
(or midway between systolic & diastolic if
systolic pressure <100) for 5 - 7' minutes-
deflation '3 minutes later count the
number of petichea in area of 3 cm diameter,
1 cm below the cubital fossa Normally up
10 if more than 20, means platelets or
capillary wall defect
HEMOSTASIS
4) Other tests
only done if there is a prolonged bleeding
time with normal platelet count
- Measurement of capillary resistance
- Measurement of Willebrand factor
- Platelets function tests (Adhesiveness,
Aggregation)
- other tests for platelets (clot retraction,
prothrombin consumption).
HEMOSTASIS
Coagulation of Blood
Def :- represent the conversion of fibrinogen
(soluble protein) to fibrin (insoluble)
meshwork which occludes the point or
vessel rupture.
HEMOSTASIS
First Step :Activation of factor X
BY One of 2 systems:
I-urgent system II-delayed system
(Extrinsic system.) (Intrinsic system.)
HEMOSTASIS
systems of coagulation
I-urgent system. II-delayed system
Extrinsic system. Intrinsic system.
12-20'' (seconds) 4-8' (minutes)
In vivo only. In vivo & in vitro
Due to tissue damage. due to contact with foreign surface
Tissue factor activation of contact system
X < ------------------------------------IX a < ---------------- IX
Xa
2- prothrombin thrombin
3-fibrinogen Fibrin
HEMOSTASIS
EXTRINSIC SYSTEM
FACTORS NICESSORY ARE:
Factor X
Tissue factor and Factor VII
Tissue F.
VIIa VII
Xa X
Blood vessel
HEMOSTASIS
INTRINSIC SYSTEM
Necessary factors: -
XII (Hageman factor)
- Contact system XI
Kallikrene
kininogene
- F. IX
- F. VIII
- F. X
- Ca. ++
- phospholipids of the platelets membrane
HEMOSTASIS
Contact System:
Foreign surface
|--------------------------------------------------|
Kalierne XII kininogene
Fragmentation
XIIa
XI XIa
Rest of intrinsic pathway
IX
HEMOSTASIS
Rest of intrinsic pathway
IX
Platelets
Ca ++
IXa
X VIIIa
VIII
Xa
II IIa
HEMOSTASIS
Second Step: of Coagulation
Thrombin Formation: (IIa)
Factors needed:
- prothrombin (II) Ca++ platelets
- Xa II V Ca++
- V (acceleririe) Xa
- phospholipids
- Ca + + IIa
HEMOSTASIS
3
rd
Step :Fibrin Formation
Fibrin Formation:-
------------------------
IIa
XIII XIIIa
(Fibrinogen) -------------------- Ia
(Soluble fibrin)
Insoluble Fibrin
HEMOSTASIS
Physiological anticoagulants
1- Serine protease inhibitors :inhibit the
coagulation cascade.
2-Neutralizers of activated coagulation
factors (components of protein C system)
HEMOSTASIS
1-Serine protease inhibitors:
1-Antithrombin (III).
2-Heparin and heparin like
substance.
3-Alpha 1 antitypsin.
4-Alpha 2 macroglobulin
HEMOSTASIS
2-Neutralizers of activated
coagulation factors :
(components of protein C
system)
1-Protein C: synthesized in the
liver, vit. K dependant, activated by
thrombin.
2-Thrombomodulin.
3-Protein S and C4b-binding
protein.
HEMOSTASIS
Fibrinolysis
, the clot fibrin is the process wherein a
, is broken down.Its coagulation product of
cuts the fibrin mesh plasmin enzyme main
at various places, leading to the
production of circulating fragments that are
or by the proteases cleared by other
liver and kidney
HEMOSTASIS
HEMOSTASIS
Measurement
When plasmin breaks down fibrin, a
number of soluble parts are
fibrin produced. These are called
(FDPs). FDPs degradation products
compete with thrombin, and so slow
down the conversion of fibrinogen to
fibrin (and thus slows down clot
formation).
Exploration of the coagulation
(I) whole blood clotting time
Normally 4-10 minutes
Generally ---> N. in platelets defects.
= coagulation defect
But not very sensitive: - only +ve when blood
coagulation is very defective
HEMOSTASIS HEMOSTA fibrinolysis
(Hyperfibrinolysis), SIS
(2) One stage prothrombin time:
general exploration or the extrinsic pathway
(Quick time)
N : 16-18 sec.
addition of tissue thromboplastin +
ca++ to decalcified plasma ---> measure
the time till coagulation occur.
& II , V , X VII, Affected by factors
fiboinogen (only severe defect)
HEMOSTASIS
(3) partial thromboplastin time (PTT)
or CKT(cephaline koalin time)
General exploration of the intrinsic pathway
clotting time of recalcified plasma in the
presence of phospholipid (cephaline),
while koalin powder for activation of
, XII Hageman factor'. Affected by factors
II , X , VIII , IX , XI
HEMOSTASIS
(4) Thrombin time
detect the defects in the conversion of
fibrinogen ---> fibrin
Measured by addition of thrombin to citrated
patients plasma
If polonged
Abnormalities of fibornogen
(hypo or hyper or dysfibrinogenemia)
Heparin
Presence of some abnormal proteinswhich inhibits the
polymerisation of monomers of fibrin. (e.g myeloma
protein
HEMOSTASIS
(5) Deficiency of F XIII (fibrin stabilizing
factor ) detected by noting the solubility of fibrin
in 5M urea or 1% monochloroacetic acid (can't
dissolve fibrin in the presence of factor XIII).In
congenital defect of f. XIII ---> dissolution of the
clot in <10.
(6) Assay for each cogulation factor is
available
HEMOSTASIS
(7) Detection of coagulation inhibitors:
1-Inhibitors for a specific factor (especially F. VIII)
usually ---> severe hemorrhage
2- Inhibitors against platelets or tissue
phospholipids ---> prolongation of tests of
coagulation (Quick or CKT) e.g L.E
but usually no hemorrhagic manifestations
3- if there is of Quick test or CKT or thrombine:-
50% of normal plasma + 50% of patient plasma
(incubation at 370c for I hour) repeat the test
If become normal ---> factor defect
if no correction ---> presence of inhibitors.
HEMOSTASIS
PRACTICAL INVESTIGATION OF
HEMOSTATIC TROUBLE
B.T
Platelets count
Quick test
CKT
Thrombin time
Dosage of fibrinogen
HEMOSTASIS
PRACTICAL INVESTIGATION OF
HEMOSTATIC TROUBLE
I- B.T, platelets ( 80.000; mm3)
Thrombocytopenia
2- B.T, platelets normal
Qualitative platelets abnormalities Willebrand disease
congenital or acquired
platelet factor tests dosage of factor VIII
HEMOSTASIS
PRACTICAL INVESTIGATION OF
HEMOSTATIC TROUBLE
3- Quick + CKT Other tests are N
Acquired defect of several defect of factor common for
factors (II, VII, X,V) 2 pathways ex. X or V or II
4- Quick N., CKT: either:
I- Hemophilia Aor B.
2- Rarely ---> defect of one factor of the contact system
(XII, or XI or others)
HEMOSTASIS
PRACTICAL INVESTIGATION OF
HEMOSTATIC TROUBLE
5- Quick , CKT N
isolated defect of factor VII
in 3, 4..5 dosage of the factors with suspected deficiency,
also search for inhibitors. Ex:
- Quick, normal dosage of factors--->
hyperfibriongenemia which inhibit the test
- Quick +CKT + no F. defect --->? Inhibitors, e.g.
antiphospholipides.
HEMOSTASIS
PRACTICAL INVESTIGATION OF
HEMOSTATIC TROUBLE
6-T.T either:
* heparine in the blood or in the tube. Here T.T
can be corrected by adding either
a- toluidine blue
b-Reptilase time (incomplete thrombin not
sensitive to heparin and not inhibited by
antithrombin III).
* If (a-b also defective) ---> troubles of fibrin
polymerisation :either due to abnormal fibrin
(dysfibrinogenimia) or inhibition e.g by --->
myeloma protein or F.D.P.
HEMOSTASIS
PRACTICAL INVESTIGATION OF
HEMOSTATIC TROUBLE
7- fibrinogen
* congenital afibrinogenimia or
hypofibrinogenimia
Acquired hypofibrinogenimia e.g.liver
cirrhosis.
consumption of fibrinogen: e.g. D.I.V.C,
fibrinolysis
HEMOSTASIS
8-All tests ate Normal:
* Capillary fragility (usually only
ecchymoses ) ---> measurement of
cap.fragility.
* deficient factor XIII
* no hemostatic troubles.
PRACTICAL INVESTIGATION OF
HEMOSTATIC TROUBLE
HEMOSTASIS
HEMOSTASIS
Das könnte Ihnen auch gefallen
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)Von EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Bewertung: 4.5 von 5 Sternen4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryVon EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryBewertung: 3.5 von 5 Sternen3.5/5 (231)
- Grit: The Power of Passion and PerseveranceVon EverandGrit: The Power of Passion and PerseveranceBewertung: 4 von 5 Sternen4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaVon EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaBewertung: 4.5 von 5 Sternen4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItVon EverandNever Split the Difference: Negotiating As If Your Life Depended On ItBewertung: 4.5 von 5 Sternen4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerVon EverandThe Emperor of All Maladies: A Biography of CancerBewertung: 4.5 von 5 Sternen4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingVon EverandThe Little Book of Hygge: Danish Secrets to Happy LivingBewertung: 3.5 von 5 Sternen3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeVon EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeBewertung: 4 von 5 Sternen4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyVon EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyBewertung: 3.5 von 5 Sternen3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeVon EverandShoe Dog: A Memoir by the Creator of NikeBewertung: 4.5 von 5 Sternen4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreVon EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreBewertung: 4 von 5 Sternen4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersVon EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersBewertung: 4.5 von 5 Sternen4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnVon EverandTeam of Rivals: The Political Genius of Abraham LincolnBewertung: 4.5 von 5 Sternen4.5/5 (234)
- Her Body and Other Parties: StoriesVon EverandHer Body and Other Parties: StoriesBewertung: 4 von 5 Sternen4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceVon EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceBewertung: 4 von 5 Sternen4/5 (895)
- The Unwinding: An Inner History of the New AmericaVon EverandThe Unwinding: An Inner History of the New AmericaBewertung: 4 von 5 Sternen4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureVon EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureBewertung: 4.5 von 5 Sternen4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealVon EverandOn Fire: The (Burning) Case for a Green New DealBewertung: 4 von 5 Sternen4/5 (74)
- Pediatrics Notes, SOAP, DischargeDokument5 SeitenPediatrics Notes, SOAP, DischargeQurrataini IbanezNoch keine Bewertungen
- The Yellow House: A Memoir (2019 National Book Award Winner)Von EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Bewertung: 4 von 5 Sternen4/5 (98)
- Anxiety DisorderDokument62 SeitenAnxiety DisorderQurrataini Ibanez100% (3)
- Pre Employment Medical Examination Form - RS - pt.FIDokument3 SeitenPre Employment Medical Examination Form - RS - pt.FINooB GAMING100% (1)
- Bleeding Time, Clotting Time PT and PTT2Dokument41 SeitenBleeding Time, Clotting Time PT and PTT2Qurrataini Ibanez100% (1)
- HydrocephalusDokument28 SeitenHydrocephalusQurrataini Ibanez100% (1)
- Common Gynecologic ProceduresDokument55 SeitenCommon Gynecologic ProceduresQurrataini IbanezNoch keine Bewertungen
- Basic Nutrition MC Questions With AnswersDokument4 SeitenBasic Nutrition MC Questions With AnswersAbo SoltanNoch keine Bewertungen
- Pedia NotesDokument8 SeitenPedia NotesQurrataini IbanezNoch keine Bewertungen
- Pediatric Reference Ranges Endocrinology 0981 PDFDokument14 SeitenPediatric Reference Ranges Endocrinology 0981 PDFMMCSTORENoch keine Bewertungen
- CBC Parameters and QCDokument17 SeitenCBC Parameters and QCQurrataini IbanezNoch keine Bewertungen
- Chapter 17Dokument44 SeitenChapter 17Qurrataini IbanezNoch keine Bewertungen
- Grading of TonsilDokument3 SeitenGrading of TonsilQurrataini IbanezNoch keine Bewertungen
- Grading of TonsilDokument1 SeiteGrading of TonsilQurrataini IbanezNoch keine Bewertungen
- Chemotherapeutic AgentDokument29 SeitenChemotherapeutic AgentQurrataini IbanezNoch keine Bewertungen
- Fungal Infections: Alma E. Malilong, MD, FPSPDokument33 SeitenFungal Infections: Alma E. Malilong, MD, FPSPQurrataini IbanezNoch keine Bewertungen
- ToxicologyDokument11 SeitenToxicologyQurrataini IbanezNoch keine Bewertungen
- BSFCR Cardio Case Group 1Dokument23 SeitenBSFCR Cardio Case Group 1Qurrataini IbanezNoch keine Bewertungen
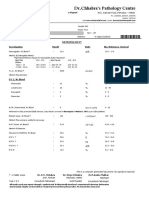
- DR - Chhabra's Pathology Centre: E-ReportDokument6 SeitenDR - Chhabra's Pathology Centre: E-ReportHimanshu KalaNoch keine Bewertungen
- Diabetes Related CKD 2Dokument1 SeiteDiabetes Related CKD 2Jia-PeiWuNoch keine Bewertungen
- Austin Journal of Nephrology and HypertensionDokument4 SeitenAustin Journal of Nephrology and HypertensionAustin Publishing GroupNoch keine Bewertungen
- CIMS Health Checkup Brochure (English) PDFDokument4 SeitenCIMS Health Checkup Brochure (English) PDFVaibhavNoch keine Bewertungen
- Diagnostic Tests in CardiologyDokument38 SeitenDiagnostic Tests in CardiologyDea Amelia YolandaNoch keine Bewertungen
- Normal Lab Values - Common Laboratory ValuesDokument4 SeitenNormal Lab Values - Common Laboratory ValuesMed PhuongNoch keine Bewertungen
- Clotting Time PDFDokument17 SeitenClotting Time PDFKhaled ZatariNoch keine Bewertungen
- Bleeding Time PDFDokument6 SeitenBleeding Time PDFMedic Guru100% (1)
- Tracking of Glycated Hemoglobin in The Original Cohort of The Framingham Heart StudyDokument7 SeitenTracking of Glycated Hemoglobin in The Original Cohort of The Framingham Heart StudySanghita BiswasNoch keine Bewertungen
- HDL DirectDokument2 SeitenHDL DirectDinesh SreedharanNoch keine Bewertungen
- IsoflavonsDokument23 SeitenIsoflavonsPiyush KhetrapalNoch keine Bewertungen
- Lipase Determination: Pipette Into Cuvettes Standard Sample/ControlDokument8 SeitenLipase Determination: Pipette Into Cuvettes Standard Sample/ControlJed BananiaNoch keine Bewertungen
- Task 9 Glucose EstimationDokument2 SeitenTask 9 Glucose EstimationJhenard John Lansangan BeltranNoch keine Bewertungen
- WS5 Structure and Properties of Fatty AcidsDokument2 SeitenWS5 Structure and Properties of Fatty AcidsDanielle SibayNoch keine Bewertungen
- Unit 1: Macromolecules: Food Tests: Outu - Be/Slp8Dcnwnj GDokument4 SeitenUnit 1: Macromolecules: Food Tests: Outu - Be/Slp8Dcnwnj GManan PatelNoch keine Bewertungen
- 1 s2.0 S0889157519310865 MainDokument8 Seiten1 s2.0 S0889157519310865 MainElvin TristanoNoch keine Bewertungen
- 36 Things For Heart Health - Reader's Digest - April 2018 UKDokument8 Seiten36 Things For Heart Health - Reader's Digest - April 2018 UKRamji RaoNoch keine Bewertungen
- CONTENTDokument13 SeitenCONTENTajeethaNoch keine Bewertungen
- Mark Scheme (Results) October 2019Dokument24 SeitenMark Scheme (Results) October 2019Zaid SulimanNoch keine Bewertungen
- Clonin ModelDokument9 SeitenClonin ModelNano AlmukasabyNoch keine Bewertungen
- Lyphochek Assayed Chemistry Control Levels 1 and 2: Erba XL SeriesDokument2 SeitenLyphochek Assayed Chemistry Control Levels 1 and 2: Erba XL SeriesMDD EngineeringNoch keine Bewertungen
- Diabetes Obesity Metabolism - 2022 - Wilding - Weight Regain and Cardiometabolic Effects After Withdrawal of SemaglutideDokument12 SeitenDiabetes Obesity Metabolism - 2022 - Wilding - Weight Regain and Cardiometabolic Effects After Withdrawal of SemaglutideElisa Villasana EguiluzNoch keine Bewertungen
- Case StudyDokument1 SeiteCase Studyapi-311718939Noch keine Bewertungen
- PT Cakra Medika Utama: Price List Boditech Med Inc (I-Chroma)Dokument2 SeitenPT Cakra Medika Utama: Price List Boditech Med Inc (I-Chroma)raditNoch keine Bewertungen
- Biocheistry Viva Question BankDokument5 SeitenBiocheistry Viva Question BankNIHAR UTHALENoch keine Bewertungen
- Effects of Dietary Chitosan On Serum Lipid and Lipoprotein Concentrations in RatsDokument5 SeitenEffects of Dietary Chitosan On Serum Lipid and Lipoprotein Concentrations in RatsEi Ei ThetNoch keine Bewertungen
- Human Nutrition 1 QPDokument11 SeitenHuman Nutrition 1 QPAzween SabtuNoch keine Bewertungen